- Research article
- Open access
- Published: 10 April 2021

The role of artificial intelligence in healthcare: a structured literature review
- Silvana Secinaro 1 ,
- Davide Calandra 1 ,
- Aurelio Secinaro 2 ,
- Vivek Muthurangu 3 &
- Paolo Biancone 1
BMC Medical Informatics and Decision Making volume 21 , Article number: 125 ( 2021 ) Cite this article
161k Accesses
306 Citations
28 Altmetric
Metrics details
Background/Introduction
Artificial intelligence (AI) in the healthcare sector is receiving attention from researchers and health professionals. Few previous studies have investigated this topic from a multi-disciplinary perspective, including accounting, business and management, decision sciences and health professions.
The structured literature review with its reliable and replicable research protocol allowed the researchers to extract 288 peer-reviewed papers from Scopus. The authors used qualitative and quantitative variables to analyse authors, journals, keywords, and collaboration networks among researchers. Additionally, the paper benefited from the Bibliometrix R software package.
The investigation showed that the literature in this field is emerging. It focuses on health services management, predictive medicine, patient data and diagnostics, and clinical decision-making. The United States, China, and the United Kingdom contributed the highest number of studies. Keyword analysis revealed that AI can support physicians in making a diagnosis, predicting the spread of diseases and customising treatment paths.
Conclusions
The literature reveals several AI applications for health services and a stream of research that has not fully been covered. For instance, AI projects require skills and data quality awareness for data-intensive analysis and knowledge-based management. Insights can help researchers and health professionals understand and address future research on AI in the healthcare field.
Peer Review reports
Artificial intelligence (AI) generally applies to computational technologies that emulate mechanisms assisted by human intelligence, such as thought, deep learning, adaptation, engagement, and sensory understanding [ 1 , 2 ]. Some devices can execute a role that typically involves human interpretation and decision-making [ 3 , 4 ]. These techniques have an interdisciplinary approach and can be applied to different fields, such as medicine and health. AI has been involved in medicine since as early as the 1950s, when physicians made the first attempts to improve their diagnoses using computer-aided programs [ 5 , 6 ]. Interest and advances in medical AI applications have surged in recent years due to the substantially enhanced computing power of modern computers and the vast amount of digital data available for collection and utilisation [ 7 ]. AI is gradually changing medical practice. There are several AI applications in medicine that can be used in a variety of medical fields, such as clinical, diagnostic, rehabilitative, surgical, and predictive practices. Another critical area of medicine where AI is making an impact is clinical decision-making and disease diagnosis. AI technologies can ingest, analyse, and report large volumes of data across different modalities to detect disease and guide clinical decisions [ 3 , 8 ]. AI applications can deal with the vast amount of data produced in medicine and find new information that would otherwise remain hidden in the mass of medical big data [ 9 , 10 , 11 ]. These technologies can also identify new drugs for health services management and patient care treatments [ 5 , 6 ].
Courage in the application of AI is visible through a search in the primary research databases. However, as Meskò et al. [ 7 ] find, the technology will potentially reduce care costs and repetitive operations by focusing the medical profession on critical thinking and clinical creativity. As Cho et al. and Doyle et al. [ 8 , 9 ] add, the AI perspective is exciting; however, new studies will be needed to establish the efficacy and applications of AI in the medical field [ 10 ].
Our paper will also concentrate on AI strategies for healthcare from the accounting, business, and management perspectives. The authors used the structured literature review (SLR) method for its reliable and replicable research protocol [ 11 ] and selected bibliometric variables as sources of investigation. Bibliometric usage enables the recognition of the main quantitative variables of the study stream [ 12 ]. This method facilitates the detection of the required details of a particular research subject, including field authors, number of publications, keywords for interaction between variables (policies, properties and governance) and country data [ 13 ]. It also allows the application of the science mapping technique [ 14 ]. Our paper adopted the Bibliometrix R package and the biblioshiny web interface as tools of analysis [ 14 ].
The investigation offers the following insights for future researchers and practitioners:
bibliometric information on 288 peer-reviewed English papers from the Scopus collection.
Identification of leading journals in this field, such as Journal of Medical Systems, Studies in Health Technology and Informatics, IEEE Journal of Biomedical and Health Informatics, and Decision Support Systems.
Qualitative and quantitative information on authors’ Lotka’s law, h-index, g-index, m-index, keyword, and citation data.
Research on specific countries to assess AI in the delivery and effectiveness of healthcare, quotes, and networks within each region.
A topic dendrogram study that identifies five research clusters: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making.
An in-depth discussion that develops theoretical and practical implications for future studies.
The paper is organised as follows. Section 2 lists the main bibliometric articles in this field. Section 3 elaborates on the methodology. Section 4 presents the findings of the bibliometric analysis. Section 5 discusses the main elements of AI in healthcare based on the study results. Section 6 concludes the article with future implications for research.
Related works and originality
As suggested by Zupic and Čater [ 15 ], a research stream can be evaluated with bibliometric methods that can introduce objectivity and mitigate researcher bias. For this reason, bibliometric methods are attracting increasing interest among researchers as a reliable and impersonal research analytical approach [ 16 , 17 ]. Recently, bibliometrics has been an essential method for analysing and predicting research trends [ 18 ]. Table 1 lists other research that has used a similar approach in the research stream investigated.
The scientific articles reported show substantial differences in keywords and research topics that have been previously studied. The bibliometric analysis of Huang et al. [ 19 ] describes rehabilitative medicine using virtual reality technology. According to the authors, the primary goal of rehabilitation is to enhance and restore functional ability and quality of life for patients with physical impairments or disabilities. In recent years, many healthcare disciplines have been privileged to access various technologies that provide tools for both research and clinical intervention.
Hao et al. [ 20 ] focus on text mining in medical research. As reported, text mining reveals new, previously unknown information by using a computer to automatically extract information from different text resources. Text mining methods can be regarded as an extension of data mining to text data. Text mining is playing an increasingly significant role in processing medical information. Similarly, the studies by dos Santos et al. [ 21 ] focus on applying data mining and machine learning (ML) techniques to public health problems. As stated in this research, public health may be defined as the art and science of preventing diseases, promoting health, and prolonging life. Using data mining and ML techniques, it is possible to discover new information that otherwise would be hidden. These two studies are related to another topic: medical big data. According to Liao et al. [ 22 ], big data is a typical “buzzword” in the business and research community, referring to a great mass of digital data collected from various sources. In the medical field, we can obtain a vast amount of data (i.e., medical big data). Data mining and ML techniques can help deal with this information and provide helpful insights for physicians and patients. More recently, Choudhury et al. [ 23 ] provide a systematic review on the use of ML to improve the care of elderly patients, demonstrating eligible studies primarily in psychological disorders and eye diseases.
Tran et al. [ 2 ] focus on the global evolution of AI research in medicine. Their bibliometric analysis highlights trends and topics related to AI applications and techniques. As stated in Connelly et al.’s [ 24 ] study, robot-assisted surgeries have rapidly increased in recent years. Their bibliometric analysis demonstrates how robotic-assisted surgery has gained acceptance in different medical fields, such as urological, colorectal, cardiothoracic, orthopaedic, maxillofacial and neurosurgery applications. Additionally, the bibliometric analysis of Guo et al. [ 25 ] provides an in-depth study of AI publications through December 2019. The paper focuses on tangible AI health applications, giving researchers an idea of how algorithms can help doctors and nurses. A new stream of research related to AI is also emerging. In this sense, Choudhury and Asan’s [ 26 ] scientific contribution provides a systematic review of the AI literature to identify health risks for patients. They report on 53 studies involving technology for clinical alerts, clinical reports, and drug safety. Considering the considerable interest within this research stream, this analysis differs from the current literature for several reasons. It aims to provide in-depth discussion, considering mainly the business, management, and accounting fields and not dealing only with medical and health profession publications.
Additionally, our analysis aims to provide a bibliometric analysis of variables such as authors, countries, citations and keywords to guide future research perspectives for researchers and practitioners, as similar analyses have done for several publications in other research streams [ 15 , 16 , 27 ]. In doing so, we use a different database, Scopus, that is typically adopted in social sciences fields. Finally, our analysis will propose and discuss a dominant framework of variables in this field, and our analysis will not be limited to AI application descriptions.
Methodology
This paper evaluated AI in healthcare research streams using the SLR method [ 11 ]. As suggested by Massaro et al. [ 11 ], an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers. As suggested by many scholars, the methodology allows qualitative and quantitative variables to highlight the best authors, journals and keywords and combine a systematic literature review and bibliometric analysis [ 27 , 28 , 29 , 30 ]. Despite its widespread use in business and management [ 16 , 31 ], the SLR is also used in the health sector based on the same philosophy through which it was originally conceived [ 32 , 33 ]. A methodological analysis of previously published articles reveals that the most frequently used steps are as follows [ 28 , 31 , 34 ]:
defining research questions;
writing the research protocol;
defining the research sample to be analysed;
developing codes for analysis; and
critically analysing, discussing, and identifying a future research agenda.
Considering the above premises, the authors believe that an SLR is the best method because it combines scientific validity, replicability of the research protocol and connection between multiple inputs.
As stated by the methodological paper, the first step is research question identification. For this purpose, we benefit from the analysis of Zupic and Čater [ 15 ], who provide several research questions for future researchers to link the study of authors, journals, keywords and citations. Therefore, RQ1 is “What are the most prominent authors, journal keywords and citations in the field of the research study?” Additionally, as suggested by Haleem et al. [ 35 ], new technologies, including AI, are changing the medical field in unexpected timeframes, requiring studies in multiple areas. Therefore, RQ2 is “How does artificial intelligence relate to healthcare, and what is the focus of the literature?” Then, as discussed by Massaro et al. [ 36 ], RQ3 is “What are the research applications of artificial intelligence for healthcare?”.
The first research question aims to define the qualitative and quantitative variables of the knowledge flow under investigation. The second research question seeks to determine the state of the art and applications of AI in healthcare. Finally, the third research question aims to help researchers identify practical and theoretical implications and future research ideas in this field.
The second fundamental step of the SLR is writing the research protocol [ 11 ]. Table 2 indicates the currently known literature elements, uniquely identifying the research focus, motivations and research strategy adopted and the results providing a link with the following points. Additionally, to strengthen the analysis, our investigation benefits from the PRISMA statement methodological article [ 37 ]. Although the SLR is a validated method for systematic reviews and meta-analyses, we believe that the workflow provided may benefit the replicability of the results [ 37 , 38 , 39 , 40 ]. Figure 1 summarises the researchers’ research steps, indicating that there are no results that can be referred to as a meta-analysis.
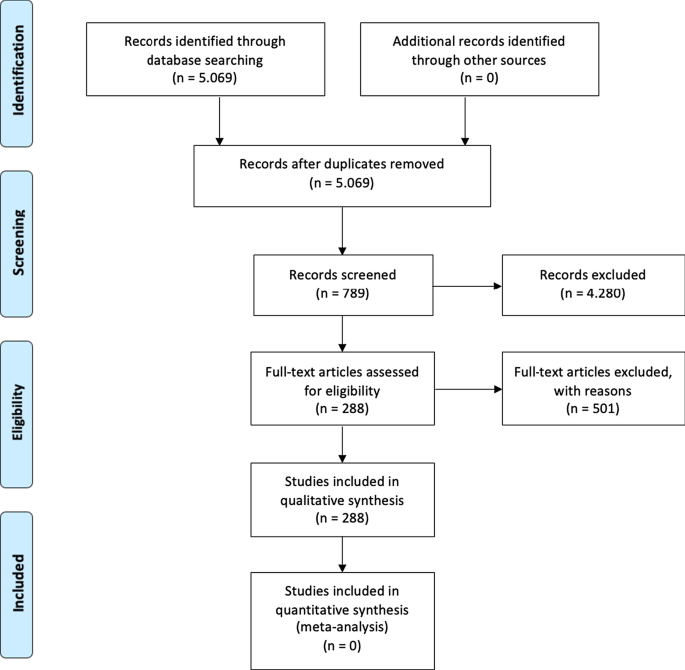
Source : Authors’ elaboration on Liberati et al. [ 37 ]
PRISMA workflow.
The third step is to specify the search strategy and search database. Our analysis is based on the search string “Artificial Intelligence” OR “AI” AND “Healthcare” with a focus on “Business, Management, and Accounting”, “Decision Sciences”, and “Health professions”. As suggested by [ 11 , 41 ] and motivated by [ 42 ], keywords can be selected through a top-down approach by identifying a large search field and then focusing on particular sub-topics. The paper uses data retrieved from the Scopus database, a multi-disciplinary database, which allowed the researchers to identify critical articles for scientific analysis [ 43 ]. Additionally, Scopus was selected based on Guo et al.’s [ 25 ] limitations, which suggest that “future studies will apply other databases, such as Scopus, to explore more potential papers” . The research focuses on articles and reviews published in peer-reviewed journals for their scientific relevance [ 11 , 16 , 17 , 29 ] and does not include the grey literature, conference proceedings or books/book chapters. Articles written in any language other than English were excluded [ 2 ]. For transparency and replicability, the analysis was conducted on 11 January 2021. Using this research strategy, the authors retrieved 288 articles. To strengthen the study's reliability, we publicly provide the full bibliometric extract on the Zenodo repository [ 44 , 45 ].
The fourth research phase is defining the code framework that initiates the analysis of the variables. The study will identify the following:
descriptive information of the research area;
source analysis [ 16 ];
author and citation analysis [ 28 ];
keywords and network analysis [ 14 ]; and
geographic distribution of the papers [ 14 ].
The final research phase is the article’s discussion and conclusion, where implications and future research trends will be identified.
At the research team level, the information is analysed with the statistical software R-Studio and the Bibliometrix package [ 15 ], which allows scientific analysis of the results obtained through the multi-disciplinary database.
The analysis of bibliometric results starts with a description of the main bibliometric statistics with the aim of answering RQ1, What are the most prominent authors, journal keywords and citations in the field of the research study?, and RQ2, How does artificial intelligence relate to healthcare, and what is the focus of the literature? Therefore, the following elements were thoroughly analysed: (1) type of document; (2) annual scientific production; (3) scientific sources; (4) source growth; (5) number of articles per author; (6) author’s dominance ranking; (7) author’s h-index, g-index, and m-index; (8) author’s productivity; (9) author’s keywords; (10) topic dendrogram; (11) a factorial map of the document with the highest contributions; (12) article citations; (13) country production; (14) country citations; (15) country collaboration map; and (16) country collaboration network.
Main information
Table 3 shows the information on 288 peer-reviewed articles published between 1992 and January 2021 extracted from the Scopus database. The number of keywords is 946 from 136 sources, and the number of keywords plus, referring to the number of keywords that frequently appear in an article’s title, was 2329. The analysis period covered 28 years and 1 month of scientific production and included an annual growth rate of 5.12%. However, the most significant increase in published articles occurred in the past three years (please see Fig. 2 ). On average, each article was written by three authors (3.56). Finally, the collaboration index (CI), which was calculated as the total number of authors of multi-authored articles/total number of multi-authored articles, was 3.97 [ 46 ].
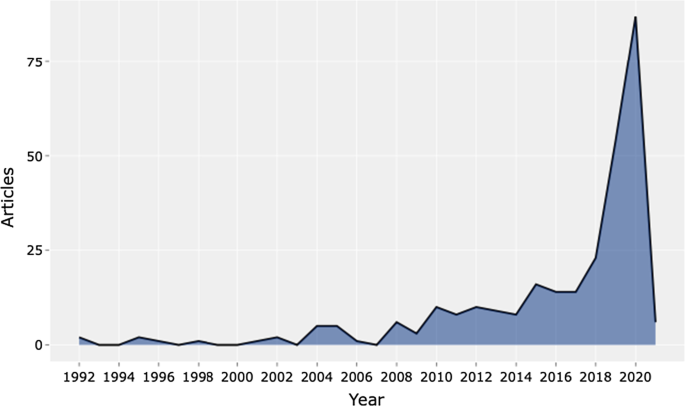
Source : Authors’ elaboration
Annual scientific production.
Table 4 shows the top 20 sources related to the topic. The Journal of Medical Systems is the most relevant source, with twenty-one of the published articles. This journal's main issues are the foundations, functionality, interfaces, implementation, impacts, and evaluation of medical technologies. Another relevant source is Studies in Health Technology and Informatics, with eleven articles. This journal aims to extend scientific knowledge related to biomedical technologies and medical informatics research. Both journals deal with cloud computing, machine learning, and AI as a disruptive healthcare paradigm based on recent publications. The IEEE Journal of Biomedical and Health Informatics investigates technologies in health care, life sciences, and biomedicine applications from a broad perspective. The next journal, Decision Support Systems, aims to analyse how these technologies support decision-making from a multi-disciplinary view, considering business and management. Therefore, the analysis of the journals revealed that we are dealing with an interdisciplinary research field. This conclusion is confirmed, for example, by the presence of purely medical journals, journals dedicated to the technological growth of healthcare, and journals with a long-term perspective such as futures.
The distribution frequency of the articles (Fig. 3 ) indicates the journals dealing with the topic and related issues. Between 2008 and 2012, a significant growth in the number of publications on the subject is noticeable. However, the graph shows the results of the Loess regression, which includes the quantity and publication time of the journal under analysis as variables. This method allows the function to assume an unlimited distribution; that is, feature can consider values below zero if the data are close to zero. It contributes to a better visual result and highlights the discontinuity in the publication periods [ 47 ].
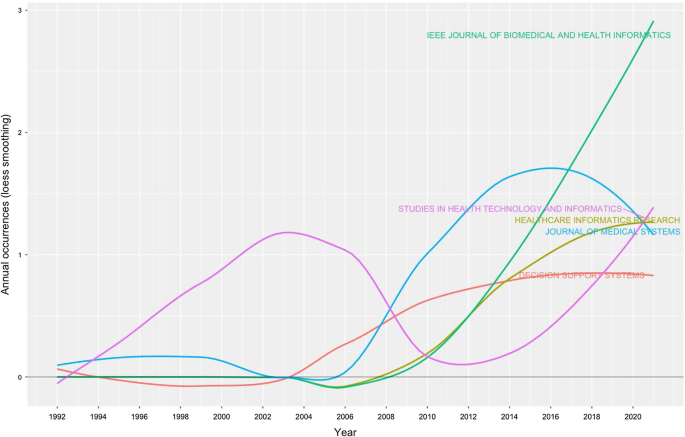
Source growth. Source : Authors’ elaboration
Finally, Fig. 4 provides an analytical perspective on factor analysis for the most cited papers. As indicated in the literature [ 48 , 49 ], using factor analysis to discover the most cited papers allows for a better understanding of the scientific world’s intellectual structure. For example, our research makes it possible to consider certain publications that effectively analyse subject specialisation. For instance, Santosh’s [ 50 ] article addresses the new paradigm of AI with ML algorithms for data analysis and decision support in the COVID-19 period, setting a benchmark in terms of citations by researchers. Moving on to the application, an article by Shickel et al. [ 51 ] begins with the belief that the healthcare world currently has much health and administrative data. In this context, AI and deep learning will support medical and administrative staff in extracting data, predicting outcomes, and learning medical representations. Finally, in the same line of research, Baig et al. [ 52 ], with a focus on wearable patient monitoring systems (WPMs), conclude that AI and deep learning may be landmarks for continuous patient monitoring and support for healthcare delivery.
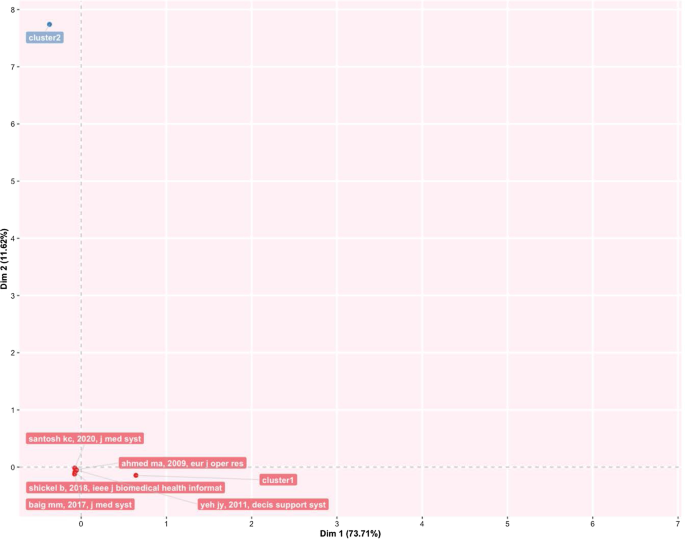
Factorial map of the most cited documents.
This section identifies the most cited authors of articles on AI in healthcare. It also identifies the authors’ keywords, dominance factor (DF) ranking, h-index, productivity, and total number of citations. Table 5 identifies the authors and their publications in the top 20 rankings. As the table shows, Bushko R.G. has the highest number of publications: four papers. He is the editor-in-chief of Future of Health Technology, a scientific journal that aims to develop a clear vision of the future of health technology. Then, several authors each wrote three papers. For instance, Liu C. is a researcher active in the topic of ML and computer vision, and Sharma A. from Emory University Atlanta in the USA is a researcher with a clear focus on imaging and translational informatics. Some other authors have two publications each. While some authors have published as primary authors, most have published as co-authors. Hence, in the next section, we measure the contributory power of each author by investigating the DF ranking through the number of elements.
Authors’ dominance ranking
The dominance factor (DF) is a ratio measuring the fraction of multi-authored articles in which an author acts as the first author [ 53 ]. Several bibliometric studies use the DF in their analyses [ 46 , 54 ]. The DF ranking calculates an author’s dominance in producing articles. The DF is calculated by dividing the number of an author’s multi-authored papers as the first author (Nmf) by the author's total number of multi-authored papers (Nmt). This is omitted in the single-author case due to the constant value of 1 for single-authored articles. This formulation could lead to some distortions in the results, especially in fields where the first author is entered by surname alphabetical order [ 55 ].
The mathematical equation for the DF is shown as:
Table 6 lists the top 20 DF rankings. The data in the table show a low level of articles per author, either for first-authored or multi-authored articles. The results demonstrate that we are dealing with an emerging topic in the literature. Additionally, as shown in the table, Fox J. and Longoni C. are the most dominant authors in the field.
Authors’ impact
Table 7 shows the impact of authors in terms of the h-index [ 56 ] (i.e., the productivity and impact of citations of a researcher), g-index [ 57 ] (i.e., the distribution of citations received by a researcher's publications), m-index [ 58 ] (i.e., the h-index value per year), total citations, total paper and years of scientific publication. The H-index was introduced in the literature as a metric for the objective comparison of scientific results and depended on the number of publications and their impact [ 59 ]. The results show that the 20 most relevant authors have an h-index between 2 and 1. For the practical interpretation of the data, the authors considered data published by the London School of Economics [ 60 ]. In the social sciences, the analysis shows values of 7.6 for economic publications by professors and researchers who had been active for several years. Therefore, the youthfulness of the research area has attracted young researchers and professors. At the same time, new indicators have emerged over the years to diversify the logic of the h-index. For example, the g-index indicates an author's impact on citations, considering that a single article can generate these. The m-index, on the other hand, shows the cumulative value over the years.
The analysis, also considering the total number of citations, the number of papers published and the year of starting to publish, thus confirms that we are facing an expanding research flow.
Authors’ productivity
Figure 5 shows Lotka’s law. This mathematical formulation originated in 1926 to describe the publication frequency by authors in a specific research field [ 61 ]. In practice, the law states that the number of authors contributing to research in a given period is a fraction of the number who make up a single contribution [ 14 , 61 ].
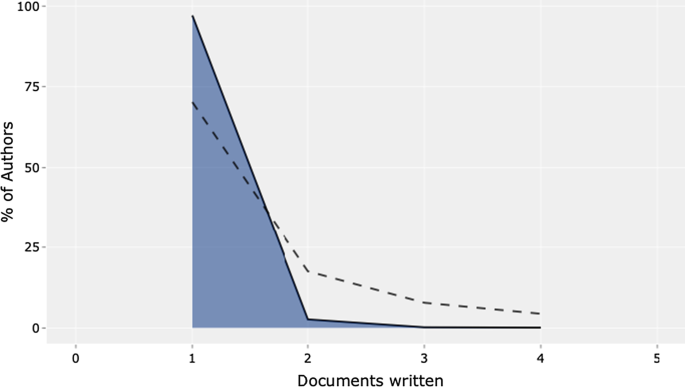
Lotka’s law.
The mathematical relationship is expressed in reverse in the following way:
where y x is equal to the number of authors producing x articles in each research field. Therefore, C and n are constants that can be estimated in the calculation.
The figure's results are in line with Lotka's results, with an average of two publications per author in a given research field. In addition, the figure shows the percentage of authors. Our results lead us to state that we are dealing with a young and growing research field, even with this analysis. Approximately 70% of the authors had published only their first research article. Only approximately 20% had published two scientific papers.
Authors’ keywords
This section provides information on the relationship between the keywords artificial intelligence and healthcare . This analysis is essential to determine the research trend, identify gaps in the discussion on AI in healthcare, and identify the fields that can be interesting as research areas [ 42 , 62 ].
Table 8 highlights the total number of keywords per author in the top 20 positions. The ranking is based on the following elements: healthcare, artificial intelligence, and clinical decision support system . Keyword analysis confirms the scientific area of reference. In particular, we deduce the definition as “Artificial intelligence is the theory and development of computer systems able to perform tasks normally requiring human intelligence, such as visual perception, speech recognition, decision-making, and translation between languages” [ 2 , 63 ]. Panch et al. [ 4 ] find that these technologies can be used in different business and management areas. After the first keyword, the analysis reveals AI applications and related research such as machine learning and deep learning.
Additionally, data mining and big data are a step forward in implementing exciting AI applications. According to our specific interest, if we applied AI in healthcare, we would achieve technological applications to help and support doctors and medical researchers in decision-making. The link between AI and decision-making is the reason why we find, in the seventh position, the keyword clinical decision support system . AI techniques can unlock clinically relevant information hidden in the massive amount of data that can assist clinical decision-making [ 64 ]. If we analyse the following keywords, we find other elements related to decision-making and support systems.
The TreeMap below (Fig. 6 ) highlights the combination of possible keywords representing AI and healthcare.
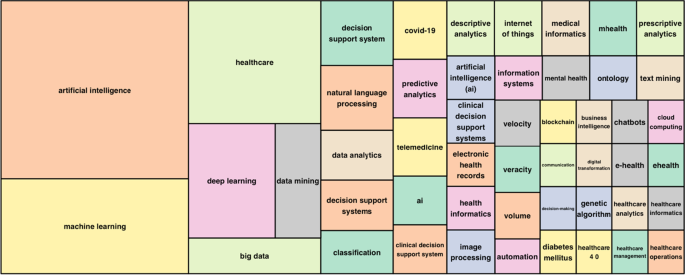
Keywords treemap.
The topic dendrogram in Fig. 7 represents the hierarchical order and the relationship between the keywords generated by hierarchical clustering [ 42 ]. The cut in the figure and the vertical lines facilitate an investigation and interpretation of the different clusters. As stated by Andrews [ 48 ], the figure is not intended to find the perfect level of associations between clusters. However, it aims to estimate the approximate number of clusters to facilitate further discussion.
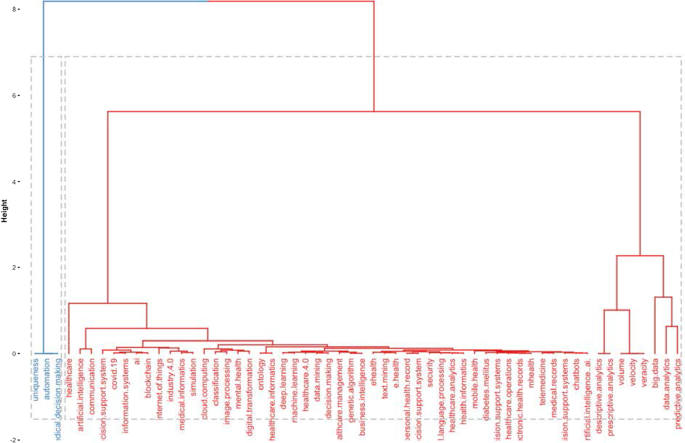
Topic dendrogram.
The research stream of AI in healthcare is divided into two main strands. The blue strand focuses on medical information systems and the internet. Some papers are related to healthcare organisations, such as the Internet of Things, meaning that healthcare organisations use AI to support health services management and data analysis. AI applications are also used to improve diagnostic and therapeutic accuracy and the overall clinical treatment process [ 2 ]. If we consider the second block, the red one, three different clusters highlight separate aspects of the topic. The first could be explained as AI and ML predictive algorithms. Through AI applications, it is possible to obtain a predictive approach that can ensure that patients are better monitored. This also allows a better understanding of risk perception for doctors and medical researchers. In the second cluster, the most frequent words are decisions , information system , and support system . This means that AI applications can support doctors and medical researchers in decision-making. Information coming from AI technologies can be used to consider difficult problems and support a more straightforward and rapid decision-making process. In the third cluster, it is vital to highlight that the ML model can deal with vast amounts of data. From those inputs, it can return outcomes that can optimise the work of healthcare organisations and scheduling of medical activities.
Furthermore, the word cloud in Fig. 8 highlights aspects of AI in healthcare, such as decision support systems, decision-making, health services management, learning systems, ML techniques and diseases. The figure depicts how AI is linked to healthcare and how it is used in medicine.
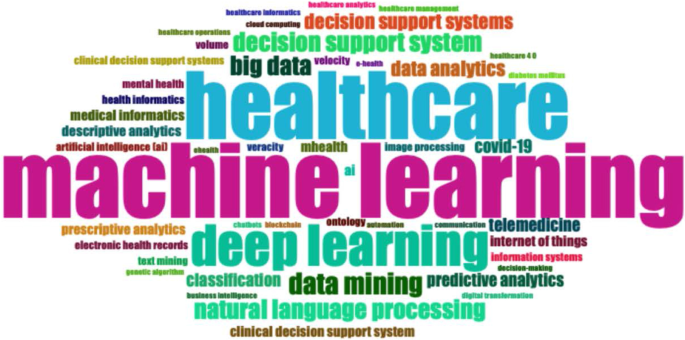
Word cloud.
Figure 9 represents the search trends based on the keywords analysed. The research started in 2012. First, it identified research topics related to clinical decision support systems. This topic was recurrent during the following years. Interestingly, in 2018, studies investigated AI and natural language processes as possible tools to manage patients and administrative elements. Finally, a new research stream considers AI's role in fighting COVID-19 [ 65 , 66 ].
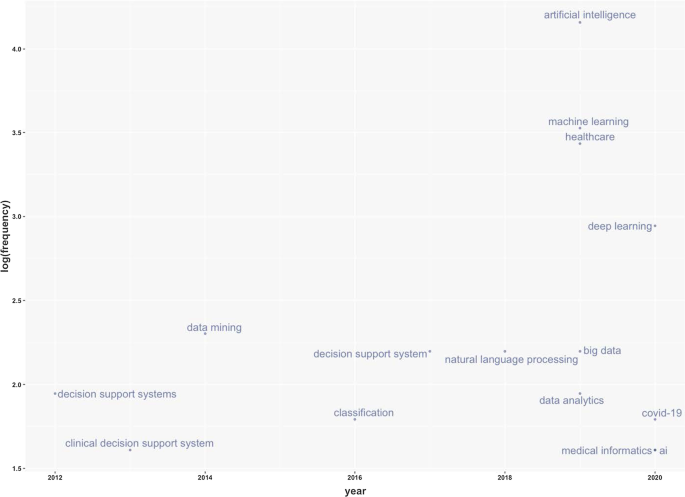
Keywords frequency.
Table 9 represents the number of citations from other articles within the top 20 rankings. The analysis allows the benchmark studies in the field to be identified [ 48 ]. For instance, Burke et al. [ 67 ] writes the most cited paper and analyses efficient nurse rostering methodologies. The paper critically evaluates tangible interdisciplinary solutions that also include AI. Immediately thereafter, Ahmed M.A.'s article proposes a data-driven optimisation methodology to determine the optimal number of healthcare staff to optimise patients' productivity [ 68 ]. Finally, the third most cited article lays the groundwork for developing deep learning by considering diverse health and administrative information [ 51 ].
This section analyses the diffusion of AI in healthcare around the world. It highlights countries to show the geographies of this research. It includes all published articles, the total number of citations, and the collaboration network. The following sub-sections start with an analysis of the total number of published articles.
Country total articles
Figure 9 and Table 10 display the countries where AI in healthcare has been considered. The USA tops the list of countries with the maximum number of articles on the topic (215). It is followed by China (83), the UK (54), India (51), Australia (54), and Canada (32). It is immediately evident that the theme has developed on different continents, highlighting a growing interest in AI in healthcare. The figure shows that many areas, such as Russia, Eastern Europe and Africa except for Algeria, Egypt, and Morocco, have still not engaged in this scientific debate.
Country publications and collaboration map
This section discusses articles on AI in healthcare in terms of single or multiple publications in each country. It also aims to observe collaboration and networking between countries. Table 11 and Fig. 10 highlight the average citations by state and show that the UK, the USA, and Kuwait have a higher average number of citations than other countries. Italy, Spain and New Zealand have the most significant number of citations.
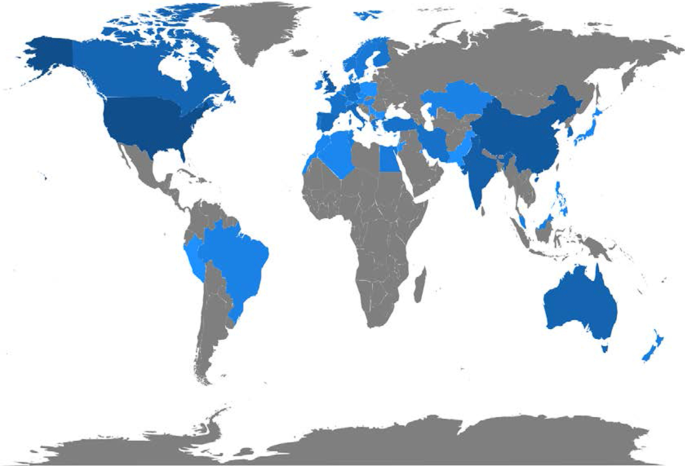
Articles per country.
Figure 11 depicts global collaborations. The blue colour on the map represents research cooperation among nations. Additionally, the pink border linking states indicates the extent of collaboration between authors. The primary cooperation between nations is between the USA and China, with two collaborative articles. Other collaborations among nations are limited to a few papers.
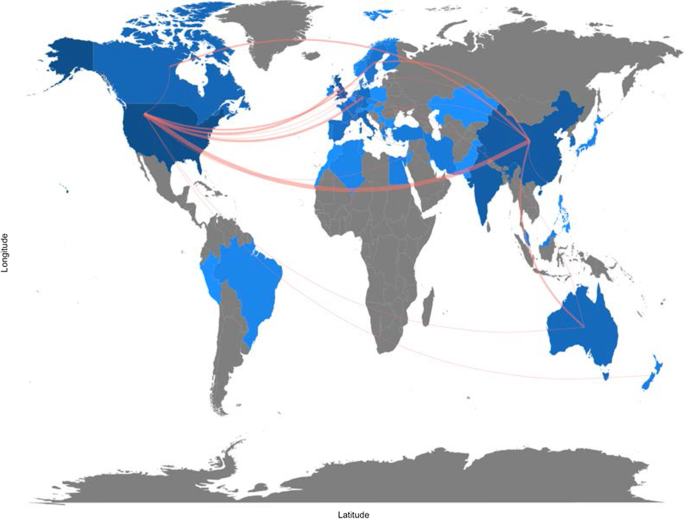
Collaboration map.
Artificial intelligence for healthcare: applications
This section aims to strengthen the research scope by answering RQ3: What are the research applications of artificial intelligence for healthcare?
Benefiting from the topical dendrogram, researchers will provide a development model based on four relevant variables [ 69 , 70 ]. AI has been a disruptive innovation in healthcare [ 4 ]. With its sophisticated algorithms and several applications, AI has assisted doctors and medical professionals in the domains of health information systems, geocoding health data, epidemic and syndromic surveillance, predictive modelling and decision support, and medical imaging [ 2 , 9 , 10 , 64 ]. Furthermore, the researchers considered the bibliometric analysis to identify four macro-variables dominant in the field and used them as authors' keywords. Therefore, the following sub-sections aim to explain the debate on applications in healthcare for AI techniques. These elements are shown in Fig. 12 .
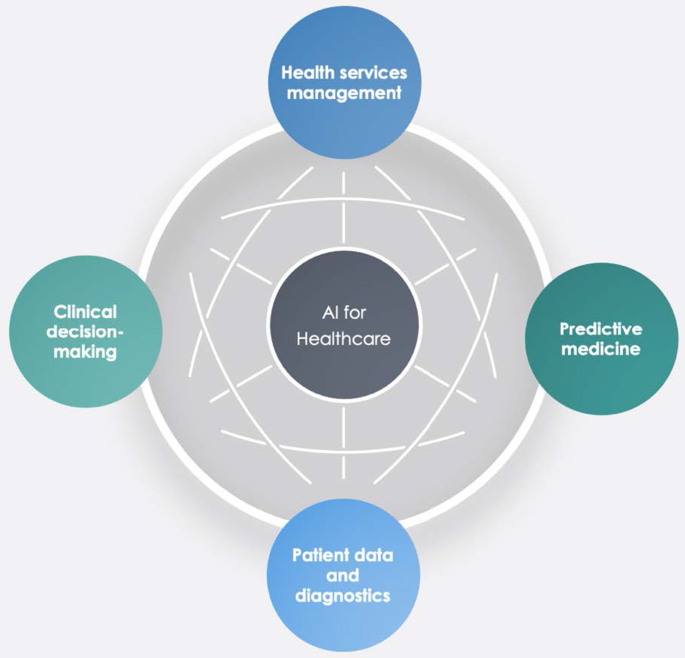
Dominant variables for AI in healthcare.
Health services management
One of the notable aspects of AI techniques is potential support for comprehensive health services management. These applications can support doctors, nurses and administrators in their work. For instance, an AI system can provide health professionals with constant, possibly real-time medical information updates from various sources, including journals, textbooks, and clinical practices [ 2 , 10 ]. These applications' strength is becoming even more critical in the COVID-19 period, during which information exchange is continually needed to properly manage the pandemic worldwide [ 71 ]. Other applications involve coordinating information tools for patients and enabling appropriate inferences for health risk alerts and health outcome prediction [ 72 ]. AI applications allow, for example, hospitals and all health services to work more efficiently for the following reasons:
Clinicians can access data immediately when they need it.
Nurses can ensure better patient safety while administering medication.
Patients can stay informed and engaged in their care by communicating with their medical teams during hospital stays.
Additionally, AI can contribute to optimising logistics processes, for instance, realising drugs and equipment in a just-in-time supply system based totally on predictive algorithms [ 73 , 74 ]. Interesting applications can also support the training of personnel working in health services. This evidence could be helpful in bridging the gap between urban and rural health services [ 75 ]. Finally, health services management could benefit from AI to leverage the multiplicity of data in electronic health records by predicting data heterogeneity across hospitals and outpatient clinics, checking for outliers, performing clinical tests on the data, unifying patient representation, improving future models that can predict diagnostic tests and analyses, and creating transparency with benchmark data for analysing services delivered [ 51 , 76 ].
Predictive medicine
Another relevant topic is AI applications for disease prediction and diagnosis treatment, outcome prediction and prognosis evaluation [ 72 , 77 ]. Because AI can identify meaningful relationships in raw data, it can support diagnostic, treatment and prediction outcomes in many medical situations [ 64 ]. It allows medical professionals to embrace the proactive management of disease onset. Additionally, predictions are possible for identifying risk factors and drivers for each patient to help target healthcare interventions for better outcomes [ 3 ]. AI techniques can also help design and develop new drugs, monitor patients and personalise patient treatment plans [ 78 ]. Doctors benefit from having more time and concise data to make better patient decisions. Automatic learning through AI could disrupt medicine, allowing prediction models to be created for drugs and exams that monitor patients over their whole lives [ 79 ].
- Clinical decision-making
One of the keyword analysis main topics is that AI applications could support doctors and medical researchers in the clinical decision-making process. According to Jiang et al. [ 64 ], AI can help physicians make better clinical decisions or even replace human judgement in healthcare-specific functional areas. According to Bennett and Hauser [ 80 ], algorithms can benefit clinical decisions by accelerating the process and the amount of care provided, positively impacting the cost of health services. Therefore, AI technologies can support medical professionals in their activities and simplify their jobs [ 4 ]. Finally, as Redondo and Sandoval [ 81 ] find, algorithmic platforms can provide virtual assistance to help doctors understand the semantics of language and learning to solve business process queries as a human being would.
Patient data and diagnostics
Another challenging topic related to AI applications is patient data and diagnostics. AI techniques can help medical researchers deal with the vast amount of data from patients (i.e., medical big data ). AI systems can manage data generated from clinical activities, such as screening, diagnosis, and treatment assignment. In this way, health personnel can learn similar subjects and associations between subject features and outcomes of interest [ 64 ].
These technologies can analyse raw data and provide helpful insights that can be used in patient treatments. They can help doctors in the diagnostic process; for example, to realise a high-speed body scan, it will be simpler to have an overall patient condition image. Then, AI technology can recreate a 3D mapping solution of a patient’s body.
In terms of data, interesting research perspectives are emerging. For instance, we observed the emergence of a stream of research on patient data management and protection related to AI applications [ 82 ].
For diagnostics, AI techniques can make a difference in rehabilitation therapy and surgery. Numerous robots have been designed to support and manage such tasks. Rehabilitation robots physically support and guide, for example, a patient’s limb during motor therapy [ 83 ]. For surgery, AI has a vast opportunity to transform surgical robotics through devices that can perform semi-automated surgical tasks with increasing efficiency. The final aim of this technology is to automate procedures to negate human error while maintaining a high level of accuracy and precision [ 84 ]. Finally, the -19 period has led to increased remote patient diagnostics through telemedicine that enables remote observation of patients and provides physicians and nurses with support tools [ 66 , 85 , 86 ].
This study aims to provide a bibliometric analysis of publications on AI in healthcare, focusing on accounting, business and management, decision sciences and health profession studies. Using the SLR method of Massaro et al. [ 11 ], we provide a reliable and replicable research protocol for future studies in this field. Additionally, we investigate the trend of scientific publications on the subject, unexplored information, future directions, and implications using the science mapping workflow. Our analysis provides interesting insights.
In terms of bibliometric variables, the four leading journals, Journal of Medical Systems , Studies in Health Technology and Informatics , IEEE Journal of Biomedical and Health Informatics , and Decision Support Systems , are optimal locations for the publication of scientific articles on this topic. These journals deal mainly with healthcare, medical information systems, and applications such as cloud computing, machine learning, and AI. Additionally, in terms of h-index, Bushko R.G. and Liu C. are the most productive and impactful authors in this research stream. Burke et al.’s [ 67 ] contribution is the most cited with an analysis of nurse rostering using new technologies such as AI. Finally, in terms of keywords, co-occurrence reveals some interesting insights. For instance, researchers have found that AI has a role in diagnostic accuracy and helps in the analysis of health data by comparing thousands of medical records, experiencing automatic learning with clinical alerts, efficient management of health services and places of care, and the possibility of reconstructing patient history using these data.
Second, this paper finds five cluster analyses in healthcare applications: health services management, predictive medicine, patient data, diagnostics, and finally, clinical decision-making. These technologies can also contribute to optimising logistics processes in health services and allowing a better allocation of resources.
Third, the authors analysing the research findings and the issues under discussion strongly support AI's role in decision support. These applications, however, are demonstrated by creating a direct link to data quality management and the technology awareness of health personnel [ 87 ].
The importance of data quality for the decision-making process
Several authors have analysed AI in the healthcare research stream, but in this case, the authors focus on other literature that includes business and decision-making processes. In this regard, the analysis of the search flow reveals a double view of the literature. On the one hand, some contributions belong to the positivist literature and embrace future applications and implications of technology for health service management, data analysis and diagnostics [ 6 , 80 , 88 ]. On the other hand, some investigations also aim to understand the darker sides of technology and its impact. For example, as Carter [ 89 ] states, the impact of AI is multi-sectoral; its development, however, calls for action to protect personal data. Similarly, Davenport and Kalakota [ 77 ] focus on the ethical implications of using AI in healthcare. According to the authors, intelligent machines raise issues of accountability, transparency, and permission, especially in automated communication with patients. Our analysis does not indicate a marked strand of the literature; therefore, we argue that the discussion of elements such as the transparency of technology for patients is essential for the development of AI applications.
A large part of our results shows that, at the application level, AI can be used to improve medical support for patients (Fig. 11 ) [ 64 , 82 ]. However, we believe that, as indicated by Kalis et al. [ 90 ] on the pages of Harvard Business Review, the management of costly back-office problems should also be addressed.
The potential of algorithms includes data analysis. There is an immense quantity of data accessible now, which carries the possibility of providing information about a wide variety of medical and healthcare activities [ 91 ]. With the advent of modern computational methods, computer learning and AI techniques, there are numerous possibilities [ 79 , 83 , 84 ]. For example, AI makes it easier to turn data into concrete and actionable observations to improve decision-making, deliver high-quality patient treatment, adapt to real-time emergencies, and save more lives on the clinical front. In addition, AI makes it easier to leverage capital to develop systems and facilities and reduce expenses at the organisational level [ 78 ]. Studying contributions to the topic, we noticed that data accuracy was included in the debate, indicating that a high standard of data will benefit decision-making practitioners [ 38 , 77 ]. AI techniques are an essential instrument for studying data and the extraction of medical insight, and they may assist medical researchers in their practices. Using computational tools, healthcare stakeholders may leverage the power of data not only to evaluate past data ( descriptive analytics ) but also to forecast potential outcomes ( predictive analytics ) and to define the best actions for the present scenario ( prescriptive analytics ) [ 78 ]. The current abundance of evidence makes it easier to provide a broad view of patient health; doctors should have access to the correct details at the right time and location to provide the proper treatment [ 92 ].
Will medical technology de-skill doctors?
Further reflection concerns the skills of doctors. Studies have shown that healthcare personnel are progressively being exposed to technology for different purposes, such as collecting patient records or diagnosis [ 71 ]. This is demonstrated by the keywords (Fig. 6 ) that focus on technology and the role of decision-making with new innovative tools. In addition, the discussion expands with Lu [ 93 ], which indicates that the excessive use of technology could hinder doctors’ skills and clinical procedures' expansion. Among the main issues arising from the literature is the possible de-skilling of healthcare staff due to reduced autonomy in decision-making concerning patients [ 94 ]. Therefore, the challenges and discussion we uncovered in Fig. 11 are expanded by also considering the ethical implications of technology and the role of skills.
Implications
Our analysis also has multiple theoretical and practical implications.
In terms of theoretical contribution, this paper extends the previous results of Connelly et al., dos Santos et al, Hao et al., Huang et al., Liao et al. and Tran et al. [ 2 , 19 , 20 , 21 , 22 , 24 ] in considering AI in terms of clinical decision-making and data management quality.
In terms of practical implications, this paper aims to create a fruitful discussion with healthcare professionals and administrative staff on how AI can be at their service to increase work quality. Furthermore, this investigation offers a broad comprehension of bibliometric variables of AI techniques in healthcare. It can contribute to advancing scientific research in this field.
Limitations
Like any other, our study has some limitations that could be addressed by more in-depth future studies. For example, using only one research database, such as Scopus, could be limiting. Further analysis could also investigate the PubMed, IEEE, and Web of Science databases individually and holistically, especially the health parts. Then, the use of search terms such as "Artificial Intelligence" OR "AI" AND "Healthcare" could be too general and exclude interesting studies. Moreover, although we analysed 288 peer-reviewed scientific papers, because the new research topic is new, the analysis of conference papers could return interesting results for future researchers. Additionally, as this is a young research area, the analysis will be subject to recurrent obsolescence as multiple new research investigations are published. Finally, although bibliometric analysis has limited the subjectivity of the analysis [ 15 ], the verification of recurring themes could lead to different results by indicating areas of significant interest not listed here.
Future research avenues
Concerning future research perspectives, researchers believe that an analysis of the overall amount that a healthcare organisation should pay for AI technologies could be helpful. If these technologies are essential for health services management and patient treatment, governments should invest and contribute to healthcare organisations' modernisation. New investment funds could be made available in the healthcare world, as in the European case with the Next Generation EU programme or national investment programmes [ 95 ]. Additionally, this should happen especially in the poorest countries around the world, where there is a lack of infrastructure and services related to health and medicine [ 96 ]. On the other hand, it might be interesting to evaluate additional profits generated by healthcare organisations with AI technologies compared to those that do not use such technologies.
Further analysis could also identify why some parts of the world have not conducted studies in this area. It would be helpful to carry out a comparative analysis between countries active in this research field and countries that are not currently involved. It would make it possible to identify variables affecting AI technologies' presence or absence in healthcare organisations. The results of collaboration between countries also present future researchers with the challenge of greater exchanges between researchers and professionals. Therefore, further research could investigate the difference in vision between professionals and academics.
In the accounting, business, and management research area, there is currently a lack of quantitative analysis of the costs and profits generated by healthcare organisations that use AI technologies. Therefore, research in this direction could further increase our understanding of the topic and the number of healthcare organisations that can access technologies based on AI. Finally, as suggested in the discussion section, more interdisciplinary studies are needed to strengthen AI links with data quality management and AI and ethics considerations in healthcare.
In pursuing the philosophy of Massaro et al.’s [ 11 ] methodological article, we have climbed on the shoulders of giants, hoping to provide a bird's-eye view of the AI literature in healthcare. We performed this study with a bibliometric analysis aimed at discovering authors, countries of publication and collaboration, and keywords and themes. We found a fast-growing, multi-disciplinary stream of research that is attracting an increasing number of authors.
The research, therefore, adopts a quantitative approach to the analysis of bibliometric variables and a qualitative approach to the study of recurring keywords, which has allowed us to demonstrate strands of literature that are not purely positive. There are currently some limitations that will affect future research potential, especially in ethics, data governance and the competencies of the health workforce.
Availability of data and materials
All the data are retrieved from public scientific platforms.
Tagliaferri SD, Angelova M, Zhao X, Owen PJ, Miller CT, Wilkin T, et al. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: three systematic reviews. NPJ Digit Med. 2020;3(1):1–16.
Article Google Scholar
Tran BX, Vu GT, Ha GH, Vuong Q-H, Ho M-T, Vuong T-T, et al. Global evolution of research in artificial intelligence in health and medicine: a bibliometric study. J Clin Med. 2019;8(3):360.
Article PubMed Central Google Scholar
Hamid S. The opportunities and risks of artificial intelligence in medicine and healthcare [Internet]. 2016 [cited 2020 May 29]. http://www.cuspe.org/wp-content/uploads/2016/09/Hamid_2016.pdf
Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8(2):020303.
Article PubMed PubMed Central Google Scholar
Yang X, Wang Y, Byrne R, Schneider G, Yang S. Concepts of artificial intelligence for computer-assisted drug discovery | chemical reviews. Chem Rev. 2019;119(18):10520–94.
Article CAS PubMed Google Scholar
Burton RJ, Albur M, Eberl M, Cuff SM. Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak. 2019;19(1):171.
Meskò B, Drobni Z, Bényei E, Gergely B, Gyorffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017;3:38.
Cho B-J, Choi YJ, Lee M-J, Kim JH, Son G-H, Park S-H, et al. Classification of cervical neoplasms on colposcopic photography using deep learning. Sci Rep. 2020;10(1):13652.
Article CAS PubMed PubMed Central Google Scholar
Doyle OM, Leavitt N, Rigg JA. Finding undiagnosed patients with hepatitis C infection: an application of artificial intelligence to patient claims data. Sci Rep. 2020;10(1):10521.
Shortliffe EH, Sepúlveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018;320(21):2199–200.
Article PubMed Google Scholar
Massaro M, Dumay J, Guthrie J. On the shoulders of giants: undertaking a structured literature review in accounting. Account Auditing Account J. 2016;29(5):767–801.
Junquera B, Mitre M. Value of bibliometric analysis for research policy: a case study of Spanish research into innovation and technology management. Scientometrics. 2007;71(3):443–54.
Casadesus-Masanell R, Ricart JE. How to design a winning business model. Harvard Business Review [Internet]. 2011 Jan 1 [cited 2020 Jan 8]. https://hbr.org/2011/01/how-to-design-a-winning-business-model
Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–75.
Zupic I, Čater T. Bibliometric methods in management and organization. Organ Res Methods. 2015;1(18):429–72.
Secinaro S, Calandra D. Halal food: structured literature review and research agenda. Br Food J. 2020. https://doi.org/10.1108/BFJ-03-2020-0234 .
Rialp A, Merigó JM, Cancino CA, Urbano D. Twenty-five years (1992–2016) of the international business review: a bibliometric overview. Int Bus Rev. 2019;28(6):101587.
Zhao L, Dai T, Qiao Z, Sun P, Hao J, Yang Y. Application of artificial intelligence to wastewater treatment: a bibliometric analysis and systematic review of technology, economy, management, and wastewater reuse. Process Saf Environ Prot. 2020;1(133):169–82.
Article CAS Google Scholar
Huang Y, Huang Q, Ali S, Zhai X, Bi X, Liu R. Rehabilitation using virtual reality technology: a bibliometric analysis, 1996–2015. Scientometrics. 2016;109(3):1547–59.
Hao T, Chen X, Li G, Yan J. A bibliometric analysis of text mining in medical research. Soft Comput. 2018;22(23):7875–92.
dos Santos BS, Steiner MTA, Fenerich AT, Lima RHP. Data mining and machine learning techniques applied to public health problems: a bibliometric analysis from 2009 to 2018. Comput Ind Eng. 2019;1(138):106120.
Liao H, Tang M, Luo L, Li C, Chiclana F, Zeng X-J. A bibliometric analysis and visualization of medical big data research. Sustainability. 2018;10(1):166.
Choudhury A, Renjilian E, Asan O. Use of machine learning in geriatric clinical care for chronic diseases: a systematic literature review. JAMIA Open. 2020;3(3):459–71.
Connelly TM, Malik Z, Sehgal R, Byrnes G, Coffey JC, Peirce C. The 100 most influential manuscripts in robotic surgery: a bibliometric analysis. J Robot Surg. 2020;14(1):155–65.
Guo Y, Hao Z, Zhao S, Gong J, Yang F. Artificial intelligence in health care: bibliometric analysis. J Med Internet Res. 2020;22(7):e18228.
Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inform. 2020;8(7):e18599.
Forliano C, De Bernardi P, Yahiaoui D. Entrepreneurial universities: a bibliometric analysis within the business and management domains. Technol Forecast Soc Change. 2021;1(165):120522.
Secundo G, Del Vecchio P, Mele G. Social media for entrepreneurship: myth or reality? A structured literature review and a future research agenda. Int J Entrep Behav Res. 2020;27(1):149–77.
Dal Mas F, Massaro M, Lombardi R, Garlatti A. From output to outcome measures in the public sector: a structured literature review. Int J Organ Anal. 2019;27(5):1631–56.
Google Scholar
Baima G, Forliano C, Santoro G, Vrontis D. Intellectual capital and business model: a systematic literature review to explore their linkages. J Intellect Cap. 2020. https://doi.org/10.1108/JIC-02-2020-0055 .
Dumay J, Guthrie J, Puntillo P. IC and public sector: a structured literature review. J Intellect Cap. 2015;16(2):267–84.
Dal Mas F, Garcia-Perez A, Sousa MJ, Lopes da Costa R, Cobianchi L. Knowledge translation in the healthcare sector. A structured literature review. Electron J Knowl Manag. 2020;18(3):198–211.
Mas FD, Massaro M, Lombardi R, Biancuzzi H. La performance nel settore pubblico tra misure di out-put e di outcome. Una revisione strutturata della letteratura ejvcbp. 2020;1(3):16–29.
Dumay J, Cai L. A review and critique of content analysis as a methodology for inquiring into IC disclosure. J Intellect Cap. 2014;15(2):264–90.
Haleem A, Javaid M, Khan IH. Current status and applications of Artificial Intelligence (AI) in medical field: an overview. Curr Med Res Pract. 2019;9(6):231–7.
Paul J, Criado AR. The art of writing literature review: what do we know and what do we need to know? Int Bus Rev. 2020;29(4):101717.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Biancone PP, Secinaro S, Brescia V, Calandra D. Data quality methods and applications in health care system: a systematic literature review. Int J Bus Manag. 2019;14(4):p35.
Secinaro S, Brescia V, Calandra D, Verardi GP, Bert F. The use of micafungin in neonates and children: a systematic review. ejvcbp. 2020;1(1):100–14.
Bert F, Gualano MR, Biancone P, Brescia V, Camussi E, Martorana M, et al. HIV screening in pregnant women: a systematic review of cost-effectiveness studies. Int J Health Plann Manag. 2018;33(1):31–50.
Levy Y, Ellis TJ. A systems approach to conduct an effective literature review in support of information systems research. Inf Sci Int J Emerg Transdiscipl. 2006;9:181–212.
Chen G, Xiao L. Selecting publication keywords for domain analysis in bibliometrics: a comparison of three methods. J Informet. 2016;10(1):212–23.
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2007;22(2):338–42.
Article PubMed CAS Google Scholar
Sicilia M-A, Garcìa-Barriocanal E, Sànchez-Alonso S. Community curation in open dataset repositories: insights from zenodo. Procedia Comput Sci. 2017;1(106):54–60.
Secinaro S, Calandra D, Secinaro A, Muthurangu V, Biancone P. Artificial Intelligence for healthcare with a business, management and accounting, decision sciences, and health professions focus [Internet]. Zenodo; 2021 [cited 2021 Mar 7]. https://zenodo.org/record/4587618#.YEScpl1KiWh .
Elango B, Rajendran D. Authorship trends and collaboration pattern in the marine sciences literature: a scientometric Study. Int J Inf Dissem Technol. 2012;1(2):166–9.
Jacoby WG. Electoral inquiry section Loess: a nonparametric, graphical tool for depicting relationships between variables q. In 2000.
Andrews JE. An author co-citation analysis of medical informatics. J Med Libr Assoc. 2003;91(1):47–56.
PubMed PubMed Central Google Scholar
White HD, Griffith BC. Author cocitation: a literature measure of intellectual structure. J Am Soc Inf Sci. 1981;32(3):163–71.
Santosh KC. AI-driven tools for coronavirus outbreak: need of active learning and cross-population train/test models on multitudinal/multimodal data. J Med Syst. 2020;44(5):93.
Shickel B, Tighe PJ, Bihorac A, Rashidi P. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J Biomed Health Inform. 2018;22(5):1589–604.
Baig MM, GholamHosseini H, Moqeem AA, Mirza F, Lindén M. A systematic review of wearable patient monitoring systems—current challenges and opportunities for clinical adoption. J Med Syst. 2017;41(7):115.
Kumar S, Kumar S. Collaboration in research productivity in oil seed research institutes of India. In: Proceedings of fourth international conference on webometrics, informetrics and scientometrics. p. 28–1; 2008.
Gatto A, Drago C. A taxonomy of energy resilience. Energy Policy. 2020;136:111007.
Levitt JM, Thelwall M. Alphabetization and the skewing of first authorship towards last names early in the alphabet. J Informet. 2013;7(3):575–82.
Saad G. Exploring the h-index at the author and journal levels using bibliometric data of productive consumer scholars and business-related journals respectively. Scientometrics. 2006;69(1):117–20.
Egghe L. Theory and practise of the g-index. Scientometrics. 2006;69(1):131–52.
Schreiber M. A modification of the h-index: the hm-index accounts for multi-authored manuscripts. J Informet. 2008;2(3):211–6.
Engqvist L, Frommen JG. The h-index and self-citations. Trends Ecol Evol. 2008;23(5):250–2.
London School of Economics. 3: key measures of academic influence [Internet]. Impact of social sciences. 2010 [cited 2021 Jan 13]. https://blogs.lse.ac.uk/impactofsocialsciences/the-handbook/chapter-3-key-measures-of-academic-influence/ .
Lotka A. The frequency distribution of scientific productivity. J Wash Acad Sci. 1926;16(12):317–24.
Khan G, Wood J. Information technology management domain: emerging themes and keyword analysis. Scientometrics. 2015;9:105.
Oxford University Press. Oxford English Dictionary [Internet]. 2020. https://www.oed.com/ .
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43.
Calandra D, Favareto M. Artificial Intelligence to fight COVID-19 outbreak impact: an overview. Eur J Soc Impact Circ Econ. 2020;1(3):84–104.
Bokolo Anthony Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132.
Burke EK, De Causmaecker P, Berghe GV, Van Landeghem H. The state of the art of nurse rostering. J Sched. 2004;7(6):441–99.
Ahmed MA, Alkhamis TM. Simulation optimization for an emergency department healthcare unit in Kuwait. Eur J Oper Res. 2009;198(3):936–42.
Forina M, Armanino C, Raggio V. Clustering with dendrograms on interpretation variables. Anal Chim Acta. 2002;454(1):13–9.
Wartena C, Brussee R. Topic detection by clustering keywords. In: 2008 19th international workshop on database and expert systems applications. 2008. p. 54–8.
Hussain AA, Bouachir O, Al-Turjman F, Aloqaily M. AI Techniques for COVID-19. IEEE Access. 2020;8:128776–95.
Agrawal A, Gans JS, Goldfarb A. Exploring the impact of artificial intelligence: prediction versus judgment. Inf Econ Policy. 2019;1(47):1–6.
Chakradhar S. Predictable response: finding optimal drugs and doses using artificial intelligence. Nat Med. 2017;23(11):1244–7.
Fleming N. How artificial intelligence is changing drug discovery. Nature. 2018;557(7707):S55–7.
Guo J, Li B. The application of medical artificial intelligence technology in rural areas of developing countries. Health Equity. 2018;2(1):174–81.
Aisyah M, Cockcroft S. A snapshot of data quality issues in Indonesian community health. Int J Netw Virtual Organ. 2014;14(3):280–97.
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8.
Mehta N, Pandit A, Shukla S. Transforming healthcare with big data analytics and artificial intelligence: a systematic mapping study. J Biomed Inform. 2019;1(100):103311.
Collins GS, Moons KGM. Reporting of artificial intelligence prediction models. Lancet. 2019;393(10181):1577–9.
Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: a Markov decision process approach. Artif Intell Med. 2013;57(1):9–19.
Redondo T, Sandoval AM. Text Analytics: the convergence of big data and artificial intelligence. Int J Interact Multimed Artif Intell. 2016;3. https://www.ijimai.org/journal/bibcite/reference/2540 .
Winter JS, Davidson E. Big data governance of personal health information and challenges to contextual integrity. Inf Soc. 2019;35(1):36–51.
Novak D, Riener R. Control strategies and artificial intelligence in rehabilitation robotics. AI Mag. 2015;36(4):23–33.
Tarassoli SP. Artificial intelligence, regenerative surgery, robotics? What is realistic for the future of surgery? Ann Med Surg (Lond). 2019;17(41):53–5.
Saha SK, Fernando B, Cuadros J, Xiao D, Kanagasingam Y. Automated quality assessment of colour fundus images for diabetic retinopathy screening in telemedicine. J Digit Imaging. 2018;31(6):869–78.
Gu D, Li T, Wang X, Yang X, Yu Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int J Med Inform. 2019;130:103947.
Madnick S, Wang R, Lee Y, Zhu H. Overview and framework for data and information quality research. J Data Inf Qual. 2009;1:1.
Chen X, Liu Z, Wei L, Yan J, Hao T, Ding R. A comparative quantitative study of utilizing artificial intelligence on electronic health records in the USA and China during 2008–2017. BMC Med Inform Decis Mak. 2018;18(5):117.
Carter D. How real is the impact of artificial intelligence? Bus Inf Surv. 2018;35(3):99–115.
Kalis B, Collier M, Fu R. 10 Promising AI Applications in Health Care. 2018;5.
Biancone P, Secinaro S, Brescia V, Calandra D. Management of open innovation in healthcare for cost accounting using EHR. J Open Innov Technol Market Complex. 2019;5(4):99.
Kayyali B, Knott D, Van Kuiken S. The ‘big data’ revolution in US healthcare [Internet]. McKinsey & Company. 2013 [cited 2020 Aug 14]. https://healthcare.mckinsey.com/big-data-revolution-us-healthcare/ .
Lu J. Will medical technology deskill doctors? Int Educ Stud. 2016;9(7):130–4.
Hoff T. Deskilling and adaptation among primary care physicians using two work innovations. Health Care Manag Rev. 2011;36(4):338–48.
Picek O. Spillover effects from next generation EU. Intereconomics. 2020;55(5):325–31.
Sousa MJ, Dal Mas F, Pesqueira A, Lemos C, Verde JM, Cobianchi L. The potential of AI in health higher education to increase the students’ learning outcomes. TEM J. 2021. ( In press ).
Download references
Acknowledgements
The authors are grateful to the Editor-in-Chief for the suggestions and all the reviewers who spend a part of their time ensuring constructive feedback to our research article.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Management, University of Turin, Turin, Italy
Silvana Secinaro, Davide Calandra & Paolo Biancone
Ospedale Pediatrico Bambino Gesù, Rome, Italy
Aurelio Secinaro
Institute of Child Health, University College London, London, UK
Vivek Muthurangu
You can also search for this author in PubMed Google Scholar
Contributions
SS and PB, Supervision; Validation, writing, AS and VM; Formal analysis, DC and AS; Methodology, DC; Writing; DC, SS and AS; conceptualization, VM, PB; validation, VM, PB. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Davide Calandra .
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Secinaro, S., Calandra, D., Secinaro, A. et al. The role of artificial intelligence in healthcare: a structured literature review. BMC Med Inform Decis Mak 21 , 125 (2021). https://doi.org/10.1186/s12911-021-01488-9
Download citation
Received : 24 December 2020
Accepted : 01 April 2021
Published : 10 April 2021
DOI : https://doi.org/10.1186/s12911-021-01488-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Patient data
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
- Health Care Services
- Public Health
- Delivery of Health Care
THE ROLE OF ARTIFICIAL INTELLIGENCE IN HEALTHCARE: A SYSTEMATIC REVIEW OF APPLICATIONS AND CHALLENGES
- International Medical Science Research Journal 4(4):500-508
- 4(4):500-508
- CC BY-NC 4.0

- The Ohio State University
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Chukwuemeka Odumegwu Ojukwu University, Anambra, Nigeria
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Ayman Mohamed El-Ashry

- Osemeike Gloria Eyieyien
- Courage Idemudia
- Patience Okpeke Paul
- Tochukwu Ignatius Ijomah
- Miss. Isha Anand Bhagat
- Miss. Komal Gajanan Wankhede
- Mr. Navoday Atul Kopawar
- Prof. Dipali A. Sananse
- Oloruntosin Tolulope Joel
- Vincent Ugochukwu Oguanobi

- U. Rajendra Acharya

- BMC Med Ethics

- A Bakhrebah

- Int J Environ Res Publ Health

- Rongrong Li

- INT J MED INFORM

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Author Biographies
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
The role of ai in hospitals and clinics: transforming healthcare in the 21st century.

1. Introduction
2. ai in clinical decision-making, 2.1. ai algorithms for diagnosis and prognosis.
- Machine learning (ML): ML algorithms learn from data to make predictions or decisions without being explicitly programmed for the task [ 18 ]. In healthcare, supervised learning algorithms have been instrumental in developing predictive models for patient outcomes based on historical data [ 19 ]. Unsupervised learning, on the other hand, is used to identify patterns or clusters within data, useful in discovering novel disease subtypes [ 20 ]. Reinforcement learning, where algorithms learn to make sequences of decisions by trial and error, has potential in personalized treatment optimization [ 21 ].
- Deep learning (DL): A subset of ML, deep learning uses neural networks with multiple layers (hence “deep”) to analyze complex data structures. Convolutional Neural Networks (CNNs) are particularly effective in processing imaging data, making them invaluable for diagnosing diseases from medical images like X-rays or MRIs [ 22 ]. Some other advanced CNN architectures include Residual Network (ResNet), Inception, Visual Geometry Group (VGG), and Graph Convolutional Networks (GCNs), each with its own strengths and applications in image analysis, classification, and graph data processing [ 23 ]. Recurrent Neural Networks (RNNs), known for their ability to handle sequential data, are used for analyzing time-series data, such as physiological signals collected during patient monitoring, to predict health deteriorations or outcomes over time [ 24 ]. For instance, Long Short-Term Memory (LSTM) networks, a sophisticated variant of RNNs, have been extensively utilized in the detection of sleep apnea using polysomnography data [ 25 ]. Additionally, Transformer models, such as BERT (Bidirectional Encoder Representations from Transformers) and GPT (Generative Pre-trained Transformer), offer revolutionary approaches to processing natural language in clinical notes, enabling more accurate extraction of patient information and insights. Generative Adversarial Networks (GANs) [ 26 ] and conditional diffusion models [ 27 ] have emerged as a powerful tool for generating synthetic medical images for training without privacy concerns, while Graph Neural Networks (GNNs) are unlocking new possibilities in modeling complex biological and health-related networks, from predicting protein interactions to understanding disease pathways.
2.2. Case Studies of AI in Detecting Diseases
- Cancer detection: One of the most groundbreaking applications of AI is in the early detection of cancer. A notable case study involves the use of deep learning algorithms in the analysis of mammograms for breast cancer detection. Research has shown that AI can identify patterns in mammographic images that are indicative of cancerous growths, often with greater accuracy than traditional methods. A notable study published in the journal Nature reported the development of an AI model by Google Health [ 35 ]. This model was trained on a large dataset of mammograms and demonstrated the ability to detect breast cancer more accurately than human radiologists. The AI system showed a reduction in both false positives and false negatives, key factors in cancer diagnostics. This progress in AI technology is significant because early detection of breast cancer can dramatically improve prognosis and treatment outcomes.
- Diabetes management: AI’s role in managing and detecting diabetes, particularly through machine learning algorithms, is a significant area of improvement in healthcare. These algorithms can analyze patient data to predict the onset and progression of diabetes and its complications, as demonstrated in different studies. In one study, several supervised classification algorithms were applied to predict and classify eight diabetes complications, including metabolic syndrome, dyslipidemia, neuropathy, nephropathy, diabetic foot, hypertension, obesity, and retinopathy [ 36 ]. The dataset utilized in this study comprises 79 input attributes, including results of medical tests and demographic information collected from 884 patients. The performance of the models was evaluated using the accuracy and F1 score, reaching a maximum of 97.8% and 97.7%, respectively. Among different classifiers, random forest (RF), Adaboost, and XGBoost achieved the best performance. This high level of accuracy demonstrates the potential of machine learning in effectively predicting diabetes complications. Another study focused on evaluating the efficacy of machine learning algorithms in predicting complications and poor glycemic control in nonadherent type 2 diabetes patients [ 37 ]. This real-world study used data from 800 type 2 diabetes patients, of which 165 met the inclusion criteria. Different machine learning algorithms were used to develop prediction models, with the predictive performance assessed using the area under the curve. The highest performance scores for predicting various complications such as diabetic nephropathy, neuropathy, angiopathy, and eye disease were 90.2%, 85.9%, 88.9%, and 83.2%, showcasing the effectiveness of these models.
- Heart disease prediction: The prediction of heart disease using AI represents a significant advancement in cardiovascular healthcare. This application not only aims to predict the occurrence of heart disease but also attempts to determine its severity, a crucial factor in effective treatment and management. One innovative study in this area focused on a machine learning-based prediction model that performs both binary and multiple classifications of heart disease [ 38 ]. The model, known as Fuzzy-GBDT, integrates fuzzy logic with a gradient boosting decision tree to streamline data complexity and improve prediction accuracy. Additionally, to avoid overfitting, the model incorporates a bagging technique, enhancing its capability to classify the severity of heart disease. The evaluation results of this model show excellent accuracy and stability in predicting heart disease, demonstrating its potential as a valuable tool in healthcare. Another interesting study introduces a cutting-edge healthcare system that employs ensemble deep learning coupled with feature fusion approaches [ 39 ]. This system is designed to overcome the limitations of traditional machine learning models that struggle with high-dimensional datasets. It achieves this by integrating sensor data with electronic medical records, creating a more holistic dataset for heart disease prediction. The system uses the information gain technique to streamline this dataset, focusing on the most relevant features and thereby reducing computational complexity. A key aspect of this model is the application of conditional probability for precise feature weighting, enhancing the overall performance of the system. Impressively, this ensemble deep learning model achieved an accuracy of 98.5%, outperforming existing models and illustrating its efficacy in heart disease prediction.
- AI in neurological disorders: The integration of AI, particularly deep learning (DL), in neurology has opened new avenues for the diagnosis and management of neurological disorders. The recent literature reveals significant progress in employing AI for the early detection and more accurate diagnosis of various conditions, including AD. One area of notable advancement is the use of deep learning in neuroimaging studies. DL’s ability to process and learn from raw data through complex, nonlinear transformations makes it well suited for identifying the subtle and diffuse alterations characteristic of many neurological and psychiatric disorders. Research in this domain has shown that DL can be a powerful tool in the ongoing search for biomarkers of such conditions, offering potential breakthroughs in understanding and diagnosing brain-based disorders [ 40 ]. Furthering this progress, a comprehensive review of deep learning techniques in the prognosis of a range of neuropsychiatric and neurological disorders, such as stroke, Alzheimer’s, Parkinson’s, epilepsy, autism, migraine, cerebral palsy, and multiple sclerosis, has underscored deep learning’s versatility in addressing real-life challenges across various domains, including disease diagnosis [ 41 ]. In the specific case of Alzheimer’s Disease (AD), the most common cause of dementia, deep learning has shown promise in enhancing diagnosis accuracy. Utilizing Convolutional Neural Networks (CNNs), researchers have developed frameworks for detecting AD characteristics from Magnetic Resonance Imaging (MRI) data [ 42 ]. By considering different stages of dementia and creating high-resolution disease probability maps, these models provide intuitive visualizations of individual AD risk. This approach, especially when addressing class imbalance in datasets, has achieved high accuracy, surpassing existing methods. The adaptation of such models to extensive datasets like the Alzheimer’s Disease Neuroimaging Initiative (ADNI) further validates their effectiveness in predicting AD classes.
- Key insights: These case studies highlight AI’s significant role in advancing disease detection across multiple medical disciplines, offering accurate and timely diagnoses, often through non-invasive methods. However, as AI technology continues to evolve, there is a critical need for addressing challenges such as data privacy, algorithmic transparency, and ensuring equitable access to these technologies. Future developments should focus on creating more robust AI systems that can handle diverse datasets, thereby reducing potential biases in diagnosis. Additionally, integrating AI with traditional diagnostic methods and enhancing interdisciplinary collaboration among technologists, clinicians, and patients will be key to harnessing AI’s full potential in disease detection and management.
2.3. The Role of AI in Personalized Medicine
- Tailoring treatments to genetic profiles: One of the most significant applications of AI in personalized medicine is in the field of genomics. AI algorithms can analyze vast genomic datasets to identify mutations and variations that might influence an individual’s response to certain treatments. For example, in oncology, AI helps in identifying specific genetic markers that are susceptible to targeted cancer therapies. This approach increases the efficacy of the treatment and minimizes the risk of adverse reactions, ensuring a more effective and safer treatment plan for the patient. A prime example of this application is a study focusing on nonmuscle invasive urothelial carcinoma, a type of bladder cancer known for its high recurrence risk [ 43 ]. In this study, researchers employed a machine learning algorithm to analyze genomic data from patients at their initial presentation. They aimed to identify genes most predictive of recurrence within five years following transurethral resection of the bladder tumor. The study involved whole-genome profiling of 112 frozen nonmuscle invasive urothelial carcinoma specimens using Human WG-6 BeadChips. A genetic programming algorithm was then applied to evolve classifier mathematical models for outcome prediction. The process involved cross-validation-based resampling and assessing gene use frequencies to pinpoint the most prognostic genes. These genes were subsequently combined into rules within a voting algorithm to predict the likelihood of cancer recurrence. Of the genes analyzed, 21 were identified as predictive of recurrence. Further validation through the quantitative polymerase chain reaction was conducted on a subset of 100 patients. The results were promising: a five-gene combined rule using the voting algorithm showed 77% sensitivity and 85% specificity in predicting recurrence in the training set. Additionally, a three-gene rule was developed, offering 80% sensitivity and 90% specificity in the training set for recurrence prediction.
- Predictive analytics in drug development: AI also plays a crucial role in drug development, particularly in predicting how different patients will respond to a drug. By analyzing historical data from clinical trials and patient records, AI models can predict the effectiveness of drugs on various demographic groups [ 44 , 45 ]. This predictive power is invaluable in designing clinical trials and in developing drugs that are more effective for specific patient populations In recent years, AI has made remarkable strides in drug development. Exscientia introduced the first AI-designed drug molecule for clinical trials in early 2020 [ 46 ]. DeepMind’s AlphaFold then achieved a breakthrough in July 2021 by predicting structures for over 330,000 proteins, including the entire human genome. In 2022, Insilico Medicine started Phase I trials for an AI-discovered molecule, a process significantly faster and more cost-effective than traditional methods. By 2023, AbSci had innovated in creating antibodies using generative AI, and Insilico Medicine saw an AI-designed drug receive FDA Orphan Drug Designation, with Phase II trials planned shortly thereafter. These milestones mark a transformative era in AI-driven drug discovery. AI’s application extends to the identification of novel proteins or genes as potential disease targets, with systems capable of predicting the 3D structures of these targets using deep learning [ 47 ]. AI is also revolutionizing molecular simulations and the prediction of drug properties such as toxicity and bioactivity, enabling high-fidelity simulations that can be run entirely in silico [ 44 ]. Moreover, AI is shifting the paradigm of traditional drug discovery from screening large libraries of molecules to generating novel drug molecules from scratch [ 48 ]. This approach can enhance the efficiency of the drug discovery process and can lead to the development of novel therapies.
3. AI in Hospital Operations and Management
3.1. ai for hospital logistics and resource management.
- Inventory management: AI systems are being used to predictively manage inventory in hospitals [ 60 , 61 ]. By analyzing usage patterns, patient inflow, and other relevant data, AI can forecast the need for medical supplies, medications, and equipment. This predictive capability ensures that hospitals maintain optimal stock levels, reducing wastage and ensuring the availability of critical supplies when needed.
- Facility management: AI also contributes to the efficient management of hospital facilities. For example, AI-powered systems can control heating, ventilation, and air conditioning (HVAC) systems more efficiently, reducing energy costs while maintaining a comfortable environment for patients and staff [ 62 ]. Additionally, AI can help in the predictive maintenance of hospital equipment, identifying potential issues before they lead to breakdowns, thus minimizing downtime and repair costs [ 63 ].
- Resource allocation: One of the most substantial applications of AI in hospital management is in the optimization of resource allocation [ 64 ]. AI algorithms can analyze complex datasets, including patient admissions, staff availability, and operational capacities, to optimize the allocation of human and material resources. This includes scheduling surgeries and medical procedures in a manner that maximizes the utilization of operating rooms and medical staff, while minimizing patient wait times [ 65 ].
- Supply chain optimization: AI enhances supply chain operations in hospitals by analyzing trends and automating ordering processes [ 66 , 67 ]. It can anticipate supply chain disruptions and suggest alternative solutions, ensuring that the hospital’s operations are not affected by external supply chain challenges. In emergency situations or during health crises, AI systems play a crucial role in managing logistics and resources [ 68 ]. They can quickly analyze the situation, predict the resources required, and assist in the efficient distribution of these resources where they are needed most.
3.2. Automating Administrative Tasks with AI
- Patient data management: AI plays an important role in managing vast amounts of patient data [ 69 ]. AI systems can organize, categorize, and process patient records, appointments, and treatment histories with high efficiency and accuracy. These systems can also extract relevant information from unstructured data, such as doctor’s notes, making it easier for healthcare providers to access and analyze patient information. For example, a study utilized AI and natural language processing (NLP) to analyze electronic medical records (EMRs), focusing on uncoded consultation notes for disease prediction [ 70 ]. Techniques like bag of words and topic modeling were applied, along with a method to match notes with a medical ontology. This approach was particularly tested for colorectal cancer. The study found that the ontology-based method significantly enhanced predictive performance, with an AUC of 0.870, surpassing traditional benchmarks. This highlights AI’s potential in extracting useful information from EMR’s unstructured data, improving disease prediction accuracy.
- Billing and claims processing: AI algorithms can also be used to automate billing and insurance claims processing. They can quickly analyze and process claims data, identify errors or inconsistencies, and ensure that billing is accurate and compliant with relevant regulations [ 71 ]. This not only speeds up the reimbursement process but also reduces the likelihood of billing errors, leading to improved financial operations and patient satisfaction. For example, a study in the insurance sector utilized machine learning to improve loss reserve estimation accuracy, crucial for financial statements [ 72 ]. Moving away from traditional macro-level models, this approach used individual claims data, integrating details about policies, policyholders, and claims. The method addressed the challenge of right-censored variables by creating tailored datasets for training and evaluating the algorithms. Compared to the conventional chain ladder method, this AI-driven approach showed notable improvements in accuracy, evidenced by a real case study with a Dutch loan insurance portfolio.
- Scheduling appointments: AI-driven scheduling systems are revolutionizing the way appointments are managed in healthcare settings [ 73 ]. These systems can analyze patterns in appointment bookings and cancellations to optimize the scheduling of patients. By predicting peak times and adjusting appointments accordingly, AI helps in reducing wait times and improving patient flow. For example, a project aimed at reducing outpatient MRI no-shows effectively utilized AI predictive analytics [ 74 ]. In this quality improvement initiative, over 32,000 anonymized outpatient MRI appointment records were analyzed using machine learning techniques, specifically an XGBoost model, a decision tree-based ensemble algorithm. This approach achieved notable results; the model’s predictive accuracy was demonstrated by an ROC AUC of 0.746 and an optimized F1 score of 0.708. When implemented alongside a practical intervention of telephone call reminders for patients identified as high-risk for no-shows, the no-show rate decreased from 19.3% to 15.9% over six months. In another study, a data-driven approach was used to optimize appointment scheduling and sequencing, especially in environments with uncertain service durations and customer punctuality [ 75 ]. Leveraging a novel method based on infinite-server queues, the study developed scalable solutions suitable for complex systems with numerous jobs and servers. Tested using a comprehensive dataset from a cancer center’s infusion unit, this approach significantly improved operational efficiency. The results showed a consistent reduction in costs—combining waiting times and overtime—by 15% to 40%, demonstrating the effectiveness of AI-based strategies in optimizing appointment scheduling.
- Document management and processing: AI technologies are adept at automating the processing of various documents, including consent forms, admission forms, and medical reports [ 76 ]. By using natural language processing (NLP) and machine learning, AI can quickly parse through documents, extract relevant information, and categorize them appropriately. This automation reduces the administrative burden on staff and speeds up document processing.
- Automated communication and reminders: A notable application of AI in healthcare is the optimization of information extraction from electronic health records (EHRs), particularly from scanned documents. A study demonstrated this by successfully extracting sleep apnea indicators from scanned sleep study reports using a combination of image preprocessing techniques and natural language processing (NLP) [ 77 ]. By employing methods like gray-scaling and OCR with Tesseract, followed by analysis through advanced models like ClinicalBERT, the study achieved high accuracy rates (over 90%) in identifying key health metrics.
- Automated communication and reminders: AI-powered chatbots and virtual assistants are increasingly used for patient communication. They can handle routine inquiries, provide information about services, and send reminders for upcoming appointments or medication schedules. This not only enhances patient engagement but also frees up staff to focus on more critical tasks. An example of this application is seen in the ChronologyMD project [ 78 ], which utilized AI to improve eHealth communication programs. The project addressed major deficiencies in existing eHealth communication strategies, which often failed to fully engage audiences and sometimes even negatively impacted the delivery of crucial health information. By strategically employing AI, the ChronologyMD project succeeded in making health communication more engaging, relevant, and actionable. Additionally, it led to increased exposure to relevant messages, reduced the workload of healthcare staff, and improved the overall efficiency of the program while minimizing costs.
- Data security and compliance: AI systems contribute significantly to data security and compliance in healthcare [ 79 ]. They can monitor and analyze data access patterns to detect and prevent unauthorized access or breaches. Additionally, AI can ensure that administrative processes are compliant with healthcare regulations, such as HIPAA, thereby safeguarding patient privacy. Building on this, recent research has explored the role of AI in ensuring compliance with the General Data Protection Regulation (GDPR), crucial for data controllers [ 80 ]. This study aimed to bridge gaps in compliance checking through a two-pronged approach: firstly, by conceptualizing a framework for document-centric compliance checking in the data supply chain, and secondly, by developing methods to automate the compliance checking of privacy policies. The study tested a two-module system, where the first module uses natural language processing (NLP) to extract data practices from privacy policies, and the second module encodes GDPR rules to ensure the inclusion of all mandatory information. The results demonstrated that this text-to-text approach was more effective than local classifiers, capable of extracting both broad and specific information with a single model. The system’s effectiveness was validated on a dataset of 30 privacy policies, annotated by legal experts.
3.3. AI in Patient Flow and Scheduling Optimization
- Optimizing patient flow: AI algorithms are particularly adept at analyzing patterns in patient admissions, discharges, and transfers, enabling more efficient patient flow throughout the hospital [ 65 , 81 ]. By predicting high-demand periods, AI can assist in preemptively allocating resources such as beds, staff, and equipment to meet patient needs. For instance, AI systems can forecast daily or seasonal fluctuations in patient admissions, allowing hospitals to adjust staffing levels and bed availability accordingly [ 82 ]. This proactive approach reduces bottlenecks, minimizes wait times, and enhances the overall patient experience.
- Dynamic scheduling systems: AI-driven scheduling systems revolutionize the way appointments and procedures are organized. These systems can analyze multiple variables, including healthcare provider availability, patient preferences, and urgency of care, to create optimal schedules. By doing so, they reduce appointment no-shows and last-minute cancellations, maximizing the utilization of healthcare professionals’ time. Moreover, these AI systems can adapt in real time to changes, such as emergency cases, by rescheduling non-urgent appointments without significant disruptions [ 83 ]. In a study aimed at improving outpatient department efficiency and patient satisfaction, researchers developed an innovative appointment scheduling system based on a Markov decision process model, incorporating patient preferences to maximize satisfaction [ 84 ]. Adaptive dynamic programming algorithms were utilized to overcome the complexity of scheduling, dynamically adjusting to patient preferences and continuously improving appointment decisions. The system’s performance was evaluated through various experiments, which demonstrated optimal convergence behavior and accuracy.
- Reducing waiting times: One of the critical benefits of AI in patient flow is the reduction in waiting times in emergency departments and outpatient clinics. AI can predict patient inflow and identify potential delays, allowing hospital staff to take proactive measures to manage patient wait times effectively [ 85 , 86 ]. For emergency departments, this means better triage processes and quicker allocation of patients to the appropriate care. Utilizing machine learning algorithms, a recent study predicted patient waiting times before consultation and throughput time in an outpatient clinic, aiming to enhance patient satisfaction by providing more accurate wait time information [ 87 ]. The study employed random forest and XGBoost algorithms, analyzing input variables such as gender, day and time of visit, and consultation session. The study achieved high accuracy (86–93%) in predicting wait and throughput times in an outpatient clinic using machine learning models with novel input variables.
- Enhancing patient experience: AI systems can also improve the overall patient experience by providing accurate information about appointment times, wait periods, and treatment schedules [ 88 ]. This transparency helps in managing patient expectations and reduces anxiety associated with medical appointments and procedures. In a recent study, a machine learning model was developed to predict patient responses to the “Doctor Communications” domain of the Hospital Consumer Assessment of Healthcare Providers and Systems survey, using data from a tertiary care hospital (2016–2020) [ 89 ]. The random forest algorithm effectively predicted patient responses about doctors’ courtesy, explanation clarity, and attentiveness. The model achieved an AUC of 88% for these doctor communication survey questions.
- Integrating with telehealth: In the era of digital health, AI in scheduling extends beyond in-person appointments to include telehealth services. AI systems can effectively schedule and manage virtual consultations, ensuring that patients receive timely care without the need to physically visit the healthcare facility, which is particularly beneficial for routine follow-ups or during health crises like pandemics [ 90 ].
4. AI in Medical Imaging and Diagnostics
4.1. ai’s role in radiology and pathology, 4.2. enhancing accuracy and efficiency in diagnostic processes.
- Improving diagnostic accuracy: AI algorithms, particularly those based on deep learning, have demonstrated remarkable accuracy in diagnosing diseases from medical images and test results. These systems are trained on vast datasets, allowing them to recognize patterns and anomalies that might be imperceptible to the human eye. For example, in dermatology, AI systems trained on images of skin lesions have shown the ability to detect skin cancers, such as melanoma, with a level of precision comparable to that of experienced dermatologists [ 104 ].
- Reducing diagnostic errors: One of the key benefits of AI in diagnostics is its potential to reduce errors [ 105 ]. Misdiagnosis and missed diagnoses are significant concerns in medicine, often leading to delayed or inappropriate treatment. AI systems provide a level of consistency and attention to detail that is challenging for humans to maintain over long periods, thus reducing the likelihood of such errors.
- Speeding up diagnostic processes: AI significantly speeds up the diagnostic process. Analyzing medical images or test results, tasks that would take a healthcare professional considerable time, can be performed by AI in a fraction of the time. This rapid analysis is particularly beneficial in urgent care situations, where quick decision-making is critical. For instance, AI algorithms can quickly analyze CT scans of stroke patients to identify blockages or bleeding in the brain, enabling faster initiation of life-saving treatments [ 106 ].
- Automated reporting and documentation: AI not only automates reporting and documentation in diagnostic processes [ 107 ] but also enhances the quality of these processes. While AI systems generate preliminary reports from image analysis for radiologist review, streamlining workflow and reducing administrative burden, a recent study has furthered this efficiency by consolidating existing ML reporting guidelines [ 108 ]. This study, after an extensive review of 192 articles and expert feedback, created a comprehensive checklist encompassing 37 reporting items for prognostic and diagnostic ML studies. This effort in standardizing ML reporting is pivotal in improving the quality and reproducibility of ML modeling studies, complementing AI’s role in simplifying diagnostic reporting.
- Integrating diagnostic data: AI excels in integrating and analyzing data from various sources. In the case of complex diseases, AI can combine information from imaging, laboratory tests, and patient histories to provide a more comprehensive diagnostic insight [ 109 ]. This integration is particularly valuable in diagnosing complex conditions like autoimmune diseases or in cases where symptoms are ambiguous. As an example, a scoping review focused on AI techniques for fusing multimodal medical data, particularly EHR with medical imaging, to develop AI methods for various clinical applications [ 110 ]. The review analyzed 34 studies, observing a workflow of combining raw data using ML or DL algorithms for clinical outcome predictions. It found that multimodality fusion models generally outperform single-modality models, with early fusion being the most commonly used technique. Neurological disorders were the dominant category studied, and conventional ML models were more frequently used than DL models. This review provides insights into the current state of multimodal medical data fusion in healthcare research.
4.3. The Role of Hardware Acceleration in AI-Powered Diagnostics
- Graphics Processing Units (GPUs): Originally designed for computer graphics rendering, GPUs excel at parallel processing, making them ideal for handling the massive datasets and complex calculations involved in AI algorithms. In the medical image analysis domain, GPUs can be used to accelerate basic image processing operations such as filtering and interpolation. Additionally, GPUs can enhance the operation of different AI algorithms used in medical imaging tasks like image registration, image segmentation, image denoising, and image classification [ 113 ].
- Tensor Processing Units (TPUs): Custom-designed chips like TPUs, pioneered by companies like Google, are specifically optimized for high-performance deep learning inference, a key technique used in medical image analysis. TPUs offer significant speed advantages over CPUs for tasks like image recognition and classification. For example, researchers implemented a system for glaucoma diagnosis using both edge TPUs and embedded GPUs [ 114 ]. While both achieved fast image segmentation and classification for real-time diagnosis support, the study found that TPUs consumed significantly less energy compared to GPUs. This makes TPUs a more attractive option for battery-powered medical devices used in edge computing scenarios.
- Field-Programmable Gate Arrays (FPGAs): These versatile chips offer flexibility for hardware customization. Unlike pre-designed GPUs and TPUs, FPGAs can be programmed to perform specific AI algorithms, potentially leading to highly optimized solutions for certain diagnostic tasks. However, programming FPGAs requires specialized expertise. For instance, researchers have proposed a MobileNet accelerator designed specifically for FPGAs that focuses on minimizing on-chip memory usage and data transfer, making it ideal for low-power devices [ 115 ]. They achieve this by using two configurable modules for different convolution operations and a new cache usage method. Their implementation demonstrates real-time processing with low memory usage, making FPGAs a viable option for running efficient CNNs in auxiliary medical tasks on portable devices.
- Application-Specific Integrated Circuits (ASICs): When dealing with a well-defined AI algorithm in a specific diagnostic application, ASICs can be designed to offer the ultimate performance [ 116 ]. Engineered for a single task, ASICs provide unparalleled efficiency and processing speed for that specific function. However, the lack of flexibility limits their application to well-established and unchanging algorithms.
4.4. Examples of AI Systems Used in Imaging
- AI in MRI analysis: AI applications in MRI analysis are versatile, encompassing the detection of brain abnormalities, tumors, strokes, neurodegenerative diseases, musculoskeletal injuries, cardiac conditions, and liver and abdominal organ pathologies, as well as evaluating breast and prostate cancers, demonstrating its broad utility in diagnosing a wide range of medical conditions [ 122 , 123 ]. In addition, deep learning is now playing a key role in accelerating the MRI acquisition process [ 92 ]. An example of AI application in MRI is an AI system developed for detecting brain abnormalities [ 118 ]. This system uses a deep CNN to analyze MRI images and can identify conditions such as tumors, strokes, and neurodegenerative diseases. The AI not only detects these abnormalities but also helps in quantifying the volume of affected areas, which is vital for treatment planning and monitoring disease progression. Another example is the application of AI in the interpretation of breast cancer. CNNs are employed to extract features from MRI breast scans, and alongside classifiers, they effectively detect the presence of cancer, showcasing the potential of AI in enhancing diagnostic accuracy in breast cancer detection [ 124 ]. AI systems are increasingly used for the automated segmentation of images in radiology [ 125 ]. These systems can differentiate and label various anatomical structures in the images, such as organs and tissues, aiding radiologists in diagnosis and in planning surgeries or treatments. For example, a study introduced a 4D deep learning model, combining 3D convolution and LSTM, for the precise segmentation of hepatocellular carcinoma (HCC) lesions in dynamic contrast-enhanced MRI images [ 126 ]. Utilizing both spatial and temporal domain information from multi-phase images, the model significantly improved liver tumor segmentation performance, achieving superior metrics compared to existing models and offering a comparable performance to the state-of-the-art nnU-Net model with reduced prediction time. AI is also being adapted for pediatric imaging, addressing the unique challenges presented by the varying sizes and developmental stages of pediatric patients [ 127 ]. AI systems in this domain are tailored to recognize and interpret patterns specific to children, aiding in the diagnosis of congenital and developmental conditions. For instance, in pediatric imaging for focal epilepsy, a deep CNN model was introduced, excelling in tract classification and identifying critical white matter pathways with 98% accuracy [ 128 ]. This model effectively predicted surgical outcomes and postoperative language changes, showcasing its potential to enhance preoperative evaluations and improve surgical precision in children.
- AI for CT scan interpretation: AI applications in CT scan interpretation span detecting lung nodules, identifying fractures and hemorrhages, assessing stroke severity, and characterizing tumor progression. One innovative AI application in CT imaging is in the rapid identification of pulmonary embolisms [ 119 ]. The AI system processes CT pulmonary angiograms to detect blood clots in the lungs with high accuracy, often faster than traditional methods. This speed is critical in emergency situations, where timely intervention can be life-saving. As another example, Google’s AI, in collaboration with researchers from Northwestern University, NYU-Langone Medical Center, and Stanford Medicine, has developed a CT scan model that diagnoses lung cancer with accuracy equal to or surpassing six radiologists [ 129 ]. This model analyzes 3D volumetric scans to predict malignancy and detect subtle lung nodules, viewing the lungs as a single 3D object and comparing scans over time to track lesion growth. Tested on over 45,800 de-identified chest CT screenings, it detected 5% more cancer cases and reduced false positives by over 11% compared to traditional radiologist evaluations, demonstrating significant potential for enhancing lung cancer diagnosis.
- AI in X-ray analysis: AI is revolutionizing X-ray analysis across various medical fields. Take mammography, for instance, AI is transforming breast cancer screening by enhancing image analysis for tumor detection, improving accuracy in identifying benign and malignant lesions, and reducing false positives and negatives, thereby streamlining the diagnostic process for early and effective treatment [ 130 ]. These systems analyze mammograms to identify signs of cancerous lesions, with some AI models demonstrating the ability to detect cancers that were initially missed by radiologists. By serving as a second reviewer, these AI systems enhance the accuracy of breast cancer screening. A recent study demonstrated that cmAssist™, an AI-based CAD algorithm based on multiple custom deep learning-based networks, significantly enhanced radiologists’ sensitivity in breast cancer detection [ 120 ]. Analyzing 122 mammograms with a blend of false negatives and BIRADS 1 and 2 ratings, radiologists showed a notable improvement in cancer detection rates (CDRs) by an average of 27% when using cmAssist, with a minimal increase in false positives. This marked improvement underscores the potential of AI-CAD software in improving accuracy and sensitivity in breast cancer screening.
- AI in ultrasound: AI is significantly impacting various applications of ultrasound. In cardiac imaging, for example, AI systems are used to analyze images from echocardiography scans to assess cardiovascular function [ 131 ]. They can measure parameters such as the ejection fraction, which indicates how well the heart is pumping blood, and detect structural abnormalities of the heart. This information is crucial in diagnosing and managing heart diseases. For example, a study evaluating a novel AI for automated left ventricular ejection time calculation in echocardiography showed high accuracy, closely correlating with cardiac MRI results [ 121 ]. The AI, which demonstrated lower bias and greater reliability especially in challenging cases, outperformed conventional methods. This algorithm is based on a patented CNN, though specific details of its architecture and training process remain proprietary. This underscores the algorithm’s potential in reducing user-dependent variability and enhancing the clinical utility of echocardiography.
5. AI in Patient Care and Monitoring
5.1. ai-powered wearable devices for continuous monitoring, 5.2. virtual nursing assistants, 5.3. ai in telemedicine and remote patient engagement, 6. methodologies for assessing ai healthcare solutions, 6.1. validation.
- Algorithm validation: The successful integration of AI algorithms into healthcare hinges on their accuracy, reliability, and performance. This necessitates comprehensive testing using diverse datasets [ 150 ]. A critical challenge in this process is overfitting, where the algorithm performs well on the training data but fails to generalize to unseen data. To address this, techniques like cross-validation are employed [ 151 ]. Cross-validation involves splitting the training data into multiple folds and iteratively training the algorithm on a subset of folds while using the remaining folds for validation. This process helps assess how well the algorithm generalizes to new data and prevents overfitting. Beyond generalizability, AI in healthcare should be adaptable for personalized use. This means the algorithms should continuously learn from individual patient data to enable tailored treatment approaches. Rigorous assessment helps identify strengths, weaknesses, and areas for improvement, ultimately enhancing the reliability of AI-based healthcare solutions. Furthermore, validation on different patient groups is essential to address potential biases in the training data. Biases can lead to unfair and ineffective outcomes for certain demographics. By ensuring the algorithms perform consistently across diverse populations, we can ensure fairness and effectiveness for all.
- Clinical validation: Clinical validation plays a crucial role in assessing the efficacy and safety of AI interventions [ 152 ]. Rigorous clinical trials and studies should be conducted to compare AI-based interventions with standard treatments or existing practices. These evaluations can encompass a range of study designs, including randomized controlled trials (RCTs), observational studies, or real-world evidence analyses. Through these studies, researchers can determine the effectiveness of AI technologies in improving patient outcomes and clinical decision-making. Furthermore, defining appropriate outcome measures is essential for assessing the impact of AI interventions on patient outcomes. Outcome measures such as mortality rates, disease progression, quality of life, and healthcare costs can be used to evaluate the effectiveness of AI technologies in improving healthcare delivery.
6.2. Interpretability and Usability
- Active stakeholder involvement: Throughout the development process, actively involving clinicians, patients, and other stakeholders provides valuable insights into their needs and expectations. This collaborative approach fosters a sense of ownership in the solution, leading to higher engagement.
- Iterative development and feedback loops: Developing AI solutions is an iterative process. By incorporating user feedback throughout development cycles, researchers can refine the AI tool to better address user needs. This ongoing feedback loop not only improves usability but also strengthens user confidence and engagement.
- User-friendly interfaces and clear visualizations: Designing clear and user-friendly interfaces is essential for user engagement. This includes presenting AI outputs in a way that is easy to understand and interpret, even for users with limited technical expertise. Additionally, providing clear visualizations of the AI’s reasoning can further enhance user trust and engagement.
6.3. Scalability and Continuous Improvement
- Post-market surveillance: Closely monitoring the performance of AI solutions after deployment in real-world settings to identify any unforeseen issues or areas for improvement [ 158 ].
- Performance monitoring: Continuously tracking the effectiveness of the AI tool in achieving its intended outcomes [ 159 ]. These data can be used to identify areas where the AI can be further optimized.
- Updating algorithms based on new data and insights: AI algorithms are not static. As new data become available, or as researchers gain a deeper understanding of the underlying problem, the algorithms can be updated to improve their performance and accuracy.
7. Ethical Considerations and Challenges
7.1. ethical implications of ai in healthcare.
- Privacy concerns: One of the foremost ethical concerns in AI healthcare is the privacy of patient data. AI systems require access to large datasets of patient information, which raises questions about the security and confidentiality of sensitive health data [ 160 ]. Ensuring that patient data used for AI applications are anonymized and securely stored is paramount. There is also a need for transparent policies regarding who has access to these data and for what purposes.
- Informed consent: The issue of informed consent in AI healthcare is complex, necessitating clear communication with patients about the use of their data, especially with AI algorithms that may be challenging for non-experts to grasp. This includes detailing data sharing implications, potential benefits and risks associated with AI-driven healthcare, and the level of human oversight in AI decisions. More details on the use of informed consent forms for AI in medicine with a comprehensive guideline for emergency physicians can be found in [ 161 ].
- Bias and fairness: AI systems are only as unbiased as the data they are trained on. There is a risk that AI algorithms may perpetuate existing biases present in healthcare data, leading to unfair treatment outcomes for certain groups [ 162 ]. For example, if an AI system is trained predominantly on data from a specific demographic, its accuracy might be lower for patients outside of that demographic. Ensuring that AI systems are developed and trained on diverse datasets is crucial to mitigate these biases. Moreover, the continuous monitoring and auditing of AI systems for biased outcomes are necessary to uphold fairness in healthcare delivery.
- Transparency and accountability: Transparency in AI decision-making processes is a key ethical concern [ 163 ]. It is important for healthcare providers and patients to understand how AI systems make their recommendations. This transparency is essential for building trust in AI systems and for accountability [ 164 ]. In cases where AI-driven decisions impact patient care, it is crucial to have mechanisms in place to review and understand these decisions, particularly in the event of adverse outcomes. A recent study highlights the need for transparent and accountable AI systems in natural NLP to address the “black box” issue of deep learning models [ 165 ]. It introduces the Explaining and Visualizing CNNs for Text Information (EVCT) framework, which offers human-interpretable solutions for text classification with minimal information loss, aligning with recent demands for fairness and transparency in AI-driven decision support systems.
7.2. Challenges in Integrating AI
- Data security concerns: As healthcare AI systems require access to large volumes of sensitive patient data, ensuring the security of these data is paramount [ 166 ]. The risk of data breaches and cyberattacks poses a significant concern. These security breaches can lead to the exposure of confidential patient information, resulting in privacy violations and potentially harming the trust between patients and healthcare providers. Implementing robust cybersecurity measures, including encryption, secure data storage solutions, and regular security audits, is crucial to protect patient data [ 167 ]. Additionally, educating healthcare staff about data security best practices is essential in safeguarding against breaches.
- Interoperability between systems: Another major challenge in integrating AI into healthcare is the issue of interoperability—the ability of different healthcare IT systems and software applications to communicate, exchange data, and use the information that has been exchanged [ 168 ]. Many healthcare systems use a variety of electronic health record (EHR) systems and other digital tools that may not be compatible with one another or with new AI technologies. This lack of interoperability can hinder the seamless exchange of patient data, reducing the effectiveness of AI tools. Developing standardized data formats and communication protocols, as well as encouraging the adoption of interoperable systems, is vital to overcome this challenge [ 169 ].
- Integration with existing clinical workflows: Integrating AI into existing clinical workflows can be challenging. Healthcare professionals may need to adjust their workflows to accommodate AI tools, which can be a time-consuming and complex process. Ensuring that AI systems are user-friendly and align with current clinical practices is essential to facilitate their adoption. Training and support for healthcare professionals in using these AI systems are also crucial for successful integration. For example, in a recent study, a three-tiered integration approach of AI-based image analysis into radiology workflows is outlined, focusing on enhancing automation and incorporating radiologist feedback for continuous AI improvement [ 170 ]. This approach entails initially visualizing AI outcomes without generating new patient records. It allows for the storage of AI-generated results in institutional systems and equips radiologists with tools to refine AI inferences for periodic retraining. This methodology was exemplified in a case study on brain metastases detection, where radiologist input substantially decreased false positives via iterative retraining with an expanded dataset.
- Data quality and quantity: The effectiveness of AI systems depends heavily on the quality and quantity of the data they are trained on. Inconsistent, incomplete, or inaccurate data can lead to poor AI performance. Ensuring the collection of high-quality, comprehensive patient data is therefore a significant challenge in AI integration [ 171 ]. Standardizing data collection methods and ensuring thorough data curation processes are essential steps in addressing this issue.
7.3. Regulatory and Compliance Issues
8. the future of ai in healthcare, 8.1. personalized healthcare applications.
- Personalized medicine: One of the most promising trends in AI healthcare is the move towards more personalized medicine [ 177 ]. AI’s ability to analyze vast amounts of genetic, health data, and lifestyle information will enable the development of more precise and effective treatments tailored to individual patient profiles. This personalized approach can improve treatment outcomes and reduce side effects.
- AI-powered tools for health and sleep monitoring: Future research should explore the development and validation of AI-driven tools and algorithms for the diagnosis, monitoring, and management of health issues and sleep disorders [ 178 ]. This includes leveraging machine learning to analyze data from wearable devices such as sleep patterns, heart rate variability, and activity levels. These analyses can, for example, help detect abnormalities such as sleep apnea and personalize treatment recommendations based on individual sleep profiles.
- Longevity and aging: By harnessing the power of predictive analytics, AI can explore vast datasets to uncover biomarkers of aging and offer personalized strategies to slow or even reverse the aging process [ 179 ]. This includes leveraging AI for genomic interventions, where it could guide the editing of genes associated with aging mechanisms, enhancing cellular repair, resilience, and longevity. The potential of AI extends to the field of drug discovery and repurposing, where it can expedite the identification of compounds with anti-aging effects [ 180 ]. Moreover, AI’s integration into healthcare promises a paradigm shift towards preventive medicine, emphasizing early detection and intervention in age-related declines.
8.2. Enhanced Treatment Technologies
- AI in drug discovery and development: AI is poised to play a significant role in accelerating drug discovery and development [ 181 ]. By rapidly analyzing molecular and clinical data, AI has the potential to identify potential drug candidates much faster than traditional methods. This acceleration could significantly reduce the time and cost associated with bringing new drugs to market.
- Advanced robotics in surgery and rehabilitation: The use of AI-driven robotics in surgery and rehabilitation is expected to advance further [ 182 ]. Robotic systems, guided by AI algorithms, could potentially perform complex surgeries with high precision, reducing risks and improving patient outcomes. In rehabilitation, AI-powered exoskeletons and prosthetics are anticipated to offer greater mobility and independence to patients.
- AI hardware accelerators: As AI applications in healthcare grow, the demand for efficient processing capabilities rises. AI hardware accelerators like GPUs, TPUs, and FPGAs optimize AI model performance, enabling real-time medical data processing with minimal latency. Integrating these accelerators into medical devices promises faster diagnosis, treatment planning, and analysis, thereby enhancing patient care outcomes. Developing dedicated AI hardware accelerators tailored to healthcare needs is a promising future direction for improving the efficiency and accessibility of AI-driven healthcare solutions.
- AI-enhanced medical imaging: Future developments in AI are likely to produce even more advanced medical imaging techniques [ 183 ]. These advancements could provide clearer, more detailed images and enable the earlier detection of diseases, potentially even identifying health risks before symptoms appear.
- Integrating AI with IoT and wearables: The integration of AI with the Internet of Things (IoT) and wearable technology is an emerging trend [ 184 ]. This combination could lead to real-time health monitoring systems that not only track health data but also provide proactive recommendations and alerts. AI can also be integrated into existing wearable technologies to provide further information regarding health and performance [ 185 ].
8.3. Healthcare System Optimization
- Enhancing patient outcomes and system efficiency: The transformative potential of AI in healthcare can revolutionize patient care and system efficiency. Future AI applications aim to detect diseases earlier, customize treatments, and significantly personalize patient care, leading to improved recovery times and reduced mortality rates. AI’s role extends to optimizing healthcare resources, reducing costs, and improving care accessibility, especially for underserved communities [ 186 ]. Moreover, AI will support healthcare professionals by augmenting decision-making, promising equitable health improvements and a more efficient healthcare delivery system.
- Global health monitoring systems: The significance of AI in addressing pandemics and global health emergencies is increasingly recognized as crucial [ 187 ]. By integrating and analyzing diverse data streams, AI is adept at quickly detecting the emergence of disease outbreaks, projecting their spread, and guiding effective public health interventions. During the COVID-19 pandemic, AI-powered models were used to predict the disease’s trajectory, showcasing the potential of AI in navigating the complexities of pandemic management [ 188 ]. Moreover, AI’s capabilities extend to enhancing public health strategies, enabling the expedited development and dissemination of vaccines and therapeutic solutions in times of crisis.
8.4. Data Management
- Addressing data scarcity: The scarcity of labeled data in healthcare poses a significant challenge for AI development, especially in areas like rare disease research where data are inherently limited. A practical solution to this problem is the implementation of semi-supervised and weakly supervised learning techniques [ 189 ]. By utilizing a combination of a small set of labeled data and a larger volume of unlabeled data, these methods improve AI’s learning efficiency from minimal information, offering a viable strategy for advancing research and treatment in fields where comprehensive labeled datasets are scarce. However, for certain applications in healthcare, even obtaining a small amount of labeled data can be difficult. In such cases, emerging techniques in the field of machine learning offer intriguing possibilities. Few-shot learning: Few-shot learning requires only a small number of labeled examples for a new concept. This could be beneficial for situations where obtaining even a small amount of labeled data for a rare disease is possible. By learning from these few examples, the model could potentially generalize to similar cases [ 190 , 191 ]. Zero-shot learning (ZSL): In theory, ZSL could allow AI models to learn about new diseases or medical conditions even with no labeled data for those specific cases. ZSL leverages existing knowledge and relationships between concepts to make predictions for unseen categories. While ZSL is still under development, it holds promise for healthcare applications where data are extremely limited [ 192 ]. Meta-learning: This approach focuses on training models to “learn how to learn” efficiently. A meta-learning model could be trained on various healthcare-related tasks with limited datasets for each task. This acquired knowledge about learning itself could then be applied to new, unseen medical problems with minimal data, potentially improving performance [ 193 ].
- Ensuring model versatility: Achieving versatility in AI models is essential for their effective application across the diverse landscape of healthcare settings and patient demographics. Techniques such as domain adaptation and transfer learning stand out as effective solutions, enabling AI models trained on one dataset to adjust and perform accurately on another with little need for retraining [ 194 ]. This capability is particularly valuable in healthcare, where patient characteristics, disease profiles, and treatment responses can vary widely [ 195 ]. By fostering such adaptability, these techniques ensure that AI can be deployed more universally, enhancing its effectiveness and utility for a broad spectrum of patients.
8.5. Ethical Considerations and Trust Building
- Ensuring data privacy: Addressing data privacy concerns in healthcare has become increasingly crucial with the rise in AI applications. An exemplary solution to this challenge is federated learning, a novel AI model training approach that enables algorithms to learn from data stored on local servers across different healthcare institutions without the need for direct data sharing [ 196 ]. This method significantly enhances privacy and security and offers a strategic advantage in the healthcare industry where the sensitivity and confidentiality of patient data are of utmost importance.
- Stakeholder acceptance: Ensuring trust and acceptance among stakeholders is critical for the successful integration of AI into healthcare practices [ 197 ]. This encompasses not only patients and clinicians but also policymakers, regulatory bodies, healthcare administrators, and other relevant parties. Patients may express concerns regarding the reliability and accountability of AI-driven decision-making processes. Therefore, transparent communication about the role of AI in treatment plans and the potential benefits it offers is essential to foster patient acceptance. Similarly, clinicians may have reservations about entrusting AI algorithms with decision-making responsibilities, fearing loss of autonomy or professional judgment, as well as doubting the accuracy of AI decisions. Establishing comprehensive training programs and collaborative frameworks that empower clinicians to understand and validate AI tools effectively can mitigate these concerns. Furthermore, building trust extends to engaging stakeholders such as policymakers, regulatory bodies, and healthcare administrators. Transparency in AI development and deployment, coupled with clear communication about ethical, legal, and regulatory considerations, is crucial for gaining stakeholder trust. Establishing robust governance frameworks that address these concerns can enhance confidence in AI systems and ensure accountability.
- Building trust with Explainable AI: Explainable AI (XAI) aims to make AI decision-making processes transparent and understandable to humans, a crucial aspect for clinical applications [ 198 ]. By providing insights into how AI models arrive at their conclusions, XAI fosters trust among healthcare professionals and patients, ensuring that AI-supported decisions are well informed and ethically sound. This transparency is vital for integrating AI into sensitive healthcare decisions, where understanding the rationale behind AI recommendations can significantly impact patient care and outcomes.
9. Conclusions
Author contributions, data availability statement, conflicts of interest.
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in health and medicine. Nat. Med. 2022 , 28 , 31–38. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McCorduck, P.; Cfe, C. Machines Who Think: A Personal Inquiry into the History and Prospects of Artificial Intelligence ; CRC Press: Boca Raton, FL, USA, 2004. [ Google Scholar ]
- Alpaydin, E. Introduction to Machine Learning ; MIT Press: Cambridge, MA, USA, 2020. [ Google Scholar ]
- Brynjolfsson, E.; McAfee, A. The Second Machine Age: Work, Progress, and Prosperity in a Time of Brilliant Technologies ; WW Norton & Company: New York, NY, USA, 2014. [ Google Scholar ]
- Russell, S.J.; Norvig, P. Artificial Intelligence a Modern Approach ; Pearson: London, UK, 2010. [ Google Scholar ]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015 , 521 , 436–444. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, F.; Preininger, A. AI in health: State of the art, challenges, and future directions. Yearb. Med. Inform. 2019 , 28 , 16–26. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- DuBois, K.N. Deep medicine: How artificial intelligence can make healthcare human again. Perspect. Sci. Christ. Faith 2019 , 71 , 199–201. [ Google Scholar ]
- Davenport, T.H. The AI Advantage: How to Put the Artificial Intelligence Revolution to Work ; MIT Press: Cambridge, MA, USA, 2018. [ Google Scholar ]
- Kaur, S.; Singla, J.; Nkenyereye, L.; Jha, S.; Prashar, D.; Joshi, G.P.; El-Sappagh, S.; Islam, M.S.; Islam, S.R. Medical diagnostic systems using artificial intelligence (ai) algorithms: Principles and perspectives. IEEE Access 2020 , 8 , 228049–228069. [ Google Scholar ] [ CrossRef ]
- Cortez, N. Digital Health: Scaling Healthcare to the World ; Springer: Cham, Switzerland, 2018; pp. 249–269. [ Google Scholar ]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J. Artificial intelligence in radiology. Nat. Rev. Cancer 2018 , 18 , 500–510. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kagiyama, N.; Shrestha, S.; Farjo, P.D.; Sengupta, P.P. Artificial intelligence: Practical primer for clinical research in cardiovascular disease. J. Am. Heart Assoc. 2019 , 8 , e012788. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bardhan, I.; Chen, H.; Karahanna, E. Connecting systems, data, and people: A multidisciplinary research roadmap for chronic disease management. MIS Q. 2020 , 44 , 185–200. [ Google Scholar ]
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges. Cancer Lett. 2020 , 471 , 61–71. [ Google Scholar ] [ CrossRef ]
- Binhowemel, S.; Alfakhri, M.; AlReshaid, K.; Alyani, A. Role of Artificial Intelligence in Diabetes Research Diagnosis and Prognosis: A Narrative Review. J. Health Inform. Dev. Ctries. 2023 , 17 , 1–12. [ Google Scholar ]
- Guan, Z.; Li, H.; Liu, R.; Cai, C.; Liu, Y.; Li, J.; Wang, X.; Huang, S.; Wu, L.; Liu, D. Artificial intelligence in diabetes management: Advancements, opportunities, and challenges. Cell Rep. Med. 2023 , 4 , 101213. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Waring, J.; Lindvall, C.; Umeton, R. Automated machine learning: Review of the state-of-the-art and opportunities for healthcare. Artif. Intell. Med. 2020 , 104 , 101822. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Eloranta, S.; Boman, M. Predictive models for clinical decision making: Deep dives in practical machine learning. J. Intern. Med. 2022 , 292 , 278–295. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nezamabadi, K.; Sardaripour, N.; Haghi, B.; Forouzanfar, M. Unsupervised ECG analysis: A review. IEEE Rev. Biomed. Eng. 2022 , 16 , 208–224. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Coronato, A.; Naeem, M.; De Pietro, G.; Paragliola, G. Reinforcement learning for intelligent healthcare applications: A survey. Artif. Intell. Med. 2020 , 109 , 101964. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sarvamangala, D.; Kulkarni, R.V. Convolutional neural networks in medical image understanding: A survey. Evol. Intell. 2022 , 15 , 1–22. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, Y.; Zhang, L.; Du, M.; Bo, J.; Liu, H.; Ren, L.; Li, X.; Deen, M.J. A comparative analysis of eleven neural networks architectures for small datasets of lung images of COVID-19 patients toward improved clinical decisions. Comput. Biol. Med. 2021 , 139 , 104887. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rim, B.; Sung, N.-J.; Min, S.; Hong, M. Deep learning in physiological signal data: A survey. Sensors 2020 , 20 , 969. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bahrami, M.; Forouzanfar, M. Sleep apnea detection from single-lead ECG: A comprehensive analysis of machine learning and deep learning algorithms. IEEE Trans. Instrum. Meas. 2022 , 71 , 4003011. [ Google Scholar ] [ CrossRef ]
- Yi, X.; Walia, E.; Babyn, P. Generative adversarial network in medical imaging: A review. Med. Image Anal. 2019 , 58 , 101552. [ Google Scholar ] [ CrossRef ]
- Hu, Y.; Kothapalli, S.V.; Gan, W.; Sukstanskii, A.L.; Wu, G.F.; Goyal, M.; Yablonskiy, D.A.; Kamilov, U.S. DiffGEPCI: 3D MRI Synthesis from mGRE Signals using 2.5 D Diffusion Model. arXiv 2023 , arXiv:2311.18073. [ Google Scholar ]
- Wang, J.; Liu, X. Medical image recognition and segmentation of pathological slices of gastric cancer based on Deeplab v3+ neural network. Comput. Methods Programs Biomed. 2021 , 207 , 106210. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nagabushanam, P.; Thomas George, S.; Radha, S. EEG signal classification using LSTM and improved neural network algorithms. Soft Comput. 2020 , 24 , 9981–10003. [ Google Scholar ] [ CrossRef ]
- Kawazoe, Y.; Shibata, D.; Shinohara, E.; Aramaki, E.; Ohe, K. A clinical specific BERT developed using a huge Japanese clinical text corpus. PLoS ONE 2021 , 16 , e0259763. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Torfi, A.; Fox, E.A.; Reddy, C.K. Differentially private synthetic medical data generation using convolutional GANs. Inf. Sci. 2022 , 586 , 485–500. [ Google Scholar ] [ CrossRef ]
- Lin, X.; Quan, Z.; Wang, Z.-J.; Ma, T.; Zeng, X. KGNN: Knowledge Graph Neural Network for Drug-Drug Interaction Prediction ; IJCAI: Pasadena, CA, USA, 2020; pp. 2739–2745. [ Google Scholar ]
- Zhou, B.; Yang, G.; Shi, Z.; Ma, S. Natural language processing for smart healthcare. IEEE Rev. Biomed. Eng. 2022 , 17 , 4–18. [ Google Scholar ] [ CrossRef ]
- Yang, X.; Chen, A.; PourNejatian, N.; Shin, H.C.; Smith, K.E.; Parisien, C.; Compas, C.; Martin, C.; Costa, A.B.; Flores, M.G. A large language model for electronic health records. NPJ Digit. Med. 2022 , 5 , 194. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McKinney, S.M.; Sieniek, M.; Godbole, V.; Godwin, J.; Antropova, N.; Ashrafian, H.; Back, T.; Chesus, M.; Corrado, G.S.; Darzi, A. International evaluation of an AI system for breast cancer screening. Nature 2020 , 577 , 89–94. [ Google Scholar ] [ CrossRef ]
- Jian, Y.; Pasquier, M.; Sagahyroon, A.; Aloul, F. A machine learning approach to predicting diabetes complications. Healthcare 2021 , 9 , 1712. [ Google Scholar ] [ CrossRef ]
- Fan, Y.; Long, E.; Cai, L.; Cao, Q.; Wu, X.; Tong, R. Machine learning approaches to predict risks of diabetic complications and poor glycemic control in nonadherent type 2 diabetes. Front. Pharmacol. 2021 , 12 , 665951. [ Google Scholar ] [ CrossRef ]
- Yuan, X.; Chen, J.; Zhang, K.; Wu, Y.; Yang, T. A stable AI-based binary and multiple class heart disease prediction model for IoMT. IEEE Trans. Ind. Inform. 2021 , 18 , 2032–2040. [ Google Scholar ] [ CrossRef ]
- Ali, F.; El-Sappagh, S.; Islam, S.R.; Kwak, D.; Ali, A.; Imran, M.; Kwak, K.-S. A smart healthcare monitoring system for heart disease prediction based on ensemble deep learning and feature fusion. Inf. Fusion 2020 , 63 , 208–222. [ Google Scholar ] [ CrossRef ]
- Vieira, S.; Pinaya, W.H.; Mechelli, A. Using deep learning to investigate the neuroimaging correlates of psychiatric and neurological disorders: Methods and applications. Neurosci. Biobehav. Rev. 2017 , 74 , 58–75. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gautam, R.; Sharma, M. Prevalence and diagnosis of neurological disorders using different deep learning techniques: A meta-analysis. J. Med. Syst. 2020 , 44 , 49. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Murugan, S.; Venkatesan, C.; Sumithra, M.; Gao, X.-Z.; Elakkiya, B.; Akila, M.; Manoharan, S. DEMNET: A deep learning model for early diagnosis of Alzheimer diseases and dementia from MR images. IEEE Access 2021 , 9 , 90319–90329. [ Google Scholar ] [ CrossRef ]
- Bartsch, G., Jr.; Mitra, A.P.; Mitra, S.A.; Almal, A.A.; Steven, K.E.; Skinner, D.G.; Fry, D.W.; Lenehan, P.F.; Worzel, W.P.; Cote, R.J. Use of artificial intelligence and machine learning algorithms with gene expression profiling to predict recurrent nonmuscle invasive urothelial carcinoma of the bladder. J. Urol. 2016 , 195 , 493–498. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Paul, D.; Sanap, G.; Shenoy, S.; Kalyane, D.; Kalia, K.; Tekade, R.K. Artificial intelligence in drug discovery and development. Drug Discov. Today 2021 , 26 , 80. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gupta, R.; Srivastava, D.; Sahu, M.; Tiwari, S.; Ambasta, R.K.; Kumar, P. Artificial intelligence to deep learning: Machine intelligence approach for drug discovery. Mol. Divers. 2021 , 25 , 1315–1360. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hasselgren, C.; Oprea, T.I. Artificial Intelligence for Drug Discovery: Are We There Yet? Annu. Rev. Pharmacol. Toxicol. 2024 , 64 , 527–550. [ Google Scholar ] [ CrossRef ]
- Senior, A.W.; Evans, R.; Jumper, J.; Kirkpatrick, J.; Sifre, L.; Green, T.; Qin, C.; Žídek, A.; Nelson, A.W.; Bridgland, A. Improved protein structure prediction using potentials from deep learning. Nature 2020 , 577 , 706–710. [ Google Scholar ] [ CrossRef ]
- Sadybekov, A.V.; Katritch, V. Computational approaches streamlining drug discovery. Nature 2023 , 616 , 673–685. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bica, I.; Alaa, A.M.; Lambert, C.; Van Der Schaar, M. From real-world patient data to individualized treatment effects using machine learning: Current and future methods to address underlying challenges. Clin. Pharmacol. Ther. 2021 , 109 , 87–100. [ Google Scholar ] [ CrossRef ]
- Vettoretti, M.; Cappon, G.; Facchinetti, A.; Sparacino, G. Advanced diabetes management using artificial intelligence and continuous glucose monitoring sensors. Sensors 2020 , 20 , 3870. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Low, D.M.; Bentley, K.H.; Ghosh, S.S. Automated assessment of psychiatric disorders using speech: A systematic review. Laryngoscope Investig. Otolaryngol. 2020 , 5 , 96–116. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Graham, S.; Depp, C.; Lee, E.E.; Nebeker, C.; Tu, X.; Kim, H.-C.; Jeste, D.V. Artificial intelligence for mental health and mental illnesses: An overview. Curr. Psychiatry Rep. 2019 , 21 , 116. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nasrullah, S.; Jalali, A. Detection of Types of Mental Illness through the Social Network Using Ensembled Deep Learning Model. Comput. Intell. Neurosci. 2022 , 2022 , 9404242. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guntuku, S.C.; Yaden, D.B.; Kern, M.L.; Ungar, L.H.; Eichstaedt, J.C. Detecting depression and mental illness on social media: An integrative review. Curr. Opin. Behav. Sci. 2017 , 18 , 43–49. [ Google Scholar ] [ CrossRef ]
- Czerwinski, M.; Hernandez, J.; McDuff, D. Building an AI That Feels: AI systems with emotional intelligence could learn faster and be more helpful. IEEE Spectr. 2021 , 58 , 32–38. [ Google Scholar ] [ CrossRef ]
- Torab-Miandoab, A.; Samad-Soltani, T.; Jodati, A.; Rezaei-Hachesu, P. Interoperability of heterogeneous health information systems: A systematic literature review. BMC Med. Inform. Decis. Mak. 2023 , 23 , 18. [ Google Scholar ] [ CrossRef ]
- Díaz-Rodríguez, N.; Del Ser, J.; Coeckelbergh, M.; de Prado, M.L.; Herrera-Viedma, E.; Herrera, F. Connecting the dots in trustworthy Artificial Intelligence: From AI principles, ethics, and key requirements to responsible AI systems and regulation. Inf. Fusion 2023 , 99 , 101896. [ Google Scholar ] [ CrossRef ]
- Gurevich, E.; El Hassan, B.; El Morr, C. In Equity within AI systems: What can health leaders expect? Healthc. Manag. Forum 2023 , 36 , 119–124. [ Google Scholar ] [ CrossRef ]
- Dwivedi, Y.K.; Hughes, L.; Ismagilova, E.; Aarts, G.; Coombs, C.; Crick, T.; Duan, Y.; Dwivedi, R.; Edwards, J.; Eirug, A. Artificial Intelligence (AI): Multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. Int. J. Inf. Manag. 2021 , 57 , 101994. [ Google Scholar ] [ CrossRef ]
- Jebbor, S.; Raddouane, C.; El Afia, A. A preliminary study for selecting the appropriate AI-based forecasting model for hospital assets demand under disasters. J. Humanit. Logist. Supply Chain Manag. 2022 , 12 , 1–29. [ Google Scholar ] [ CrossRef ]
- Galli, L.; Levato, T.; Schoen, F.; Tigli, L. Prescriptive analytics for inventory management in health care. J. Oper. Res. Soc. 2021 , 72 , 2211–2224. [ Google Scholar ] [ CrossRef ]
- Tien, P.W. Deep Learning-Powered Vision-Based Energy Management System for Next-Gen Built Environment ; University of Nottingham: Nottingham, UK, 2023. [ Google Scholar ]
- Zamzam, A.H.; Hasikin, K.; Wahab, A.K.A. Integrated failure analysis using machine learning predictive system for smart management of medical equipment maintenance. Eng. Appl. Artif. Intell. 2023 , 125 , 106715. [ Google Scholar ] [ CrossRef ]
- Mizan, T.; Taghipour, S. Medical resource allocation planning by integrating machine learning and optimization models. Artif. Intell. Med. 2022 , 134 , 102430. [ Google Scholar ] [ CrossRef ]
- Munavalli, J.R.; Boersma, H.J.; Rao, S.V.; Van Merode, G. Real-time capacity management and patient flow optimization in hospitals using AI methods. Artif. Intell. Data Min. Healthc. 2021 , 2021 , 55–69. [ Google Scholar ]
- Adhikari, A.; Joshi, R.; Basu, S. Collaboration and coordination strategies for a multi-level AI-enabled healthcare supply chain under disaster. Int. J. Prod. Res. 2023 , 2023 , 1–27. [ Google Scholar ] [ CrossRef ]
- Samadhiya, A.; Yadav, S.; Kumar, A.; Majumdar, A.; Luthra, S.; Garza-Reyes, J.A.; Upadhyay, A. The influence of artificial intelligence techniques on disruption management: Does supply chain dynamism matter? Technol. Soc. 2023 , 75 , 102394. [ Google Scholar ] [ CrossRef ]
- Sun, W.; Bocchini, P.; Davison, B.D. Applications of artificial intelligence for disaster management. Nat. Hazards 2020 , 103 , 2631–2689. [ Google Scholar ] [ CrossRef ]
- Tang, A.; Tam, R.; Cadrin-Chênevert, A.; Guest, W.; Chong, J.; Barfett, J.; Trump, D.; Noorbakhsh-Sabet, N.; Zand, R.; Zhang, Y. Health information management: Implications of artificial intelligence on healthcare data and information management. Yearb. Med. Inform. 2019 , 28 , 56–64. [ Google Scholar ]
- Hoogendoorn, M.; Szolovits, P.; Moons, L.M.; Numans, M.E. Utilizing uncoded consultation notes from electronic medical records for predictive modeling of colorectal cancer. Artif. Intell. Med. 2016 , 69 , 53–61. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Thesmar, D.; Sraer, D.; Pinheiro, L.; Dadson, N.; Veliche, R.; Greenberg, P. Combining the power of artificial intelligence with the richness of healthcare claims data: Opportunities and challenges. Pharmacoeconomics 2019 , 37 , 745–752. [ Google Scholar ] [ CrossRef ]
- Baudry, M.; Robert, C.Y. A machine learning approach for individual claims reserving in insurance. Appl. Stoch. Models Bus. Ind. 2019 , 35 , 1127–1155. [ Google Scholar ] [ CrossRef ]
- Samorani, M.; Blount, L.G. Machine learning and medical appointment scheduling: Creating and perpetuating inequalities in access to health care. Am. Public Health Assoc. 2020 , 110 , 440–441. [ Google Scholar ] [ CrossRef ]
- Chong, L.R.; Tsai, K.T.; Lee, L.L.; Foo, S.G.; Chang, P.C. Artificial intelligence predictive analytics in the management of outpatient MRI appointment no-shows. Am. J. Roentgenol. 2020 , 215 , 1155–1162. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mandelbaum, A.; Momčilović, P.; Trichakis, N.; Kadish, S.; Leib, R.; Bunnell, C.A. Data-driven appointment-scheduling under uncertainty: The case of an infusion unit in a cancer center. Manag. Sci. 2020 , 66 , 243–270. [ Google Scholar ] [ CrossRef ]
- Pandey, M.; Arora, M.; Arora, S.; Goyal, C.; Gera, V.K.; Yadav, H. AI-based Integrated Approach for the Development of Intelligent Document Management System (IDMS). Procedia Comput. Sci. 2023 , 230 , 725–736. [ Google Scholar ] [ CrossRef ]
- Hsu, E.; Malagaris, I.; Kuo, Y.-F.; Sultana, R.; Roberts, K. Deep learning-based NLP data pipeline for EHR-scanned document information extraction. JAMIA Open 2022 , 5 , ooac045. [ Google Scholar ] [ CrossRef ]
- Kreps, G.L.; Neuhauser, L. Artificial intelligence and immediacy: Designing health communication to personally engage consumers and providers. Patient Educ. Couns. 2013 , 92 , 205–210. [ Google Scholar ] [ CrossRef ]
- Kingston, J. Using artificial intelligence to support compliance with the general data protection regulation. Artif. Intell. Law 2017 , 25 , 429–443. [ Google Scholar ] [ CrossRef ]
- Hamdani, R.E.; Mustapha, M.; Amariles, D.R.; Troussel, A.; Meeùs, S.; Krasnashchok, K. A combined rule-based and machine learning approach for automated GDPR compliance checking. In Proceedings of the Eighteenth International Conference on Artificial Intelligence and Law, São Paulo, Brazil, 21–25 June 2021; pp. 40–49. [ Google Scholar ]
- El-Bouri, R.; Taylor, T.; Youssef, A.; Zhu, T.; Clifton, D.A. Machine learning in patient flow: A review. Prog. Biomed. Eng. 2021 , 3 , 022002. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, T.; Asanjan, A.A.; Welles, E.; Gao, X.; Sorooshian, S.; Liu, X. Developing reservoir monthly inflow forecasts using artificial intelligence and climate phenomenon information. Water Resour. Res. 2017 , 53 , 2786–2812. [ Google Scholar ] [ CrossRef ]
- Knight, D.; Aakre, C.A.; Anstine, C.V.; Munipalli, B.; Biazar, P.; Mitri, G.; Valery, J.R.; Brigham, T.; Niazi, S.K.; Perlman, A.I. Artificial Intelligence for Patient Scheduling in the Real-World Health Care Setting: A Metanarrative Review. Health Policy Technol. 2023 , 12 , 100824. [ Google Scholar ] [ CrossRef ]
- Wang, J.; Fung, R.Y. Adaptive dynamic programming algorithms for sequential appointment scheduling with patient preferences. Artif. Intell. Med. 2015 , 63 , 33–40. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, X.; Tian, D.; Li, W.; Dong, B.; Wang, H.; Yuan, J.; Li, B.; Shi, L.; Lin, X.; Zhao, L. Artificial intelligence-assisted reduction in patients’ waiting time for outpatient process: A retrospective cohort study. BMC Health Serv. Res. 2021 , 21 , 237. [ Google Scholar ] [ CrossRef ]
- Joshi, I. Waiting for deep medicine. Lancet 2019 , 393 , 1193–1194. [ Google Scholar ] [ CrossRef ]
- Joseph, J.; Senith, S.; Kirubaraj, A.A.; Ramson, J.S. Machine Learning for Prediction of Wait Times in Outpatient Clinic. Procedia Comput. Sci. 2022 , 215 , 230–239. [ Google Scholar ] [ CrossRef ]
- Khanbhai, M.; Anyadi, P.; Symons, J.; Flott, K.; Darzi, A.; Mayer, E. Applying natural language processing and machine learning techniques to patient experience feedback: A systematic review. BMJ Health Care Inform. 2021 , 28 , e100262. [ Google Scholar ] [ CrossRef ]
- Bari, V.; Hirsch, J.S.; Narvaez, J.; Sardinia, R.; Bock, K.R.; Oppenheim, M.I.; Meytlis, M. An approach to predicting patient experience through machine learning and social network analysis. J. Am. Med. Inform. Assoc. 2020 , 27 , 1834–1843. [ Google Scholar ] [ CrossRef ]
- Darley, S.; Coulson, T.; Peek, N.; Moschogianis, S.; Van Der Veer, S.N.; Wong, D.C.; Brown, B.C. Understanding how the design and implementation of online consultations affect primary care quality: Systematic review of evidence with recommendations for designers, providers, and researchers. J. Med. Internet Res. 2022 , 24 , e37436. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Frid-Adar, M.; Amer, R.; Gozes, O.; Nassar, J.; Greenspan, H. COVID-19 in CXR: From detection and severity scoring to patient disease monitoring. IEEE J. Biomed. Health Inform. 2021 , 25 , 1892–1903. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, Y.; Schönlieb, C.-B.; Lio, P.; Leiner, T.; Dragotti, P.L.; Wang, G.; Rueckert, D.; Firmin, D.; Yang, G. AI-based reconstruction for fast MRI—A systematic review and meta-analysis. Proc. IEEE 2022 , 110 , 224–245. [ Google Scholar ] [ CrossRef ]
- Fusco, R.; Grassi, R.; Granata, V.; Setola, S.V.; Grassi, F.; Cozzi, D.; Pecori, B.; Izzo, F.; Petrillo, A. Artificial intelligence and COVID-19 using chest CT scan and chest X-ray images: Machine learning and deep learning approaches for diagnosis and treatment. J. Pers. Med. 2021 , 11 , 993. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Panayides, A.S.; Amini, A.; Filipovic, N.D.; Sharma, A.; Tsaftaris, S.A.; Young, A.; Foran, D.; Do, N.; Golemati, S.; Kurc, T. AI in medical imaging informatics: Current challenges and future directions. IEEE J. Biomed. Health Inform. 2020 , 24 , 1837–1857. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, Y.; Zhang, F.; Chen, C.; Wang, S.; Wang, Y.; Yu, Y. Act like a radiologist: Towards reliable multi-view correspondence reasoning for mammogram mass detection. IEEE Trans. Pattern Anal. Mach. Intell. 2021 , 44 , 5947–5961. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, F.; Zhang, Q.; Huang, C.; Shi, C.; Wang, L.; Shi, N.; Fang, C.; Shan, F.; Mei, X.; Shi, J. CT quantification of pneumonia lesions in early days predicts progression to severe illness in a cohort of COVID-19 patients. Theranostics 2020 , 10 , 5613. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Johnson, D.; Goodman, R.; Patrinely, J.; Stone, C.; Zimmerman, E.; Donald, R.; Chang, S.; Berkowitz, S.; Finn, A.; Jahangir, E. Assessing the accuracy and reliability of AI-generated medical responses: An evaluation of the Chat-GPT model. Res. Sq. 2023 , Preprint. [ Google Scholar ]
- Bera, K.; Braman, N.; Gupta, A.; Velcheti, V.; Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 2022 , 19 , 132–146. [ Google Scholar ] [ CrossRef ]
- Lee, R.Y.; Wu, Y.; Goh, D.; Tan, V.; Ng, C.W.; Lim, J.C.T.; Lau, M.C.; Yeong, J.P.S. Application of Artificial Intelligence to in vitro Tumor Modeling and Characterization of the Tumor Microenvironment. Adv. Healthc. Mater. 2023 , 12 , 2202457. [ Google Scholar ] [ CrossRef ]
- Acs, B.; Rantalainen, M.; Hartman, J. Artificial intelligence as the next step towards precision pathology. J. Intern. Med. 2020 , 288 , 62–81. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bera, K.; Schalper, K.A.; Rimm, D.L.; Velcheti, V.; Madabhushi, A. Artificial intelligence in digital pathology—New tools for diagnosis and precision oncology. Nat. Rev. Clin. Oncol. 2019 , 16 , 703–715. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pandey, I.; Misra, V.; Pandey, A.T.; Ramteke, P.W.; Agrawal, R. Artificial intelligence technologies empowering identification of novel diagnostic molecular markers in gastric cancer. Ind. J. Pathol. Microbiol. 2021 , 64 (Suppl. S1), S63–S68. [ Google Scholar ]
- Segura, F.; Segura, P.; Segura, F. Measuring Tumor Aggressiveness Through Artificial Intelligence. J. Asoc. Argent. Ortop. Traumatol. 2023 , 88 , 653–661. [ Google Scholar ] [ CrossRef ]
- Liopyris, K.; Gregoriou, S.; Dias, J.; Stratigos, A.J. Artificial intelligence in dermatology: Challenges and perspectives. Dermatol. Ther. 2022 , 12 , 2637–2651. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahmad, S.; Wasim, S. Prevent medical errors through artificial intelligence: A review. Saudi J. Med. Pharm. Sci. 2023 , 9 , 419–423. [ Google Scholar ] [ CrossRef ]
- Soun, J.; Chow, D.; Nagamine, M.; Takhtawala, R.; Filippi, C.; Yu, W.; Chang, P. Artificial intelligence and acute stroke imaging. Am. J. Neuroradiol. 2021 , 42 , 2–11. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brereton, T.A.; Malik, M.M.; Lifson, M.; Greenwood, J.D.; Peterson, K.J.; Overgaard, S.M. The Role of Artificial Intelligence Model Documentation in Translational Science: Scoping Review. Interact. J. Med. Res. 2023 , 12 , e45903. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Klement, W.; El Emam, K. Consolidated reporting guidelines for prognostic and diagnostic machine learning modeling studies: Development and validation. J. Med. Internet Res. 2023 , 25 , e48763. [ Google Scholar ] [ CrossRef ]
- Huang, S.-C.; Pareek, A.; Seyyedi, S.; Banerjee, I.; Lungren, M.P. Fusion of medical imaging and electronic health records using deep learning: A systematic review and implementation guidelines. NPJ Digit. Med. 2020 , 3 , 136. [ Google Scholar ] [ CrossRef ]
- Mohsen, F.; Ali, H.; El Hajj, N.; Shah, Z. Artificial intelligence-based methods for fusion of electronic health records and imaging data. Sci. Rep. 2022 , 12 , 17981. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Deng, L.; Li, G.; Han, S.; Shi, L.; Xie, Y. Model compression and hardware acceleration for neural networks: A comprehensive survey. Proc. IEEE 2020 , 108 , 485–532. [ Google Scholar ] [ CrossRef ]
- Alcaín, E.; Fernandez, P.R.; Nieto, R.; Montemayor, A.S.; Vilas, J.; Galiana-Bordera, A.; Martinez-Girones, P.M.; Prieto-de-la-Lastra, C.; Rodriguez-Vila, B.; Bonet, M. Hardware architectures for real-time medical imaging. Electronics 2021 , 10 , 3118. [ Google Scholar ] [ CrossRef ]
- Eklund, A.; Dufort, P.; Forsberg, D.; LaConte, S.M. Medical image processing on the GPU–Past, present and future. Med. Image Anal. 2013 , 17 , 1073–1094. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Corral, J.M.R.; Civit-Masot, J.; Luna-Perejón, F.; Díaz-Cano, I.; Morgado-Estévez, A.; Domínguez-Morales, M. Energy efficiency in edge TPU vs. embedded GPU for computer-aided medical imaging segmentation and classification. Eng. Appl. Artif. Intell. 2024 , 127 , 107298. [ Google Scholar ] [ CrossRef ]
- Lin, Y.; Zhang, Y.; Yang, X. A Low Memory Requirement MobileNets Accelerator Based on FPGA for Auxiliary Medical Tasks. Bioengineering 2022 , 10 , 28. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Azghadi, M.R.; Lammie, C.; Eshraghian, J.K.; Payvand, M.; Donati, E.; Linares-Barranco, B.; Indiveri, G. Hardware implementation of deep network accelerators towards healthcare and biomedical applications. IEEE Trans. Biomed. Circuits Syst. 2020 , 14 , 1138–1159. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jiang, W.; Ye, X.; Chen, R.; Su, F.; Lin, M.; Ma, Y.; Zhu, Y.; Huang, S. Wearable on-device deep learning system for hand gesture recognition based on FPGA accelerator. Math. Biosci. Eng. 2021 , 18 , 132–153. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nayak, D.R.; Dash, R.; Majhi, B. Automated diagnosis of multi-class brain abnormalities using MRI images: A deep convolutional neural network based method. Pattern Recog. Lett. 2020 , 138 , 385–391. [ Google Scholar ] [ CrossRef ]
- Soffer, S.; Klang, E.; Shimon, O.; Barash, Y.; Cahan, N.; Greenspana, H.; Konen, E. Deep learning for pulmonary embolism detection on computed tomography pulmonary angiogram: A systematic review and meta-analysis. Sci. Rep. 2021 , 11 , 15814. [ Google Scholar ] [ CrossRef ]
- Lång, K.; Josefsson, V.; Larsson, A.-M.; Larsson, S.; Högberg, C.; Sartor, H.; Hofvind, S.; Andersson, I.; Rosso, A. Artificial intelligence-supported screen reading versus standard double reading in the Mammography Screening with Artificial Intelligence trial (MASAI): A clinical safety analysis of a randomised, controlled, non-inferiority, single-blinded, screening accuracy study. Lancet Oncol. 2023 , 24 , 936–944. [ Google Scholar ] [ PubMed ]
- Sveric, K.M.; Ulbrich, S.; Dindane, Z.; Winkler, A.; Botan, R.; Mierke, J.; Trausch, A.; Heidrich, F.; Linke, A. Improved assessment of left ventricular ejection fraction using artificial intelligence in echocardiography: A comparative analysis with cardiac magnetic resonance imaging. Int. J. Cardiol. 2024 , 394 , 131383. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Khan, P.; Kader, M.F.; Islam, S.R.; Rahman, A.B.; Kamal, M.S.; Toha, M.U.; Kwak, K.-S. Machine learning and deep learning approaches for brain disease diagnosis: Principles and recent advances. IEEE Access 2021 , 9 , 37622–37655. [ Google Scholar ] [ CrossRef ]
- Adam, R.; Dell’Aquila, K.; Hodges, L.; Maldjian, T.; Duong, T.Q. Deep learning applications to breast cancer detection by magnetic resonance imaging: A literature review. Breast Cancer Res. 2023 , 25 , 87. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sheth, D.; Giger, M.L. Artificial intelligence in the interpretation of breast cancer on MRI. J. Magn. Reson. Imaging 2020 , 51 , 1310–1324. [ Google Scholar ] [ CrossRef ]
- McCrindle, B.; Zukotynski, K.; Doyle, T.E.; Noseworthy, M.D. A radiology-focused review of predictive uncertainty for AI interpretability in computer-assisted segmentation. Radiol. Artif. Intell. 2021 , 3 , e210031. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zheng, R.; Wang, Q.; Lv, S.; Li, C.; Wang, C.; Chen, W.; Wang, H. Automatic liver tumor segmentation on dynamic contrast enhanced mri using 4D information: Deep learning model based on 3D convolution and convolutional lstm. IEEE Trans. Med. Imaging 2022 , 41 , 2965–2976. [ Google Scholar ] [ CrossRef ]
- Schalekamp, S.; Klein, W.M.; van Leeuwen, K.G. Current and emerging artificial intelligence applications in chest imaging: A pediatric perspective. Pediatr. Radiol. 2022 , 52 , 2120–2130. [ Google Scholar ] [ CrossRef ]
- Lee, M.-H.; O’Hara, N.; Sonoda, M.; Kuroda, N.; Juhasz, C.; Asano, E.; Dong, M.; Jeong, J.-W. Novel deep learning network analysis of electrical stimulation mapping-driven diffusion MRI tractography to improve preoperative evaluation of pediatric epilepsy. IEEE Trans. Biomed. Eng. 2020 , 67 , 3151–3162. [ Google Scholar ] [ CrossRef ]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019 , 25 , 954–961. [ Google Scholar ] [ CrossRef ]
- Watanabe, A.T.; Lim, V.; Vu, H.X.; Chim, R.; Weise, E.; Liu, J.; Bradley, W.G.; Comstock, C.E. Improved cancer detection using artificial intelligence: A retrospective evaluation of missed cancers on mammography. J. Digit. Imaging 2019 , 32 , 625–637. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sermesant, M.; Delingette, H.; Cochet, H.; Jais, P.; Ayache, N. Applications of artificial intelligence in cardiovascular imaging. Nat. Rev. Cardiol. 2021 , 18 , 600–609. [ Google Scholar ] [ CrossRef ]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022 , 213 , 106541. [ Google Scholar ] [ CrossRef ]
- Stangl, F.J.; Riedl, R. Measurement of heart rate and heart rate variability with wearable devices: A systematic review. Wirtschaftsinformatik 2022 , 2022 , 15. [ Google Scholar ]
- Huang, J.-D.; Wang, J.; Ramsey, E.; Leavey, G.; Chico, T.J.; Condell, J. Applying artificial intelligence to wearable sensor data to diagnose and predict cardiovascular disease: A review. Sensors 2022 , 22 , 8002. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bahrami, M.; Forouzanfar, M. Deep learning forecasts the occurrence of sleep apnea from single-lead ECG. Cardiovasc. Eng. Technol. 2022 , 13 , 809–815. [ Google Scholar ] [ CrossRef ]
- Joeris, A.; Zhu, T.Y.; Lambert, S.; Wood, A.; Jayakumar, P. Real-world patient data: Can they support decision making and patient engagement? Injury 2023 , 54 , S51–S56. [ Google Scholar ] [ CrossRef ]
- Asthana, S.; Megahed, A.; Strong, R. A recommendation system for proactive health monitoring using IoT and wearable technologies. In Proceedings of the 2017 IEEE International Conference on AI & Mobile Services (AIMS), Honolulu, HI, USA, 25–30 June 2017; IEEE: New, York, NY, USA, 2017; pp. 14–21. [ Google Scholar ]
- Djanian, S.; Bruun, A.; Nielsen, T.D. Sleep classification using Consumer Sleep Technologies and AI: A review of the current landscape. Sleep Med. 2022 , 100 , 390–403. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sabry, F.; Eltaras, T.; Labda, W.; Alzoubi, K.; Malluhi, Q. Machine learning for healthcare wearable devices: The big picture. J. Healthc. Eng. 2022 , 2022 , 1–25. [ Google Scholar ] [ CrossRef ]
- Van Bulck, L.; Couturier, R.; Moons, P. Applications of Artificial Intelligence for Nursing: Has a New Era Arrived? Oxford University Press US: Cary, NC, USA, 2023; Volume 22, pp. e19–e20. [ Google Scholar ]
- Jadczyk, T.; Wojakowski, W.; Tendera, M.; Henry, T.D.; Egnaczyk, G.; Shreenivas, S. Artificial intelligence can improve patient management at the time of a pandemic: The role of voice technology. J. Med. Internet Res. 2021 , 23 , e22959. [ Google Scholar ] [ CrossRef ]
- Adus, S.; Macklin, J.; Pinto, A. Exploring patient perspectives on how they can and should be engaged in the development of artificial intelligence (AI) applications in health care. BMC Health Serv. Res. 2023 , 23 , 1163. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Curtis, R.G.; Bartel, B.; Ferguson, T.; Blake, H.T.; Northcott, C.; Virgara, R.; Maher, C.A. Improving user experience of virtual health assistants: Scoping review. J. Med. Internet Res. 2021 , 23 , e31737. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ye, J.; He, L.; Beestrum, M. Implications for implementation and adoption of telehealth in developing countries: A systematic review of China’s practices and experiences. NPJ Digit. Med. 2023 , 6 , 174. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jeddi, Z.; Bohr, A. Remote patient monitoring using artificial intelligence. In Artificial Intelligence in Healthcare ; Elsevier: Amsterdam, The Netherlands, 2020; pp. 203–234. [ Google Scholar ]
- Shaik, T.; Tao, X.; Higgins, N.; Li, L.; Gururajan, R.; Zhou, X.; Acharya, U.R. Remote patient monitoring using artificial intelligence: Current state, applications, and challenges. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2023 , 13 , e1485. [ Google Scholar ] [ CrossRef ]
- Khadija, A.; Zahra, F.F.; Naceur, A. AI-powered health chatbots: Toward a general architecture. Procedia Comput. Sci. 2021 , 191 , 355–360. [ Google Scholar ] [ CrossRef ]
- Görtz, M.; Baumgärtner, K.; Schmid, T.; Muschko, M.; Woessner, P.; Gerlach, A.; Byczkowski, M.; Sültmann, H.; Duensing, S.; Hohenfellner, M. An artificial intelligence-based chatbot for prostate cancer education: Design and patient evaluation study. Digit. Health 2023 , 9 , 20552076231173304. [ Google Scholar ] [ CrossRef ]
- Sharma, S.; Rawal, R.; Shah, D. Addressing the challenges of AI-based telemedicine: Best practices and lessons learned. J. Educ. Health Promot. 2023 , 12 , 338. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Maleki, F.; Muthukrishnan, N.; Ovens, K.; Reinhold, C.; Forghani, R. Machine learning algorithm validation: From essentials to advanced applications and implications for regulatory certification and deployment. Neuroimaging Clin. 2020 , 30 , 433–445. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lei, J. Cross-validation with confidence. J. Am. Stat. Assoc. 2020 , 115 , 1978–1997. [ Google Scholar ] [ CrossRef ]
- Ebrahimian, S.; Kalra, M.K.; Agarwal, S.; Bizzo, B.C.; Elkholy, M.; Wald, C.; Allen, B.; Dreyer, K.J. FDA-regulated AI algorithms: Trends, strengths, and gaps of validation studies. Acad. Radiol. 2022 , 29 , 559–566. [ Google Scholar ] [ CrossRef ]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable ai: A review of machine learning interpretability methods. Entropy 2020 , 23 , 18. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Davagdorj, K.; Li, M.; Ryu, K.H. Local interpretable model-agnostic explanations of predictive models for hypertension, Advances in Intelligent Information Hiding and Multimedia Signal Processing. In Proceeding of the 16th International Conference on IIHMSP in Conjunction with the 13th International Conference on FITAT, Ho Chi Minh City, Vietnam, 5–7 November 2020 ; Springer: Berlin/Heidelberg, Germany, 2021; Volume 2, pp. 426–433. [ Google Scholar ]
- Nohara, Y.; Matsumoto, K.; Soejima, H.; Nakashima, N. Explanation of machine learning models using shapley additive explanation and application for real data in hospital. Comput. Methods Programs Biomed. 2022 , 214 , 106584. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Puerta-Beldarrain, M.; Gómez-Carmona, O.; Casado-Mansilla, D.; López-de-Ipiña, D. Human-AI collaboration to promote trust, engagement and adaptation in the process of pro-environmental and health behaviour change. In Proceedings of the International Conference on Ubiquitous Computing and Ambient Intelligence, Córdoba, Spain, 29 November–2 December 2022; Springer: Berlin/Heidelberg, Germany, 2022; pp. 381–392. [ Google Scholar ]
- Mishra, A. Scalable AI Governance and Ethics. In Scalable AI and Design Patterns: Design, Develop, and Deploy Scalable AI Solutions ; Springer: Berlin/Heidelberg, Germany, 2024; pp. 147–165. [ Google Scholar ]
- Badnjević, A.; Pokvić, L.G.; Deumić, A.; Bećirović, L.S. Post-market surveillance of medical devices: A review. Technol. Health Care 2022 , 30 , 1315–1329. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Feng, J.; Phillips, R.V.; Malenica, I.; Bishara, A.; Hubbard, A.E.; Celi, L.A.; Pirracchio, R. Clinical artificial intelligence quality improvement: Towards continual monitoring and updating of AI algorithms in healthcare. NPJ Digit. Med. 2022 , 5 , 66. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Murdoch, B. Privacy and artificial intelligence: Challenges for protecting health information in a new era. BMC Med. Ethics 2021 , 22 , 122. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Iserson, K.V. Informed consent for artificial intelligence in emergency medicine: A practical guide. Am. J. Emerg. Med. 2024 , 76 , 225–230. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fletcher, R.R.; Nakeshimana, A.; Olubeko, O. Addressing fairness, bias, and appropriate use of artificial intelligence and machine learning in global health. Front. Media SA 2021 , 3 , 561802. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Smith, H. Clinical AI: Opacity, accountability, responsibility and liability. AI Soc. 2021 , 36 , 535–545. [ Google Scholar ] [ CrossRef ]
- Moltubakk Kempton, A.; Vassilakopoulou, P. Accountability, Transparency and Explainability in AI for Healthcare. 2021. Available online: https://dl.eusset.eu/items/9c739979-ec3f-4510-a02a-553eadee47e2 (accessed on 28 February 2024).
- Kim, B.; Park, J.; Suh, J. Transparency and accountability in AI decision support: Explaining and visualizing convolutional neural networks for text information. Decis. Support Syst. 2020 , 134 , 113302. [ Google Scholar ] [ CrossRef ]
- Carmody, J.; Shringarpure, S.; Van de Venter, G. AI and privacy concerns: A smart meter case study. J. Inf. Commun. Ethics Soc. 2021 , 19 , 492–505. [ Google Scholar ] [ CrossRef ]
- Bandari, V. Enterprise Data Security Measures: A Comparative Review of Effectiveness and Risks Across Different Industries and Organization Types. Int. J. Bus. Intell. Big Data Anal. 2023 , 6 , 1–11. [ Google Scholar ]
- Lehne, M.; Sass, J.; Essenwanger, A.; Schepers, J.; Thun, S. Why digital medicine depends on interoperability. NPJ Digit. Med. 2019 , 2 , 79. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Perugu, B.; Wadhwa, V.; Kim, J.; Cai, J.; Shin, A.; Gupta, A. Pragmatic Approaches to Interoperability–Surmounting Barriers to Healthcare Data and Information Across Organizations and Political Boundaries. Telehealth Med. Today 2023 , 8 , 421. [ Google Scholar ]
- Dikici, E.; Bigelow, M.; Prevedello, L.M.; White, R.D.; Erdal, B.S. Integrating AI into radiology workflow: Levels of research, production, and feedback maturity. J. Med. Imaging 2020 , 7 , 016502. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Balagurunathan, Y.; Mitchell, R.; El Naqa, I. Requirements and reliability of AI in the medical context. Phys. Med. 2021 , 83 , 72–78. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schneeberger, D.; Stöger, K.; Holzinger, A. The European Legal Framework for Medical AI, International Cross-Domain Conference for Machine Learning and Knowledge Extraction ; Springer: Berlin/Heidelberg, Germany, 2020; pp. 209–226. [ Google Scholar ]
- Larson, D.B.; Harvey, H.; Rubin, D.L.; Irani, N.; Justin, R.T.; Langlotz, C.P. Regulatory frameworks for development and evaluation of artificial intelligence–based diagnostic imaging algorithms: Summary and recommendations. J. Am. Coll. Radiol. 2021 , 18 , 413–424. [ Google Scholar ] [ CrossRef ]
- Benjamens, S.; Dhunnoo, P.; Meskó, B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: An online database. NPJ Digit. Med. 2020 , 3 , 118. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Muehlematter, U.J.; Daniore, P.; Vokinger, K.N. Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015–2020): A comparative analysis. Lancet Digit. Health 2021 , 3 , e195–e203. [ Google Scholar ] [ CrossRef ]
- Baric-Parker, J.; Anderson, E.E. Patient data-sharing for AI: Ethical challenges, catholic solutions. Linacre Q. 2020 , 87 , 471–481. [ Google Scholar ] [ CrossRef ]
- Johnson, K.B.; Wei, W.Q.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision medicine, AI, and the future of personalized health care. Clin. Transl. Sci. 2021 , 14 , 86–93. [ Google Scholar ] [ CrossRef ]
- Bandyopadhyay, A.; Goldstein, C. Clinical applications of artificial intelligence in sleep medicine: A sleep clinician’s perspective. Sleep Breath. 2023 , 27 , 39–55. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Galkin, F.; Zhavoronkov, A. AI in Longevity. In Artificial Intelligence for Healthy Longevity ; Springer: Berlin/Heidelberg, Germany, 2023; pp. 3–13. [ Google Scholar ]
- Zhavoronkov, A.; Mamoshina, P.; Vanhaelen, Q.; Scheibye-Knudsen, M.; Moskalev, A.; Aliper, A. Artificial intelligence for aging and longevity research: Recent advances and perspectives. Ageing Res. Rev. 2019 , 49 , 49–66. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jiménez-Luna, J.; Grisoni, F.; Weskamp, N.; Schneider, G. Artificial intelligence in drug discovery: Recent advances and future perspectives. Expert Opin. Drug Discov. 2021 , 16 , 949–959. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Feizi, N.; Tavakoli, M.; Patel, R.V.; Atashzar, S.F. Robotics and ai for teleoperation, tele-assessment, and tele-training for surgery in the era of COVID-19: Existing challenges, and future vision. Front. Robot. AI 2021 , 8 , 610677. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bitencourt, A.; Naranjo, I.D.; Gullo, R.L.; Saccarelli, C.R.; Pinker, K. AI-enhanced breast imaging: Where are we and where are we heading? Eur. J. Radiol. 2021 , 142 , 109882. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shi, Q.; Dong, B.; He, T.; Sun, Z.; Zhu, J.; Zhang, Z.; Lee, C. Progress in wearable electronics/photonics—Moving toward the era of artificial intelligence and internet of things. InfoMat 2020 , 2 , 1131–1162. [ Google Scholar ] [ CrossRef ]
- Forghani, N.; Maghooli, K.; Dabanloo, N.J.; Farahani, A.V.; Forouzanfar, M. Intelligent oscillometric system for automatic detection of peripheral arterial disease. IEEE J. Biomed. Health Inform. 2021 , 25 , 3209–3218. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Huang, C.-H.; Batarseh, F.A.; Boueiz, A.; Kulkarni, A.; Su, P.-H.; Aman, J. Measuring outcomes in healthcare economics using Artificial Intelligence: With application to resource management. Data Policy 2021 , 3 , e30. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Giuste, F.; Shi, W.; Zhu, Y.; Naren, T.; Isgut, M.; Sha, Y.; Tong, L.; Gupte, M.; Wang, M.D. Explainable artificial intelligence methods in combating pandemics: A systematic review. IEEE Rev. Biomed. Eng. 2022 , 16 , 5–21. [ Google Scholar ] [ CrossRef ]
- Cao, L. AI in Combating the COVID-19 Pandemic. IEEE Intell. Syst. 2022 , 37 , 3–13. [ Google Scholar ] [ CrossRef ]
- Gu, X.; Deligianni, F.; Han, J.; Liu, X.; Chen, W.; Yang, G.-Z.; Lo, B. Beyond supervised learning for pervasive healthcare. IEEE Rev. Biomed. Eng. 2023 , 17 , 42–62. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fechter, T.; Baltas, D. One-shot learning for deformable medical image registration and periodic motion tracking. IEEE Trans. Med. Imaging 2020 , 39 , 2506–2517. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Feng, R.; Zheng, X.; Gao, T.; Chen, J.; Wang, W.; Chen, D.Z.; Wu, J. Interactive few-shot learning: Limited supervision, better medical image segmentation. IEEE Trans. Med. Imaging 2021 , 40 , 2575–2588. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mahapatra, D.; Bozorgtabar, B.; Ge, Z. Medical image classification using generalized zero shot learning. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, QC, Canada, 10–17 October 2021; pp. 3344–3353. [ Google Scholar ]
- Hospedales, T.; Antoniou, A.; Micaelli, P.; Storkey, A. Meta-learning in neural networks: A survey. IEEE Trans. Pattern Anal. Mach. Intell. 2021 , 44 , 5149–5169. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, J.; Soltan, A.A.; Clifton, D.A. Machine learning generalizability across healthcare settings: Insights from multi-site COVID-19 screening. NPJ Digit. Med. 2022 , 5 , 69. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Khoshnevisan, F.; Chi, M. Unifying domain adaptation and domain generalization for robust prediction across minority racial groups, Machine Learning and Knowledge Discovery in Databases. In Proceedings of the Research Track: European Conference, ECML PKDD 2021, Bilbao, Spain, 13–17 September 2021; Proceedings, Part I 21. Springer: Berlin/Heidelberg, Germany, 2021; pp. 521–537. [ Google Scholar ]
- Rieke, N.; Hancox, J.; Li, W.; Milletari, F.; Roth, H.R.; Albarqouni, S.; Bakas, S.; Galtier, M.N.; Landman, B.A.; Maier-Hein, K. The future of digital health with federated learning. NPJ Digit. Med. 2020 , 3 , 119. [ Google Scholar ] [ CrossRef ]
- Hogg, H.D.J.; Al-Zubaidy, M.; Talks, J.; Denniston, A.K.; Kelly, C.J.; Malawana, J.; Papoutsi, C.; Teare, M.D.; A Keane, P.; Beyer, F.R.; et al. Stakeholder perspectives of clinical artificial intelligence implementation: Systematic review of qualitative evidence. J. Med. Internet Res. 2023 , 25 , e39742. [ Google Scholar ] [ CrossRef ]
- Gerlings, J.; Jensen, M.S.; Shollo, A. Explainable ai, but explainable to whom? an exploratory case study of xai in healthcare. In Handbook of Artificial Intelligence in Healthcare: Vol 2: Practicalities and Prospects ; Springer: Berlin/Heidelberg, Germany, 2022; pp. 169–198. [ Google Scholar ]
Click here to enlarge figure
| Algorithm Type | General Application | Limitations | Comments | Example |
|---|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Image recognition and analysis in medical imaging (e.g., X-rays, MRI, CT scans) | Require large labeled datasets and substantial computational resources; can be a “black box” making interpretability difficult | Highly effective for spatial data; state of the art in medical image analysis | Deeplab v3+, a CNN variant for gastric cancer segmentation [ ]. Results: 95.76% accuracy, outperforming SegNet/ICNet. |
| Recurrent Neural Networks (RNNs) and Long Short-Term Memory (LSTM) Networks | Analysis of sequential data such as ECG, EEG signals, or patient health records | Prone to overfitting on smaller datasets; long training times; difficulty in parallelizing the tasks | Suited for time-series data; LSTM addresses vanishing gradient problem in RNNs | LSTM for EEG signal classification [ ]. Results: 71.3% accuracy, utilizing novel one-dimensional gradient descent activation functions for enhanced performance. |
| Transformer Models (e.g., BERT, GPT) | Natural language processing tasks, including clinical text analysis and patient history summarization | Require significant computational power and memory; pre-training on large datasets is time-consuming | Offer state-of-the-art performance in NLP; enable understanding of context in clinical documentation | Clinical-specific BERT (Transformer) for Japanese text analysis [ ]: pre-trained on 120 million texts, achieving 0.773 Masked-LM and 0.975 Next Sentence Prediction accuracy, indicating potential for complex medical NLP tasks. |
| Generative Adversarial Networks (GANs) | Synthetic data generation for training models without compromising patient privacy; augmenting datasets | Training stability issues; generating high-quality data is challenging | Useful in data-limited scenarios; potential in creating realistic medical images for training | Differentially private GAN for synthetic data generation: utilizes convolutional AEs and GANs to produce realistic synthetic medical data, preserving data characteristics and outperforming existing models [ ]. |
| Graph Neural Networks (GNNs) | Modeling complex relationships and interactions between health data points (e.g., drug interaction prediction, disease progression modeling) | Complex model architectures that are difficult to interpret; scalability to very large graphs | Effective for data represented as graphs; emerging applications in personalized medicine | Knowledge-GNN for drug–drug interaction prediction: leverages knowledge graphs to capture complex drug relationships and neighborhood information, outperforming conventional models [ ]. |
| Aspect | Applications |
|---|---|
| AI for hospital logistics and resource management | Predictive inventory management for medical supplies, medications, and equipment; efficient facility management including HVAC systems and predictive maintenance; optimization of resource allocation for staff and materials; and supply chain optimization and management during emergencies and health crises. |
| Automating administrative tasks with AI | Patient data management including EMRs and unstructured data analysis; billing and claims processing automation for accuracy and compliance; AI-driven scheduling systems for appointments and procedures; document management and processing automation; automated communication and reminders for patient engagement; and data security and compliance monitoring. |
| AI in patient flow and scheduling optimization | Optimization of patient flow through predictive analysis of admissions, discharges, and transfers; dynamic scheduling systems for appointments and procedures, minimizing no-shows and cancellations; reduction in waiting times through better triage processes and real-time patient wait time prediction; and enhancement of patient experience by providing accurate information and integrating with telehealth services for virtual consultations. |
| Imaging Modality | Application | Example of AI System | Impact |
|---|---|---|---|
| MRI | AI applications in MRI analysis encompass detection of brain abnormalities, tumors, strokes, neurodegenerative diseases, and more. AI can analyze images and quantify the volume of affected areas. | An AI system analyzes MRI images to detect brain abnormalities, such as tumors or strokes, and quantifies their volume, aiding in treatment planning [ ]. | Improved detection of tumors, strokes, and neurodegenerative diseases; quantification of affected areas aids in treatment planning and disease monitoring. |
| CT | AI in CT scan interpretation includes detecting lung nodules, identifying fractures and hemorrhages, assessing stroke severity, and characterizing tumor progression. AI systems can process CT scans rapidly and accurately, aiding in timely diagnosis. | An AI model diagnoses lung cancer with high accuracy and reduced false positives, improving diagnostic precision [ ]. | Faster detection of life-threatening conditions; enhanced accuracy compared to traditional methods; potential to save lives in emergency situations. |
| X-ray | AI applications in X-ray enhance image analysis for tumor detection, improving accuracy and reducing false positives and negatives. AI systems serve as a second reviewer, enhancing the sensitivity of cancer screening. | AI-based CAD algorithms significantly improve radiologists’ sensitivity in breast cancer detection, reducing false negatives and improving cancer detection rates [ ]. | Increased sensitivity in detecting breast cancer lesions; reduction in false positives and negatives; enhancement of radiologists’ diagnostic accuracy. |
| Ultrasound | AI aids in analyzing echocardiography scans to assess cardiovascular function and detect structural abnormalities of the heart. AI systems measure parameters such as ejection fraction and aid in diagnosing and managing heart diseases. | A novel AI algorithm accurately calculates left ventricular ejection time in echocardiography, providing reliable metrics for cardiac function assessment [ ]. | Accurate assessment of cardiovascular parameters; reduction in user-dependent variability; enhancement of clinical utility in echocardiography. |
| Main Applications | Key Technologies and Applications | Benefits | Challenges |
|---|---|---|---|
| AI-powered wearable devices | Continuous physiological monitoring (heart rate, blood pressure, etc.); early detection of health issues; personalized recommendations for lifestyle changes | Improved patient engagement; proactive health management | Data collection and model deployment; balancing accuracy with wearable device limitations |
| Virtual nursing assistants | 24/7 patient support and health reminders; chronic disease management; patient education and behavior monitoring | Enhanced patient engagement and education; improved treatment plan compliance | Data privacy and information accuracy; ensuring they complement human care |
| AI in telemedicine and remote patient engagement | Advanced diagnostics and consultations; personalized virtual consultations; remote patient monitoring and predictive analytics | Increased healthcare accessibility; proactive chronic condition care | Data privacy, system accuracy, and integration |
| Trend/Application | Potential Impact | Challenges | Future Directions |
|---|---|---|---|
| Personalized medicine | Revolutionizes treatment for diseases with genetic components, significantly improving patient outcomes through customized care plans. | Data privacy, integration into clinical practice, and ensuring equitable access across diverse patient populations. | Expanding personalized medicine to encompass mental health, lifestyle diseases, and integrating real-time health monitoring data for dynamic treatment adjustments. |
| AI-powered tools for health and sleep monitoring | Improved detection and diagnosis of sleep disorders, early identification of potential health issues, personalized treatment, and proactive interventions. | Data privacy, accuracy of predictions, and user acceptance and comfort with interventional technologies. | Designing analysis and intervention technologies to monitor, predict, and manage health issues and sleep disorders; integration with wearable devices and smart home technology, providing real-time adjustments. |
| Longevity and aging | Unlocks new possibilities in aging research, promoting healthier, extended lifespans through AI-driven genomic interventions and predictive analytics for preventive medicine. | Addressing ethical implications of longevity research, ensuring accessibility and fairness in anti-aging treatments. | Leveraging AI for comprehensive health longevity platforms, integrating AI with regenerative medicine, and creating personalized anti-aging treatment plans based on predictive health analytics. |
| AI in drug discovery and development | Reduces time and costs in drug market introduction, enhances the efficacy of new drugs by identifying optimal candidate molecules. | Ensuring the reliability of AI predictions; ethical concerns around automated decision-making in drug development. | Leveraging AI to explore novel drug pathways, improve clinical trial design, and predict patient responses to treatments more accurately. |
| Advanced robotics in surgery and rehabilitation | Improves precision in surgeries and patient outcomes in rehabilitation, potentially reducing recovery times and healthcare costs. | Ethical considerations around autonomy; the need for robust training programs for medical staff on robotic systems. | Developing autonomous surgical robots, enhancing robotic systems with sensory feedback for improved rehabilitation outcomes, and expanding applications in minimally invasive procedures. |
| AI hardware accelerators | Faster diagnoses, treatment planning, and analysis, improved patient care outcomes, and real-time medical data processing. | Integration with medical devices; cost and power consumption of accelerators. | Develop healthcare-specific AI hardware; improve accessibility of AI-driven healthcare. |
| AI-enhanced medical imaging | Enables earlier and more accurate disease detection, potentially even identifying health risks before symptoms appear, thus shifting towards preventive healthcare models. | Balancing the need for patient privacy with the benefits of data sharing for AI training; integrating AI tools with existing healthcare infrastructures. | Developing AI systems capable of cross-modality analysis, improving 3D imaging techniques, and creating predictive models for disease progression based on imaging data. |
| Integrating AI with IoT and wearables | Leads to proactive health management and personalized health recommendations, potentially reducing emergency healthcare interventions. | Addressing data security and ensuring device interoperability across different healthcare systems. | Enhancing predictive analytics for early detection of health anomalies, creating an ecosystem of interconnected devices for holistic health monitoring; unobtrusive health monitoring. |
| Enhancing patient outcomes and system efficiency | Promises significant improvements in patient care through earlier disease detection, customized treatments, and optimized healthcare resource management. | Ensuring equitable improvements across all populations, addressing the digital divide in healthcare access. | Implementing AI-driven health advisories in public health strategies, optimizing healthcare delivery models with predictive resource allocation, and enhancing remote patient monitoring systems. |
| Global health monitoring systems | Strengthens global health security by enabling rapid response to disease outbreaks and guiding public health interventions with data-driven insights. | Integrating diverse data streams in real time, adapting models quickly to emerging health threats. | Developing global AI-powered surveillance systems, enhancing predictive models for epidemic and pandemic forecasting, and creating AI-driven platforms for vaccine and therapeutic development. |
| Addressing data scarcity | Facilitates AI development in under-researched areas, such as rare diseases, by making efficient use of limited data resources. | Creating effective models with sparse data, ensuring the generalizability of findings from limited datasets. | Exploring novel data augmentation techniques, crowdsourcing for data collection, and cross-institutional data sharing initiatives to enrich datasets. Developing advanced techniques based on few-shot leaning. |
| Ensuring model versatility | Allows for the broader application of AI models across varying healthcare settings and patient demographics, improving the universality and accessibility of AI-driven healthcare solutions. | Developing adaptable models that maintain high accuracy across diverse datasets, addressing potential biases in AI training. | Advancing transfer learning and domain adaptation techniques that can be personalized at the point of care. |
| Ensuring data privacy | Enhances privacy and security in healthcare applications, addressing one of the major concerns of digital health data management. | Balancing the utility of data for AI training with stringent privacy requirements, adapting regulations to keep pace with technological advancements. | Developing more advanced privacy-preserving AI techniques, such as secure multi-party computation, federated learning, and advanced encryption methods for health data. |
| Stakeholder acceptance | Successful AI integration in healthcare; improved trust and collaboration. | Concerns about AI reliability and clinician autonomy. | Transparent communication and training programs. |
| Building trust with Explainable AI (XAI) | Enhances the trustworthiness of AI systems among healthcare professionals and patients, ensuring that AI-supported decisions are well informed and ethically sound. | Simplifying complex AI decision-making processes for non-technical stakeholders, ensuring explanations are meaningful and actionable. | Integrating XAI into clinical workflows, developing standards for AI explanations in healthcare, and educating healthcare professionals on interpreting AI decisions. |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Maleki Varnosfaderani, S.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024 , 11 , 337. https://doi.org/10.3390/bioengineering11040337
Maleki Varnosfaderani S, Forouzanfar M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering . 2024; 11(4):337. https://doi.org/10.3390/bioengineering11040337
Maleki Varnosfaderani, Shiva, and Mohamad Forouzanfar. 2024. "The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century" Bioengineering 11, no. 4: 337. https://doi.org/10.3390/bioengineering11040337
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 March 2024
Generative AI and large language models in health care: pathways to implementation
- Marium M. Raza ORCID: orcid.org/0000-0001-8050-9402 1 ,
- Kaushik P. Venkatesh ORCID: orcid.org/0000-0002-1736-4367 1 &
- Joseph C. Kvedar ORCID: orcid.org/0000-0002-7517-2291 1
npj Digital Medicine volume 7 , Article number: 62 ( 2024 ) Cite this article
9139 Accesses
6 Citations
20 Altmetric
Metrics details
- Health care economics
- Health policy
Generative AI is designed to create new content from trained parameters. Learning from large amounts of data, many of these models aim to simulate human conversation. Generative AI is being applied to many different sectors. Within healthcare there has been innovation specifically towards generative AI models trained on electronic medical record data. A recent review characterizes these models, their strengths, and weaknesses. Inspired by that work, we present our evaluation checklist for generative AI models applied to electronic medical records.
Introduction
In November 2022, OpenAI launched ChatGPT, an artificial intelligence (AI) chatbot and search tool. ChatGPT is a tool that uses generative AI: AI that is designed to create or generate new content, such as text, images, or music from trained parameters 1 . Tools like ChatGPT use “large language models” (LLMs), multi-layer neural networks that are trained on large amounts of data to simulate human conversation 2 . Other LLM tools include Google’s Bard, Microsoft Bing, Chatsonic, Github Copilot, and ChatSonic to name just a few. LLMs themselves are an example of a “foundation model,” a broader term for an AI model trained on a large quantity of data at scale.
The buzz around generative AI has skyrocketed, with ChatGPT expanding to have over 100 million users 3 . Over the past year, many have shown excitement for potential generative AI applications to healthcare. LLMs have already been used to pass the United States Medical Licensing Examination 4 , write research articles 5 , and interpret electronic medical record data 6 . This last use case is perhaps closest to the bedside. Generative AI models trained on EMR data, such as notes, lab values, and billing codes, hold the promise of better predictive performance, simpler model development (with less labeled data required) and cheaper model deployment 7 . At the same time, those critiquing the utility of these applications have argued that generative AI is simply another health-tech fad, with many roadblocks preventing its implementation 8 . One valid concern for example is regarding generative AI models ‘hallucinating,’ or inventing responses when they do not have sufficient information 9 .
Evaluating generative AI models for EMRs
In their review, Wornow et al. explore the current state of generative AI models for EMRs 7 . Specifically, Wornow et al. conducted a review of 84 foundation models trained on clinical structured text data from EMRs. This is the largest review of foundation models within health care to date. To define the key characteristics of the models, Wornow et al. make the distinction between (i) clinical language models, which intake, and output clinical text, and (ii) EMR models that intake a patient’s entire EMR to output a machine-understandable ‘representation’ for a patient, similar to a digital twin 10 .
Wornow et al. found evidence that both types of models enable more accurate model predictions, but authors also found limitations. Currently, nearly all clinical text models are trained on either a single relatively small database or the entirety of PubMed. The ‘representation’ models are trained on small public datasets only or a single private healthcare system’s EMR. Thus, Wornow et al. found that current uses of generative AI within healthcare are limited by their lack of generalizability and issues of data privacy. Specifically, AI models based on data from different EMR systems are not generalizable, and very few AI models have had details, such as model weights, published due to data privacy concerns. Additionally, minimal work has been conducted to validate whether other, potentially more valuable benefits of FMs will be realized in healthcare (Table 1 ).
Noting those limitations, Wornow et al. propose an improved framework to evaluate generative AI models for healthcare settings. They elaborate upon six criteria: predictive performance, data labeling, model deployment, emergent clinical applications, multimodality, and novel human-AI interfaces. By evaluating models around these criteria, Wornow et al. argue that health systems will be better able to judge which are best for more stratified clinical needs.
Applying the Wornow et al. framework
This work comes at a time when exciting new EMR LLMs are being launched. For example, in April Microsoft announced a partnership integrating its OpenAI service with the Epic EHR. This collaboration may involve using generative AI to auto-draft responses to common and/or time-intensive patient messages 11 . Oracle Cerner has also integrated generative AI into its EHR. Recently, (Nov 2023), Oracle Cerner announced the Oracle Clinical Digital Assistant tool, a multimodal voice and screen-based tool that will participate in appointments by automating notetaking and proposing actions such as medication orders, labs, and follow-up appointments. Providers should be able to talk to the tool to access elements of a patient’s EHR, while patients should be able to talk to the tool to book appointments and ask questions 12 . In deciding to implement either Epic or Oracle Cerner’s generative AI applications, Wornow et al.’s evaluation framework becomes important to assess each model’s true clinical value. Below is a checklist to be used while conducting a model evaluation, stemming from Wornow et al.’s six points. This type of checklist could be modified based on a specific generative AI model or clinical setting, and then could be used regularly for model evaluation.
The pathway forward: leadership, incentives, and regulation
The improved evaluation framework Wornow et al. propose is one important step forward. To truly make generative AI more than just a fad within healthcare, a broader pathway to implementation is required. This pathway must include defined leadership for development, adoption incentives, and continued regulation.
Leadership will be required first and foremost to push continued model development, validation, and implementation. Currently, generative AI models have been developed by startup companies, research groups, as well as academic healthcare systems. Given these varied developers, guidance from a leadership body is needed to clarify the practical path towards implementation. Leadership should focus on developing guidelines for model performance (i.e. minimizing model hallucination), data sharing, finding the optimal healthcare settings for clinical trials using generative AI tools, as well as clarifying the needs of different healthcare settings (i.e. community vs. academic, private vs. public institutions). Ideally, this type of leadership will come from an organization involving physicians, healthcare administrators, developers, and investors. A sub-committee within the FDA could be well positioned to undertake such responsibility.ßß
Alongside leadership, continued regulation will be required to balance the interests of developers, healthcare systems, payers, and patients. The continued evaluation of tools based on frameworks such as that developed by Wornow et al. must be conducted on the scale of individual health institutions so that tools with clinical relevance are prioritized. On the larger scale, as with other AI tools, policies surrounding liability, data privacy, and bias within predictive modeling must be clarified before insights from generative AI tools can be put into practice. While the FDA has begun to adapt its regulatory framework to address AI technology as medical devices it must move from discussion to action, and provide specific guidance for LLMs 13 , 14 . The FDA can learn from the strengths as well as the criticisms of the EU’s AI Act, one of the first formal regulations for generative AI 15 .
Finally, as with any other healthcare technology, payer incentives must be present before widespread implementation. Generative AI tools will likely be considered a capital expense in the books of most providers and can follow along the same or similar financing path as EHR systems. Additionally, given that the cost to create and evaluate generative AI tools remains somewhat prohibitive, both private and public investment will be required to truly push the field forward.
The time is now to capitalize on the excitement around generative AI and LLMs. The weakness of the generative AI space that Wornow et al. highlight, including those around model generalizability and evaluation, should be taken as guideposts for improvement. With leadership, incentivization, and regulation, generative AI within healthcare can be put on a feasible pathway for implementation.
Data availability
No datasets were produced or analyzed for this article.
Code availability
No computer code was produced or analyzed for this article.
Boscardin C. K., Gin B., Golde P. B. & Hauer K. E. ChatGPT and generative artificial intelligence for medical education: potential impact and opportunity. Acad Med https://doi.org/10.1097/ACM.0000000000005439 (2023).
Alberts, IanL. et al. Large language models (LLM) and ChatGPT: what will the impact on nuclear medicine be? Eur. J. Nuclear Med. Mol. Imag. 50 , 1549–1552 (2023).
Article Google Scholar
Hu, K. ChatGPt sets record for fastest-growing user base. Reuters www.reuters.com/technology/chatgpt-sets-record-fastest-growing-user-base-analyst-note-2023-02-01/ (2023).
Kung, T. H. et al. Performance of ChatGPT on USMLE: potential for AI-assisted medical education using large language models. PLoS Digit Health 2 , e0000198 (2023).
Article PubMed PubMed Central Google Scholar
Macdonald, C., Adeloye, D., Sheikh, A. & Rudan, I. Can ChatGPT draft a research article? An example of population-level vaccine effectiveness analysis. J. Glob. Health 13 , 01003 (2023).
Pang, C. et al. CEHR-BERT: Incorporating temporal information from structured EHR data to improve prediction tasks. arXiv https://doi.org/10.48550/arXiv.2111.08585 (2021)
Wornow, M. et al. The shaky foundations of large language models and foundation models for electronic health records. npj Digit. Med. 6 , 135 (2023).
Duffourc, M. & Gerke, S. Generative Ai in health care and liability risks for physicians and safety concerns for patients. JAMA. 330 , 313–314, https://doi.org/10.1001/jama.2023.9630 (2023).
Article PubMed Google Scholar
Weise K. & Metz C. When A.I. Chatbots Hallucinate. The New York Times . The New York Times Company https://www.nytimes.com/2023/05/01/business/ai-chatbots-hallucination.html (2023).
Venkatesh, K. P., Raza, M. M. & Kvedar, J. C. Health digital twins as tools for precision medicine: Considerations for computation, implementation, and regulation. npj Digit. Med. 5 , 150 (2022).
Microsoft News Center. Microsoft and epic expand strategic collaboration with integration of azure openai service. Microsoft News , Microsoft. news.microsoft.com/2023/04/17/microsoft-and-epic-expand-strategic-collaboration-with-integration-of-azure-openai-service/ (2023).
Landi, H. Oracle Health integrates generative AI, voice tech into EHR system to automate medical note-taking. Fierce Healthcare . Questex LLC https://www.fiercehealthcare.com/ai-and-machine-learning/oracle-health-integrates-generative-ai-conversational-voice-tech-ehr-system (2023).
FDA. Software as a Medical Device (SAMD): Clinical Evaluation . https://www.fda.gov/media/100714/download (2017).
Meskó, B. & Topol, E. J. The imperative for regulatory oversight of large language models (or generative AI) in healthcare. npj Digit. Med. 6 , 120 (2023).
EU AI Act: first regulation on artificial intelligence. European Parliament . https://www.europarl.europa.eu/news/en/headlines/society/20230601STO93804/eu-ai-act-first-regulation-on-artificial-intelligence (2023).
Download references
Author information
Authors and affiliations.
Harvard Medical School, Boston, MA, USA
Marium M. Raza, Kaushik P. Venkatesh & Joseph C. Kvedar
You can also search for this author in PubMed Google Scholar
Contributions
First draft by M.M.R. Critical revisions by K.P.V. and J.C.K. All authors approved the final draft.
Corresponding author
Correspondence to Marium M. Raza .
Ethics declarations
Competing interests.
J.C.K. is the Editor-in-Chief of npj Digital Medicine . The other authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Raza, M.M., Venkatesh, K.P. & Kvedar, J.C. Generative AI and large language models in health care: pathways to implementation. npj Digit. Med. 7 , 62 (2024). https://doi.org/10.1038/s41746-023-00988-4
Download citation
Received : 17 October 2023
Accepted : 06 December 2023
Published : 07 March 2024
DOI : https://doi.org/10.1038/s41746-023-00988-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Politics of Development
- Public Policy
- Public Administration
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

41 Artificial Intelligence in Healthcare
Nakul Aggarwal, MD-PhD Candidate, Medical Scientist Training Program, University of Wisconsin-Madison
Michael E. Matheny, Professor of Biomedical Informatics, Vanderbilt University Medical Center
Carmel Shachar, Assistant Clinical Professor of Law and Faculty Director, Center for Health Law and Policy Innovation, Harvard Law School, Harvard Law School
Samantha Wang, Clinical Assistant Professor, Department of Medicine, Stanford University
Sonoo Thadaney-Israni, Executive Director, PRESENCE @ Stanford Medicine, Stanford University
- Published: 18 March 2022
- Cite Icon Cite
- Permissions Icon Permissions
Artificial intelligence (AI) is poised to significantly impact healthcare systems, including clinical diagnosis, healthcare administration and delivery, and public health infrastructures. In the context of the Quintuple Aim of healthcare (patient outcomes, cost reduction, population impact, provider wellness, and equity/inclusion), this chapter discusses the current state of AI in healthcare, focusing on issues that may inform the development of adaptive, efficient, and equitable governance frameworks for AI in healthcare. The chapter introduces prominent examples of clinical AI applications in recent years, highlighting their successes and extant limitations. It emphasizes the processes of clinical AI algorithm development, implementation, and provider adoption, noting important policy considerations for active maintenance and updating of such algorithms. It also focuses on the issue of bias in AI algorithms for healthcare by (1) illustrating how unrepresentative and/or inappropriate datasets can exacerbate health disparities and inequities, and (2) emphasizing the need for diversity, transparency, and accountability in algorithm development. It provides an overview of current national and international regulatory approaches for AI-driven medical devices. It concludes with recommendations of strategic goals for developers, healthcare providers, and governmental agencies to work towards cooperatively in building a productive and equitable future for AI in healthcare.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.

Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| October 2022 | 20 |
| November 2022 | 3 |
| December 2022 | 11 |
| January 2023 | 8 |
| February 2023 | 13 |
| March 2023 | 9 |
| April 2023 | 8 |
| May 2023 | 29 |
| June 2023 | 13 |
| July 2023 | 29 |
| August 2023 | 19 |
| September 2023 | 24 |
| October 2023 | 36 |
| November 2023 | 19 |
| December 2023 | 12 |
| January 2024 | 19 |
| February 2024 | 25 |
| March 2024 | 23 |
| April 2024 | 19 |
| May 2024 | 26 |
| June 2024 | 29 |
| July 2024 | 16 |
| August 2024 | 4 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 27 July 2024
Artificial intelligence in medical education - perception among medical students
- Preetha Jackson 1 ,
- Gayathri Ponath Sukumaran 1 ,
- Chikku Babu 1 ,
- M. Christa Tony 1 ,
- Deen Stephano Jack 1 ,
- V. R. Reshma 1 ,
- Dency Davis 1 ,
- Nisha Kurian 1 &
- Anjum John 1
BMC Medical Education volume 24 , Article number: 804 ( 2024 ) Cite this article
581 Accesses
10 Altmetric
Metrics details
As Artificial Intelligence (AI) becomes pervasive in healthcare, including applications like robotic surgery and image analysis, the World Medical Association emphasises integrating AI education into medical curricula. This study evaluates medical students’ perceptions of ‘AI in medicine’, their preferences for AI training in education, and their grasp of AI’s ethical implications in healthcare.
Materials & methods
A cross-sectional study was conducted among 325 medical students in Kerala using a pre-validated, semi structured questionnaire. The survey collected demographic data, any past educational experience about AI, participants’ self-evaluation of their knowledge and evaluated self-perceived understanding of applications of AI in medicine. Participants responded to twelve Likert-scale questions targeting perceptions and ethical aspects and their opinions on suggested topics on AI to be included in their curriculum.
Results & discussion
AI was viewed as an assistive technology for reducing medical errors by 57.2% students and 54.2% believed AI could enhance medical decision accuracy. About 49% agreed that AI could potentially improve accessibility to healthcare. Concerns about AI replacing physicians were reported by 37.6% and 69.2% feared a reduction in the humanistic aspect of medicine. Students were worried about challenges to trust (52.9%), patient-physician relationships (54.5%) and breach of professional confidentiality (53.5%). Only 3.7% felttotally competent in informing patients about features and risks associated with AI applications. Strong demand for structured AI training was expressed, particularly on reducing medical errors (76.9%) and ethical issues (79.4%).
This study highlights medical students’ demand for structured AI training in undergraduate curricula, emphasising its importance in addressing evolving healthcare needs and ethical considerations. Despite widespread ethical concerns, the majority perceive AI as an assistive technology in healthcare. These findings provide valuable insights for curriculum development and defining learning outcomes in AI education for medical students.
Peer Review reports
Introduction
The concept of Artificial Intelligence (AI) dates back to the 1950s when Alan Turing, often referred to as the father of computer science, proposed the question, “Can machines think”? Interestingly, he designed the now famous ‘Turing Test’ where humans were to identify the responder of a question as human or machine [ 1 ]. Subsequently in 1956 John McCarthy coined the term “Artificial Intelligence” [ 2 ] and the next decade saw the birth of the first ever artificial neural network which was “the first machine which is capable of having an original idea” [ 3 ]. Thus progressed the growth of this once unimaginable phenomenon. In this 21st century, most people are familiar with the term AI because of Siri (Intelligent Virtual Assistant) [ 4 ], Open AI’s ChatGPT (language model based chatbot) [ 5 ], traffic prediction by Google Maps or Uber [ 6 ] or customer service bots (AI powered assistants) [ 4 ] that intelligently provide suggestions.
There is no universally accepted definition for AI, but it can be simply defined as “the ability of machines to mimic intelligent human behaviour, including problem solving and learning” [ 7 ]. Specific applications of AI include expert systems, natural language processing, speech recognition, machine vision, and many more, applying which AI has exhibited qualities similar to or even above those of humans [ 8 ].
The use of AI and related technologies is becoming increasingly prevalent in all aspects of human life and beginning to influence the field of healthcare too [ 9 ]. AI technologies have already developed algorithms to analyse a variety of health data, including clinical, behavioural, environmental, and drug information using data from both patients as well as biomedical literature [ 10 ]. Convoluted Neural Networks, designed to automatically and adaptively learn spatial hierarchies of features, can be successfully used to develop diabetic retinopathy screening [ 11 ], skin lesion classification [ 12 ], lymph node metastasis detection [ 13 ], and detection of an abnormality in a radiograph [ 14 ].
Artificial Intelligence can help patients understand their symptoms, influence health seeking behaviour, and thereby improve their quality of life [ 15 ]. AI assistants have even suggested medicines for cancer patients with equal or better efficiency than human experts [ 16 ]. With a capable AI assistant, it is possible to sift through and analyse multitudes of data in a matter of seconds and make conclusions, thus exponentially increasing its applications in biomedical research. AI promises future influences in healthcare in terms of AI assisted robotic surgery, virtual nursing assistants, and image analysis. Simply put, AI can help patients and healthcare providers in diagnosing a disease, assessing risk of disease, estimating treatment success, managing complications, and supporting patients [ 17 ].
Though AI has limitless potential, it has certain vulnerabilities and weaknesses. The quality and relevance of the input data can affect the accuracy of a deep learning diagnostic AI.The kind of funding that is required to construct the machinery and develop an intelligence is not easily accessible in the field of medicine, not to mention the constraints of machine ethics and confidentiality. However, being familiar with the concepts, applications and advantages of AI is definitely beneficial and therefore advisable, especially in the field of medical education and policy making [ 17 , 18 ].
The World Medical Association advocates for a change in medical curricula and educational opportunities for patients, physicians, medical students, health administrators, and other health care professionals to foster a better understanding of the numerous aspects of the healthcare AI, both positive and negative [ 19 ]. Additionally, in 2019, the Standing Committee of European Doctors stressed the need to use AI systems in basic and continuing medical education [ 20 ]. They recommended the need for AI systems to be integrated into medical education, residency training, and continuing medical education courses to increase awareness of the proper use of AI. In this context, there is an emerging need for developing curricula specifically designed to train future physicians on AI.
To develop an effective AI curriculum, we need to understand how today’s medical students perceive AI in medicine, and their comprehension of AI’s ethical dimension as well. However, the available need assessment studies in an Indian setting are barely enough. Grunhut et al. had recommended in 2021 that national surveys need to be carried out among medical students on the attitude and expectations of learning AI in medical colleges for developing a curriculum [ 21 ]. Similar unbiased probability based, large scale surveys would identify the realistic goals physicians will be asked to meet, the expectations that will be put on them, and the resources and knowledge they would need to meet these goals. Also, current literature falls short of a comprehensive needs assessment which is important for curriculum development and defining learning outcomes. Hence in this study we aimed to assess the perceptions on ‘AI in medicine’ among Indian medical students, to assess the proportion of medical students who are in favour of structured training on AI applications during their undergraduate course, and also to assess their perceptions on AI’s ethical dimensions.
Recruitment: A cross-sectional study was conducted among the undergraduate medical students of Pushpagiri Institute of Medical Sciences and Research Centre during the period of June – August 2023. An introductory discussion on the purpose and importance of this study was conducted with each batch of students from first year to house surgeons following which the link to the Google-form containing the consent and questionnaire was shared in the batch Whatsapp groups.
There were a total of 500 medical students in the Institute from 1st year MBBS to the medical students undergoing their internship. The Google form was open for 3 months, with reminder messages sent at intervals of one month. Participation was voluntary (informed consent was obtained through the first section of the Google form)due to which no randomisation could be ensured, implying that some selection bias can be expected.
Participants who did not consent or submitted incomplete questionnaires were excluded from the study. An online survey using Google forms was conducted using a validated semi structured questionnaire which had 3 sections. The questions were adopted from a Turkish study by Civaner et al. [ 22 ]. Since the questionnaire was originally drafted in English, there was no need for translation into a comprehensible language. The first section dealt with demographic details (age, gender and year of study), any past educational experience about AI (had attended training or seminars) and participants’ self-evaluation of their knowledge of AI. The second section consisted of 12 five point Likert questions on medical students’ perceptions of AI including five questions on ethical aspects as well, which were expressed in the form of agreement or disagreement. The last section was about their opinions on selected topics on AI - whether they should be included in their medical curriculum or not. A pilot study was undertaken by administering the questionnaire to a group of 20 medical students who were then posted in the Department of Community Medicine.
Statistical Analysis: Responses on medical students’ perception on the possible influences of AI were graded using Likert scale ranging from 0 (totally disagree) to 4 (totally agree). Data was entered into Microsoft Excel and analysed using Statistical Package for Social Sciences 25.0. Age of the participants is expressed as mean with standard deviation and categorical variables such as opinions, perceptions and year of study are expressed as frequencies and percentages.
Out of 500 medical students in the institution, 327 students participated in the survey. After excluding the incomplete questionnaires, data of 325 participants were analysed. Therefore the response rate amounts to 65%.
The mean (SD) age of the participants was 21.4 (1.9) years, (ranging from 18 to 25 years) with 76% (248/325) females.
AI in medicine- prior knowledge and self-evaluation
Majority of students (91.4%)(297/325) stated that they had not received any training on AI in their medical curriculum, while the others mentioned that they had attended events like seminars and presentations on AI. Almost 52%(169/325) students have heard about AI but possess no knowledge of it. One third of the participants (106/325) self-reported to have ‘partial knowledge’ on AI while none of them reported to be ‘very knowledgeable.’
Of all the participants, only 37.2% (121/325) did not agree with the opinion that AI could replace physicians; instead, the majority thought that it could be an assistant or a tool that would help them. About 37.6% (122/325) of participants agreed that the use of AI would reduce the need for physicians and thus result in loss of jobs. More than half of the participants (173/325) agreed that they would become better physicians with the widespread use of AI applications. Almost 35% (114/325) stated that their choice of specialization would be influenced by how AI was used in that field. Only 26.8% (87/325) of participants totally or mostly agreed that they felt competent enough to give information on AI to patients. More than half of the participants (166/325) were unsure of protecting patient confidentiality while using AI.
Perceptions on the possible influences of AI in medicine
Regarding student perceptions on the possible influences of AI in medicine (Fig. 1 ), the highest agreement (72.3%) was observed on the item ‘reduces error in medical practice’ (235/325) while the lowest agreement (40.3%) was on ‘devalues the medical profession’ (131/325). Students were mostly in favour of applying AI in medicine because they felt it would enable them to make more accurate decisions (72%, (234/325) and would facilitate patients’ access to healthcare (60.9%, 198/325). There were 59.4% (193/325) of participants who agreed that AI would facilitate patient education and 50.5% (164/325) who agreed that AI would allow the patient to increase their control over their own health.
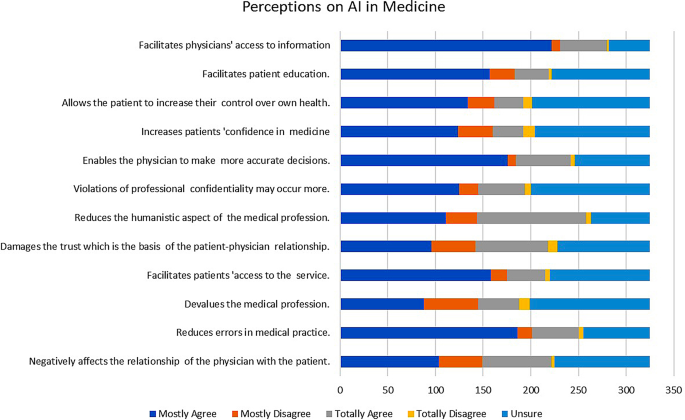
Frequency distribution of perceptions of medical students on AI in medicine
Need for training on AI in medical curriculum
Almost three-fourths of the participants were in favour of structured training on AI applications that should be given during medical education (74.8%, 243/325). The participants thought that it was important to be trained on various topics related to AI in medicine as depicted in Fig. 2 . The most frequent topics that they perceived necessary in this domain were knowledge and skills about AI applications (84.3%274/325), training to prevent and solve ethical problems that may arise with AI applications (79.4%258/325), and AI assisted risk analysis for diseases (78.1%254/325).
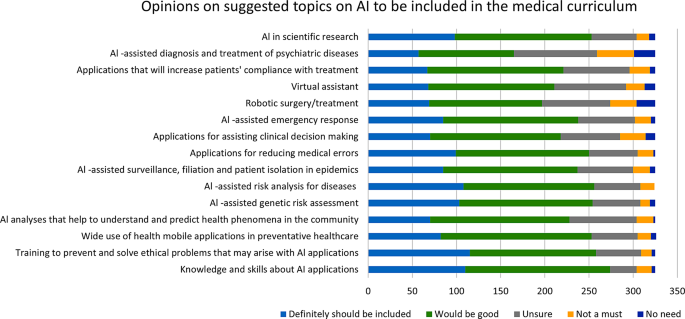
Frequency distribution of opinions of medical students as to whether the suggested topics should be included in their medical curriculum
Ethical concerns regarding AI in medicine (Table 1 )
On the topic of disadvantages and risks of using AI in medicine 69.2% (225/325) agreed that AI would reduce the humanistic aspect of the medical profession, 54.5% (177/325) agreed that it could negatively affect the patient-physician relationship, 52.9% (173/325) were concerned that using AI assisted applications can damage trust in patients while 53.5% (174/325) thought that AI could possibly cause violations of professional confidentiality.
Sub group analysis
Perceptions about being a better doctor with the use of AI applications, being competent enough to inform patients about features & risks of AI applications and the perception about the use of AI in medicine causing a reduction in job opportunities were the ones which showed significant association with the baseline variables like gender, year of study and having prior exposure to course of AI applications as shown in Table 2 .
Although there has been extensive research on the utilisation of AI in medical education the perceptions of medical professionals, and their dilemmas regarding its integration into their daily practice remains relatively underexplored. This research is focused on the perception of medical students about the use of Artificial Intelligence in medicine and its ethical aspects, which reflects their confusions and concerns regarding the situation.
The mean age of the medical students studied was around 21 years and the majority of students were females. Most participants in our study (53.3%) agreed that AI could not replace the presence of a physician but could help them in their work. This is in accordance with the 2021 study conducted by Bisdas S et al. on medical students from 63 countries that AI could work as a “partner” rather than as a “competitor” in their medical practice. A third of our participants (37.6%) felt that the use of AI would reduce the need for physicians and would result in a loss of job opportunities for them. This is a different finding than the study published by D Pinto Dos Santos in European Radiology in 2019 where a majority of participants (83%) felt that human radiologists would not be replaced by robots or computers [ 23 ]. In fact, there are many studies which argue that rather than physicians becoming redundant because of AI, they would change their practice and become “managers” rather than “custodians of information” [ 24 , 25 ].
More than half the respondents in our study (53.3%) agreed that they would become better physicians with the widespread use of AI applications. This is in concurrence with a recently published Western Australian study among medical students which showed about 75% of the participants agreeing that AI would improve their practice [ 26 ]. Respondents from other studies felt that currently available AI systems would actually complement physicians’ decision-making skills by synthesising large amounts of medical literature in order to produce the most up-to-date medical protocols and evidence [ 27 , 28 , 29 , 30 ]. Similarly, studies show that AI systems actually work by complementing the practice of medicine, rather than competing with human minds. After all, human minds have designed artificial intelligence. Furthermore, the study by Paranjape et al. comments that physicians will be able to focus on providing patients with the humanistic care considering the biopsychosocial model of disease as the technicalities can be handled by the AI supported technologies to a greater extent [ 28 ].
A third of the participants (35.1%) in our research stated that their choice of specialisation would be influenced by how AI was used in that field. Much has been written about how AI might replace specialists in the fields of radiology and pathology as perceived by medical doctors and students. These are specialisations that use computers and digital algorithms more when compared to other medical specialties. A Canadian study published in 2019 by Bo Gong et al. found that 67% of the respondents felt that AI would “reduce the demand” for radiologists. Many of the medical students interviewed in this study said that the anxiety they felt about being “displaced” by AI technologies in radiology would discourage them from considering the field for specialisation [ 14 , 31 , 32 , 33 ]. In fact, a paper published by Yurdasik et al. in 2021 had respondents encouraging practitioners to move away from specialisations that used AI [ 34 ]. However, there were other studies that reported results encouraging radiologists to get exposed to AI technologies so as to lower the rates of “imaging related medical errors” and “lessening time spent in reading films,” resulting in more time spent with patients. German medical students have shown a positive attitude towards AI and have reported “not being afraid of being replaced by AI” should they choose radiology as their specialisation [ 23 ]. Attitude towards the choice of specialisation being influenced by AI depended on where the person was viewing the problem from- as a student or as a specialist and also from the degree of familiarity they had with AI applications.
The majority of the students (91.4%) stated that they had not received any training on AI in medicine. The American Medical Association meeting of 2018 on Augmented Intelligence advocated for the training of physicians so that they could understand algorithms and work effectively with AI systems to make the best clinical care decisions for their patients [ 35 ]. Despite this, Paranjape et al. reported that training on the backend of electronic health record systems like, the quality of the data obtained, impact of computer use in front of patients, patient physician relationships etc. have not been addressed through medical education. If used with adequate training and understanding, AI will free up physicians’ time/ optimise a physician’s work hours, so that they can care and communicate with patients in the free time thus obtained. The findings of the research published by Jha et al. in the year 2022 agrees with this observation regarding inadequate coverage of AI and machine learning in medical curricula [ 36 ]. This deficiency leaves medical students underprepared to navigate the integration of AI technologies into their future practice. A significant percentage (37.6%) of respondents expressed concerns about job displacements due to AI, echoing sentiments observed in previous research. The concerns on AI induced loss of jobs particularly in fields like radiology and pathology, accentuate the importance of addressing misconceptions and fostering a meticulous understanding of AI’s role in healthcare. Jha et al’s study also highlights the importance of integrating soft skills, such as compassion and empathy, alongside AI education. Medical students must be equipped not only with technical AI competencies but also with the interpersonal skills necessary for holistic patient care. Collaborative efforts are needed to develop curricula that balance AI education with the cultivation of humanistic values, ensuring that future healthcare professionals can effectively navigate the intersection of technology and patient-centred care.
A major proportion of students in the study conducted by Sharma et al. demonstrated only a limited understanding of AI’s applications in medicine, primarily attributed to a lack of formal education, awareness, and interest. Interestingly, while a substantial portion (26.3%) of respondents demonstrated familiarity with AI, the majority (53.6%) exhibited only a superficial understanding of its applications in medicine [ 37 ]. This gap in knowledge highlights the need for enhanced educational initiatives to provide comprehensive insights into the potential of AI in healthcare delivery and patient outcomes. Concerns about the overreliance (49.2%) on AI and perceived lack of empathy (43.7%) were highlighted by a considerable proportion of students. These concerns underscore the importance of fostering a balanced approach to AI adoption in medical practice and education, ensuring that students are equipped to navigate the ethical challenges associated with AI integration.
Medical curriculum does not address mathematical concepts (to understand algorithms), the fundamentals of AI like data science, or the ethical and legal issues that can come up with the use of AI [ 27 ]. Only 26.8% of participants felt partially or completely competent to give information on AI to patients. Unless physicians have a foundational understanding of AI, or the methods to critically appraise AI, they will be at a loss when called to train medical students on the use of AI tools that assist in medical decision making. Consequently, medical students will be deficient in AI skills. Liaw et al. advocate for Quintuple Competencies for the use of AI in primary health care, one of which is the need to understand how to communicate with patients regarding the why and how of the use of AI tools, privacy and confidentiality questions that patients may raise during patient physician interactions, and understand the emotional, trust or patient satisfaction issues that may arise because of use of AI in health care [ 38 ].
More than half of the participants (51.1%) are unsure of being able to protect professional confidentiality of patients during the use of AI technologies. Direct providers of health care need to be aware of what precautions to take when sharing data with third parties who are not the direct care providers to the patients [ 16 ]. Artificial intelligence algorithms are derived from large data sets from human participants, and they may use data differently at different points in time. In such cases, patients can lose control of information they had consented to share especially where the impact on their privacy have not been adequately addressed [ 39 ]. However much regulations might be made to protect patient confidentiality and privacy of data, they might always fall behind AI advances, which means the human brain has to work consistently to remain ahead of the artificial intelligence it created. Guidelines set forth by reputable organisations such as the European Union’s “Guidelines for Trustworthy AI“ [ 40 ] and the World Health Organization’s “Ethics and Governance of Artificial Intelligence for Health” address critical ethical concerns in AI [ 41 ]. These core principles can be integrated into medical education to cultivate ethical awareness among medical students.
The perceptions of medical students on the possible influences of AI in medicine were evaluated through the questionnaire. The highest agreement was found on the question, whether they thought the use of AI ‘reduces error in medical practice’ (72.3%) while the lowest agreement was on the question AI ‘devalues the medical profession’ (40.3%).Students were mostly in favour of the use of AI in medicine because they felt that it would enable them as physicians to make more accurate decisions (72%) and facilitate patients’ access to healthcare (60.9%). Research by Topol et al. and Sharique et al. have shown that AI technologies can help reduce medical errors by improving data flow patterns and improving diagnostic accuracy [ 39 , 42 ]. The study from Western Australian students mentioned above [ 26 ] showed 74.4% of the participants agreeing that the use of AI would improve practice of medicine in general. It is encouraging to find that medical students in this research showed low agreement when asked if AI would devalue the medical profession and agreed that the use of AI would reduce medical errors caused inadvertently. It should also be noted that some research has shown that the inappropriate use of AI itself can introduce errors in medical practice [ 43 ].
On “disadvantages and risks of AI in medicine”, 69.2% of the students agreed that AI would reduce the humanistic aspect of the medical profession, 54.5% agreed that it can negatively affect the patient-physician relationship, 52.9% were concerned that using AI assisted applications could damage the trust patients placed on physicians, 59.4% agreed that AI would facilitate patient education, and 50.5% agreed that AI would allow the patient to increase their control over their own health. Hadithy et al. (2023) found that students believed AI technology was advantageous for improving overall health by personalising health care through analysing patient information [ 44 ].
Medical education in the 21st century is swiftly transitioning from the conventional approach of observing patients objectively from a distance and holding the belief that compassion is an innate skill to a contemporary paradigm. The new model emphasises the development of competencies such as doctor-patient relationships, communication skills, and professionalism. In modern medicine, AI is being viewed as an additional barrier between a patient and his physician. Machines have many advantages over humans as rightly observed by Wartman especially in view of not being affected by many of the human frailties like fatigue, information overload, inability to retain material beyond a limit etc. [ 24 ]. Scepticism over the use of AI in medical practice often stems from the lack of knowledge in this domain. Medical students, in many studies, opined that classes on artificial intelligence need to be included in syllabus, but only very few medical schools have included these in their medical curricula. Practising with compassion and empathy must be a learnt and cultivated skill along with artificial intelligence. The two should go together, taught in tandem throughout the medical course. Studies such as this have highlighted that students are open to being taught but are deficient in the skills and knowledge. There is a gap here that needs to be addressed. Man, and machine have to work as partners so as to improve the health of the people.
Limitations
Though this research was one of the first conducted in the state of Kerala and covered about 65% of medical students of the institution, which is more than other similar surveys conducted, there are a few limitations that have been identified. As an online survey method using Google Forms was implied for data collection, the voluntary nature of the participation from only those who were interested, might have introduced a self-selection bias and a non-response bias in this research. As this study only includes the responses from the medical students of one institution, it might not have captured a wide variety of responses. Hence the generalizability of the study may be limited. The questionnaire did not delve deep into how AI terms are understood, or how proficient students were with AI and so might have missed more relevant AI terms and concepts that students might be unfamiliar with. Most data collected in this study were quantitative so we might not have captured the depth of the students’ understanding or perceptions about AI. As many of the students had no exposure to computer science or had not attended AI classes, their perceptions might have been influenced by lack of exposure. Thus, the study might not have captured the views of those who had a more informed background on the subject.
Future studies are recommended to replicate and validate the findings in larger and more diverse populations to understand regional variations in knowledge, attitude, and perceptions among medical students. This study tool (questionnaire) was adopted from a parent study by Civaner M M [ 10 ], but the last question on the need for any other topic to be included was not met with enthusiasm.
This exploration into the perceptions of medical students regarding the integration of Artificial Intelligence (AI) into medical education reveals a nuanced landscape. The majority of participants in this study recognize the collaborative potential of AI, viewing it not as a replacement for physicians but as a valuable ally in healthcare. Interestingly, concerns on job displacement coexist with the optimism about improved decision-making and enhanced medical practice. The knowledge deficit in this context can extend an incompetence in communicating AI related information to patients, highlighting the urgent need for a holistic approach to medical education. The findings complement the perceived need of a proactive approach in preparing medical students for a future where AI plays a pivotal role in healthcare, ensuring that they not only embrace technological advancements but also uphold the humanistic values inherent to the practice of medicine.
Data availability
Data is provided as supplementary information files.
Abbreviations
Artificial Intelligence
Indian Institute of Technology
McCarthy J. What is artificial intelligence? [Internet]. Stanford.edu. [cited 2023 Jul 24]. https://www-formal.stanford.edu/jmc/whatisai.pdf .
Turing AM. Computing Machinery and Intelligence. Parsing the Turing Test. Dordrecht: Springer Netherlands; 2009;23–65.
Google Scholar
Rosenblatt F. The Perceptron-a perceiving and recognizing automaton. 1957.
Nobles AL, Leas EC, Caputi TL, Zhu SH, Strathdee SA, Ayers JW. Responses to addiction help-seeking from Alexa, Siri, Google Assistant, Cortana, and Bixby intelligent virtual assistants. NPJ Digit Med. 2020;3:11. https://doi.org/10.1038/s41746-019-0215-9 . PMID: 32025572; PMCID: PMC6989668.
Article Google Scholar
Research [Internet]. Openai.com. [cited 2023 Jul 24]. https://openai.com/research/overview .
Biswal A. Top 18 Artificial Intelligence (AI) applications in 2023 [Internet]. Simplilearn.com. Simplilearn; 2020 [cited 2023 Jul 24]. https://www.simplilearn.com/tutorials/artificial-intelligence-tutorial/artificial-intelligence-applications .
Michalski RS, Carbonell JG, Mitchell TM. Machine learning an artificial intelligence approach (volume I). Morgan Kaufmann; 1984.
Jimma BL. Artificial intelligence in healthcare: A bibliometric analysis. Telematics and Informatics Reports [Internet]. 2023;9(100041):100041. https://www.sciencedirect.com/science/article/pii/S2772503023000014 .
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94.
Civaner MM, Uncu Y, Bulut F, Chalil EG, Tatli A. Artificial intelligence in medical education: a cross-sectional needs assessment. BMC Med Educ. 2022;22(1):772.
Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA [Internet]. 2016 [cited 2023 Jul 24];316(22):2402–10. https://pubmed.ncbi.nlm.nih.gov/27898976/ .
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature [Internet]. 2017 [cited 2023 Jul 24];542(7639):115–8. https://www.nature.com/articles/nature21056 .
Ehteshami Bejnordi B, Veta M, van Johannes P, van Ginneken B, Karssemeijer N, Litjens G et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA [Internet]. 2017 [cited 2023 Jul 24];318(22):2199–210. https://doi.org/10.1001/jama.2017.14585 .
Yamashita R, Nishio M, Do RKG, Togashi K. Convolutional neural networks: an overview and application in radiology. Insights Imaging [Internet]. 2018;9(4):611–29. https://doi.org/10.1007/s13244-018-0639-9 .
Kreps GL, Neuhauser L. Artificial intelligence and immediacy: designing health communication to personally engage consumers and providers. Patient Educ Couns [Internet]. 2013;92(2):205–10. Available from:. https://www.sciencedirect.com/science/article/pii/S0738399113001729 .
Bali J, Garg R, Bali RT. Artificial intelligence (AI) in healthcare and biomedical research: Why a strong computational/AI bioethics framework is required? Indian J Ophthalmol [Internet]. 2019 [cited 2023 Jul 24];67(1):3–6. https://doi.org/10.4103/ijo.IJO_1292_18 .
Guo Y, Hao Z, Zhao S, Gong J, Yang F. Artificial intelligence in health care: Bibliometric analysis. J Med Internet Res [Internet]. 2020 [cited 2023 Jul 24];22(7):e18228. https://www.jmir.org/2020/7/e18228/ .
Becker A. Artificial intelligence in medicine: What is it doing for us today? Health Policy Technol [Internet]. 2019;8(2):198–205. https://www.sciencedirect.com/science/article/pii/S2211883718301758 .
WMA - The World Medical Association-WMA Statement on Augmented Intelligence. in Medical Care [Internet]. [cited 2023 Jul 17]. https://www.wma.net/policies-post/wma-statement-on-augmented-intelligence-in-medical-care/ .
Bisdas S, Topriceanu CC, Zakrzewska Z, Irimia AV, Shakallis L, Subhash J et al. Artificial Intelligence in Medicine: A Multinational Multi-Center Survey on the Medical and Dental Students’ Perception. Front Public Health [Internet]. 2021 [cited 2023 Jul 10];9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8739771/ .
Grunhut J, Wyatt AT, Marques O. Educating Future Physicians in Artificial Intelligence (AI): an integrative review and proposed changes. J Med Educ Curric Dev. 2021;8:23821205211036836.
Artificial intelligence in medical applications and ethical problems: knowledge and thoughts of medical students Survey form used in: Civaner MM, Uncu Y, Bulut F, Chalil EG, Tatlı A. Artificial intelligence in medical education: a cross-sectional needs assessment. BMC Medical Education. 2022;22(1):772. [email protected].
Pinto Dos Santos D, Giese D, Brodehl S, Chon SH, Staab W, Kleinert R, Maintz D, Baeßler B. Medical students’ attitude towards artificial intelligence: a multicentre survey. Eur Radiol. 2019;29(4):1640–6. https://doi.org/10.1007/s00330-018-5601-1 . Epub 2018 Jul 6. PMID: 29980928.
Wartman SA, Combs CD. Medical Education Must Move From the Information Age to the Age of Artificial Intelligence. Acad Med. 2018;93(8):1107–1109. https://doi.org/10.1097/ACM.0000000000002044 . PMID: 29095704.
Wartman SA, Medicine, Machines. and Medical Education. Acad Med. 2021;96(7):947–950. https://doi.org/10.1097/ACM.0000000000004113 . PMID: 33788788.
Stewart J, Lu J, Gahungu N, Goudie A, Fegan PG, Bennamoun M, et al. Western Australian medical students’ attitudes towards artificial intelligence in healthcare. PLoS ONE. 2023;18(8):e0290642. https://doi.org/10.1371/journal.pone.0290642 .
Fabien Lareyre Cédric, Adam M, Carrier N, Chakfé. Juliette Raffort.Artificial Intelligence for Education of Vascular Surgeons.European Journal of Vascular and Endovascular Surgery,Volume 59, Issue 6,2020,Pages 870–871, https://doi.org/10.1016/j.ejvs.2020.02.030 .(https://www.sciencedirect.com/science/article/pii/S1078588420301659 ).
Paranjape K, Schinkel M, Nannan Panday R, CAr J, Nanayakkara P. Introducing artificial intelligence training in medical education. JMIR Med Educ. 2019;5:e16048.
Srivastava TK, Waghmere L, Mar. Vol. -14(3): JI01–2.
Park SH, Do KH, Kim S, Park JH, Lim YS. What should medical students know about artificial intelligence in medicine? J Educ Eval Health Prof. 2019;16:18. https://doi.org/10.3352/jeehp.2019.16.18 . Epub 2019 Jul 3. PMID: 31319450; PMCID: PMC6639123.
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18(8):500.
Sit C, Srinivasan R, Amlani A, Muthuswamy K, Azam A, Monzon L et al. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging [Internet]. 2020 Dec [cited 2023 Jul 10];11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7002761/ .
Gong B, Nugent JP, Guest W, Parker W, Chang PJ, Khosa F, Nicolaou S. Influence of Artificial Intelligence on Canadian Medical Students’ Preference for Radiology Specialty: ANational Survey Study. Acad Radiol. 2019;26(4):566–577. https://doi.org/10.1016/j.acra.2018.10.007 . Epub 2018 Nov 11. PMID: 30424998.
Yurdaisik I, Aksoy SH. Evaluation of knowledge and attitudes of radiology department workers about artificial intelligence. Ann Clin Anal Med. 2021;12:186–90. https://doi.org/10.4328/ACAM.20453 .
Augmented Intelligence in Health Care. AMA AI, Board Report. 2018. https://www.ama-assn.org/system/files/2019-08/ai-2018-board-report.pdf .
Jha N, Shankar PR, Al-Betar MA, Mukhia R, Hada K, Palaian S. Undergraduate medical students’ and interns’ knowledge and perception of artificial intelligence in medicine. Adv Med Educ Pract [Internet]. 2022 [cited 2024 Mar 25];13:927–37. https://doi.org/10.2147/amep.s368519 .
Vipul Sharma U, Saini V, Pareek L, Sharma. Susheel Kumar. Artificial Intelligence (AI) integration in Medical Education: a Pan-india Cross-sectional Observation of Acceptance and understanding among students. Scripta Med. 2023;55:343–52.
Liaw W, Kueper JK, Lin S, Bazemore A, Kakadiaris I. Competencies for the Use of Artificial Intelligence in Primary Care. Ann Fam Med. 2022 Nov-Dec;20(6):559–63. https://doi.org/10.1370/afm.2887 . PMID: 36443071; PMCID: PMC9705044.
Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. 2021;22:122. https://doi.org/10.1186/s12910-021-00687-3 .
Cannarsa M. Ethics guidelines for trustworthy AI. The Cambridge Handbook of lawyering in the Digital Age. Cambridge University Press; 2021. pp. 283–97.
Ethics and governance of artificial intelligence for health [Internet]. Who.int. World Health Organization; 2021 [cited 2024 Mar 25]. https://www.who.int/publications/i/item/9789240029200 .
Sharique Ahmad & Saeeda Wasim. Prevent medical errors through Artificial Intelligence: a review. Saudi J Med Pharm Sci. 2023;9(7):419–23.
Choudhury A, Asan O. Role of Artificial Intelligence in Patient Safety outcomes: systematic literature review. JMIR Med Inf. 2020;8(7):e18599. https://doi.org/10.2196/18599 . PMID: 32706688; PMCID: PMC7414411.
Al Hadithy ZA, Al Lawati A, Al-Zadjali R, Al Sinawi H. Knowledge, attitudes, and perceptions of Artificial Intelligence in Healthcare among Medical students at Sultan Qaboos University. Cureus. 2023;15(9):e44887. https://doi.org/10.7759/cureus.44887 . PMID: 37814766; PMCID: PMC10560391.
Download references
Acknowledgements
Dr. Civaner and team - for providing us with the questionnaire that we used for this research and being available to answer any questions we had.Dr. Rosin George Varghese and Dr. Joe Abraham- for reviewing the protocol of the research and suggesting corrections. Dr. Felix Johns- the Head of the department of Community Medicine for his support during the project.
There has been no funding provided for this research or publication so far.
Author information
Authors and affiliations.
Pushpagiri Medical College, Tiruvalla, Kerala, India
Preetha Jackson, Gayathri Ponath Sukumaran, Chikku Babu, M. Christa Tony, Deen Stephano Jack, V. R. Reshma, Dency Davis, Nisha Kurian & Anjum John
You can also search for this author in PubMed Google Scholar
Contributions
P.J. - Design, acquisition, analysis, interpretation of data, drafting of the work and revisions.G.P.S.- Acquisition, analysis, interpretation of data, substantially revising the work.D.D- Acquisition, interpretation of data, substantially revising the work. C.B., C.T.M, & D.S.J.- acquisition, and reading through manuscript during final revision.R.V.R- Analysis, Interpretation of data, reading through manuscript and substantial revisions.N.K- Substantially revising the work.A.J- Conception, design, acquisition, drafting of the work and substantially contributing to revisions. All authors reviewed the final manuscript.
Corresponding author
Correspondence to Anjum John .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval of the study was obtained from the Institutional Ethics Committee of Pushpagiri Institute of Medical Sciences and Research Centre (Dated: 29 June 2023 No. PIMSRC /E1/388A/72/2023).
Informed consent
Informed consent to participate was obtained from each participant through Google Forms after information about the study was provided.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jackson, P., Ponath Sukumaran, G., Babu, C. et al. Artificial intelligence in medical education - perception among medical students . BMC Med Educ 24 , 804 (2024). https://doi.org/10.1186/s12909-024-05760-0
Download citation
Received : 04 January 2024
Accepted : 09 July 2024
Published : 27 July 2024
DOI : https://doi.org/10.1186/s12909-024-05760-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Medical curriculum
- Medical ethics
- Medical education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
More From Forbes
AI In Healthcare: Revolutionizing Medicine Or Overhyped Promise?
- Share to Facebook
- Share to Twitter
- Share to Linkedin
AI is going to change healthcare forever. In the near future, we can look forward to revolutionary new cures and treatments, personalized medicine, and a new generation of hospitals and facilities where super-smart robots take care of everything from cleaning to brain surgery .
At least – so we’re told . Now, I’m a believer in the power of AI to change the world for the better. But I can also plainly see that there’s a lot of hype around it. Technology companies stand to make trillions from selling it, and they all want us to believe their models and algorithms are the ones that will change the world.
In a world that’s quickly becoming flooded with AI washing , it’s critical that we learn how to cut through the hype and marketing bluster. So here I’ll take a look at how well one of the most frequent claims – that it will transform the fields of healthcare, medicine and wellbeing – stands up to scrutiny.
Where Are We Today?
So far, attempts to improve research and delivery of healthcare using AI have provided some encouraging success stories, as well as some clear examples of over-exaggerated expectations.
In drug and vaccine discovery, for example, it accelerated the discovery of mRNA vaccines for COVID-19. The same technology is now being used to create new protections against many other diseases . And generative AI built on similar technology to ChatGPT has also been used to create new immunotherapy drugs .
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
It has been used to analyze and interpret medical scans, images, medical records and tissue samples, and has been shown to be able to spot signs of diseases such as cancer and Alzheimer’s disease .
According to the American College Of Surgeons, “Most research shows that scan interpretation from AI is more robust and accurate than those from radiologists, often picking up small, rare spots in the images.”
It can shorten the length of time we need to stay in hospital, with one study of patients diagnosed with pulmonary embolism finding that those triaged with AI tools were able to return home an average of two days earlier.
The use of chatbots to answer patient questions or assist with the training of clinical staff, as well as analytics tools to help hospitals plan their use of resources more efficiently, all promise to streamline delivery and ultimately improve outcomes.
However, that isn’t to say that there haven’t also been missteps and over-inflated claims, particularly in the early days. In 2017, a partnership between IBM and MD Anderson Cancer Center was discontinued after it was found that the Watson Health system’s decision-making wasn’t accurate enough, creating a “credibility gap” with physicians.
In 2002, a study of online symptom-checker and self-diagnosis tools, some of which involve using AI to provide self-triage, found that “overall, the diagnostic and triage accuracy of symptom checkers are variable and of low accuracy … this study demonstrates that reliance upon symptom checkers could pose significant patient safety hazards.”
It should also be noted that despite the fact that many hospitals and healthcare providers are exploring the use of AI systems for creating efficiencies in administerial, record-keeping and staffing processes, it’s hard to find evidence that this has yet led to significant cost savings or improvements in patient care.
What Are The Experts Saying?
If we look beyond the words of marketers and the CEOs of big tech companies, opinions vary on the value that AI has – or will – bring to the field of healthcare.
Geneticist and cardiologist Dr Eric Topol, author of Deep Medicine , says that while AI will probably never replace a thorough physical examination by an experienced doctor, many applications are already proving highly valuable. These include self-administered kits that test for urinary tract infections and analyze lung problems from the sound of a cough.
In the future, he believes , mobile phones are likely to provide inexpensive ultrasound scans, and recognize early warning signs of diabetes from a picture of the retina.
Perhaps most valuable of all, he suggests, will be the ability of AI to restore the “ human element ” to medicine. By handling routine tasks, AI will free up doctors to spend more face-to-face time with patients, enabling them to develop a better understanding of their condition.
This is a position echoed by Dr Fei-Fei Li, director of Stanford University’s Institute for Human-Centered AI, who says “We’re seeing the medical profession using AI technology … [doctors] tell me that medical summaries are very painful … they take away from patients. Now you can get a language model to help.”
However an article in MIT Technology review presents a more cautionary outlook. Tools designed to diagnose disease or predict outbreaks could be trained on limited or biased data – for example, research has shown that some tools are less effective with female patients simply because less women take part in medical studies.
And Dr. Robert Glatter, assistant professor of emergency medicine at the Zucker School of Medicine, together with Dr. Peter Papadakos, professor of anesthesiology and surgery at the University of Rochester Medical Center, in their article No AI Can Ever Learn The Art Of Medicine , argue “Even with the advent and ongoing evolution of AI … empathy is best learned and communicated in the form of bedside teaching by humans – not AI or chatbots.”
The Verdict – Hype Or Reality?
While AI has undoubtedly already made significant impacts and seems likely to become more valuable as we move forward, it’s unlikely to be the literal panacea that will cure all of our ills.
However, we’re in the very early days of the AI revolution, and successes in fields such as drug discovery and detection of early warning signals clearly demonstrate that the potential to improve care and outcomes is real.
Challenges – particularly around data privacy, implementation costs and training of healthcare professionals in its use – will need to be overcome before the most optimistic predictions become viable.
As in other fields, professionals agree that its most valuable applications will involve augmenting rather than replacing human skills, experience and expertise.
For the technology companies building tools, keeping this firmly in mind while developing the next generation of AI-enhanced medical applications will be key to driving real change that will benefit us all.
- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 2, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Growing use of AI in health care reveals the need for global sustainability initiatives
by Osaka Metropolitan University

Similar to other sectors around the world, the light speed development of artificial intelligence (AI) has made its way into health care, particularly the radiology field. As such, AI-based diagnostic systems are flourishing, with hospitals quickly adopting the technology to assist radiologists. In contrast, there are concerns about the environmental impact of increasingly complex AI models and the need for more sustainable AI solutions.
Therefore, Associate Professor Daiju Ueda of Osaka Metropolitan University's Graduate School of Medicine, a member of the Japan Radiological Society, led a research team in the investigation of the environmental costs of AI. The results were published in Diagnostic and Interventional Imaging .
In this research review, head members of the Japan Radiological Society and medical field researchers discussed the energy consumption of AI systems in the medical field, carbon emissions from data centers , and electronic waste issues.
Specific solutions to mitigate these environmental impacts were discussed, including the development of energy-efficient AI models, the implementation of green computing, and the use of renewable energy.
In addition, the review proposes measures for the sustainable deployment of AI in the medical field. These are important guidelines for medical institutions, policymakers, and AI developers to operate AI systems in an environmentally responsible manner.
"AI has the potential to improve the quality of health care , but at the same time its environmental impact cannot be ignored. The best practices we have recommended are the first steps toward balancing these two factors," stated Professor Ueda.
"The challenge for the future will be to verify and further elaborate these recommendations in actual medical practice. They are also expected to contribute to the standardization of methods for assessing AI's environmental impact and the development of an international regulatory framework."
Explore further
Feedback to editors

Interplay of sex, marital status, education, race linked to 18 year US lifespan gap

Hospital pneumonia diagnoses are uncertain, revised more than half the time, study finds
3 hours ago

EMS training on key skills improves heart attack survival
4 hours ago

Effective mental health care takes varying forms, says new study

New biomaterial regrows damaged cartilage in joints
5 hours ago

A new drug could turn back the clock on multiple sclerosis

New method tracks how psychedelics affect neurons in minutes

Botanicals like turmeric, green tea are harming Americans' livers
7 hours ago

In law enforcement, a survey finds a link between head injuries and depression, PTSD
8 hours ago

Study finds omega-3 supplements reduce genetic risk of high total cholesterol, LDL and triglyceride levels
Related stories.

Researchers look at environmental impacts of AI tools in radiology
Feb 27, 2024

Highly accurate AI model can estimate lung function just by using chest X-rays
Jul 8, 2024

Examining the status and prospects of complex network modeling for energy and carbon emission systems
Jun 20, 2024

Inclusivity needed in patient radiology information systems, review suggests
Jul 19, 2024

Reaching new heights: AI can help us build better buildings
Jun 25, 2024

Experts outline considerations to deploy AI in radiology
Jul 24, 2024
Recommended for you

Researchers explore generative AI benefits and shortfalls in medical education
10 hours ago

ChatGPT still not very good at diagnosing human ailments
Aug 1, 2024

Generation X, millennials in US have higher risk of developing 17 cancers compared to older generations
Jul 31, 2024

Study evaluates AI that creates cardiology reports for patients
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Clinical Research
- Interventional
- Radiation Oncology
- Women's
- Artificial Intelligence
- Enterprise Imaging
- Imaging Informatics
- Informatics
- Compensation
- Education & Training
- Patient Care
- Policy & Regulations
- Practice Management
- Professional Associations
- Experience Stories
- Webinars & Videos
Search form
1 day of training with ai makes novice sonographers as accurate as experts in gestational measurements.

As the pregnancy advances, the embryo is easier to see, and accurate measurements can be obtained with transabdominal ultrasound. A crown-rump length (CRL) measurement. This ultrasound scan shows the CRL, which is the average of discrete fetal measurements from the tip of the head end to the tip of the rump end in the midsagittal plane of the embryo. This is highly accurate for pregnancy dating. Images courtesy of RSNA
An ultrasound probe integrated with artificial intelligence enables novice clinicians to measure gestational age with accuracy comparable to expert sonographers.
This sort of tool could be a game changer for prenatal care in low resource settings, authors of a new paper published in JAMA suggest.
“The World Health Organization recommends that all pregnant people receive at least one ultrasonography examination prior to 24 weeks. Although this policy recommendation remains largely aspirational in many low- and middle-income countries, recent advances in ultrasonography hardware and artificial intelligence–enabled medical image analysis could facilitate broader access to this critical diagnostic tool," Jeffrey S. A. Stringer, MD, with the UNC School of Medicine in North Carolina, and colleagues write.
The deep learning model is integrated directly into ultrasonography device software that runs on an Android tablet computer. It enables image processing and feature extraction to occur in real time on the local device, allowing providers to immediately make clinical determinations.
Researchers recently tested the AI device on a group of 400 women in Chapel Hill, North Carolina and Lusaka, Zambia who were in their first trimester of pregnancy. To determine whether the tool could provide accurate gestational age (GA) measurements when in the hands of individuals less experienced with conducting prenatal ultrasound exams, researchers had expert sonographers establish ground truth GA for all study participants via transvaginal ultrasound. During follow-up visits throughout gestation (between 14 and 27 weeks), novice users measured GA themselves (after just a single day of training) by conducting blind sweeps of the patients’ abdomen using the AI-enabled device.
Accuracy was measured based on the mean absolute error (MAE) of users’ estimation of GA, which was considered equivalent if it fell within ±2 days of the ground truth.
With the AI device, novice users yielded a MAE of 3.2 (0.1) days vs 3 (0.1) days for the sonographers. Just over 90% of the AI assessments fell within seven days of the ground truth—just shy of the 92.5% achieved by sonographers. AI's performance was consistent for patients in both locations and among patients with a higher body mass index.
Given the tool’s accuracy and ease of use, it could provide much needed access to accurate GA measurements in areas with fewer healthcare resources, the group suggests.
“The deep learning model was incorporated directly into the ultrasonography device software, which runs on an Android tablet computer, allowing image processing, feature extraction, and inference to occur in real time on the local device, facilitating immediate clinical decision-making,” the authors explain, later adding that their findings “have immediate implications for obstetrical care in low-resource settings.”
Similar AI systems could be utilized in low-resource settings to further advance the World Health Organization’s goal of providing accurate GA measurements for all pregnant people, the experts said.
The study abstract is available here .
Multimodal AI model helps differentiate between benign and malignant pancreatic lesions
Could focused ultrasound help rewire the brain to be more present research suggests it's a possibility, how does ai ti-rads compare to other thyroid nodule risk stratification systems.

In addition to her background in journalism, Hannah also has patient-facing experience in clinical settings, having spent more than 12 years working as a registered rad tech. She joined Innovate Healthcare in 2021 and has since put her unique expertise to use in her editorial role with Health Imaging.
Related Content
To revisit this article, visit My Profile, then View saved stories .
- The Big Story
- Newsletters
- Steven Levy's Plaintext Column
- WIRED Classics from the Archive
- WIRED Insider
- WIRED Consulting
Here’s What Happens When You Give People Free Money

OpenAI CEO Sam Altman’s decade-in-the-making effort to understand how handing out free money affects recipients and the broader economy delivered its first big results Monday. OpenResearch found that when it gave some of the poorest Americans $1,000 a month for three years with no strings attached, they put much of the money toward basic needs such as food, housing, and transportation. But what amounted to $36,000 wasn’t enough to significantly improve their physical well-being or long-term financial health, researchers concluded.
The initial results from what OpenResearch, an Altman-funded research lab , describes as the most comprehensive study on “unconditional cash” show that while the grants had their benefits and weren’t spent on items such as drugs and alcohol, they were hardly a panacea for treating some of the biggest concerns about income inequality and the prospect of AI and other automation technologies taking jobs .
Some progressive organizations in the US and elsewhere have advocated for fighting poverty through forms of unconditional cash such as universal basic income . Conservative groups have largely panned the projects as handouts for undeserving people who refuse to work. In two papers published on Monday and a third coming next month, OpenResearch staff and its university collaborators offer data that could help fuel the full spectrum of views.
OpenResearch, which has also drawn funding from organizations like OpenAI and the US government, handed out the unconditional $1,000 transfers from November 2020 to October 2023. The cash provided a 40 percent income boost to a diverse group of 1,000 people ages 21 to 40 who started out in households earning about $30,000 annually across 10 counties apiece in Illinois and Texas. As a control group, 2,000 people with similar characteristics received $50 a month. Participants answered surveys, shared credit reports, and took blood tests.
The perceived benefits for those who received $1,000 monthly varied across facets of life. Their biggest jump in spending involved giving an average of $22 more per month to others, such as helping out relatives in need or gifts to friends. People started seeking out more health care such as dental braces, and started better stocking their refrigerators and pantries.
Some began considering or pursuing startups. By year three of the payments, “Black recipients were 9 percentage points more likely to report starting or helping to start a business than control participants, and women were 5 percentage points more likely,” according to one of the studies.
Participants also moved out on their own, especially those who started out at the lowest incomes, and enjoyed themselves more. The forthcoming paper, of which OpenResearch shared a draft version with WIRED, estimates that roughly 81 cents of each dollar transferred went to higher spending on items such as housing, 22 cents went to leisure, and negative 3 cents went to increased borrowing as recipients took on more car loans and mortgages.
The increased debt brought down participants’ net worth over the three years. Combined with little change in credit access, bankruptcies, and foreclosures, researchers concluded that “the transfer did not improve participant’s long-run financial position.” People did put more money into savings and initially felt better about their financial situation. But they also slightly cut back on work and let the free cash fill in the gap. For every $1 received from OpenResearch, participants’ earnings excluding the free money dropped by at least 12 cents and total household income fell by at least 21 cents.
“Cash offers flexibility and may increase agency to make employment decisions that align with recipients’ individual circumstances, goals, and values,” the researchers wrote. They may be “taking more time to find a job, taking a lower paying position that they find more meaningful, or simply taking a break.”
What critics of assistance programs fear, though, is that instead of investing in the future, people eventually give up on working completely and become ever more reliant on support. OpenResearch found “the total amount of work withdrawn from the market” was “fairly substantial” in its experiment.
Adding the fact that researchers found “no effect” from the cash on several measures of physical health and welfare, and critics may have plenty to snarl at. But the studies’ authors say it’s important not to forget that participants showed with their spending what they valued most. “Policymakers should take into account the fact that recipients have demonstrated—by their own choices—that time away from work is something they prize highly,” authors wrote. If anything OpenResearch has proved true the adage: Money can buy time.

You Might Also Like …
Politics Lab: Get the newsletter and listen to the podcast
What happens when you give people free money
Not everyone loses weight on Ozempic
The Pentagon wants to spend $141 billion on a doomsday machine
Event: Join us for the Energy Tech Summit on October 10 in Berlin

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Future Healthc J
- v.6(2); 2019 Jun

The potential for artificial intelligence in healthcare
Thomas davenport.
A Babson College, Wellesley, USA
Ravi Kalakota
B Deloitte Consulting, New York, USA
The complexity and rise of data in healthcare means that artificial intelligence (AI) will increasingly be applied within the field. Several types of AI are already being employed by payers and providers of care, and life sciences companies. The key categories of applications involve diagnosis and treatment recommendations, patient engagement and adherence, and administrative activities. Although there are many instances in which AI can perform healthcare tasks as well or better than humans, implementation factors will prevent large-scale automation of healthcare professional jobs for a considerable period. Ethical issues in the application of AI to healthcare are also discussed.
Introduction
Artificial intelligence (AI) and related technologies are increasingly prevalent in business and society, and are beginning to be applied to healthcare. These technologies have the potential to transform many aspects of patient care, as well as administrative processes within provider, payer and pharmaceutical organisations.
There are already a number of research studies suggesting that AI can perform as well as or better than humans at key healthcare tasks, such as diagnosing disease. Today, algorithms are already outperforming radiologists at spotting malignant tumours, and guiding researchers in how to construct cohorts for costly clinical trials. However, for a variety of reasons, we believe that it will be many years before AI replaces humans for broad medical process domains. In this article, we describe both the potential that AI offers to automate aspects of care and some of the barriers to rapid implementation of AI in healthcare.
Types of AI of relevance to healthcare
Artificial intelligence is not one technology, but rather a collection of them. Most of these technologies have immediate relevance to the healthcare field, but the specific processes and tasks they support vary widely. Some particular AI technologies of high importance to healthcare are defined and described below.
Machine learning – neural networks and deep learning
Machine learning is a statistical technique for fitting models to data and to ‘learn’ by training models with data. Machine learning is one of the most common forms of AI; in a 2018 Deloitte survey of 1,100 US managers whose organisations were already pursuing AI, 63% of companies surveyed were employing machine learning in their businesses. 1 It is a broad technique at the core of many approaches to AI and there are many versions of it.
In healthcare, the most common application of traditional machine learning is precision medicine – predicting what treatment protocols are likely to succeed on a patient based on various patient attributes and the treatment context. 2 The great majority of machine learning and precision medicine applications require a training dataset for which the outcome variable (eg onset of disease) is known; this is called supervised learning.
A more complex form of machine learning is the neural network – a technology that has been available since the 1960s has been well established in healthcare research for several decades 3 and has been used for categorisation applications like determining whether a patient will acquire a particular disease. It views problems in terms of inputs, outputs and weights of variables or ‘features’ that associate inputs with outputs. It has been likened to the way that neurons process signals, but the analogy to the brain's function is relatively weak.
The most complex forms of machine learning involve deep learning , or neural network models with many levels of features or variables that predict outcomes. There may be thousands of hidden features in such models, which are uncovered by the faster processing of today's graphics processing units and cloud architectures. A common application of deep learning in healthcare is recognition of potentially cancerous lesions in radiology images. 4 Deep learning is increasingly being applied to radiomics, or the detection of clinically relevant features in imaging data beyond what can be perceived by the human eye. 5 Both radiomics and deep learning are most commonly found in oncology-oriented image analysis. Their combination appears to promise greater accuracy in diagnosis than the previous generation of automated tools for image analysis, known as computer-aided detection or CAD.
Deep learning is also increasingly used for speech recognition and, as such, is a form of natural language processing (NLP), described below. Unlike earlier forms of statistical analysis, each feature in a deep learning model typically has little meaning to a human observer. As a result, the explanation of the model's outcomes may be very difficult or impossible to interpret.
Natural language processing
Making sense of human language has been a goal of AI researchers since the 1950s. This field, NLP, includes applications such as speech recognition, text analysis, translation and other goals related to language. There are two basic approaches to it: statistical and semantic NLP. Statistical NLP is based on machine learning (deep learning neural networks in particular) and has contributed to a recent increase in accuracy of recognition. It requires a large ‘corpus’ or body of language from which to learn.
In healthcare, the dominant applications of NLP involve the creation, understanding and classification of clinical documentation and published research. NLP systems can analyse unstructured clinical notes on patients, prepare reports (eg on radiology examinations), transcribe patient interactions and conduct conversational AI.
Rule-based expert systems
Expert systems based on collections of ‘if-then’ rules were the dominant technology for AI in the 1980s and were widely used commercially in that and later periods. In healthcare, they were widely employed for ‘clinical decision support’ purposes over the last couple of decades 5 and are still in wide use today. Many electronic health record (EHR) providers furnish a set of rules with their systems today.
Expert systems require human experts and knowledge engineers to construct a series of rules in a particular knowledge domain. They work well up to a point and are easy to understand. However, when the number of rules is large (usually over several thousand) and the rules begin to conflict with each other, they tend to break down. Moreover, if the knowledge domain changes, changing the rules can be difficult and time-consuming. They are slowly being replaced in healthcare by more approaches based on data and machine learning algorithms.
Physical robots
Physical robots are well known by this point, given that more than 200,000 industrial robots are installed each year around the world. They perform pre-defined tasks like lifting, repositioning, welding or assembling objects in places like factories and warehouses, and delivering supplies in hospitals. More recently, robots have become more collaborative with humans and are more easily trained by moving them through a desired task. They are also becoming more intelligent, as other AI capabilities are being embedded in their ‘brains’ (really their operating systems). Over time, it seems likely that the same improvements in intelligence that we've seen in other areas of AI would be incorporated into physical robots.
Surgical robots, initially approved in the USA in 2000, provide ‘superpowers’ to surgeons, improving their ability to see, create precise and minimally invasive incisions, stitch wounds and so forth. 6 Important decisions are still made by human surgeons, however. Common surgical procedures using robotic surgery include gynaecologic surgery, prostate surgery and head and neck surgery.
Robotic process automation
This technology performs structured digital tasks for administrative purposes, ie those involving information systems, as if they were a human user following a script or rules. Compared to other forms of AI they are inexpensive, easy to program and transparent in their actions. Robotic process automation (RPA) doesn't really involve robots – only computer programs on servers. It relies on a combination of workflow, business rules and ‘presentation layer’ integration with information systems to act like a semi-intelligent user of the systems. In healthcare, they are used for repetitive tasks like prior authorisation, updating patient records or billing. When combined with other technologies like image recognition, they can be used to extract data from, for example, faxed images in order to input it into transactional systems. 7
We've described these technologies as individual ones, but increasingly they are being combined and integrated; robots are getting AI-based ‘brains’, image recognition is being integrated with RPA. Perhaps in the future these technologies will be so intermingled that composite solutions will be more likely or feasible.
Diagnosis and treatment applications
Diagnosis and treatment of disease has been a focus of AI since at least the 1970s, when MYCIN was developed at Stanford for diagnosing blood-borne bacterial infections. 8 This and other early rule-based systems showed promise for accurately diagnosing and treating disease, but were not adopted for clinical practice. They were not substantially better than human diagnosticians, and they were poorly integrated with clinician workflows and medical record systems.
More recently, IBM's Watson has received considerable attention in the media for its focus on precision medicine, particularly cancer diagnosis and treatment. Watson employs a combination of machine learning and NLP capabilities. However, early enthusiasm for this application of the technology has faded as customers realised the difficulty of teaching Watson how to address particular types of cancer 9 and of integrating Watson into care processes and systems. 10 Watson is not a single product but a set of ‘cognitive services’ provided through application programming interfaces (APIs), including speech and language, vision, and machine learning-based data-analysis programs. Most observers feel that the Watson APIs are technically capable, but taking on cancer treatment was an overly ambitious objective. Watson and other proprietary programs have also suffered from competition with free ‘open source’ programs provided by some vendors, such as Google's TensorFlow.
Implementation issues with AI bedevil many healthcare organisations. Although rule-based systems incorporated within EHR systems are widely used, including at the NHS, 11 they lack the precision of more algorithmic systems based on machine learning. These rule-based clinical decision support systems are difficult to maintain as medical knowledge changes and are often not able to handle the explosion of data and knowledge based on genomic, proteomic, metabolic and other ‘omic-based’ approaches to care.
This situation is beginning to change, but it is mostly present in research labs and in tech firms, rather than in clinical practice. Scarcely a week goes by without a research lab claiming that it has developed an approach to using AI or big data to diagnose and treat a disease with equal or greater accuracy than human clinicians. Many of these findings are based on radiological image analysis, 12 though some involve other types of images such as retinal scanning 13 or genomic-based precision medicine. 14 Since these types of findings are based on statistically-based machine learning models, they are ushering in an era of evidence- and probability-based medicine, which is generally regarded as positive but brings with it many challenges in medical ethics and patient/clinician relationships. 15
Tech firms and startups are also working assiduously on the same issues. Google, for example, is collaborating with health delivery networks to build prediction models from big data to warn clinicians of high-risk conditions, such as sepsis and heart failure. 16 Google, Enlitic and a variety of other startups are developing AI-derived image interpretation algorithms. Jvion offers a ‘clinical success machine’ that identifies the patients most at risk as well as those most likely to respond to treatment protocols. Each of these could provide decision support to clinicians seeking to find the best diagnosis and treatment for patients.
There are also several firms that focus specifically on diagnosis and treatment recommendations for certain cancers based on their genetic profiles. Since many cancers have a genetic basis, human clinicians have found it increasingly complex to understand all genetic variants of cancer and their response to new drugs and protocols. Firms like Foundation Medicine and Flatiron Health, both now owned by Roche, specialise in this approach.
Both providers and payers for care are also using ‘population health’ machine learning models to predict populations at risk of particular diseases 17 or accidents 18 or to predict hospital readmission. 19 These models can be effective at prediction, although they sometimes lack all the relevant data that might add predictive capability, such as patient socio-economic status.
But whether rules-based or algorithmic in nature, AI-based diagnosis and treatment recommendations are sometimes challenging to embed in clinical workflows and EHR systems. Such integration issues have probably been a greater barrier to broad implementation of AI than any inability to provide accurate and effective recommendations; and many AI-based capabilities for diagnosis and treatment from tech firms are standalone in nature or address only a single aspect of care. Some EHR vendors have begun to embed limited AI functions (beyond rule-based clinical decision support) into their offerings, 20 but these are in the early stages. Providers will either have to undertake substantial integration projects themselves or wait until EHR vendors add more AI capabilities.
Patient engagement and adherence applications
Patient engagement and adherence has long been seen as the ‘last mile’ problem of healthcare – the final barrier between ineffective and good health outcomes. The more patients proactively participate in their own well-being and care, the better the outcomes – utilisation, financial outcomes and member experience. These factors are increasingly being addressed by big data and AI.
Providers and hospitals often use their clinical expertise to develop a plan of care that they know will improve a chronic or acute patient's health. However, that often doesn't matter if the patient fails to make the behavioural adjustment necessary, eg losing weight, scheduling a follow-up visit, filling prescriptions or complying with a treatment plan. Noncompliance – when a patient does not follow a course of treatment or take the prescribed drugs as recommended – is a major problem.
In a survey of more than 300 clinical leaders and healthcare executives, more than 70% of the respondents reported having less than 50% of their patients highly engaged and 42% of respondents said less than 25% of their patients were highly engaged. 21
If deeper involvement by patients results in better health outcomes, can AI-based capabilities be effective in personalising and contextualising care? There is growing emphasis on using machine learning and business rules engines to drive nuanced interventions along the care continuum. 22 Messaging alerts and relevant, targeted content that provoke actions at moments that matter is a promising field in research.
Another growing focus in healthcare is on effectively designing the ‘choice architecture’ to nudge patient behaviour in a more anticipatory way based on real-world evidence. Through information provided by provider EHR systems, biosensors, watches, smartphones, conversational interfaces and other instrumentation, software can tailor recommendations by comparing patient data to other effective treatment pathways for similar cohorts. The recommendations can be provided to providers, patients, nurses, call-centre agents or care delivery coordinators.
Administrative applications
There are also a great many administrative applications in healthcare. The use of AI is somewhat less potentially revolutionary in this domain as compared to patient care, but it can provide substantial efficiencies. These are needed in healthcare because, for example, the average US nurse spends 25% of work time on regulatory and administrative activities. 23 The technology that is most likely to be relevant to this objective is RPA. It can be used for a variety of applications in healthcare, including claims processing, clinical documentation, revenue cycle management and medical records management. 24
Some healthcare organisations have also experimented with chatbots for patient interaction, mental health and wellness, and telehealth. These NLP-based applications may be useful for simple transactions like refilling prescriptions or making appointments. However, in a survey of 500 US users of the top five chatbots used in healthcare, patients expressed concern about revealing confidential information, discussing complex health conditions and poor usability. 25
Another AI technology with relevance to claims and payment administration is machine learning, which can be used for probabilistic matching of data across different databases. Insurers have a duty to verify whether the millions of claims are correct. Reliably identifying, analysing and correcting coding issues and incorrect claims saves all stakeholders – health insurers, governments and providers alike – a great deal of time, money and effort. Incorrect claims that slip through the cracks constitute significant financial potential waiting to be unlocked through data-matching and claims audits.
Implications for the healthcare workforce
There has been considerable attention to the concern that AI will lead to automation of jobs and substantial displacement of the workforce. A Deloitte collaboration with the Oxford Martin Institute 26 suggested that 35% of UK jobs could be automated out of existence by AI over the next 10 to 20 years. Other studies have suggested that while some automation of jobs is possible, a variety of external factors other than technology could limit job loss, including the cost of automation technologies, labour market growth and cost, benefits of automation beyond simple labour substitution, and regulatory and social acceptance. 27 These factors might restrict actual job loss to 5% or less.
To our knowledge thus far there have been no jobs eliminated by AI in health care. The limited incursion of AI into the industry thus far, and the difficulty of integrating AI into clinical workflows and EHR systems, have been somewhat responsible for the lack of job impact. It seems likely that the healthcare jobs most likely to be automated would be those that involve dealing with digital information, radiology and pathology for example, rather than those with direct patient contact. 28
But even in jobs like radiologist and pathologist, the penetration of AI into these fields is likely to be slow. Even though, as we have argued, technologies like deep learning are making inroads into the capability to diagnose and categorise images, there are several reasons why radiology jobs, for example, will not disappear soon. 29
First, radiologists do more than read and interpret images. Like other AI systems, radiology AI systems perform single tasks. Deep learning models in labs and startups are trained for specific image recognition tasks (such as nodule detection on chest computed tomography or hemorrhage on brain magnetic resonance imaging). However, thousands of such narrow detection tasks are necessary to fully identify all potential findings in medical images, and only a few of these can be done by AI today. Radiologists also consult with other physicians on diagnosis and treatment, treat diseases (for example providing local ablative therapies) and perform image-guided medical interventions such as cancer biopsies and vascular stents (interventional radiology), define the technical parameters of imaging examinations to be performed (tailored to the patient's condition), relate findings from images to other medical records and test results, discuss procedures and results with patients, and many other activities.
Second, clinical processes for employing AI-based image work are a long way from being ready for daily use. Different imaging technology vendors and deep learning algorithms have different foci: the probability of a lesion, the probability of cancer, a nodule's feature or its location. These distinct foci would make it very difficult to embed deep learning systems into current clinical practice.
Third, deep learning algorithms for image recognition require ‘labelled data’ – millions of images from patients who have received a definitive diagnosis of cancer, a broken bone or other pathology. However, there is no aggregated repository of radiology images, labelled or otherwise.
Finally, substantial changes will be required in medical regulation and health insurance for automated image analysis to take off.
Similar factors are present for pathology and other digitally-oriented aspects of medicine. Because of them, we are unlikely to see substantial change in healthcare employment due to AI over the next 20 years or so. There is also the possibility that new jobs will be created to work with and to develop AI technologies. But static or increasing human employment also mean, of course, that AI technologies are not likely to substantially reduce the costs of medical diagnosis and treatment over that timeframe.
Ethical implications
Finally, there are also a variety of ethical implications around the use of AI in healthcare. Healthcare decisions have been made almost exclusively by humans in the past, and the use of smart machines to make or assist with them raises issues of accountability, transparency, permission and privacy.
Perhaps the most difficult issue to address given today's technologies is transparency. Many AI algorithms – particularly deep learning algorithms used for image analysis – are virtually impossible to interpret or explain. If a patient is informed that an image has led to a diagnosis of cancer, he or she will likely want to know why. Deep learning algorithms, and even physicians who are generally familiar with their operation, may be unable to provide an explanation.
Mistakes will undoubtedly be made by AI systems in patient diagnosis and treatment and it may be difficult to establish accountability for them. There are also likely to be incidents in which patients receive medical information from AI systems that they would prefer to receive from an empathetic clinician. Machine learning systems in healthcare may also be subject to algorithmic bias, perhaps predicting greater likelihood of disease on the basis of gender or race when those are not actually causal factors. 30
We are likely to encounter many ethical, medical, occupational and technological changes with AI in healthcare. It is important that healthcare institutions, as well as governmental and regulatory bodies, establish structures to monitor key issues, react in a responsible manner and establish governance mechanisms to limit negative implications. This is one of the more powerful and consequential technologies to impact human societies, so it will require continuous attention and thoughtful policy for many years.
The future of AI in healthcare
We believe that AI has an important role to play in the healthcare offerings of the future. In the form of machine learning, it is the primary capability behind the development of precision medicine, widely agreed to be a sorely needed advance in care. Although early efforts at providing diagnosis and treatment recommendations have proven challenging, we expect that AI will ultimately master that domain as well. Given the rapid advances in AI for imaging analysis, it seems likely that most radiology and pathology images will be examined at some point by a machine. Speech and text recognition are already employed for tasks like patient communication and capture of clinical notes, and their usage will increase.
The greatest challenge to AI in these healthcare domains is not whether the technologies will be capable enough to be useful, but rather ensuring their adoption in daily clinical practice. For widespread adoption to take place, AI systems must be approved by regulators, integrated with EHR systems, standardised to a sufficient degree that similar products work in a similar fashion, taught to clinicians, paid for by public or private payer organisations and updated over time in the field. These challenges will ultimately be overcome, but they will take much longer to do so than it will take for the technologies themselves to mature. As a result, we expect to see limited use of AI in clinical practice within 5 years and more extensive use within 10.
It also seems increasingly clear that AI systems will not replace human clinicians on a large scale, but rather will augment their efforts to care for patients. Over time, human clinicians may move toward tasks and job designs that draw on uniquely human skills like empathy, persuasion and big-picture integration. Perhaps the only healthcare providers who will lose their jobs over time may be those who refuse to work alongside artificial intelligence.

COMMENTS
Artificial intelligence (AI) is a powerful and disruptive area of computer science, with the potential to fundamentally transform the practice of medicine and the delivery of healthcare. In this review article, we outline recent breakthroughs in the application of AI in healthcare, describe a roadmap to building effective, reliable and safe AI ...
The remainder of this paper is oriented toward the main AI applications. ... Futuristic biosensors for cardiac health care: an artificial intelligence approach. 3. Biotech, 8 (8) (2018), p. 358. ... Global evolution of research in artificial intelligence in health and medicine: a bibliometric study. J Clin Med, 8 (3) ...
This paper evaluated AI in healthcare research streams using the SLR method [].As suggested by Massaro et al. [], an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers.As suggested by many scholars, the methodology allows qualitative and quantitative variables to highlight ...
Artificial Intelligence (AI) has emerged as a transformative force in healthcare, offering a. plethora of applications that promise to revolutionize the industry. This paper explores the. diverse ...
This paper explores artificial intelligence's evolving role in healthcare, focusing on its application in hospitals and clinics. ... This review provides insights into the current state of multimodal medical data fusion in healthcare research. In conclusion, AI's significant role in improving diagnostic accuracy and efficiency is ...
This research aims to investigate and assess the integration of AI into the French healthcare system, particularly in personalized medicine and predictive health analytics, to identify and address ...
Abstract. Artificial intelligence (AI) is poised to broadly reshape medicine, potentially improving the experiences of both clinicians and patients. We discuss key findings from a 2-year weekly ...
The advancements in artificial intelligence (AI) have provided a wealth of opportunities for clinical practice and healthcare. Large language models (LLMs), such as BERT, GPT, and LaMDA have experienced exponential growth, with some now containing over a trillion parameters. 1 This growth in AI capabilities allows for seamless integration between different types of data and has led to ...
The implementation of artificial intelligence (AI) is driving significant transformation inside the administrative and clinical workflows of healthcare organizations at an accelerated rate. This modification highlights the significant impact that AI has on a variety of tasks, especially in health procedures relating to early detection and diagnosis. Papers done in the past imply that AI has ...
Artificial intelligence (AI) has the potential to transform care delivery by improving health outcomes, patient safety, and the affordability and accessibility of high-quality care. AI will be ...
To our knowledge, to date no theoretically grounded paper integrates both organizational- and individual-level factors that may influence the adoption of AI in healthcare, although several clinical and technical papers call for studies on implementation and adoption [20, 22].To fill this research gap and add to the academic literature on adoption, we formulate our research objective as follows:
In this paper, we present the current research concerning a) the state of AI innovation in healthcare, b) its adoption, c) the development and growth of AI-based healthcare startups globally, and d) future research directions for AI-healthcare researchers and leaders and delve into the implications of our findings for global public health ...
As healthcare systems around the world face challenges such as escalating costs, limited access, and growing demand for personalized care, artificial intelligence (AI) is emerging as a key force for transformation. This review is motivated by the urgent need to harness AI's potential to mitigate these issues and aims to critically assess AI's integration in different healthcare domains.
Artificial Intelligence (AI) is evolving rapidly in healthcare, and various AI applications have been developed to solve some of the most pressing problems that health organizations currently face. It is crucial for health leaders to understand the state of AI technologies and the ways that such technologies can be used to improve the ...
Generative AI is designed to create new content from trained parameters. Learning from large amounts of data, many of these models aim to simulate human conversation. Generative AI is being ...
Artificial intelligence (AI) is poised to significantly impact healthcare systems, including clinical diagnosis, healthcare administration and delivery, and public health infrastructures. In the context of the Quintuple Aim of healthcare (patient outcomes, cost reduction, population impact, provider wellness, and equity/inclusion), this chapter ...
INTRODUCTION. The ascent of artificial intelligence (AI) in healthcare has been accompanied by hopes that algorithmic technologies will usher in a golden age of personalized medicine, optimized diagnoses, and streamlined care (Cutler, 2023).Nurses use AI tools to assist in various aspects of patient care, such as care planning and patient monitoring (Clancy, 2020).
Explainability is a heavily debated topic with far-reaching implications that extend beyond the technical properties of AI. Even though research indicates that AI algorithms can outperform humans in certain analytical tasks (e.g. pattern recognition in imaging), the lack of explainability has been criticized in the medical domain . Legal and ...
This paper is based on a selective review of articles concerning AI in mental healthcare and implementation science, with the aim to identify challenges and opportunities for the use of AI in mental healthcare and describe key insights from implementation science of potential relevance to understand and facilitate AI implementation in mental ...
Background As Artificial Intelligence (AI) becomes pervasive in healthcare, including applications like robotic surgery and image analysis, the World Medical Association emphasises integrating AI education into medical curricula. This study evaluates medical students' perceptions of 'AI in medicine', their preferences for AI training in education, and their grasp of AI's ethical ...
This paper presents a comprehensive analysis of AI's current healthcare research landscape. Employing bibliometric analytics, it explores document trends, top sources, influential countries, dynamic keywords, and emerging research topics. The study highlights the United States as a dominant force in AI healthcare research, with over 5,000 ...
The MITRE Corporation 7515 Colshire Drive McLean, VA 22102-7508 (703) 983-6997. This study centers on how computer-based decision procedures, under the broad umbrella of artificial intelligence (AI), can assist in improving health and health care.
This paper evaluated AI in healthcare research streams using the SLR method . As suggested by Massaro et al. , an SLR enables the study of the scientific corpus of a research field, including the scientific rigour, reliability and replicability of operations carried out by researchers.
So far, attempts to improve research and delivery of healthcare using AI have provided some encouraging success stories, as well as some clear examples of over-exaggerated expectations.
Abstract. Artificial intelligence (AI) aims to mimic human cognitive functions. It is bringing a paradigm shift to healthcare, powered by increasing availability of healthcare data and rapid progress of analytics techniques. We survey the current status of AI applications in healthcare and discuss its future. AI can be applied to various types ...
More information: Daiju Ueda et al, Climate change and artificial intelligence in healthcare: Review and recommendations towards a sustainable future, Diagnostic and Interventional Imaging (2024 ...
State of the art research 1-3 indicates that AI techniques can be implemented in various tasks for early architectural design: from performance based goals to form finding, spatial programming and multi-objective optimization. While the state of the art shows which AI techniques have been used in research, it fails to provide a strategic overview on which AI techniques are useful for ...
With the AI device, novice users yielded a MAE of 3.2 (0.1) days vs 3 (0.1) days for the sonographers. Just over 90% of the AI assessments fell within seven days of the ground truth—just shy of the 92.5% achieved by sonographers. AI's performance was consistent for patients in both locations and among patients with a higher body mass index.
OpenResearch, which has also drawn funding from organizations like OpenAI and the US government, handed out the unconditional $1,000 transfers from November 2020 to October 2023.
The complexity and rise of data in healthcare means that artificial intelligence (AI) will increasingly be applied within the field. Several types of AI are already being employed by payers and providers of care, and life sciences companies. The key categories of applications involve diagnosis and treatment recommendations, patient engagement ...