0800 118 2892
- +44 (0)203 151 1280


Teen Cocaine Addiction Case Study: Chloe's Story

This case study of drug addiction can affect anyone – it doesn’t discriminate on the basis of age, gender or background. At Serenity Addiction Centres, our drug detox clinic is open to everyone, and our friendly and welcoming approach is changing the way rehab clinics are helping clients recover from addiction.
We’ve asked former Serenity client, Chloe, to share her experience of drug rehab with Serenity Addiction Centre’s assistance.
Chloe’s Addiction
If you met Chloe today, you would never know about her past. This born and bred London girl is 20 years old, and a flourishing law student with a bright future in the City.
A few years ago though, it seemed as if this straight A student was about to throw away her life, thanks to a class A drug addiction .
Chloe had a great childhood. By her own admission, school was a breeze for her, with strong academic achievement and social skills making her as successful on the playground as she was in the classroom.
Age 7, Chloe started at a boarding school, and loved having friends around her all the time. With no parents about, Chloe and her friends found themselves invited to house parties. As soon as I could convince people they we 18, they moved on to London’s nightclubs.
It was here where Chloe first came across drugs, and it was a slippery slope to cocaine addiction. She explains: “At 15, I was taking poppers, graduated to MDMA at 16, and then I tried cocaine at our year 13 parties. I got separated from my friends, and found them taking cocaine in a back room. I didn’t want to be left out, so I tried it.”
Chloe scored straight As in her A levels, and accepted a place at Kings College London to study law. She was introduced to new people, and it seemed that cocaine was available at every place they went. Parties, clubs, and even her new friends were all good sources of a line of cocaine. As a self confessed wild child by this point, Chloe didn’t want to miss out.
The demands of a law degree were high, but so was Chloe’s desire for more cocaine.
Going out almost every night to snort coke, she started to wonder if she was becoming an addict. She spent every penny of the generous allowance from her parents. Chloe spent every penny available on credit cards, and even took on a £2000 bank loan to support her habit.
Chloe estimated that at one point, her addiction had saddled her with more than £13,000 of debt.
Coming out of Addiction Denial
Chloe’s light bulb moment finally came when her best friend, who she shared a flat with, sat her down and asked why they were drifting apart.
Chloe realised that cocaine had become more important to her than her friends, family, and studies. It had to stop. Chloe found the details for Serenity Addiction Centres, and called the same day to ask for help with her addiction.
One thing Chloe particularly appreciated about Serenity Addiction Centres was the flexible approach of the counsellors . They got to know Chloe, listening to her worries, and working out a non-residential rehab plan for her. This allowed her to continue with her studies.
Chloe’s treatment was organised at a clinic not far from her university, allowing her to keep her studies on track, and keeping her life as normal as possible.
Chloe says: “Talking about how I was using cocaine, along with contributing problems from earlier in my life, were a massive help. I didn’t want to be known just as a party girl”.
“If I’d not found Serenity Addiction Centres, there would probably have been a long wait for NHS treatment. Serenity Addiction Centres got the right treatment. Everything was organised with privacy and discretion. I only shared what was happening with my flatmate.”
This level of discretion was really helpful, and the rapid results of her treatment meant that after just three months Chloe felt able to tell her parents what had been happening.
Life after rehab
It’s amazing that Chloe has now had nearly a year where not taken cocaine, and faced her debts by working part time to repay what she owes. Even better, thanks to Serenity’s fast intervention. Chloe is on course for a 2:1 in her law degree.
If you’re ready to detox? Serenity Addiction Centre’s addiction support team are here to help you find the rehab programme which works for you. Serenity can help you beat your addiction. Gaining control over drugs, allowing you to move on and take back control of your life.
This Drug Addiction Case Study is here so others may identify. Contact us today , and begin your detox journey with Serenity Addiction Centres.
FREE CONSULTATION
Get a no-obligation confidential advice from our medical experts today
Request a call back
We provide a healthy environment uniquely suited to support your growth and healing.
- Rehab Clinic - Serenity Rehabilitation LTD. Arquen House,4-6 Spicer Street, St Albans, Hertfordshire AL3 4PQ
- 0800 118 2892 +44(0)203 151 1280

- Testimonials
- Case Studies
Popular Pages
- Alcohol Addiction
- How To Home Detox From Alcohol
- Alcohol Rehab Centres
- Methadone addiction
Top Locations
- Leicestershire
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
News & Publications
New research and insights into substance use disorder.
Addictions to alcohol, illicit drugs and other substances remain a serious threat: According to the National Center for Health Statistics, part of the Centers for Disease Control and Prevention, from April 2020 to April 2021, nearly 92,000 people in the U.S. fatally overdosed on drugs — the single highest reported death toll during a 12-month period. The National Center for Drug Abuse Statistics has deemed the situation “a public health emergency.” All groups ages 15 and older experienced a rise in these grim statistics, intensified by the use of fentanyl.
Currently, substance use disorder affects more than 20 million Americans ages 12 and over. These numbers are troubling, says Johns Hopkins neuroscientist and addiction researcher Andrew Huhn , “but with a multifaceted approach, people with substance use disorders can recover.”
Drawing from his background in neuroscience and behavioral pharmacology, Huhn identifies risk factors for relapse and medication strategies — bolstered by supervised withdrawal and counseling — to improve treatment outcomes. “My research focuses on understanding the human experience of substance use disorder,” he says, noting that medications for opioid overdose, withdrawal and addiction “are safe, effective and continue to save lives.”
Now, thanks to a recent collaboration with Ashley Addiction Treatment, a residential treatment center in Havre de Grace, Maryland, Huhn, Kelly Dunn and colleagues are combining efforts to identify patients likely to benefit from supervised withdrawal or opioid maintenance therapy. The goal is to expand treatment options to improve health care for people with the condition. “Relapse remains common, but a subset of patients have done well,” says Dunn.
Concurrently, Huhn, Dunn and colleagues are building a research database based on the Trac9 program, which charts patients’ progress in real-time through technology, such as a tablet or phone — as well as alerting clinicians to a relapse and the need for intervention. They are also using wearable devices to monitor sleep and cardiovascular outcomes, and a smart phone application to track each time a patient notes having successfully ignored a craving for alcohol or a drug. Much of this research takes place at Behavioral Pharmacology Research Unit , located on the Johns Hopkins Bayview Medical Center campus.
Their published work includes studies showing a greater need for treatment of older adults with alcohol and opioid use disorders. Two additional studies have garnered national attention, both on how fentanyl use affects the treatment of opioid use disorder . Much of the illicit opioid supply in the U.S. is mixed with fentanyl, leading to a recent surge in fentanyl-related overdose deaths.
Yet another study showed promise in the use of a sleep medication to improve opioid withdrawal outcomes. Researchers in Huhn’s lab continue to glean insights from neuroimaging, ambulatory monitoring in real time, and repeated measures of behaviors.
Greg Hobelmann , the CEO of Ashley, who trained at Johns Hopkins and is a part-time faculty member, chairs an elective at the Ashley facility in addictions psychiatry. He, along with Eric Strain and Huhn are building infrastructure that includes intake data on every patient, as well as outcomes data when people complete the Ashley program — and for the year that follows. Biospecimens will also be included in the project, for studies in areas such as genetics.
“The biggest and most exciting thing is being able to create predictive models of relapse risk and then create strategies to improve those outcomes,” says Huhn. Jimmy Potash , director of the Johns Hopkins Department of Psychiatry and Behavioral Sciences couldn’t agree more. “This will be a powerful platform for discovery of better approaches to treating addiction,” he says. “I’m eager to see it — and our relationship with Ashley Addiction — move forward.”
Despite enduring challenges in addictions psychiatry, Huhn is hopeful. “We have the ability to continue collecting data and to test hypotheses,” he says. “It’s the kind of stuff we hope will turn into a game-changer, similar to what has happened in cancer and heart disease treatments. We build research into the treatment and let that guide our approach to care.”
Learn about a web-based education intervention to reduce opioid overdose, Low-Cost Intervention Reduces Risk of Opioid Overdose.
Related Reading
Johns hopkins bayview’s center for addiction and pregnancy supports new mothers and their babies in the fight against substance use disorders.
Center offers judgment-free care, helping moms and newborns

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Challenges to Studying Illicit Drug Users
Affiliations.
- 1 Alpha Nu , Postdoctoral Research Fellow, Center for the Study of Drugs, Alcohol, Smoking and Health, University of Michigan, T32 (NR016914) Complexity: Innovations for Promoting Health and Safety, Ann Arbor, MI, USA.
- 2 Alpha Nu , Director of Office of Nursing Research and Evaluation an The Richard and Marianne Kreider Endowed Professor in Nursing for Vulnerable Populations, M. Louise Fitzpatrick College of Nursing, Villanova University, Villanova, PA, USA.
- 3 Alpha Nu , Professor, M. Louise Fitzpatrick College of Nursing, Villanova University, Villanova, PA, USA.
- PMID: 31106524
- PMCID: PMC6671678
- DOI: 10.1111/jnu.12486
Purpose: Throughout the world, illicit drug use continues to pose a significant risk to public health. The opioid crisis in North America, the diversion of the prescription drug tramadol throughout Africa, and the increasing supply of methamphetamines in East and South Asia all contribute to increasing risks to individual and societal health. Furthermore, the violation of human rights in efforts to enforce prohibitionist values poses significant threats to many individuals worldwide. With these evolving situations, it is imperative that researchers direct their attention to the various populations of illicit drug users. However, the inclusion of illicit drug users, often considered a vulnerable population, as participants in research studies presents several increased risks that must be addressed in study protocols. Researchers are required to provide "additional safeguards" to all study protocols involving illicit drug users, but there is often substantial variability and inconsistency in how these safeguards are applied. Additional safeguards can be timely, costly, and unduly burdensome for researchers, ethical review boards, and research participants.
Approach: Through synthesis of the current literature, this article addresses the barriers to studying illicit drug users and the methods researchers can utilize to minimize risk. A case study is provided to illustrate the high level of scrutiny of study protocols involving the participation of illicit drug users and the effect of such scrutiny on recruitment of participants. The article concludes with a discussion of the effects of the current political climate on the recruitment of illicit drug users in research.
Conclusions: Individuals who participate in criminal or illegal behaviors such as illicit drug use, prostitution, illegal entry into a country, and human trafficking are susceptible to multiple physical, mental, and social health risks, as well as criminal prosecution. The importance of research on the health of marginalized populations cannot be overstated. This work must continue, and at the same time, we must continue to protect these individuals to the best of our ability through diligent attention to sound research methods.
Clinical relevance: The use of illicit drugs continues to pose a substantial threat to global health. Individuals who use illicit drugs are susceptible to multiple physical, mental, and social health risks, as well as criminal prosecution. It is imperative that researchers study these vulnerable populations in order to develop interventions to minimize individual and societal harm. There are several barriers to the study of illicit drug users that must be addressed through rigorous methodology and the addition of safeguards.
Keywords: Illicit drug use; research ethics; research methodology; vulnerable populations.
© 2019 Sigma Theta Tau International.
PubMed Disclaimer
Similar articles
- Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, Salomon J, Vassall A, Volchenkov G, White R, Wilson D, Yadav P. Bloom BR, et al. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major Infectious Diseases. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 3. Chapter 11. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major Infectious Diseases. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 3. Chapter 11. PMID: 30212088 Free Books & Documents. Review.
- Estimation of the Social Costs of Illegal Drug Use in Poland Using Standardized Methodology. Mielecka-Kubie ZJ. Mielecka-Kubie ZJ. J Ment Health Policy Econ. 2020 Sep 1;23(3):139-149. J Ment Health Policy Econ. 2020. PMID: 33411676
- American Society of Clinical Oncology policy statement: oversight of clinical research. American Society of Clinical Oncology. American Society of Clinical Oncology. J Clin Oncol. 2003 Jun 15;21(12):2377-86. doi: 10.1200/JCO.2003.04.026. Epub 2003 Apr 29. J Clin Oncol. 2003. PMID: 12721281
- Illicit drug use while admitted to hospital: Patient and health care provider perspectives. Strike C, Robinson S, Guta A, Tan DH, O'Leary B, Cooper C, Upshur R, Chan Carusone S. Strike C, et al. PLoS One. 2020 Mar 5;15(3):e0229713. doi: 10.1371/journal.pone.0229713. eCollection 2020. PLoS One. 2020. PMID: 32134973 Free PMC article.
- Realising the technological promise of smartphones in addiction research and treatment: An ethical review. Capon H, Hall W, Fry C, Carter A. Capon H, et al. Int J Drug Policy. 2016 Oct;36:47-57. doi: 10.1016/j.drugpo.2016.05.013. Epub 2016 Jun 1. Int J Drug Policy. 2016. PMID: 27455467 Review.
- Suicidal thoughts and behaviors among untreated illicit substance users: a population-based study. Shiraly R, Jazayeri SA, Seifaei A, Jeihooni AK, Griffiths MD. Shiraly R, et al. Harm Reduct J. 2024 May 16;21(1):96. doi: 10.1186/s12954-024-01015-9. Harm Reduct J. 2024. PMID: 38755587 Free PMC article.
- Promoting research engagement among women with addiction: Impact of recovery peer support in a pilot randomized mixed-methods study. Zgierska AE, Hilliard F, Deegan S, Turnquist A, Goldstein E. Zgierska AE, et al. Contemp Clin Trials. 2023 Jul;130:107235. doi: 10.1016/j.cct.2023.107235. Epub 2023 May 19. Contemp Clin Trials. 2023. PMID: 37211273 Free PMC article. Clinical Trial.
- A mixed-methods analysis of risk-reduction strategies adopted by syringe services program participants and non-syringe services program participants in New York City. Beharie N, Urmanche A, Harocopos A. Beharie N, et al. Harm Reduct J. 2023 Mar 25;20(1):38. doi: 10.1186/s12954-023-00772-3. Harm Reduct J. 2023. PMID: 36966342 Free PMC article.
- Risk of Central Serous Chorioretinopathy in Male Androgen Abusers. Subhi Y, Windfeld-Mathiasen J, Horwitz A, Horwitz H. Subhi Y, et al. Ophthalmol Ther. 2023 Apr;12(2):1073-1080. doi: 10.1007/s40123-023-00658-4. Epub 2023 Jan 24. Ophthalmol Ther. 2023. PMID: 36692812 Free PMC article.
- Abbott L, & Grady C (2011). A systematic review of the empirical literature evaluating IRBs: What we know and what we still need to learn. Journal of Empirical Research on Human Research Ethics, 6(1), 3 10.1525/jer.2011.6.1.3 - DOI - PMC - PubMed
- Aldridge J, & Charles V (2008). Researching the intoxicated: Informed consent implications for alcohol and drug research. Drug and Alcohol Dependence, 93(3), 191–196. 10.1016/j.drugalcdep.2007.09.001 - DOI - PubMed
- Anderson EE, & DuBois JM (2007). The need for evidence-based research ethics: A review of the substance abuse literature. Drug and Alcohol Dependence, 86(2–3), 95–105. 10.1016/j.drugalcdep.2006.06.011 - DOI - PubMed
- Australian Injecting and Illicit Drug Users League. (2012). The involvement of drug users organizations in Australian drugs policy; a research report from AIVL’s “Trackmarks” project. Retrieved from https://nuaa.org.au/wp-content/uploads/2016/11/T4.7.2-aivl-drug-user.pdf .
- Bell K, & Salmon A (2011). What women who use drugs have to say about ethical research: Findings of an exploratory qualitative study. Journal of Empirical Research on Human Research Ethics, 6(4), 84–98. - PubMed
- Search in MeSH
Grants and funding
- T32 NR016914/NR/NINR NIH HHS/United States
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- MLibrary (Deep Blue)
- Ovid Technologies, Inc.
- PubMed Central
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open Access
- By Publication (A-Z)
- Case Reports
- Publication Ethics
- Publishing Policies
- Editorial Policies
- Submit Manuscript
- About Graphy

New to Graphy Publications? Create an account to get started today.
Registered Users
Have an account? Sign in now.

- Full-Text HTML
- Full-Text PDF
- About This Journal
- Aims & Scope
- Editorial Board
- Editorial Process
- Author Guidelines
- Special Issues
- Articles in Press

Jo-Hanna Ivers 1* and Kevin Ducray 2
In October 2012, 83 front-line Irish service providers working in the addiction treatment field received accreditation as trained practitioners in the delivery of a number of evidence-based positive reinforcement approaches that address substance use: 52 received accreditation in the Community Reinforcement Approach (CRA), 19 in the Adolescent Community Reinforcement Approach (ACRA) and 12 in Community Reinforcement and Family Training (CRAFT). This case study presents the treatment of a 17-year-old white male engaging in high-risk substance use. He presented for treatment as part of a court order. Treatment of the substance use involved 20 treatment sessions and was conducted per Adolescent Community Reinforcement Approach (A-CRA). This was a pilot of A-CRA a promising treatment approach adapted from the United States that had never been tried in an Irish context. A post-treatment assessment at 12-week follow-up revealed significant improvements. At both assessment and following treatment, clinician severity ratings on the Maudsley Addiction Profile (MAP) and the Alcohol Smoking and Substance Involvement Screening Test (ASSIST) found decreased score for substance use was the most clinically relevant and suggests that he had made significant changes. Also his MAP scores for parental conflict and drug dealing suggest that he had made significant changes in the relevant domains of personal and social functioning as well as in diminished engagement in criminal behaviour. Results from this case study were quite promising and suggested that A-CRA was culturally sensitive and applicable in an Irish context.
1. Theoretical and Research Basis for Treatment
Substance use disorders (SUDs) are distinct conditions characterized by recurrent maladaptive use of psychoactive substances associated with significant distress. These disorders are highly common with lifetime rates of substance use or dependence estimated at over 30% for alcohol and over 10% for other substances [1 , 2] . Changing substance use patterns and evolving psychosocial and pharmacologic treatments modalities have necessitated the need to substantiate both the efficacy and cost effectiveness of these interventions.
Evidence for the clinical application of cognitive behavioural therapy (CBT) for substance use disorders has grown significantly [3 - 8] . Moreover, CBT for substance use disorders has demonstrated efficacy both as a monotherapy and as part of combination treatment [7] . CBT is a time-limited, problem-focused, intervention that seeks to reduce emotional distress through the modification of maladaptive beliefs, assumptions, attitudes, and behaviours [9] . The underlying assumption of CBT is that learning processes play an imperative function in the development and maintenance of substance misuse. These same learning processes can be used to help patients modify and reduce their drug use [3] .
Drug misuse is viewed by CBT practitioners as learned behaviours acquired through experience [10] . If an individual uses alcohol or a substance to elicit (positively or negatively reinforced) desired states (e.g. euphorigenic, soothing, calming, tension reducing) on a recurrent basis, it may become the preferred way of achieving those effects, particularly in the absence of alternative ways of attaining those desired results. A primary task of treatment for problem substance users is to (1) identify the specific needs that alcohol and substances are being used to meet and (2) develop and reinforce skills that provide alternative ways of meeting those needs [10 , 11] .
CRA is a broad-spectrum cognitive behavioural programme for treating substance use and related problems by identifying the specific needs that alcohol and or other substances are satisfying or meeting. The goal is then to develop and reinforce skills that provide alternative ways of meeting those needs. Consistent with traditional CBT, CRA through exploration, allows the patient to identify negative thoughts, behaviours and beliefs that maintain addiction. By getting the patient to identify, positive non-drug using behaviours, interests, and activities, CRA attempts to provide alternatives to drug use. As therapy progresses the objective is to prevent relapse, increase wellness, and develop skills to promote and sustain well-being. The ultimate aim of CRA, as with CBT is to assist the patient to master a specific set of skills necessary to achieve their goals. Treatment is not complete until those skills are mastered and a reasonable degree of progress has been made toward attaining identified therapy goals. CRA sessions are highly collaborative, requiring the patient to engage in ‘between session tasks’ or homework designed reinforce learning, improve coping skills and enhance self efficacy in relevant domains.
The use of the Community Reinforcement Approach is empirically supported with inpatients [12 , 13] , outpatients [14 - 16] and homeless populations (Smith et al., 1998). In addition, three recent metaanalytic reviews cited CRA as one of the most cost-effective treatment programmes currently available [17 , 18] .
A-CRA is a evidenced based behavioural intervention that is an adapted version of the adult CRA programme [19] . Garner et al [19] modified several of the CRA procedures and accompanying treatment resources to make them more developmentally appropriate for adolescents. The main distinguishing aspect of A-CRA is that it involves caregivers—namely parents or guardians who are ultimately responsible for the adolescent and with whom the adolescent is living.
A-CRA has been tested and found effective in the context of outpatient continuing care following residential treatment [20 - 22] and without the caregiver components as an intervention for drug using, homeless adolescents [23] . More recently, Garner et al [19] collected data from 399 adolescents who participated in one of four randomly controlled trials of the A-CRA intervention, the purpose of which was to examine the extent to which exposure to A-CRA procedures mediated the relationship between treatment retention and outcomes. The authors found adolescents who were exposed to 12 or more A-CRA procedures were significantly more likely to be in recovery at follow-up.
Combining A-CRA with relapse prevention strategies receives strong support as an evidence based, best practice model and is widely employed in addiction treatment programmes. Providing a CBT-ACRA therapeutic approach is imperative as it develops alternative ways of meeting needs and thus altering dependence.
2. Case Introduction
Alan is a 17 year-old male currently living in County Dublin. Alan presented to the agency involuntarily and as a requisite of his Juvenile Liaison Officer who was seeing him on foot of prior drugs arrest for ‘possession with intent to supply’; a more serious charge than a simple ‘drugs possession’ charge. As Alan had no previous charges he was placed on probation for one year. This was Alan’s first contact with the treatment services. A diagnostic assessment was completed upon entry to treatment and included completion of a battery of instruments comprising the Maudsley Addiction Profile (MAP), The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and the Beck Youth Inventory (BYI) (see appendices for full description of outcome measures) (Table 1).

3. Diagnostic Criteria
The apparent symptoms of substance dependency were: (1) Loss of Control - Alan had made several attempts at controlling the amounts of cannabis he consumed, but those times when he was able to abstain from cannabis use were when he substituted alcohol and/or other drugs. (2) Family History of Alcohol/Drug Usage - Alan’s eldest sister who is now 23 years old is in recovery from opiate abuse. She was a chronic heroin user during her early adult years [17 - 21] . During this period, which corresponds to Alan’s early adolescent years [12 - 15] she lived in the family home (3) Changes in Tolerance - Alan began per day. At presentation he was smoking six to eight cannabis joints daily through the week, and eight to twelve joints daily on weekends.
4. Psychosocial, Medical and Family History
At time of intake Alan was living with both of his parents and a sister, two years his senior, in the family home. Alan was the youngest and the only boy in his family. He had two other older sisters, 5 and 7 years his senior. He was enrolled in his 5th year of secondary school but at the time of assessment was expelled from all classes. Alan had superior sporting abilities. He played for the junior team of a first division football team and had the prospect of a professional career in football. He reported a family history positive for substance use disorders. An older sister was in recovery for opiate dependence. Apart from his substance use Alan reported no significant psychological difficulties or medical problems. His motives for substance use were cited as boredom, curiosity, peer pressure, and pleasure seeking. His triggers for use were relationship difficulties at home, boredom and peer pressure. Pre-morbid personality traits included thrill seeking and impulsivity (Table 2).

5. Case Conceptualisation
A CBT case formulation is based on the cognitive model, which hypothesizes that "a person’s feelings and emotions are influenced by their perception of events" . It is not the actual event that determines how the person feels, but rather how they construe the event (Beck, 1995 p14). Moreover, cognitive theory posits that the “child learns to construe reality through his or her early experiences with the environment, especially with significant others” and that “sometimes these early experiences lead children to accept attitudes and beliefs that will later prove maladaptive” [24] . A CBT formulation (or case conceptualisation) is one of the key underpinnings of Cognitive Behavioural Therapy (CBT). It is the ‘blueprint’ which aids the therapist to understand and explain the patient’s’ problems.
Formulation driven CBT enables the therapist to develop an individualised understanding of the patient and can help to predict the difficulties that a patient may encounter during therapy. In Alan’s case, exploring his existing negative automatic thoughts about regarding school and his academic competences highlighted the difficulties he could experience with CBT homework completion. Whilst Alan was good at between session therapy assignments, an exploration of what is meant by ‘homework’ in a CBT context was crucial.
A collaborative CBT formulation was done diagrammatically together with Alan (Figure 1). This formulation aimed to describe his presenting problems and using CBT theory, to explore explanatory inferences about the initiating and maintaining factors of his drug use which could practically inform meaningful interventions.

Simmons and Griffiths et al. make the insightful observation that particular group differences need to be specifically considered and suggest that the therapist should be cognizant of the role of both society and culture when developing a formulation. They firstly suggest that the impact played by gender, sexuality and socio-cultural roles in the genesis of a psychological disorder, namely the contribution that being a member of a group may have on predisposing and precipitating factors, be carefully considered. An example they offer is the role of poverty on the development of psychological problems, such as the link evidenced between socio economic group and onset of schizophrenia. This was clearly evident in the case of Alan, who being a member of a deprived socioeconomic group, growing up and living in an area with a high level of economic deprivation, perceived that his choices for success were limited. His thinking, as an adolescent boy, was dichotomous in that he saw himself as having only two fixed and limited choices (a) being good at sport he either pursue a career as a professional sportsman or alternatively (b) he engage in crime and work his way up through the ranks as a ‘career criminal’. Simmons & Griffiths secondly suggest that being a member of a particular group can heavily influence a person’s understanding of the causality of their psychological disorder. A third consideration when developing a formulation is the degree to which being a member of a particular group may influence the acceptance or rejection of a member experiencing a psychological illness. Again this is pertinent in Alan’s case as he was part of a sub-group, a gang engaged in crime. For this cohort, crime and drug use were synonymous. Using drugs was viewed as a rite of passage for Alan.
Drug use, according to CBT models, are socially learned behaviours initiated, maintained and altered through the dynamic interaction of triggers, cues, reinforcers, cognitions and environmental factors. The application of a such a formulation, sensitive to Simmons and Griffiths (2009) aforementioned observations, proved useful in affording insights into the contextual and maintaining factors of Alan’s drug use which was heavily influenced by the availability of drugs ,his peer group (with whom he spent long periods of time) and their petty drug dealing and criminality. Similarly, engaging with his football team mates during the lead up to an important match significantly reduced his drug use and at certain times of the year even lead to abstinence. Sharing this formulation allowed him to note how his drug use patterns were driven, as per the CBT paradigm, by modifiable external, transient, and specific factors (e.g. cues, reinforcements, social networks and related expectations and social pressures).
Employing the A-CRA model allowed for this tailored fit as A-CRA specifically encourages the patient to identify their own need and desire for change. Alan identified the specific needs that were met by using substances and he developed and reinforced skills that provided him with alternative ways of meeting those needs. This model worked extremely well for Alan as he had identified and had ready access to a pro- social ‘alternative group’ or community. As he had had access to an alternative positive peer group and another activity (sport) which he was ‘really good at’, he simply needed to see the evidence of how his context could radically affect his substance use; more specifically how his beliefs, thinking and actions in certain circumstances produced very different drug use consequences and outcomes.
6. Course of Treatment and Assessment of Progress
One focus of CBT treatment is on teaching and practising specific helpful behaviours, whilst trying to limit cognitive demands on clients. Repetition is central to the learning process in order to develop proficiency and to ensure that newly acquired behaviours will be available when needed. Therefore, behavioural using rehearsal will emphasize varied, realistic case examples to enhance generalization to real life settings. During practice periods and exercises, patients are asked to identify signals that indicate high-risk situations, demonstrating their understanding of when to use newly acquired coping skills. CBT is designed to remedy possible deficits in coping skills by better managing those identified antecedents to substance use. Individuals who rely primarily on substances to cope have little choice but to resort to substance use when the need to cope arises. Understanding, anticipating and avoiding high risk drug use scenarios or the “early warning signals” of imminent drug use is a key CBT clinical activity.
A major goal of a CBT/A-CRA therapeutic approach is to provide a range of basic alternative skills to cope with situations that might otherwise lead to substance use. As ‘skill deficits’ are viewed as fundamental to the drug use trajectory or relapse process, an emphasis is placed on the development and practice of coping skills. A-CRA was manualised in 2001 as part of the Cannabis Youth Treatment Series (CYT) and was tested in that study [21] and more recently with homeless youth [23] . It was also adapted for use in a manual for Assertive Continuing Care following residential treatment [20] .
There are twelve standard and three optional procedures proposed in the A-CRA model. The delivery of the intervention is flexible and based on individual adolescent needs, though the manual provides some general guidelines regarding the general order of procedures. Optional procedures are ‘Dealing with Failure to Attend’, ‘Job-Seeking Skills’, and ‘Anger Management’. Standard procedures are included in table 3 below. For a more detailed description of sessions and procedures please see appendices.

Smith and Myers describe the theoretical underpinnings of CRA as a comprehensive behavioural program for treating substance-abuse problems. It is based on the belief that environmental contingencies can play a powerful role in encouraging or discouraging drinking or drug use. Consequently, it utilizes social, recreational, familial, and vocational reinforcers to assist consumers in the recovery process. Its goal is to essentially make a sober lifestyle more rewarding than the use of substances. Interestingly the authors note: ‘Oddly enough, however, while virtually every review of alcohol and drug treatment outcome research lists CRA among approaches with the strongest scientific evidence of efficacy, very few clinicians who treat consumers with addictions are familiar with it’. ‘The overall philosophy is to promote community based rewarding of non drug-using behaviour so that the patient makes healthy lifestyle changes’ p.3 [25] .
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment. This tailored approach is facilitated by conducting a ‘functional analysis’ of the adolescent’s behaviour at the beginning of therapy so they can better understand and interrupt the links in the behavioural chain typically leading to episodes of drug use. A-CRA therapists then teach individuals how to improve communication and other skills, build on their reinforcers for abstinence and use existing community resources that will support positive change and constructive support systems.
A-CRA emphasises lapse and relapse prevention. Relapseprevention cognitive behavioural therapy (RP-CBT) is derived from a cognitive model of drug misuse. The emphasis is on identifying and modifying irrational thoughts, managing negative mood and intervening after a lapse to prevent a full-blown relapse [26] . The emphasis is on development of skills to (a) recognize High Risk Situations (HRS) or states where clients are most vulnerable to drug use, (b) avoidance of HRS, and (C) to use a variety of cognitive and behavioural strategies to cope effectively with these situations. RPCBT differs from typical CBT in that the accent is on training people who misuse drugs to develop skills to identify and anticipate situations or states where they are most vulnerable to drug use and to use a range of cognitive and behavioural strategies to cope effectively with these situations [26] .
7. Access and Barriers to Care
Alan engaged with the service for eight months. During this time he received twenty sessions, three of which were assessment focused, the remaining seventeen sessions were A-CRA focused; two of the seventeen involved his mother, the remaining fifteen were individual. As Alan was referred by the probation services, he was initially somewhat ambivalent about drug use focussed interventions. His early motivation for engagement was primarily to avoid the possibility of a custodial sentence.
8. Treatment
My sessions with Alan were guided by the principles of A-CRA [27] which focuses on coping skills training and relapse prevention approaches to the treatment of addictive disorders. Prior to engaging with Alan, I had completed the training course and commenced the A-CRA accreditation process, both under the stewardship of Dr Bob Meyers, whose training and publication offers detailed guidelines on skills training and relapse prevention with young people in a similar context [27] .
During the early part of each session I focused on getting a clear understanding of Alan’s current concerns, his general level of functioning, his substance abuse and pattern of craving during the past week. His experiences with therapy homework, the primary focus being on what insight he gained by completing such exercises was also explored. I spent considerable time engaged in a detailed review of Alan’s experience with the implementation of homework tasks during which the following themes were reviewed:
-Gauging whether drug use cessation was easier or harder than he anticipated? -Which, if any, of the coping strategies worked best? -Which strategies did not work as well as expected. Did he develop any new strategies? -Conveying the importance of skills practice, emphasising how we both gained greater insights into how cognitions influenced his behaviour. After developing a clear sense of Alan’s general functioning, current concerns and progress with homework implementation, I initiated the session topic for that week. I linked the relevance of the session topic to Alan’s current cannabis-related concerns and introduced the topic by using concrete examples from Alan’s recent experience. While reviewing the material, I repeatedly ensured that Alan understood the topic by asking for concrete examples, while also eliciting Alan’s views on how he might use these particular skills in the future.
Godley & Meyers [21] propose a homework exercise to accompany each session. An advantage of using these homework sheets is that they also summarise key points about each topic and therefore serve as a useful reminder to the patient of the material discussed each week. Meyers, et al. (2011) suggests that rather than being bound by the suggested exercises in the manualised approach, they may be used as a starting point for discussing the best way to implement the required skill and to develop individualised variations for new assignments [27] . The final part of each session focused on Alan’s plan for the week ahead and any anticipated high-risk situations. I endeavoured to model the idea that patients can literally ‘plan themselves out of using’ cannabis or other drugs. For each anticipated high-risk situation, we identified appropriate and viable coping skills. Better understanding, anticipating and planning for high-risk situations was difficult in the beginning of treatment as Alan was not particularly used to planning or thinking through his activities. For a patient like Alan, whose home life is often chaotic, this helped promote a growing sense of self efficacy. Similarly, as Alan had been heavily involved with drug use for a long time, he discovered through this process that he had few meaningful activities to fill his time or serve as alternatives to drug use. This provided me with an opportunity to discuss strategies to rebuild an activity schedule and a social network.
During our sessions, several skill topics were covered. I carefully selected skills to match Alan’s needs. I selected coping skills that he has used in the past and introduced one or two more that were consistent with his cognitive style. Alan’s cognitive score indicated a cognitive approach reflecting poor problem solving or planning. Sessions focused on generic skills including interpersonal skills, goal setting, coping with criticism or anger, problem solving and planning. The goal was to teach Alan how to build on his pro- social reinforcers, how to use existing community resources supportive of positive change and how to develop a positive support system.
The sequence in which these topics were presented was based on (a) patient needs and (b) clinician judgment (a full description of individual sessions may be found in appendices).
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment.
9. Assessment of Treatment Outcome
A baseline diagnostic assessment of outcomes was completed upon treatment entry. This assessment consisted of a battery of psychological instruments including (see appendices for full a description of assessment measures):
-The Maudsley Addiction Profile (MAP). -The Beck Youth Inventories. -The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST).
In addition to the above, objective feedback on Alan’s clinical and drug use status through urine toxicology screens was an important part of his drug treatment. Urine specimens were collected before each session and available for the following session. The use of toxicology reports throughout treatment are considered a valuable clinical tool. This part of the session presents a good opportunity to review the results of the most recent urine toxicology screen and promote meaningful therapeutic activities in the context of the patient’s treatment goals [28] .
In reporting on substance use since the last session, patients are likely to reveal a great deal about their general level of functioning and the types of issues and problems of most current concern. This allows the clinician to gauge if the patient has made progress in reducing drug use, his current level of motivation, whether there is a reasonable level of support available in efforts to remain abstinent and what is currently bothering him. Functional analyses are opportunistically used throughout treatment as needed. For example, if cannabis use occurs, patients are encouraged to analyse antecedent events so as to determine how to avoid using in similar situations in the future. The purpose is to help the patient understand the trajectory and modifiable contextual factors associated with drug use, challenge unhelpful positive drug use expectancies, identify possible skills deficiencies as well as seeking functionally equivalent non- drug using behaviours so as to reduce the probability of future drug use. The approach I used is based on the work of [28] .
The Functional Analysis was used to identify a number of factors occurring within a relatively brief time frame that influenced the occurrence of problem behaviours. It was used as an initial screening tool as part of a comprehensive functional assessment or analysis of problem behaviour. The results of the functional analysis then served as a basis for conducting direct observations in a number of different contexts to attest to likely behavioural functions, clarify ambiguous functions, and identify other relevant factors that are maintaining the behaviour.
The Happiness Scale rates the adolescent’s feelings about several critical areas of life. It helps therapists and adolescents identify areas of life that adolescents feel happy about and alternatively areas in which they have problems or challenges. Most importantly it identifies potential treatment goals subjectively meaningful to the patient, facilitates positive behaviour change in a range of life domains as well as help clients track their progress during treatment.
Alan’s BYI score (Table 4) indicates that at the time of assessment he was within the average scoring range on ‘self-concept’, and moderately elevated in the areas of ‘depression’, ‘anxiety’, and ‘disruptive behaviour’. His score for ‘anger’ suggested that his anger fell within the extremely elevated range. When this was discussed with Alan he agreed that this was quite accurate. Anger, and in particular controlling his anger, was subjectively identified as a treatment goal.

10. Follow-up
Given that follow-up occurred by telephone it was not feasible to administer the full battery of tests. With Alan’s treatment goals in mind it was decided to administer the MAP and ASSIST. Table 5 below illustrates Alan’s score at baseline and follow-up for the MAP and ASSIST. For summary purposes I have taken areas for concern at baseline for both instruments.

Alan’s score for cannabis was the most clinically relevant as it placed him in the 'high risk’ domain while his alcohol score indicated that he had engaged in binge drinking (6+ drinks) at T1. However, at T2 Alan’s score suggests that he had made considerable reductions in the use of both substances. Also his MAP scores for parental conflict and drug dealing suggest that he had also made major positive changes in the relevant domains of personal and social functioning as well as ceasing criminal behaviour.
At 3 months post-discharge I contacted Alan by phone. He had maintained and continued to further his progress. His drug use was at a minimal level (1 or 2 shared joints per month). He was no longer engaged in crime and his probationary period with the judicial system had passed. He had received a caution for his earlier drugs charge. At the time of follow-up he was enjoying participating in a Sports Coaching course and was excelling with his study assignments. Relationships had improved considerably with his mother and sister and he had re-engaged with a previous, positive, peer group linked to his involvement with the GAA . Overall he felt he was doing extremely well.
11. Complicating Factors with A-CRA Model
There are many challenges that may arise in the treatment of substance use disorders that can serve as barriers to successful treatment. These include acute or chronic cognitive deficits, health problems, social stressors and a lack of social resources [7] . Among individuals presenting with substance use there are often other significant life challenges including early school leaving, family conflicts, legal issues, poor or deviant social networks, etc. A particular challenge with Alan’s case was the social and environmental milieu which he shared with his drug using peers. For Alan, who initially had few skills and resources, engaging in treatment meant not only being asked to change his overall way of life but also to renounce some of those components in which he enjoyed a sense of belonging, particularly as he had invested significantly in these friendships. A sense of ‘belonging to the substance use culture’ can increase ambivalence for change [7] . Alan’s mother strongly disapproved of his drug using peer group and failed to acknowledge Alan’s perceived loss. This resulted in mother- son conflict. The use of the caregiver session allowed an exploration of perceived ‘losses’ relative to the ‘gains’ associated with Alan’s abstinence. It was moreover seen to be critical to establish alternatives for achieving a sense of belonging, including both his social connection and his social effectiveness. Alan’s sports ability allowed for this to be fostered. He is a talented sportsman which often meant his acceptance within a team or group is a given.
Despite the positive effects of A-CRA it is not without its shortcomings. The approach is at times quite American- oriented, particularly around identifying local resources and its focus on culturally specific outlets in promoting social engagement as alternatives to substance use. While this is supported in the literature, it may not necessarily be transferable to certain Irish adolescent contexts or subcultures.
12. Treatment Implications of the Case
A-CRA captures a broad range of behavioural treatments including those targeting operant learning processes, motivational barriers to improvement and other more traditional elements of cognitivebehavioural interventions. Overall, this intervention has demonstrated efficacy. Despite this heterogeneity, core elements emerge based in a conceptual model of SUDs as disorders characterized by learning processes and driven by the strongly reinforcing effects of the substances of abuse. There is rich evidence in the substance use disorders literature that improvement achieved by CBT (7) and indeed A-CRA (Godley et al. and Garner et al. [22 , 20] ) generalizes to all areas of functioning, including social, work, family and marital adjustment domains. The present study’s finding that a reduction in substance-related symptoms was accompanied by improved levels of functioning, social adjustment and enhanced quality of life, provides further support for this point.
In conclusion, there is some preliminary evidence that A-CRA is a promising treatment in the rehabilitation of adolescent substance users in Ireland and culturally similar societies. Clearly, results from a case study have limited generalisability and there is need for larger controlled studies providing robust outcomes to confirm the efficacy of A-CRA in an Irish context. A more systematic study of this issue is in the interest of adolescent substance users and the health services providers faced with the challenge of providing affordable, evidencebased mental health and addiction care to young people.
13. Recommendations to Clinicians and Students
The ACRA model is a structured assemblage of a range of cognitive and behavioural activities (e.g. a rationale and overview of the paradigm, sobriety sampling, functional analyses, communication skills, problem solving skills, refusal skills, jobs counselling, anger management and relapse prevention) which are shared in varying degrees with other CBT approaches. The ACRA model has the advantage of established effectiveness. A foundation in empirical research together with its manual- supported approach results in it being an appropriate “off the shelf ” intervention, highly applicable to many adolescent substance misusers. Such a focussed approach also has the advantage of limiting therapist “drift”. Notwithstanding the accessible manual and other resources available on- line, clinicians and students are strongly encouraged to undergo accredited ACRA training and supervision.
Unfortunately such a structured model, despite its many advantages, does have limitations. This model may not meet the sum of all drug misusing adolescent service user treatment needs, nor is it applicable to all adolescent drug users, particularly highly chaotic individuals with high levels of co- morbidities or multi-morbidities as often found in this population [29 , 30] . Whilst focussing on specifically on drug use, ACRA does not directly address co-existing problem behaviours or challenges such as depression, anxiety, personality disorder, or post traumatic stress disorder (PTSD) synergistically linked to drug use. It is possible that given the high levels of dual diagnoses encountered in this population as well as the compounding effect that drug use exerts on multiple systems, clinicians and practitioners may find a strict application of the ACRA model limiting, necessitating the application of an additional range or layer of psychotherapeutic competencies? Additionally the ACRA model does not focus explicitly on other psychological activities useful in the treatment of drug misuse such as the control and management of unhelpful cognitive styles or habits; breathing or progressive relaxation skills; anger management; imagery, visualisation and mindfulness. That is, as a manual based approach comprising a number of fixed components, a major potential challenge facing clinicians and students is the tension they may experience between maintaining strict fidelity to a pure ACRA approach, versus the flexibility l approved by more formulation driven CBT approaches?
The advantages of a skilled application of a formulation driven approach which are cited and summarised in are multiple and include the collaborative nature of goal setting, the facilitation of problem prioritisation in a meaningful and useful manner; a more immediate direction and structuring of the course of treatment; the provision of a rationale for the most fitting intervention point or spotlight for the treatment; an integration of seemingly unrelated or dissimilar difficulties in a meaningful yet parsimonious fashion; an influence on the choice of procedures and “homework” exercises; theory based mechanisms to understand the dynamics of the therapeutic relationship and a sense of targeted and ‘extra-therapeutic’ issues and how they could be best explained and managed, especially in terms of precipitators or triggers, core beliefs, assumptions and automatic thoughts.
Thus given the above observations and together with the importance placed on engagement and retention, the high variability in the cognitive, emotional, social and developmental domains [4] differences in roles (e.g. teenagers who are also parents) and levels of autonomy as well as high degrees of dual diagnosis or co- morbidities found in this group [29 , 30] practitioners are encouraged to also develop competencies in allied psychological treatment models such as Motivational Interviewing [31] ; familiarity with the core principles of CBT, disorder specific and problem-specific CBT competences, the generic and meta- competences of CBT as well as an advanced knowledge and understanding of mental health problems that will provide practitioners with the confidence and capacity to implement treatment models in a more flexible yet coherent manner,. In addition to seeking supervision and mentorship students and practitioners are directed, as a starting point, to University College London’s excellent resources outlining the competencies required to provide a more comprehensive interventions [11] .
Both authors reported no conflict of interest in the content of this paper.
Author Contributions
Conceived and designed the experiments: JI. Recruitment & assessment and on going treatment t of patient JI. On going supervision of case KD. Contributed reagents/materials/analysis tools: JI, & KD. Wrote the paper: JI. Contributed to final draft paper KD.
Acknowledgments
We thank Adolescent Addiction Services, Health Service Executive.
- Compton WM, Thomas YF, Stinson FS, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 64: 566-576. View
- Hasin DS, Stinson FS, Ogburn E, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 64: 830-842. View
- Carroll KM, Nich C, Ball SA, McCance E, Frankforter TL, et al. (2000) Oneyear follow-up of disulfiram and psychotherapy for cocaine-alcohol users: sustained effects of treatment. Addiction 95: 1335-1349. View
- Stetler CB, Ritchie J, Rycroft-Malone J, Schultz A, Charns M (2007) Improving quality of care through routine, successful implementation of evidence-based practice at the bedside: an organizational case study protocol using the Pettigrew and Whipp model of strategic change. Imp Sci 2: 1-13. View
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, et al. (2004) Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients: a randomized placebo-controlled trial. Arch Gen Psychiatry 61: 264-272. View
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, et al. (2008) Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry 165: 881-888. View
- McHugh RK, Hearon BA, Otto MW (2010) Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am 33: 511-525. View
- Waldron HB, Kaminer Y (2004) On the learning curve: the emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction 99 Suppl 2: 93-105. View
- Freeman A, Reinecke MA (1995) Cognitive therapy. New York: Guilford Press.
- Stephens RS, Babor TF, Kadden R, Miller M; Marijuana Treatment Project Research Group (2002) The Marijuana Treatment Project: rationale, design and participant characteristics. Addiction 97 Suppl 1: 109-124. View
- Pilling S, Hesketh K, Mitcheson L (2009) Psychosocial interventions in drug misuse: a framework and toolkit for implementing NICE-recommended treatment interventions. London: British Psychological Society, Centre for Outcomes, Research and Effectiveness (CORE) Research Department of Clinical, Educational and Health Psychology, University College. View
- Azrin NH (1976) Improvements in the community-reinforcement approach to alcoholism. Behav Res Ther 14: 339-348. View
- Hunt GM, Azrin NH (1973) A community-reinforcement approach to alcoholism. Behav Res Ther 11: 91-104. View
- Azrin NH, Sisson RW, Meyers R, Godley M (1982) Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiatry 13: 105-112. View
- Meyers RJ, Miller WR (2001) A community reinforcement approach to addiction treatment: (International Research Monographs in the Addictions) Cambridge Univ Press.
- Mallams JH, Godley MD, Hall GM, Meyers RJ (1982) A social-systems approach to resocializing alcoholics in the community. J Stud Alcohol 43: 1115-1123.
- Finney JW, Monahan SC (1996) The cost-effectiveness of treatment for alcoholism: a second approximation. J Stud Alcohol 57: 229-243. View
- Rollnick S, Miller WR (1999) What is motivational interviewing? Behav Cogn Psychotherapy. 23: 325-334. View
- Garner BR, Barnes B, Godley SH (2009) Monitoring fidelity in the Adolescent Community Reinforcement Approach (A-CRA): the training process for A-CRA raters. J Behav Anal Health Fit Med 2: 43-54. View
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, et al. (2004) The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat 27: 197-213. View
- Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH (2007) The impact of continuing care adherence on environmental risks, substance use, and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 21: 488-497. View
- Slesnick N, Prestopnik JL, Meyers RJ, Glassman M (2007) Treatment outcome for street-living, homeless youth. Addict Behav 32: 1237-1251. View
- Beck AT, Hollon SD, Young JE, Bedrosian RC, Budenz D (1985) Treatment of depression with cognitive therapy and amitriptyline. Arch Gen Psychiatry 42: 142-148. View
- Smith C (1998) Assessing health needs in women's prisons. PSJ 224.
- Maude-Griffin PM1, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, et al. (1998) Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol 66: 832-837. View
- Godley SH, Meyers RJ, Smith JE, Karvinen T, Titus JC, et al. (2001) The adolescent community reinforcement approach for adolescent cannabis users: US Department of Health and Human Services. View
- Carroll KM (1998) A cognitive-behavioral approach: Treating cocaine addiction. National Institute on Drug Abuse. View
- Bukstein OG, Glancy LJ, Kaminer Y (1992) Pattern of affective comorbidity in a clinical population of dually diagonised adolescent substance abusers. J Ame Aca Child Adol Psychiat 31: 1041-1045. View
- Kaminer Y, Burleson JA, Goldberger R (2002) Psychotherapies for adolescent substance abusers: Short- and long-term outcomes. J Nerv Ment Dis 190: 737-745.
- Miller WR, Rollnick S (2002) Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press. View
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
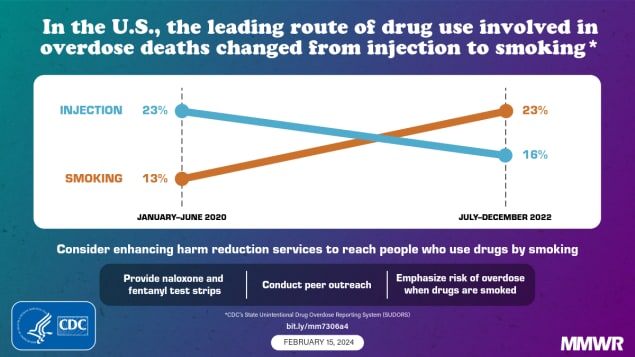
Routes of Drug Use Among Drug Overdose Deaths — United States, 2020–2022
Weekly / February 15, 2024 / 73(6);124–130
Lauren J. Tanz, ScD 1 ; R. Matt Gladden, PhD 1 ; Amanda T. Dinwiddie, MPH 1 ; Kimberly D. Miller, MPH 1 ; Dita Broz, PhD 2 ; Eliot Spector, MS 1 ,3 ; Julie O’Donnell, PhD 1 ( View author affiliations )
What is already known about this topic?
More than 109,000 drug overdose deaths occurred in the United States in 2022; nearly 70% involved illegally manufactured fentanyls (IMFs). Data from the western United States suggested a transition from injecting heroin to smoking IMFs.
What is added by this report?
From January–June 2020 to July–December 2022, the percentage of overdose deaths with evidence of smoking increased 73.7%, and the percentage with evidence of injection decreased 29.1%; similar changes were observed in all U.S. regions. Changes were most pronounced in deaths with IMFs detected, with or without stimulant detection.
What are the implications for public health practice?
Strengthening and expanding public health and harm reduction services to address overdose risk with smoking and other noninjection routes might reduce deaths.
- Article PDF
- Full Issue PDF
Preliminary reports indicate that more than 109,000 drug overdose deaths occurred in the United States in 2022; nearly 70% of these involved synthetic opioids other than methadone, primarily illegally manufactured fentanyl and fentanyl analogs (IMFs). Data from the western United States suggested a transition from injecting heroin to smoking IMFs. CDC analyzed data from the State Unintentional Drug Overdose Reporting System to describe trends in routes of drug use in 27 states and the District of Columbia among overdose deaths that occurred during January 2020–December 2022, overall and by region and drugs detected. From January–June 2020 to July–December 2022, the percentage of overdose deaths with evidence of injection decreased 29.1%, from 22.7% to 16.1%, whereas the percentage with evidence of smoking increased 73.7%, from 13.3% to 23.1%. The number of deaths with evidence of smoking increased 109.1%, from 2,794 to 5,843, and by 2022, smoking was the most commonly documented route of use in overdose deaths. Trends were similar in all U.S. regions. Among deaths with only IMFs detected, the percentage with evidence of injection decreased 41.6%, from 20.9% during January–June 2020 to 12.2% during July–December 2022, whereas the percentage with evidence of smoking increased 78.9%, from 10.9% to 19.5%. Similar trends were observed among deaths with both IMFs and stimulants detected. Strengthening public health and harm reduction services to address overdose risk related to diverse routes of drug use, including smoking and other noninjection routes, might reduce drug overdose deaths.
Introduction
Preliminary data indicate that U.S. drug overdose deaths surpassed 109,000 in 2022; nearly 70% of these deaths involved synthetic opioids other than methadone, primarily illegally manufactured fentanyl and fentanyl analogs (IMFs).* In recent years, deaths co-involving IMFs and stimulants have increased steadily ( 1 ). The estimated number of U.S. adults who inject drugs increased from approximately 774,000 in 2011 to nearly 3.7 million in 2018, corresponding to shifts from prescription opioid misuse to the use of heroin and IMFs ( 2 ). More recent data suggest transitions from injecting heroin to smoking IMFs; however, limited data exist on recent changes in routes of drug use for all drugs, and for IMFs beyond the western United States † ( 3 , 4 ). Routes of drug use have implications for overdose risk, infectious disease transmission, other comorbidities, and harm reduction services ( 5 ).
Jurisdictions entered data from death certificates, postmortem toxicology testing, and medical examiner or coroner reports on unintentional and undetermined intent drug overdose deaths into CDC’s State Unintentional Drug Overdose Reporting System (SUDORS). § Routes of drug use were identified using information from scene investigations, witness reports, or autopsy data and were categorized into nonmutually exclusive categories of ingestion, ¶ injection,** smoking, †† and snorting §§ ; other routes (e.g., transdermal) are not presented because sample sizes were small. Among 28 jurisdictions ¶¶ with complete data,*** numbers and percentages of overdose deaths were calculated by route of drug use and by 6-month period during January 2020–December 2022, overall, and for each U.S. Census Bureau region. ††† To understand how routes of drug use are related to drugs commonly involved in overdose deaths, percentages of overdose deaths with evidence of each route were calculated by 6-month period for mutually exclusive categories of drugs detected (IMFs §§§ only, stimulants only, both IMFs and stimulants, and neither IMFs nor stimulants) ¶¶¶ ( 6 ). Analyses were performed using SAS software (version 9.4; SAS Institute). This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.****
Overall Trends
During January 2020–December 2022, a total of 139,740 overdose deaths occurred in 28 jurisdictions; deaths increased 20.2%, from 21,046 during January–June 2020 to 25,301 during July–December 2022. The percentage of deaths with IMFs detected increased 8.4% from 71.4% during January–June 2020 to 77.4% during July–December 2022. Evidence of at least one route of drug use was documented in 71,480 (51.2%) overdose deaths. From January–June 2020 to July–December 2022, the number and percentage of overdose deaths with evidence of smoking increased 109.1% (from 2,794 to 5,843) and 73.7% (from 13.3% to 23.1%), respectively ( Figure 1 ). The number and percentage of deaths with evidence of snorting increased 43.1% (from 2,858 to 4,090) and 19.1% (from 13.6% to 16.2%), respectively. In contrast, the number and percentage of overdose deaths with evidence of injection decreased 14.6% (from 4,780 to 4,080) and 29.1% (from 22.7% to 16.1%), respectively, from January–June 2020 to July–December 2022. Although the number of deaths with evidence of ingestion increased 14.6%, from 3,189 to 3,656, the percentage of such deaths declined 4.6%, from 15.2% to 14.5%.
The leading route of use in drug overdose deaths changed from injection during January–June 2020 (22.7% of deaths) compared with ingestion (15.2%), snorting (13.6%), and smoking (13.3%) to smoking during July–December 2022 (23.1% of deaths) compared with snorting (16.2%), injection (16.1%), and ingestion (14.5%). During July–December 2022, most deaths with evidence of smoking (79.7%), snorting (84.5%), or ingestion (86.5%) had no evidence of injection; among deaths with information on route of use, 81.9% had evidence of a noninjection route.
Regional Trends
Regional trends were largely consistent with overall trends. The percentage of overdose deaths with evidence of smoking increased in all U.S. Census Bureau regions (Northeast: 91.0% increase, from 8.9% to 17.0%; Midwest: 75.0%, from 12.4% to 21.7%; South: 48.0%, from 12.5% to 18.5%; and West: 68.9%, from 25.1% to 42.4%) ( Figure 2 ). The percentage of deaths with evidence of snorting increased in three regions (Northeast: 28.2%, from 11.7% to 15.0%; Midwest: 23.0%, from 13.9% to 17.1%; and South: 12.4%, from 14.5% to 16.3%). The percentage with evidence of injection decreased in all regions (Northeast: −21.2%, from 21.2% to 16.7%; Midwest: −36.2%, from 21.8% to 13.9%; South: −27.8%, from 25.9% to 18.7%; and West: −34.3%, from 19.8% to 13.0%). By July–December 2022, smoking was the most commonly identified route of use in overdose deaths in the Midwest (21.7%) and West (42.4%); injection and smoking were most common in the Northeast (16.7% and 17.0%, respectively) and South (18.7% and 18.5%, respectively).
Trends by Drugs Detected
Among overdose deaths with only IMFs detected (13,107; 9.6%), deaths with both IMFs and stimulants detected (58,754; 43.1%), and deaths with only stimulants detected (8,525; 6.2%), the percentage with evidence of smoking increased, and the percentage with evidence of injection decreased from January–June 2020 to July–December 2022 ( Figure 3 ). For IMFs only, the percentage of overdose deaths with evidence of smoking increased 78.9%, from 10.9% to 19.5%, whereas the percentage with evidence of injection decreased 41.6%, from 20.9% to 12.2%. Among deaths with both IMFs and stimulants detected, the percentage with evidence of smoking increased 65.4%, from 17.9% to 29.6%, whereas the percentage with evidence of injection decreased 25.5%, from 28.6% to 21.3%. A similar pattern was observed among deaths with only stimulants detected (smoking: 29.7% increase, from 15.5% to 20.1%; injection: 22.5% decrease, from 10.2% to 7.9%). Among deaths with neither IMFs nor stimulants detected (10,628; 7.8%), the percentage with evidence of smoking did not change, and the percentage with evidence of injection decreased 42.2% (11.6% to 6.7%); ingestion was the most common route during July–December 2022 (39.4% of deaths) and throughout the study period.
The percentage of drug overdose deaths with evidence of smoking increased sharply in all U.S. regions from 2020 to 2022, indicating the importance of an updated response. By late 2022, among decedents with information on route of drug use, more than three fourths had evidence of a noninjection route, highlighting the diversification of methods through which they used drugs.
From January–June 2020 to July–December 2022, the number of overdose deaths with evidence of smoking doubled, and the percentage of deaths with evidence of smoking increased across all geographic regions. By late 2022, smoking was the predominant route of use among drug overdose deaths overall and in the Midwest and West regions. Increases were most pronounced when IMFs were detected, with or without stimulants. Increases in the number and percentage of deaths with evidence of smoking, and the corresponding decrease in those with evidence of injection, might be partially driven by 1) the transition from injecting heroin to smoking IMFs ( 3 , 4 ), 2) increases in deaths co-involving IMFs and stimulants that might be smoked †††† ( 1 ), and 3) increases in the use of counterfeit pills, which frequently contain IMFs and are often smoked ( 7 ). Motivations for transitioning from injection to smoking include fewer adverse health effects (e.g., fewer abscesses), reduced cost and stigma, sense of more control over drug quantity consumed per use (e.g., smoking small amounts during a period versus a single injection bolus), and a perception of reduced overdose risk among persons who use drugs ( 3 , 5 , 8 ). These motivations might also signify lower barriers for initiating drug use by smoking, or for transitioning from ingestion to smoking; compared with ingestion, smoking can intensify drug effects and increase overdose risk ( 9 ). Despite some risk reduction associated with smoking compared with injection (e.g., fewer bloodborne infections), smoking carries substantial overdose risk because of rapid drug absorption ( 5 , 9 ).
Nearly 80% of overdose deaths with evidence of smoking had no evidence of injection; persons who use drugs by smoking but do not inject drugs might not use traditional syringe services programs where harm reduction messaging and supplies are often provided. In response, some jurisdictions have adapted harm reduction services to provide safer smoking supplies or established health hubs to expand reach to persons using drugs through noninjection routes. §§§§ In addition, harm reduction services (e.g., peer outreach and provision of fentanyl test strips for testing drug products and naloxone to reverse opioid overdoses), messaging specific to smoking drugs, and linkage to treatment for substance use disorders can be integrated into other health care delivery (e.g., emergency departments) and public safety (e.g., drug diversion) settings.
The percentage and number of deaths with evidence of injection decreased across regions and drug categories. Observed decreases might reflect transitions to noninjection routes and response to public health efforts to reduce injection drug use because of its risk for overdose and infectious disease transmission ( 3 , 4 , 10 ). Despite these declines, more than 4,000 drug overdose deaths had evidence of injection during July–December 2022. Syringe services programs help to engage persons who use drugs in services ( 10 ); sustained efforts to provide sterile injection supplies, additional harm reduction tools, and linkage to treatment for substance use disorders, including medications for opioid use disorder, are important for further reduction in the number of overdose deaths from injection drug use. Lessons learned from implementing syringe services programs could be applied to other harm reduction and outreach models to reach more persons who use drugs by any route.
Limitations
The findings in this report are subject to at least four limitations. First, analyses included 28 jurisdictions; results might not be generalizable to the rest of the United States. Second, for nearly one half of deaths, no information about route of drug use was available; thus, percentages of deaths with evidence of each route are underestimated. However, no notable differences by time or demographic characteristics among deaths with and without route of drug use information were identified. Third, percentages of noninjection routes are likely underestimated more than those with injection because evidence of injection is easier to identify (e.g., syringes) than evidence of other routes (e.g., stems and straws can be evidence of snorting or smoking). Finally, routes could not be linked to the use of a specific drug unless only one drug class was detected. Analyses of single drug classes detected (IMFs only and stimulants only) were presented to better link routes to drugs.
Implications for Public Health Practice
Routes of drug use have implications for overdose risk, infectious disease transmission, and harm reduction services ( 5 ). Although unsafe injection drug use practices might be most risky in terms of infectious disease transmission, other routes, particularly smoking, still carry substantial overdose risk ( 9 ). Sharp increases in deaths with evidence of smoking and continued prevalence of other routes of drug use highlight the importance of 1) expanded messaging emphasizing overdose risk associated with smoking and other routes; 2) continued and expanded support for syringe services programs to provide comprehensive, integrated health services; and 3) enhanced outreach and harm reduction services (e.g., peer outreach and provision of fentanyl test strips and naloxone) across multiple settings for persons using drugs by smoking and other routes. These strategies might increase access to lifesaving services for persons who use drugs through all routes.
Acknowledgments
Jurisdictions participating in CDC’s Overdose Data to Action (OD2A) and Overdose Data to Action in States (OD2A-States) programs and providing data to the State Unintentional Drug Overdose Reporting System, including state and jurisdictional health departments, vital records offices, and medical examiner and coroner offices; CDC OD2A and OD2A-States teams, Division of Overdose Prevention, National Center for Injury Prevention and Control, CDC.
Corresponding author: Lauren J. Tanz, [email protected] .
1 Division of Overdose Prevention, National Center for Injury Prevention and Control, CDC; 2 Division of HIV Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, CDC; 3 Oak Ridge Institute for Science and Education, Oak Ridge, Tennessee.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm (Accessed January 11, 2024).
† https://adai.uw.edu/wordpress/wp-content/uploads/dlm_uploads/FentanylQualitativeReport2023.pdf
§ https://www.cdc.gov/drugoverdose/fatal/sudors.html
¶ Evidence of ingestion included witness reports of taking pills or tablets orally or ingesting liquid orally (e.g., liquid methadone), or the discovery of prescription pills, prescription bottles, liquid substances, or vials for containing liquid substances at the scene of the overdose or on the decedent’s body.
** Evidence of injection included witness reports of injecting drugs, items used to prepare and inject substances found at the scene (e.g., needles, cookers, filters, tourniquets, or alcohol pads), or track marks found on the decedent that appeared to be recent.
†† Evidence of smoking included witness reports of smoking drugs or drug paraphernalia at the overdose scene associated with smoking (e.g., pipes, stems, aluminum foil, vape pens, matches, disposable lighters, or gas torches). Fewer than 6.0% of deaths with evidence of smoking had vape pens or e-cigarettes endorsed as evidence; fewer than 3.0% had vape pens or e-cigarettes endorsed with no other evidence of smoking.
§§ Evidence of snorting included witness reports of snorting drugs, drug paraphernalia at the overdose scene associated with snorting (e.g., razor blades or credit cards used to chop and separate powder; straws, rolled paper, dollar bills, or tubes for nasal inhalation; or powder visible on a table or mirror), or powder on the decedent’s nose.
¶¶ Alaska, Arizona, Colorado, Connecticut, Delaware, District of Columbia, Georgia, Illinois, Kansas, Kentucky, Maine, Maryland, Massachusetts, Minnesota, Nebraska, New Hampshire, New Jersey, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Utah, Vermont, Virginia, Washington, and West Virginia. Illinois and Washington reported deaths from counties that accounted for ≥75% of drug overdose deaths in the respective state in 2017, per SUDORS funding requirements; all other jurisdictions reported deaths from the full jurisdiction.
*** Jurisdictions were included if medical examiner or coroner reports and toxicology reports were available for ≥75% of deaths during January 2020–December 2022. Analyses were restricted to decedents with an available medical examiner or coroner report (139,740; 95.8% of all deaths).
††† U.S. Census Bureau regions were used to stratify jurisdictions into geographic regions ( https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf ). Region analysis included eight of nine jurisdictions in the Northeast Region, five of 12 jurisdictions in the Midwest Region, nine of 17 jurisdictions in the South Region, and six of 13 jurisdictions in the West Region.
§§§ Fentanyl was classified as likely illegally manufactured using toxicology, scene, and witness evidence. For the 8.1% of deaths involving fentanyl that had insufficient evidence for classification as illegal or prescription, fentanyl was classified as illegal because the majority of fentanyl overdose deaths involve illegal fentanyl. All fentanyl analogs except alfentanil, remifentanil, and sufentanil, which have legitimate human medical use, were included as IMFs.
¶¶¶ Analysis of drugs detected was restricted to decedents with an available toxicology report (136,466; 97.7% of deaths with a medical examiner or coroner report).
**** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
†††† https://adai.uw.edu/wordpress/wp-content/uploads/SaferSmokingBrief_2022.pdf
§§§§ https://www.maricopa.gov/DocumentCenter/View/86245/OUD-SUD-Needs-Assessment-Final-Report?bidId= ; https://www.cdph.ca.gov/Programs/CID/DOA/CDPH%20Document%20Library/HR_Supplies_Clearinghouse_Factsheet_FINAL.pdf ; https://www.health.ny.gov/diseases/aids/consumers/prevention/
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep 2021;70:202–7. https://doi.org/10.15585/mmwr.mm7006a4 PMID:33571180
- Bradley H, Hall EW, Asher A, et al. Estimated number of people who inject drugs in the United States. Clin Infect Dis 2023;76:96–102. https://doi.org/10.1093/cid/ciac543 PMID:35791261
- Kral AH, Lambdin BH, Browne EN, et al. Transition from injecting opioids to smoking fentanyl in San Francisco, California. Drug Alcohol Depend 2021;227:109003. https://doi.org/10.1016/j.drugalcdep.2021.109003 PMID:34482046
- Valasek CJ, Streuli SA, Pines HA, et al. “A lotta people switched playing hard ball to playing Russian roulette”: experiences with rising overdose incidence caused by drug supply changes during the COVID-19 pandemic in the San Diego-Tijuana border metroplex. Drug Alcohol Depend Rep 2023;7:100154. https://doi.org/10.1016/j.dadr.2023.100154 PMID:37089868
- Megerian CE, Bair L, Smith J, et al. Health risks associated with smoking versus injecting fentanyl among people who use drugs in California. Drug Alcohol Depend 2024;255:111053. https://doi.org/10.1016/j.drugalcdep.2023.111053 PMID:38128362
- O’Donnell J, Gladden RM, Kariisa M, Mattson CL. Using death scene and toxicology evidence to define involvement of heroin, pharmaceutical morphine, illicitly manufactured fentanyl and pharmaceutical fentanyl in opioid overdose deaths, 38 states and the District of Columbia, January 2018–December 2019. Addiction 2022;117:1483–90. https://doi.org/10.1111/add.15768 PMID:34882865
- O’Donnell J, Tanz LJ, Miller KD, et al. Drug overdose deaths with evidence of counterfeit pill use—United States, July 2019–December 2021. MMWR Morb Mortal Wkly Rep 2023;72:949–56. https://doi.org/10.15585/mmwr.mm7235a3 PMID:37651284
- LaForge K, Stack E, Shin S, et al. Knowledge, attitudes, and behaviors related to the fentanyl-adulterated drug supply among people who use drugs in Oregon. J Subst Abuse Treat 2022;141:108849. https://doi.org/10.1016/j.jsat.2022.108849 PMID:35932759
- Howland M. Pharmacokinetic and toxicokinetic principles [Chapter 9]. In: Nelson LS, Howland M, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, eds. Goldfrank’s toxicologic emergencies, 11th ed. New York, NY: McGraw Hill; 2019.
- Broz D, Carnes N, Chapin-Bardales J, et al. Syringe services programs’ role in ending the HIV epidemic in the U.S.: why we cannot do it without them. Am J Prev Med 2021;61(Suppl 1):S118–29. https://doi.org/10.1016/j.amepre.2021.05.044 PMID:34686281
FIGURE 1 . Number and percentage of drug overdose deaths with evidence of selected routes of drug use, * , † by 6-month period of death (N = 139,740) — State Unintentional Drug Overdose Reporting System, 28 jurisdictions, § , ¶ January 2020–December 2022
Abbreviation: SUDORS = State Unintentional Drug Overdose Reporting System.
* Percentages with evidence of other routes (i.e., buccal, sublingual, suppository, or transdermal) (583; 0.4%) are not presented because of small sample sizes; decedents with drug use via these routes are included in the denominators. In addition, percentages of decedents with no information on route (68,260; 48.8%) are not shown; these decedents are also included in the denominators.
† Routes of drug use are not mutually exclusive; decedents might have used multiple routes.
§ Alaska, Arizona, Colorado, Connecticut, Delaware, District of Columbia, Georgia, Illinois, Kansas, Kentucky, Maine, Maryland, Massachusetts, Minnesota, Nebraska, New Hampshire, New Jersey, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Utah, Vermont, Virginia, Washington, and West Virginia. Illinois and Washington reported deaths from counties that accounted for ≥75% of drug overdose deaths in the respective state in 2017, per SUDORS funding requirements; all other jurisdictions reported deaths from the full jurisdiction.
¶ Jurisdictions were included if medical examiner or coroner reports and toxicology reports were available for ≥75% of deaths during January 2020–December 2022. Analysis was restricted to deaths with an available medical examiner or coroner report (139,740; 95.8% of all deaths).
FIGURE 2 . Percentage of drug overdose deaths with evidence of selected routes of drug use,* by U.S. Census Bureau region † and 6-month period of death (N = 139,740) — State Unintentional Drug Overdose Reporting System, 28 jurisdictions, § January 2020–December 2022
* Percentages with evidence of other routes (i.e., buccal, sublingual, suppository, or transdermal) are not presented because of small sample sizes (Panel A [Northeast]: 136, 0.4%; Panel B [Midwest]: 121, 0.4%; Panel C [South]: 223, 0.5%; and Panel D [West]: 103, 0.5%); decedents with drug use via these routes are included in the denominators. In addition, percentages of decedents with no information on route are not shown (Panel A: 22,541, 58.4%; Panel B: 15,381, 50.3%; Panel C: 22,571, 47.3%; and Panel D: 7,767, 34.0%); these decedents are also included in the denominators.
† Analysis included some, but not all, of the jurisdictions in each U.S. Census Bureau region. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, Pennsylvania, Rhode Island, and Vermont; Midwest: Illinois, Kansas, Minnesota, Nebraska, and Ohio; South: Delaware, District of Columbia, Georgia, Kentucky, Maryland, North Carolina, Oklahoma, Virginia, and West Virginia; West: Alaska, Arizona, Colorado, Oregon, Utah, and Washington.
§ Jurisdictions were included if medical examiner or coroner reports and toxicology reports were available for ≥75% of deaths during January 2020–December 2022. Analysis was restricted to deaths with an available medical examiner or coroner report (139,740; 95.8% of all deaths).
FIGURE 3 . Percentage of drug overdose deaths with evidence of selected routes of drug use,* by drugs detected † , § , ¶ , ** , †† and 6-month period of death — State Unintentional Drug Overdose Reporting System, 28 jurisdictions, §§ January 2020–December 2022
Abbreviations: IMFs = illegally manufactured fentanyls; SUDORS = State Unintentional Drug Overdose Reporting System.
* Percentages with evidence of other routes (i.e., buccal, sublingual, suppository, or transdermal) are not presented because of small sample sizes (Panel A [IMFs only]: 23, 0.2%; Panel B [Stimulants only]: 11, 0.1%; Panel C [IMFs and stimulants]: 146, 0.2%; and Panel D [Neither IMFs nor stimulants]: 158, 1.5%); decedents with drug use via these routes are included in the denominators. In addition, percentages of decedents with no information on route are not shown (Panel A: 6,802, 51.9%; Panel B: 5,652, 66.3%; Panel C: 25,597, 43.6%; and Panel D: 5,435, 51.1%); these decedents are also included in the denominators.
† Data on drugs detected come from postmortem toxicology reports; among decedents with a medical examiner or coroner report, analysis was further restricted to decedents with a toxicology report (136,466; 97.7% of decedents with a medical examiner or coroner report).
§ Ethanol and other selected drugs (e.g., naloxone and cotinine) were not considered a drug for this analysis; deaths categorized as IMFs only (Panel A) or stimulant only (Panel B) might have also had ethanol or these other selected drugs detected.
¶ Deaths with IMFs and stimulants detected (Panel C) could also have other drugs detected (e.g., prescription opioids).
** Deaths with neither IMFs nor stimulants detected primarily had prescription opioids (65.3%) or benzodiazepines (37.3%) detected.
†† Drug categories are not comprehensive; some deaths are excluded because they contain drug combinations that are not presented in the panels (e.g., deaths with only IMFs and prescription opioids detected).
§§ Alaska, Arizona, Colorado, Connecticut, Delaware, District of Columbia, Georgia, Illinois, Kansas, Kentucky, Maine, Maryland, Massachusetts, Minnesota, Nebraska, New Hampshire, New Jersey, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Utah, Vermont, Virginia, Washington, and West Virginia. Illinois and Washington reported deaths from counties that accounted for ≥75% of drug overdose deaths in the respective state in 2017, per SUDORS funding requirements; all other jurisdictions reported deaths from the full jurisdiction.
Suggested citation for this article: Tanz LJ, Gladden RM, Dinwiddie AT, et al. Routes of Drug Use Among Drug Overdose Deaths — United States, 2020–2022. MMWR Morb Mortal Wkly Rep 2024;73:124–130. DOI: http://dx.doi.org/10.15585/mmwr.mm7306a2 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
- Skip to main content
- Keyboard shortcuts for audio player
Some Health Workers Suffering From Addiction Steal Drugs Meant For Patients

The federal government estimates one in 10 healthcare workers experience substance use disorder. There is rising concern that medical professionals are stealing powerful opioid pain medications meant for their patients. Kaz Fantone/NPR hide caption
The federal government estimates one in 10 healthcare workers experience substance use disorder. There is rising concern that medical professionals are stealing powerful opioid pain medications meant for their patients.
When Kristin Waite-Labott, a nurse in Wisconsin, began stealing fentanyl and morphine from her hospital's medical supply cabinets, she found it was relatively easy to cover her tracks.
Her drug inventory paperwork often didn't add up, but she found coworkers willing to cover for her.
"They trusted me" she said. "Unfortunately I was taking advantage of that trust and that happens all the time."
But Waite-Labott's addiction to fentanyl quickly spiraled out of control.

Doctors And Dentists Still Flooding U.S. With Opioid Prescriptions
"Taking it one time, I instantly craved more. It's so powerful and deadly," she said.
Waite-Labott eventually lost her job and spent time in jail before entering recovery and regaining her nursing license.
She works now helping other health workers who struggle with addiction and says she's still haunted by the thought of patients she might have harmed.
"I don't know that I made any errors," she said. "But I can't be certain of that because I was under the influence at work."
NPR found a growing number of health industry experts and researchers who warn this kind of on-the-job drug theft by health workers may be increasing.
"It's extremely common and the consequences can be very very grave," said Kimberly New, an expert on medical drug misuse, known in the industry as diversion.
Patients in pain, patients taking contaminated medications
Harm to patients from drug diversion can be severe. In extreme cases, health workers divert so much medication, patients wind up undergoing cancer treatments or post-surgical recovery without pain relief.
"Patients will be left to linger in pain and not receive the doses that they were supposed to receive," New said. "The diverter has progressed to the point where they're no longer willing to share with the patients."
Studies by the Centers for Disease Control and Prevention and the Mayo Clinic also found healthcare workers who steal drugs frequently tamper with medications, leaving them contaminated.
"I go and take a fentanyl vial, I administer the entire vial to myself and I refill the vial with water," New said, describing a typical scenario. "Unfortunately many patients have been infected with blood-born pathogens."
The Mayo Clinic study found as many as 28,000 hospital patients were put at risk of contracting Hepatitis C over a 10-year period because of this kind of drug theft and tampering.
Last year, physicians at a Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., reported six of their patients contracted a rare bacterial blood infection after a nurse replaced opioid medications with tap water.
"We share our experience to alert health care providers," the doctors wrote in The New England Journal of Medicine . "[I]n this age of profound prevalence of opioid addiction, drug diversion is an important consideration when a cluster of waterborne bacteremia is identified."
For doctors and nurses, lives destroyed and careers ended
Consequences for healthcare workers can also be devastating. Two years ago, Denise Keller got a call from the University of Texas Southwest Medical Center in Dallas where her daughter Iyesha worked as a nurse.
"When I first heard from the hospital, they were like, there's an accident," Keller recalled.
Iyesha Keller, who was 36, had overdosed on a variety of drugs, including fentanyl, likely stolen from her hospital's supply of pain medication.
"She died on the floor of a bathroom at her hospital. If all this was in her system how did she do her job?" Denise Keller asked.

Shots - Health News
To stop deadly overdoses, 'the opioid fix' urges better use of tools we already have.
Iyesha Keller was the second nurse to die from a fentanyl overdose at UT Southwestern Medical Center over a two-year period.
Last year, a nurse at Parker Adventist Hospital in Denver was sentenced to 44 months in federal prison after she stole fentanyl from her facility's intensive care unit, replacing doses of medication with saline.
In that case, the hospital's automated drug inventory system identified the theft. But experts told NPR many healthcare facilities still lack proper controls and security systems needed to spot drug diversion.
Only "a fraction" of hospital drug thefts are discovered
In one case at a hospital in Massachusetts , two nurses were able to steal more than 16,000 Oxycodone opioid pills before being detected. Another hospital, Effingham Health System in Atlanta paid $4.3 million in federal fines after "tens of thousands" of opioid medications were stolen over a four-year period.
"Hospitals put lives at risk when they fail to maintain accurate record-keeping of their inventory," the Drug Enforcement Agency's Robert J. Murphy said in a 2018 statement .
The frequency of drug diversion in hospitals and clinics is debated but last year the Joint Commission, a nonprofit that provides accreditation to thousands of hospitals and clinics, issued a warning that "only a fraction of those who are diverting drugs are ever caught."
This summer Kit Check, a company that monitors drug inventories at hundreds of U.S. hospitals, raised another red flag.
Coronavirus Pandemic Compounds Another Ongoing Crisis: The Opioid Epidemic
They issued a report showing tens of thousands of unexplained "variances" where high risk medications couldn't be accounted for by healthcare facilities.
"There's a 111,000 instances here where the folks that were reviewing [drug inventories] could not figure out why the math didn't add up," said Kit Check CEO Kevin MacDonald.
All hospitals and clinics are required by federal law to have some kind of security and inventory system for opioids and other controlled medications. But Mark Fan, a researcher at North York General Hospital in Toronto says those systems often break down.
"We know that staff are really overworked, they're under a lot of time pressure. It's not uncommon for people to let things slide," Fan said.
He published a study in the Journal of Hospital Medicine last year warning that drug theft in U.S. hospitals appears to be "accelerating."
The DEA plays little direct role in hospital oversight
The DEA told NPR it investigated roughly 3,600 cases of alleged drug theft at healthcare facilities over the last five years, including 280 cases so far in 2020.
But Tim McDermott, the DEA's assistant administrator for diversion control, said his agency's attention is largely focused elsewhere.
"We don't spend a lot of time targeting hospital employees or clinic employees," he said. "That is not where our biggest problem is in the United States right now."
In sheer numbers, the thousands of overdose deaths caused each year by illegal street fentanyl pose a far deadlier risk than fentanyl and other opioids misused by workers within the healthcare industry.
McDermott said the DEA believes the overall rate of drug diversion within the healthcare industry remains "very low." But he acknowledged the DEA can't say with confidence how big the problem of hospital drug theft has become.
That's because hospitals and clinics are largely responsible for self-policing. If medical facilities don't detect and report a problem, the DEA and other law enforcement have little chance of learning about it.
"So it limits the ability of us as an agency to see diversion that is being done whether it's a a clinic, whether it's at a hospital," McDermott told NPR.
The DEA has reportedly opened an investigation into drug security practices at UT Southwestern Medical Center in Dallas, where nurse Iyesha Keller died of a a fentanyl overdose in 2018.
Federal officials declined to confirm a probe is underway and the hospital didn't respond to NPR's repeated phone calls and emails seeking comment.
But Keller's mom, Denise, said she hopes someone will find out what went wrong at her daughter's hospital and make things safer for staff and patients.
"This hospital is having deaths, medications are disappearing and no one is able to stop and do anything about it," Keller told NPR. "It doesn't make any sense."
Correction Oct. 5, 2020
In a previous version of this digital story, we misspelled Kevin MacDonald's last name as McDonald.
- health workers
- opioid abuse
- opioid addiction
Science, evidence-based facts, key to help end scourge of drug abuse: UN chief

Facebook Twitter Print Email
The world’s drug problem remains an urgent challenge that threatens to exacerbate COVID-19 pandemic impacts and hinder a healthy and inclusive recovery, warned the UN Secretary General ahead of The International Day Against Drug Abuse and Illicit Trafficking.
In a statement published on Friday, Antonio Guterres underscored that trusting science is the “hero and lesson of the pandemic”, and the same action based on evidence is crucial for the responses to drugs.
Worsening problem
The World Drug Report published this week by the UN Office on Drugs and Crime ( UNODC ) showed that drug related deaths have nearly doubled over the past decade. Moreover, 10% of HIV cases in 2019, were due to people injecting themselves with harmful substances.
The UN chief warned that although international cooperation has helped limit the proliferation of new psychoactive drugs, the problem is shifting to poorer regions where control systems are weaker.
Meanwhile, dark web drug sales continue to rise, and non-medical use of pharmaceuticals, including opioids, is expanding.
“ Drug trafficking and organized crime fuel and perpetuate cycles of violence and conflict. Armed groups and terrorists’ profit from the illicit drug trade, and the economic fallout of the COVID-19 pandemic has left millions of people even more vulnerable to drug crime and illicit crop cultivation”, Mr. Guterres underscored.
Invest in prevention
The Secretary General pointed out that investing in balanced prevention as well as control of drug use and drug use disorders produces solid returns such as lives saved, healthier populations, improved workforce participation and productivity, and reduced criminal justice costs.
“ Many of the risk factors associated with crime and violent behaviour are also drivers of drug use, and targeted efforts focusing on these overlapping dynamics - including childhood maltreatment and lack of social support - can help to strengthen prevention”, he said.
More partnerships and data
Public-private partnerships - with tech companies, postal and courier services, and shipping companies - represent an essential frontline response in the new fight against drug traffickers, who “are increasingly exploiting the legal cargo trade and postal services to move their illicit product”, added Mr. Guterres, underscoring that better data is also useful to identify trends and enable real-time monitoring of the trafficking routes.
The Secretary General urged Member States to listen to the science and take action, building on agreed international frameworks and drawing on UN support for health and justice initiatives.
He also reminded that greater cooperation and support are needed to help low-income countries take advantage of cutting edge anti-drug enforcement techniques.
‘Share facts on drugs and save lives’
The head of UNODC, Ms. Ghada Waly, echoed the UN chief’s call for leveraging trustworthy, scientific information and the power of community in influencing health choices and addressing the world drug problem.
“Drugs are destroying health and stealing futures, with drug use alone killing almost half a million people in 2019. Awareness of the risks and access to evidence-based treatment and care can help prevent such tragedies”, she said.
In a statement, Ms. Waly explained the theme of this year’s International Day: Share facts on drugs. Save lives . “It highlights the need for evidence-based approaches to equip the public, as well as health and service providers, and decision makers with the tools to inform choices and effective services”, she emphasized.
The campaign highlights key statistics and data drawn from UNODC’s yearly World Drug Report. Thus, providing facts and practical solutions to the current world drug problem, to attain a vision of health for all, based on science.
Ms. Waly urged governments to expand evidence-based prevention and treatment programmes, as well as monitoring and early warning mechanisms to help lower-income countries detect and counter new substances and use trends.
About the day
Through resolution 42/112 of 7 December 1987, the General Assembly decided to observe 26 June as the International Day against Drug Abuse and Illicit Trafficking as an expression of its determination to strengthen action and cooperation to achieve the goal of an international society free of drug abuse.
Supported each year by individuals, communities, and various organizations all over the world, this global observance aims to raise awareness of the major problem that illicit drugs represent to society.
- International Days

New Case Western Reserve University study reveals high risk of overdose deaths in Cuyahoga County among those using drugs when they’re alone
In Cuyahoga County, the stark reality of the opioid crisis is that most drug overdose victims die alone, with no one nearby to help.
A recent study , done in partnership with Case Western Reserve University and Cuyahoga County, highlights the critical need for “targeted harm-reduction strategies” in Northeast Ohio, where the opioid epidemic continues to claim lives at nearly twice the national average.
Those strategies include the distribution of Naloxone (an opioid antagonist that can reverse the effects of an overdose), and increasing the availability of medication-assisted treatment options and fentanyl test strips.
The research, using data from the Cuyahoga County Medical Examiner’s Office , examined overdose deaths between 2016 and 2020, focusing on people using drugs when they were alone.

The study revealed that a staggering 75% of overdose victims were using drugs alone, a behavior strongly associated with increased mortality. Key findings indicate that individuals using drugs alone were more likely to be at home and less likely to receive life-saving interventions like naloxone, said Daniel Flannery , the Dr. Semi J. and Ruth Begun Professor and director of the Begun Center for Violence Prevention Research and Education at CWRU’s Jack, Joseph and Morton Mandel School of Applied Social Sciences .
“Being informed is crucial—knowledge equips you to take action,” Flannery said. “It’s about reviving someone in need, and if that’s not possible, contacting emergency services immediately. The chances of a fatal outcome significantly increase when there’s no one around to help.”

New policies and community efforts must prioritize reaching individuals at risk of using alone to curb the devastating impact of the opioid crisis, said Vaishali Deo , research associate at the Begun Center and co-principal investigator in the research.
“Our findings underscore the urgent need for innovative harm-reduction strategies aimed at those most vulnerable—those using drugs alone,” Deo said. “Interventions must focus on reducing isolation and improving access to emergency medical care to prevent further loss of life.”
The research findings were published by the National Institutes of Health’s National Library of Medicine .
Additional insights
- In Cuyahoga County, from 2016 through 2020, there were 2,944 unintentional overdose deaths for those over 18 years old. That’s 54 deaths per 100,000 residents. The national average is 28 overdose deaths per 100,000 residents.
- The study further details the demographics and circumstances surrounding overdose deaths in Cuyahoga County from 2016 to 2020. Most were non-Hispanic (94.9%), white (72.2%) and male (71.3%), with a significant portion 35 to 64 years old. Most lived in the City of Cleveland. Over half attained at least a high school diploma.
- Toxicology reports revealed that synthetic opioids, specifically illicitly manufactured fentanyl, was present in 72.7% of the deaths. Cocaine and heroin were also significant contributors, found in 41.6% and 29.6% of cases, respectively. Nearly 80% of overdose deaths involved the use of multiple substances.
- Despite the presence of bystanders in more than half the cases, most victims (74.9%) were using drugs alone at the time of their fatal overdose, mainly at home. Emergency medical services responded to most of the incidents, yet over 60% of victims were pronounced dead at the scene—highlighting the critical timing needed for interventions like naloxone, which was administered in just 28.6% of the cases.
Deo and Flannery were joined in the research by Sarah Fulton, a research associate at the Begun Center, and Manreet K. Bhullar, a senior forensic epidemiologist at the Cuyahoga County Medical Examiner’s Office, and Thomas P. Gilson, chief medical examiner of Cuyahoga County.
“These findings paint a stark picture of the opioid crisis in our community,” Gilson said. “The tragic reality is that too many people are dying alone, and we must act swiftly to implement lifesaving measures that can prevent these unnecessary deaths.”
For more information, contact Colin McEwen at [email protected] .
- Open access
- Published: 13 November 2021
Risk and protective factors of drug abuse among adolescents: a systematic review
- Azmawati Mohammed Nawi 1 ,
- Rozmi Ismail 2 ,
- Fauziah Ibrahim 2 ,
- Mohd Rohaizat Hassan 1 ,
- Mohd Rizal Abdul Manaf 1 ,
- Noh Amit 3 ,
- Norhayati Ibrahim 3 &
- Nurul Shafini Shafurdin 2
BMC Public Health volume 21 , Article number: 2088 ( 2021 ) Cite this article
148k Accesses
113 Citations
20 Altmetric
Metrics details
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was adopted for the review which utilized three main journal databases, namely PubMed, EBSCOhost, and Web of Science. Tobacco addiction and alcohol abuse were excluded in this review. Retrieved citations were screened, and the data were extracted based on strict inclusion and exclusion criteria. Inclusion criteria include the article being full text, published from the year 2016 until 2020 and provided via open access resource or subscribed to by the institution. Quality assessment was done using Mixed Methods Appraisal Tools (MMAT) version 2018 to assess the methodological quality of the included studies. Given the heterogeneity of the included studies, a descriptive synthesis of the included studies was undertaken.
Out of 425 articles identified, 22 quantitative articles and one qualitative article were included in the final review. Both the risk and protective factors obtained were categorized into three main domains: individual, family, and community factors. The individual risk factors identified were traits of high impulsivity; rebelliousness; emotional regulation impairment, low religious, pain catastrophic, homework completeness, total screen time and alexithymia; the experience of maltreatment or a negative upbringing; having psychiatric disorders such as conduct problems and major depressive disorder; previous e-cigarette exposure; behavioral addiction; low-perceived risk; high-perceived drug accessibility; and high-attitude to use synthetic drugs. The familial risk factors were prenatal maternal smoking; poor maternal psychological control; low parental education; negligence; poor supervision; uncontrolled pocket money; and the presence of substance-using family members. One community risk factor reported was having peers who abuse drugs. The protective factors determined were individual traits of optimism; a high level of mindfulness; having social phobia; having strong beliefs against substance abuse; the desire to maintain one’s health; high paternal awareness of drug abuse; school connectedness; structured activity and having strong religious beliefs.
The outcomes of this review suggest a complex interaction between a multitude of factors influencing adolescent drug abuse. Therefore, successful adolescent drug abuse prevention programs will require extensive work at all levels of domains.
Peer Review reports
Introduction
Drug abuse is a global problem; 5.6% of the global population aged 15–64 years used drugs at least once during 2016 [ 1 ]. The usage of drugs among younger people has been shown to be higher than that among older people for most drugs. Drug abuse is also on the rise in many ASEAN (Association of Southeast Asian Nations) countries, especially among young males between 15 and 30 years of age. The increased burden due to drug abuse among adolescents and young adults was shown by the Global Burden of Disease (GBD) study in 2013 [ 2 ]. About 14% of the total health burden in young men is caused by alcohol and drug abuse. Younger people are also more likely to die from substance use disorders [ 3 ], and cannabis is the drug of choice among such users [ 4 ].
Adolescents are the group of people most prone to addiction [ 5 ]. The critical age of initiation of drug use begins during the adolescent period, and the maximum usage of drugs occurs among young people aged 18–25 years old [ 1 ]. During this period, adolescents have a strong inclination toward experimentation, curiosity, susceptibility to peer pressure, rebellion against authority, and poor self-worth, which makes such individuals vulnerable to drug abuse [ 2 ]. During adolescence, the basic development process generally involves changing relations between the individual and the multiple levels of the context within which the young person is accustomed. Variation in the substance and timing of these relations promotes diversity in adolescence and represents sources of risk or protective factors across this life period [ 6 ]. All these factors are crucial to helping young people develop their full potential and attain the best health in the transition to adulthood. Abusing drugs impairs the successful transition to adulthood by impairing the development of critical thinking and the learning of crucial cognitive skills [ 7 ]. Adolescents who abuse drugs are also reported to have higher rates of physical and mental illness and reduced overall health and well-being [ 8 ].
The absence of protective factors and the presence of risk factors predispose adolescents to drug abuse. Some of the risk factors are the presence of early mental and behavioral health problems, peer pressure, poorly equipped schools, poverty, poor parental supervision and relationships, a poor family structure, a lack of opportunities, isolation, gender, and accessibility to drugs [ 9 ]. The protective factors include high self-esteem, religiosity, grit, peer factors, self-control, parental monitoring, academic competence, anti-drug use policies, and strong neighborhood attachment [ 10 , 11 , 12 , 13 , 14 , 15 ].
The majority of previous systematic reviews done worldwide on drug usage focused on the mental, psychological, or social consequences of substance abuse [ 16 , 17 , 18 ], while some focused only on risk and protective factors for the non-medical use of prescription drugs among youths [ 19 ]. A few studies focused only on the risk factors of single drug usage among adolescents [ 20 ]. Therefore, the development of the current systematic review is based on the main research question: What is the current risk and protective factors among adolescent on the involvement with drug abuse? To the best of our knowledge, there is limited evidence from systematic reviews that explores the risk and protective factors among the adolescent population involved in drug abuse. Especially among developing countries, such as those in South East Asia, such research on the risk and protective factors for drug abuse is scarce. Furthermore, this review will shed light on the recent trends of risk and protective factors and provide insight into the main focus factors for prevention and control activities program. Additionally, this review will provide information on how these risk and protective factors change throughout various developmental stages. Therefore, the objective of this systematic review was to determine the risk and protective factors of drug abuse among adolescents worldwide. This paper thus fills in the gaps of previous studies and adds to the existing body of knowledge. In addition, this review may benefit certain parties in developing countries like Malaysia, where the national response to drugs is developing in terms of harm reduction, prison sentences, drug treatments, law enforcement responses, and civil society participation.
This systematic review was conducted using three databases, PubMed, EBSCOhost, and Web of Science, considering the easy access and wide coverage of reliable journals, focusing on the risk and protective factors of drug abuse among adolescents from 2016 until December 2020. The search was limited to the last 5 years to focus only on the most recent findings related to risk and protective factors. The search strategy employed was performed in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) checklist.
A preliminary search was conducted to identify appropriate keywords and determine whether this review was feasible. Subsequently, the related keywords were searched using online thesauruses, online dictionaries, and online encyclopedias. These keywords were verified and validated by an academic professor at the National University of Malaysia. The keywords used as shown in Table 1 .
Selection criteria
The systematic review process for searching the articles was carried out via the steps shown in Fig. 1 . Firstly, screening was done to remove duplicate articles from the selected search engines. A total of 240 articles were removed in this stage. Titles and abstracts were screened based on the relevancy of the titles to the inclusion and exclusion criteria and the objectives. The inclusion criteria were full text original articles, open access articles or articles subscribed to by the institution, observation and intervention study design and English language articles. The exclusion criteria in this search were (a) case study articles, (b) systematic and narrative review paper articles, (c) non-adolescent-based analyses, (d) non-English articles, and (e) articles focusing on smoking (nicotine) and alcohol-related issues only. A total of 130 articles were excluded after title and abstract screening, leaving 55 articles to be assessed for eligibility. The full text of each article was obtained, and each full article was checked thoroughly to determine if it would fulfil the inclusion criteria and objectives of this study. Each of the authors compared their list of potentially relevant articles and discussed their selections until a final agreement was obtained. A total of 22 articles were accepted to be included in this review. Most of the excluded articles were excluded because the population was not of the target age range—i.e., featuring subjects with an age > 18 years, a cohort born in 1965–1975, or undergraduate college students; the subject matter was not related to the study objective—i.e., assessing the effects on premature mortality, violent behavior, psychiatric illness, individual traits, and personality; type of article such as narrative review and neuropsychiatry review; and because of our inability to obtain the full article—e.g., forthcoming work in 2021. One qualitative article was added to explain the domain related to risk and the protective factors among the adolescents.
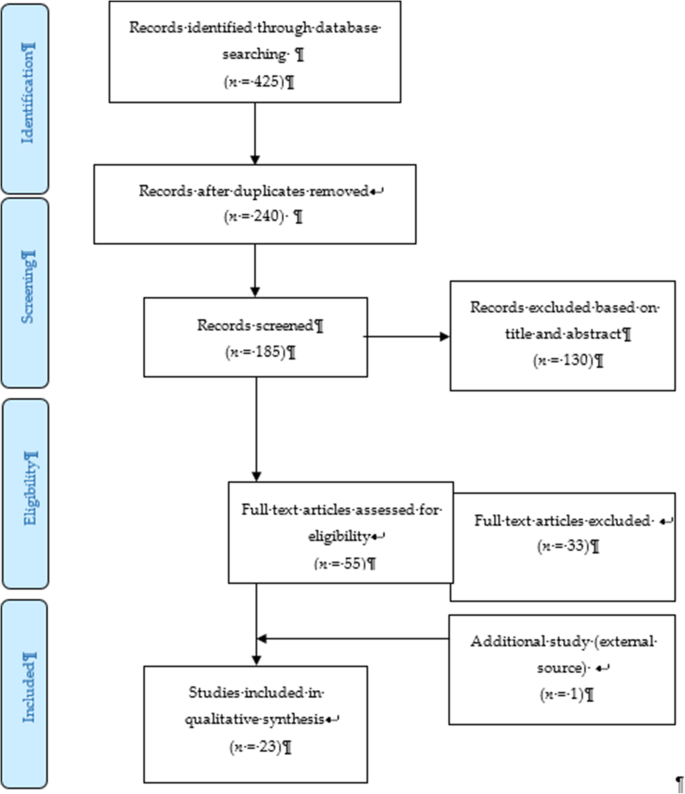
PRISMA flow diagram showing the selection of studies on risk and protective factors for drug abuse among adolescents.2.2. Operational Definition
Drug-related substances in this context refer to narcotics, opioids, psychoactive substances, amphetamines, cannabis, ecstasy, heroin, cocaine, hallucinogens, depressants, and stimulants. Drugs of abuse can be either off-label drugs or drugs that are medically prescribed. The two most commonly abused substances not included in this review are nicotine (tobacco) and alcohol. Accordingly, e-cigarettes and nicotine vape were also not included. Further, “adolescence” in this study refers to members of the population aged between 10 to 18 years [ 21 ].

Data extraction tool
All researchers independently extracted information for each article into an Excel spreadsheet. The data were then customized based on their (a) number; (b) year; (c) author and country; (d) titles; (e) study design; (f) type of substance abuse; (g) results—risks and protective factors; and (h) conclusions. A second reviewer crossed-checked the articles assigned to them and provided comments in the table.
Quality assessment tool
By using the Mixed Method Assessment Tool (MMAT version 2018), all articles were critically appraised for their quality by two independent reviewers. This tool has been shown to be useful in systematic reviews encompassing different study designs [ 22 ]. Articles were only selected if both reviewers agreed upon the articles’ quality. Any disagreement between the assigned reviewers was managed by employing a third independent reviewer. All included studies received a rating of “yes” for the questions in the respective domains of the MMAT checklists. Therefore, none of the articles were removed from this review due to poor quality. The Cohen’s kappa (agreement) between the two reviewers was 0.77, indicating moderate agreement [ 23 ].
The initial search found 425 studies for review, but after removing duplicates and applying the criteria listed above, we narrowed the pool to 22 articles, all of which are quantitative in their study design. The studies include three prospective cohort studies [ 24 , 25 , 26 ], one community trial [ 27 ], one case-control study [ 28 ], and nine cross-sectional studies [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. After careful discussion, all reviewer panels agreed to add one qualitative study [ 46 ] to help provide reasoning for the quantitative results. The selected qualitative paper was chosen because it discussed almost all domains on the risk and protective factors found in this review.
A summary of all 23 articles is listed in Table 2 . A majority of the studies (13 articles) were from the United States of America (USA) [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], three studies were from the Asia region [ 32 , 33 , 38 ], four studies were from Europe [ 24 , 28 , 40 , 44 ], and one study was from Latin America [ 35 ], Africa [ 43 ] and Mediterranean [ 45 ]. The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. There were a wide range of drugs assessed in the quantitative articles, with marijuana being mentioned in 11 studies, cannabis in five studies, and opioid (six studies). There was also large heterogeneity in terms of the study design, type of drug abused, measurements of outcomes, and analysis techniques used. Therefore, the data were presented descriptively.
After thorough discussion and evaluation, all the findings (both risk and protective factors) from the review were categorized into three main domains: individual factors, family factors, and community factors. The conceptual framework is summarized in Fig. 2 .
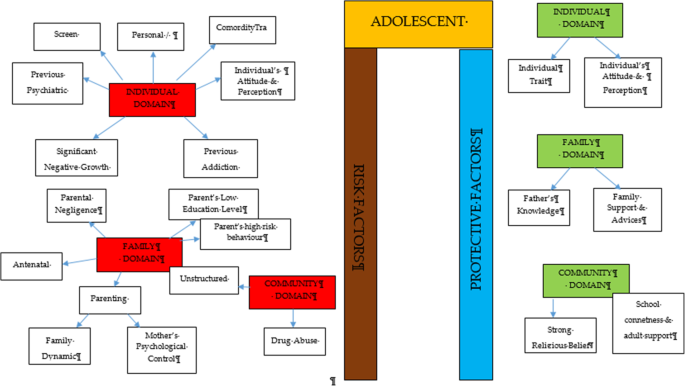
Conceptual framework of risk and protective factors related to adolescent drug abuse
DOMAIN: individual factor
Risk factors.
Almost all the articles highlighted significant findings of individual risk factors for adolescent drug abuse. Therefore, our findings for this domain were further broken down into five more sub-domains consisting of personal/individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance history, comorbidity and an individual’s attitude and perception.
Personal/individual traits
Chuang et al. [ 29 ] found that adolescents with high impulsivity traits had a significant positive association with drug addiction. This study also showed that the impulsivity trait alone was an independent risk factor that increased the odds between two to four times for using any drug compared to the non-impulsive group. Another longitudinal study by Guttmannova et al. showed that rebellious traits are positively associated with marijuana drug abuse [ 27 ]. The authors argued that measures of rebelliousness are a good proxy for a youth’s propensity to engage in risky behavior. Nevertheless, Wilson et al. [ 37 ], in a study involving 112 youths undergoing detoxification treatment for opioid abuse, found that a majority of the affected respondents had difficulty in regulating their emotions. The authors found that those with emotional regulation impairment traits became opioid dependent at an earlier age. Apart from that, a case-control study among outpatient youths found that adolescents involved in cannabis abuse had significant alexithymia traits compared to the control population [ 28 ]. Those adolescents scored high in the dimension of Difficulty in Identifying Emotion (DIF), which is one of the key definitions of diagnosing alexithymia. Overall, the adjusted Odds Ratio for DIF in cannabis abuse was 1.11 (95% CI, 1.03–1.20).
Significant negative growth exposure
A history of maltreatment in the past was also shown to have a positive association with adolescent drug abuse. A study found that a history of physical abuse in the past is associated with adolescent drug abuse through a Path Analysis, despite evidence being limited to the female gender [ 25 ]. However, evidence from another study focusing at foster care concluded that any type of maltreatment might result in a prevalence as high as 85.7% for the lifetime use of cannabis and as high as 31.7% for the prevalence of cannabis use within the last 3-months [ 30 ]. The study also found significant latent variables that accounted for drug abuse outcomes, which were chronic physical maltreatment (factor loading of 0.858) and chronic psychological maltreatment (factor loading of 0.825), with an r 2 of 73.6 and 68.1%, respectively. Another study shed light on those living in child welfare service (CWS) [ 35 ]. It was observed through longitudinal measurements that proportions of marijuana usage increased from 9 to 18% after 36 months in CWS. Hence, there is evidence of the possibility of a negative upbringing at such shelters.
Personal psychiatric diagnosis
The robust studies conducted in the USA have deduced that adolescents diagnosed with a conduct problem (CP) have a positive association with marijuana abuse (OR = 1.75 [1.56, 1.96], p < 0.0001). Furthermore, those with a diagnosis of Major Depressive Disorder (MDD) showed a significant positive association with marijuana abuse.
Previous substance and addiction history
Another study found that exposure to e-cigarettes within the past 30 days is related to an increase in the prevalence of marijuana use and prescription drug use by at least four times in the 8th and 10th grades and by at least three times in the 12th grade [ 34 ]. An association between other behavioral addictions and the development of drug abuse was also studied [ 29 ]. Using a 12-item index to assess potential addictive behaviors [ 39 ], significant associations between drug abuse and the groups with two behavioral addictions (OR = 3.19, 95% CI 1.25,9.77) and three behavioral addictions (OR = 3.46, 95% CI 1.25,9.58) were reported.
Comorbidity
The paper by Dash et al. (2020) highlight adolescent with a disease who needs routine medical pain treatment have higher risk of opioid misuse [ 38 ]. The adolescents who have disorder symptoms may have a risk for opioid misuse despite for the pain intensity.
Individual’s attitudes and perceptions
In a study conducted in three Latin America countries (Argentina, Chile, and Uruguay), it was shown that adolescents with low or no perceived risk of taking marijuana had a higher risk of abuse (OR = 8.22 times, 95% CI 7.56, 10.30) [ 35 ]. This finding is in line with another study that investigated 2002 adolescents and concluded that perceiving the drug as harmless was an independent risk factor that could prospectively predict future marijuana abuse [ 27 ]. Moreover, some youth interviewed perceived that they gained benefits from substance use [ 38 ]. The focus group discussion summarized that the youth felt positive personal motivation and could escape from a negative state by taking drugs. Apart from that, adolescents who had high-perceived availability of drugs in their neighborhoods were more likely to increase their usage of marijuana over time (OR = 11.00, 95% CI 9.11, 13.27) [ 35 ]. A cheap price of the substance and the availability of drug dealers around schools were factors for youth accessibility [ 38 ]. Perceived drug accessibility has also been linked with the authorities’ enforcement programs. The youth perception of a lax community enforcement of laws regarding drug use at all-time points predicted an increase in marijuana use in the subsequent assessment period [ 27 ]. Besides perception, a study examining the attitudes towards synthetic drugs based on 8076 probabilistic samples of Macau students found that the odds of the lifetime use of marijuana was almost three times higher among those with a strong attitude towards the use of synthetic drugs [ 32 ]. In addition, total screen time among the adolescent increase the likelihood of frequent cannabis use. Those who reported daily cannabis use have a mean of 12.56 h of total screen time, compared to a mean of 6.93 h among those who reported no cannabis use. Adolescent with more time on internet use, messaging, playing video games and watching TV/movies were significantly associated with more frequent cannabis use [ 44 ].
Protective factors
Individual traits.
Some individual traits have been determined to protect adolescents from developing drug abuse habits. A study by Marin et al. found that youth with an optimistic trait were less likely to become drug dependent [ 33 ]. In this study involving 1104 Iranian students, it was concluded that a higher optimism score (measured using the Children Attributional Style Questionnaire, CASQ) was a protective factor against illicit drug use (OR = 0.90, 95% CI: 0.85–0.95). Another study found that high levels of mindfulness, measured using the 25-item Child Acceptance and Mindfulness Measure, CAMM, lead to a slower progression toward injectable drug abuse among youth with opioid addiction (1.67 years, p = .041) [ 37 ]. In addition, the social phobia trait was found to have a negative association with marijuana use (OR = 0.87, 95% CI 0.77–0.97), as suggested [ 31 ].
According to El Kazdouh et al., individuals with a strong belief against substance use and those with a strong desire to maintain their health were more likely to be protected from involvement in drug abuse [ 46 ].
DOMAIN: family factors
The biological factors underlying drug abuse in adolescents have been reported in several studies. Epigenetic studies are considered important, as they can provide a good outline of the potential pre-natal factors that can be targeted at an earlier stage. Expecting mothers who smoke tobacco and alcohol have an indirect link with adolescent substance abuse in later life [ 24 , 39 ]. Moreover, the dynamic relationship between parents and their children may have some profound effects on the child’s growth. Luk et al. examined the mediator effects between parenting style and substance abuse and found the maternal psychological control dimension to be a significant variable [ 26 ]. The mother’s psychological control was two times higher in influencing her children to be involved in substance abuse compared to the other dimension. Conversely, an indirect risk factor towards youth drug abuse was elaborated in a study in which low parental educational level predicted a greater risk of future drug abuse by reducing the youth’s perception of harm [ 27 , 43 ]. Negligence from a parental perspective could also contribute to this problem. According to El Kazdouh et al. [ 46 ], a lack of parental supervision, uncontrolled pocket money spending among children, and the presence of substance-using family members were the most common negligence factors.
While the maternal factors above were shown to be risk factors, the opposite effect was seen when the paternal figure equipped himself with sufficient knowledge. A study found that fathers with good information and awareness were more likely to protect their adolescent children from drug abuse [ 26 ]. El Kazdouh et al. noted that support and advice could be some of the protective factors in this area [ 46 ].
DOMAIN: community factors
- Risk factor
A study in 2017 showed a positive association between adolescent drug abuse and peers who abuse drugs [ 32 , 39 ]. It was estimated that the odds of becoming a lifetime marijuana user was significantly increased by a factor of 2.5 ( p < 0.001) among peer groups who were taking synthetic drugs. This factor served as peer pressure for youth, who subconsciously had desire to be like the others [ 38 ]. The impact of availability and engagement in structured and unstructured activities also play a role in marijuana use. The findings from Spillane (2000) found that the availability of unstructured activities was associated with increased likelihood of marijuana use [ 42 ].
- Protective factor
Strong religious beliefs integrated into society serve as a crucial protective factor that can prevent adolescents from engaging in drug abuse [ 38 , 45 ]. In addition, the school connectedness and adult support also play a major contribution in the drug use [ 40 ].
The goal of this review was to identify and classify the risks and protective factors that lead adolescents to drug abuse across the three important domains of the individual, family, and community. No findings conflicted with each other, as each of them had their own arguments and justifications. The findings from our review showed that individual factors were the most commonly highlighted. These factors include individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance and addiction history, and an individual’s attitude and perception as risk factors.
Within the individual factor domain, nine articles were found to contribute to the subdomain of personal/ individual traits [ 27 , 28 , 29 , 37 , 38 , 39 , 40 , 43 , 44 ]. Despite the heterogeneity of the study designs and the substances under investigation, all of the papers found statistically significant results for the possible risk factors of adolescent drug abuse. The traits of high impulsivity, rebelliousness, difficulty in regulating emotions, and alexithymia can be considered negative characteristic traits. These adolescents suffer from the inability to self-regulate their emotions, so they tend to externalize their behaviors as a way to avoid or suppress the negative feelings that they are experiencing [ 41 , 47 , 48 ]. On the other hand, engaging in such behaviors could plausibly provide a greater sense of positive emotions and make them feel good [ 49 ]. Apart from that, evidence from a neurophysiological point of view also suggests that the compulsive drive toward drug use is complemented by deficits in impulse control and decision making (impulsive trait) [ 50 ]. A person’s ability in self-control will seriously impaired with continuous drug use and will lead to the hallmark of addiction [ 51 ].
On the other hand, there are articles that reported some individual traits to be protective for adolescents from engaging in drug abuse. Youth with the optimistic trait, a high level of mindfulness, and social phobia were less likely to become drug dependent [ 31 , 33 , 37 ]. All of these articles used different psychometric instruments to classify each individual trait and were mutually exclusive. Therefore, each trait measured the chance of engaging in drug abuse on its own and did not reflect the chance at the end of the spectrum. These findings show that individual traits can be either protective or risk factors for the drugs used among adolescents. Therefore, any adolescent with negative personality traits should be monitored closely by providing health education, motivation, counselling, and emotional support since it can be concluded that negative personality traits are correlated with high risk behaviours such as drug abuse [ 52 ].
Our study also found that a history of maltreatment has a positive association with adolescent drug abuse. Those adolescents with episodes of maltreatment were considered to have negative growth exposure, as their childhoods were negatively affected by traumatic events. Some significant associations were found between maltreatment and adolescent drug abuse, although the former factor was limited to the female gender [ 25 , 30 , 36 ]. One possible reason for the contrasting results between genders is the different sample populations, which only covered child welfare centers [ 36 ] and foster care [ 30 ]. Regardless of the place, maltreatment can happen anywhere depending on the presence of the perpetrators. To date, evidence that concretely links maltreatment and substance abuse remains limited. However, a plausible explanation for this link could be the indirect effects of posttraumatic stress (i.e., a history of maltreatment) leading to substance use [ 53 , 54 ]. These findings highlight the importance of continuous monitoring and follow-ups with adolescents who have a history of maltreatment and who have ever attended a welfare center.
Addiction sometimes leads to another addiction, as described by the findings of several studies [ 29 , 34 ]. An initial study focused on the effects of e-cigarettes in the development of other substance abuse disorders, particularly those related to marijuana, alcohol, and commonly prescribed medications [ 34 ]. The authors found that the use of e-cigarettes can lead to more severe substance addiction [ 55 ], possibly through normalization of the behavior. On the other hand, Chuang et al.’s extensive study in 2017 analyzed the combined effects of either multiple addictions alone or a combination of multiple addictions together with the impulsivity trait [ 29 ]. The outcomes reported were intriguing and provide the opportunity for targeted intervention. The synergistic effects of impulsiveness and three other substance addictions (marijuana, tobacco, and alcohol) substantially increased the likelihood for drug abuse from 3.46 (95%CI 1.25, 9.58) to 10.13 (95% CI 3.95, 25.95). Therefore, proper rehabilitation is an important strategy to ensure that one addiction will not lead to another addiction.
The likelihood for drug abuse increases as the population perceives little or no harmful risks associated with the drugs. On the opposite side of the coin, a greater perceived risk remains a protective factor for marijuana abuse [ 56 ]. However, another study noted that a stronger determinant for adolescent drug abuse was the perceived availability of the drug [ 35 , 57 ]. Looking at the bigger picture, both perceptions corroborate each other and may inform drug use. Another study, on the other hand, reported that there was a decreasing trend of perceived drug risk in conjunction with the increasing usage of drugs [ 58 ]. As more people do drugs, youth may inevitably perceive those drugs as an acceptable norm without any harmful consequences [ 59 ].
In addition, the total spent for screen time also contribute to drug abuse among adolescent [ 43 ]. This scenario has been proven by many researchers on the effect of screen time on the mental health [ 60 ] that leads to the substance use among the adolescent due to the ubiquity of pro-substance use content on the internet. Adolescent with comorbidity who needs medical pain management by opioids also tend to misuse in future. A qualitative exploration on the perspectives among general practitioners concerning the risk of opioid misuse in people with pain, showed pain management by opioids is a default treatment and misuse is not a main problem for the them [ 61 ]. A careful decision on the use of opioids as a pain management should be consider among the adolescents and their understanding is needed.
Within the family factor domain, family structures were found to have both positive and negative associations with drug abuse among adolescents. As described in one study, paternal knowledge was consistently found to be a protective factor against substance abuse [ 26 ]. With sufficient knowledge, the father can serve as the guardian of his family to monitor and protect his children from negative influences [ 62 ]. The work by Luk et al. also reported a positive association of maternal psychological association towards drug abuse (IRR 2.41, p < 0.05) [ 26 ]. The authors also observed the same effect of paternal psychological control, although it was statistically insignificant. This construct relates to parenting style, and the authors argued that parenting style might have a profound effect on the outcomes under study. While an earlier literature review [ 63 ] also reported such a relationship, a recent study showed a lesser impact [ 64 ] with regards to neglectful parenting styles leading to poorer substance abuse outcomes. Nevertheless, it was highlighted in another study that the adolescents’ perception of a neglectful parenting style increased their odds (OR 2.14, p = 0.012) of developing alcohol abuse, not the parenting style itself [ 65 ]. Altogether, families play vital roles in adolescents’ risk for engaging in substance abuse [ 66 ]. Therefore, any intervention to impede the initiation of substance use or curb existing substance use among adolescents needs to include parents—especially improving parent–child communication and ensuring that parents monitor their children’s activities.
Finally, the community also contributes to drug abuse among adolescents. As shown by Li et al. [ 32 ] and El Kazdouh et al. [ 46 ], peers exert a certain influence on other teenagers by making them subconsciously want to fit into the group. Peer selection and peer socialization processes might explain why peer pressure serves as a risk factor for drug-abuse among adolescents [ 67 ]. Another study reported that strong religious beliefs integrated into society play a crucial role in preventing adolescents from engaging in drug abuse [ 46 ]. Most religions devalue any actions that can cause harmful health effects, such as substance abuse [ 68 ]. Hence, spiritual beliefs may help protect adolescents. This theme has been well established in many studies [ 60 , 69 , 70 , 71 , 72 ] and, therefore, could be implemented by religious societies as part of interventions to curb the issue of adolescent drug abuse. The connection with school and structured activity did reduce the risk as a study in USA found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity and social activity [ 73 ]. The school activity should highlight on the importance of developmental perspective when designing and offering school-based prevention programs [75].
Limitations
We adopted a review approach that synthesized existing evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in different settings, there are some potential limitations to this work. We may have missed some other important factors, as we only included English articles, and article extraction was only done from the three search engines mentioned. Nonetheless, this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and cigarettes, thereby making this paper more focused.
Conclusions
This review has addressed some recent knowledge related to the individual, familial, and community risk and preventive factors for adolescent drug use. We suggest that more attention should be given to individual factors since most findings were discussed in relation to such factors. With the increasing trend of drug abuse, it will be critical to focus research specifically on this area. Localized studies, especially those related to demographic factors, may be more effective in generating results that are specific to particular areas and thus may be more useful in generating and assessing local control and prevention efforts. Interventions using different theory-based psychotherapies and a recognition of the unique developmental milestones specific to adolescents are among examples that can be used. Relevant holistic approaches should be strengthened not only by relevant government agencies but also by the private sector and non-governmental organizations by promoting protective factors while reducing risk factors in programs involving adolescents from primary school up to adulthood to prevent and control drug abuse. Finally, legal legislation and enforcement against drug abuse should be engaged with regularly as part of our commitment to combat this public health burden.
Data availability and materials
All data generated or analysed during this study are included in this published article.
Nation, U. World Drug Report 2018 (United Nations publication, Sales No. E.18X.XI.9. United Nation publication). 2018. Retrieved from https://www.unodc.org/wdr2018
Google Scholar
Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–64. https://doi.org/10.1016/S2215-0366(15)00508-8 Elsevier Ltd.
Article PubMed Google Scholar
Ritchie H, Roser M. Drug Use - Our World in Data: Global Change Data Lab; 2019. https://ourworldindata.org/drug-use [10 June 2020]
Holm S, Sandberg S, Kolind T, Hesse M. The importance of cannabis culture in young adult cannabis use. J Subst Abus. 2014;19(3):251–6.
Luikinga SJ, Kim JH, Perry CJ. Developmental perspectives on methamphetamine abuse: exploring adolescent vulnerabilities on brain and behavior. Progress Neuro Psychopharmacol Biol Psychiatry. 2018;87(Pt A):78–84. https://doi.org/10.1016/j.pnpbp.2017.11.010 Elsevier Inc.
Article CAS Google Scholar
Ismail R, Ghazalli MN, Ibrahim N. Not all developmental assets can predict negative mental health outcomes of disadvantaged youth: a case of suburban Kuala Lumpur. Mediterr J Soc Sci. 2015;6(1):452–9. https://doi.org/10.5901/mjss.2015.v6n5s1p452 .
Article Google Scholar
Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. https://doi.org/10.1016/j.pbb.2006.12.001 .
Article CAS PubMed Google Scholar
Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2). https://doi.org/10.1007/bf03391702 Technosdar Ltd.
Somani, S.; Meghani S. Substance Abuse among Youth: A Harsh Reality 2016. doi: https://doi.org/10.4172/2165-7548.1000330 , 6, 4.
Book Google Scholar
Drabble L, Trocki KF, Klinger JL. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: findings from the National Alcohol Survey. Drug Alcohol Depend. 2016;161:127–34. https://doi.org/10.1016/j.drugalcdep.2016.01.022 .
Article PubMed PubMed Central Google Scholar
Goliath V, Pretorius B. Peer risk and protective factors in adolescence: Implications for drug use prevention. Soc Work. 2016;52(1):113–29. https://doi.org/10.15270/52-1-482 .
Guerrero LR, Dudovitz R, Chung PJ, Dosanjh KK, Wong MD. Grit: a potential protective factor against substance use and other risk behaviors among Latino adolescents. Acad Pediatr. 2016;16(3):275–81. https://doi.org/10.1016/j.acap.2015.12.016 .
National Institutes on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse (NIDA); 2003. Retrieved from https://www.drugabuse.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
Nguyen NN, Newhill CE. The role of religiosity as a protective factor against marijuana use among African American, White, Asian, and Hispanic adolescents. J Subst Abus. 2016;21(5):547–52. https://doi.org/10.3109/14659891.2015.1093558 .
Schinke S, Schwinn T, Hopkins J, Wahlstrom L. Drug abuse risk and protective factors among Hispanic adolescents. Prev Med Rep. 2016;3:185–8. https://doi.org/10.1016/j.pmedr.2016.01.012 .
Macleod J, Oakes R, Copello A, Crome PI, Egger PM, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–88. https://doi.org/10.1016/S0140-6736(04)16200-4 .
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3 .
Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–94. https://doi.org/10.1177/0269881105049040 .
Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the united states: A social ecological perspective. J Stud Alcohol Drugs. 2015;76(1):5–20. https://doi.org/10.15288/jsad.2015.76.5 .
Guxensa M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007;21(3):252–60. https://doi.org/10.1157/13106811 .
Susan MS, Peter SA, Dakshitha W, George CP. The age of adolescence. Lancet Child Adolesc Health. 2018;2(Issue 3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1 .
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
McHugh ML. Interrater reliability: The kappa statistic. Biochem Med. 2012;22(3):276–82. https://doi.org/10.11613/bm.2012.031 .
Cecil CAM, Walton E, Smith RG, Viding E, McCrory EJ, Relton CL, et al. DNA methylation and substance-use risk: a prospective, genome-wide study spanning gestation to adolescence. Transl Psychiatry. 2016;6(12):e976. https://doi.org/10.1038/tp.2016.247 Nature Publishing Group.
Article CAS PubMed PubMed Central Google Scholar
Kobulsky JM. Gender differences in pathways from physical and sexual abuse to early substance use. Child Youth Serv Rev. 2017;83:25–32. https://doi.org/10.1016/j.childyouth.2017.10.027 .
Luk JW, King KM, McCarty CA, McCauley E, Stoep A. Prospective effects of parenting on substance use and problems across Asian/Pacific islander and European American youth: Tests of moderated mediation. J Stud Alcohol Drugs. 2017;78(4):521–30. https://doi.org/10.15288/jsad.2017.78.521 .
Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, Hawkins JD. The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prev Sci. 2019;20(2):235–45. https://doi.org/10.1007/s11121-018-0882-9 .
Dorard G, Bungener C, Phan O, Edel Y, Corcos M, Berthoz S. Is alexithymia related to cannabis use disorder? Results from a case-control study in outpatient adolescent cannabis abusers. J Psychosom Res. 2017;95:74–80. https://doi.org/10.1016/j.jpsychores.2017.02.012 .
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74:41–7. https://doi.org/10.1016/j.addbeh.2017.05.021 .
Gabrielli J, Jackson Y, Brown S. Associations between maltreatment history and severity of substance use behavior in youth in Foster Care. Child Maltreat. 2016;21(4):298–307. https://doi.org/10.1177/1077559516669443 .
Khoddam R, Jackson NJ, Leventhal AM. Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 2016;169:48–55. https://doi.org/10.1016/j.drugalcdep.2016.10.007 .
Li SD, Zhang X, Tang W, Xia Y. Predictors and implications of synthetic drug use among adolescents in the gambling Capital of China. SAGE Open. 2017;7(4):215824401773303. https://doi.org/10.1177/2158244017733031 .
Marin S, Heshmatian E, Nadrian H, Fakhari A, Mohammadpoorasl A. Associations between optimism, tobacco smoking and substance abuse among Iranian high school students. Health Promot Perspect. 2019;9(4):279–84. https://doi.org/10.15171/hpp.2019.38 .
Miech RA, O’Malley PM, Johnston LD, Patrick ME. E-cigarettes and the drug use patterns of adolescents. Nicotine Tob Res. 2015;18(5):654–9. https://doi.org/10.1093/ntr/ntv217 .
Schleimer JP, Rivera-Aguirre AE, Castillo-Carniglia A, Laqueur HS, Rudolph KE, Suárez H, et al. Investigating how perceived risk and availability of marijuana relate to marijuana use among adolescents in Argentina, Chile, and Uruguay over time. Drug Alcohol Depend. 2019;201:115–26. https://doi.org/10.1016/j.drugalcdep.2019.03.029 .
Traube DE, Yarnell LM, Schrager SM. Differences in polysubstance use among youth in the child welfare system: toward a better understanding of the highest-risk teens. Child Abuse Negl. 2016;52:146–57. https://doi.org/10.1016/j.chiabu.2015.11.020 .
Wilson JD, Vo H, Matson P, Adger H, Barnett G, Fishman M. Trait mindfulness and progression to injection use in youth with opioid addiction. Subst Use Misuse. 2017;52(11):1486–93. https://doi.org/10.1080/10826084.2017.1289225 .
Dash GF, Feldstein Ewing SW, Murphy C, Hudson KA, Wilson AC. Contextual risk among adolescents receiving opioid prescriptions for acute pain in pediatric ambulatory care settings. Addict Behav. 2020;104:106314. https://doi.org/10.1016/j.addbeh.2020.106314 Epub 2020 Jan 11. PMID: 31962289; PMCID: PMC7024039.
Osborne V, Serdarevic M, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Age of first use of prescription opioids and prescription opioid non-medical use among older adolescents. Substance Use Misuse. 2020;55(14):2420–7. https://doi.org/10.1080/10826084.2020.1823420 .
Zuckermann AME, Qian W, Battista K, Jiang Y, de Groh M, Leatherdale ST. Factors influencing the non-medical use of prescription opioids among youth: results from the COMPASS study. J Subst Abus. 2020;25(5):507–14. https://doi.org/10.1080/14659891.2020.1736669 .
De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. https://doi.org/10.1089/lgbt.2016.0132 .
Spillane NS, Schick MR, Kirk-Provencher KT, Hill DC, Wyatt J, Jackson KM. Structured and unstructured activities and alcohol and marijuana use in middle school: the role of availability and engagement. Substance Use Misuse. 2020;55(11):1765–73. https://doi.org/10.1080/10826084.2020.1762652 .
Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun state, Nigeria. Int J Adolesc Med Health. 2016;29(3). https://doi.org/10.1515/ijamh-2015-0096 .
Doggett A, Qian W, Godin K, De Groh M, Leatherdale ST. Examining the association between exposure to various screen time sedentary behaviours and cannabis use among youth in the COMPASS study. SSM Population Health. 2019;9:100487. https://doi.org/10.1016/j.ssmph.2019.100487 .
Afifi RA, El Asmar K, Bteddini D, Assi M, Yassin N, Bitar S, et al. Bullying victimization and use of substances in high school: does religiosity moderate the association? J Relig Health. 2020;59(1):334–50. https://doi.org/10.1007/s10943-019-00789-8 .
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Substance Abuse Treat Prevent Policy. 2018;13(1):–31. https://doi.org/10.1186/s13011-018-0169-y .
Sussman S, Lisha N, Griffiths M. Prevalence of the addictions: a problem of the majority or the minority? Eval Health Prof. 2011;34(1):3–56. https://doi.org/10.1177/0163278710380124 .
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. https://doi.org/10.1016/j.cpr.2009.11.004 .
Ricketts T, Macaskill A. Gambling as emotion management: developing a grounded theory of problem gambling. Addict Res Theory. 2003;11(6):383–400. https://doi.org/10.1080/1606635031000062074 .
Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cogn Ther Res. 2012;36(5):451–7. https://doi.org/10.1007/s10608-011-9384-9 .
National Institutes on Drug Abuse. Drugs, brains, and behavior the science of addiction national institute on drug abuse (nida). 2014. Retrieved from https://www.drugabuse.gov/sites/default/files/soa_2014.pdf
Hokm Abadi ME, Bakhti M, Nazemi M, Sedighi S, Mirzadeh Toroghi E. The relationship between personality traits and drug type among substance abuse. J Res Health. 2018;8(6):531–40.
Longman-Mills S, Haye W, Hamilton H, Brands B, Wright MGM, Cumsille F, et al. Psychological maltreatment and its relationship with substance abuse among university students in Kingston, Jamaica, vol. 24. Florianopolis: Texto Contexto Enferm; 2015. p. 63–8.
Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychol Trauma Theory Res Pract Policy. 2014;6(1):25–33. https://doi.org/10.1037/a0031920 .
Krishnan-Sarin S, Morean M, Kong G, et al. E-Cigarettes and “dripping” among high-school youth. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-3224 .
Adinoff B. Neurobiologic processes in drug reward and addiction. Harvard review of psychiatry. NIH Public Access. 2004;12(6):305–20. https://doi.org/10.1080/10673220490910844 .
Kandel D, Kandel E. The gateway hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica. 2014;104(2):130–7.
Dempsey RC, McAlaney J, Helmer SM, Pischke CR, Akvardar Y, Bewick BM, et al. Normative perceptions of Cannabis use among European University students: associations of perceived peer use and peer attitudes with personal use and attitudes. J Stud Alcohol Drugs. 2016;77(5):740–8.
Cioffredi L, Kamon J, Turner W. Effects of depression, anxiety and screen use on adolescent substance use. Prevent Med Rep. 2021;22:101362. https://doi.org/10.1016/j.pmedr.2021.101362 .
Luckett T, NewtonJohn T, Phillips J, et al. Risk of opioid misuse in people with cancer and pain and related clinical considerations:a qualitative study of the perspectives of Australian general practitioners. BMJ Open. 2020;10(2):e034363. https://doi.org/10.1136/bmjopen-2019-034363 .
Lipari RN. Trends in Adolescent Substance Use and Perception of Risk from Substance Use. The CBHSQ Report. Substance Abuse Mental Health Serv Admin. 2013; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27656743 .
Muchiri BW, dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Substance Abuse. 2018;13(1):24. https://doi.org/10.1186/s13011-018-0163-4 .
Becoña E, Martínez Ú, Calafat A, Juan M, Fernández-Hermida JR, Secades-Villa R. Parental styles and drug use: a review. In: Drugs: Education, Prevention and Policy: Taylor & Francis; 2012. https://doi.org/10.3109/09687637.2011.631060 .
Berge J, Sundel K, Ojehagen A, Hakansson A. Role of parenting styles in adolescent substance use: results from a Swedish longitudinal cohort study. BMJ Open. 2016;6(1):e008979. https://doi.org/10.1136/bmjopen-2015-008979 .
Opara I, Lardier DT, Reid RJ, Garcia-Reid P. “It all starts with the parents”: a qualitative study on protective factors for drug-use prevention among black and Hispanic girls. Affilia J Women Soc Work. 2019;34(2):199–218. https://doi.org/10.1177/0886109918822543 .
Martínez-Loredo V, Fernández-Artamendi S, Weidberg S, Pericot I, López-Núñez C, Fernández-Hermida J, et al. Parenting styles and alcohol use among adolescents: a longitudinal study. Eur J Invest Health Psychol Educ. 2016;6(1):27–36. https://doi.org/10.1989/ejihpe.v6i1.146 .
Baharudin MN, Mohamad M, Karim F. Drug-abuse inmates maqasid shariah quality of lifw: a conceotual paper. Hum Soc Sci Rev. 2020;8(3):1285–94. https://doi.org/10.18510/hssr.2020.83131 .
Henneberger AK, Mushonga DR, Preston AM. Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev. 2020;6(1):57–73. https://doi.org/10.1007/s40894-019-00130-0 Springer.
Gomes FC, de Andrade AG, Izbicki R, Almeida AM, de Oliveira LG. Religion as a protective factor against drug use among Brazilian university students: a national survey. Rev Bras Psiquiatr. 2013;35(1):29–37. https://doi.org/10.1016/j.rbp.2012.05.010 .
Kulis S, Hodge DR, Ayers SL, Brown EF, Marsiglia FF. Spirituality and religion: intertwined protective factors for substance use among urban American Indian youth. Am J Drug Alcohol Abuse. 2012;38(5):444–9. https://doi.org/10.3109/00952990.2012.670338 .
Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the national comorbidity survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–7. https://doi.org/10.1097/00004583-200009000-00020 .
Moon SS, Rao U. Social activity, school-related activity, and anti-substance use media messages on adolescent tobacco and alcohol use. J Hum Behav Soc Environ. 2011;21(5):475–89. https://doi.org/10.1080/10911359.2011.566456 .
Simone A. Onrust, Roy Otten, Jeroen Lammers, Filip smit, school-based programmes to reduce and prevent substance use in different age groups: what works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev. 2016;44:45–59. https://doi.org/10.1016/j.cpr.2015.11.002 .
Download references
Acknowledgements
The authors acknowledge The Ministry of Higher Education Malaysia and The Universiti Kebangsaan Malaysia, (UKM) for funding this study under the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). We also thank the team for their commitment and tireless efforts in ensuring that manuscript was well executed.
Financial support for this study was obtained from the Ministry of Higher Education, Malaysia through the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Community Health, Universiti Kebangsaan Malaysia, Cheras, 56000, Kuala Lumpur, Malaysia
Azmawati Mohammed Nawi, Mohd Rohaizat Hassan & Mohd Rizal Abdul Manaf
Centre for Research in Psychology and Human Well-Being (PSiTra), Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Rozmi Ismail, Fauziah Ibrahim & Nurul Shafini Shafurdin
Clinical Psychology and Behavioural Health Program, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Noh Amit & Norhayati Ibrahim
You can also search for this author in PubMed Google Scholar
Contributions
Manuscript concept, and drafting AMN and RI; model development, FI, NI and NA.; Editing manuscript MRH, MRAN, NSS,; Critical revision of manuscript for important intellectual content, all authors. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Rozmi Ismail .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Secretariat of Research Ethics, Universiti Kebangsaan Malaysia, Faculty of Medicine, Cheras, Kuala Lumpur (Reference no. UKMPPI/111/8/JEP-2020.174(2). Dated 27 Mac 2020.
Consent for publication
Not applicable.
Competing interests
The authors AMN, RI, FI, MRM, MRAM, NA, NI NSS declare that they have no conflict of interest relevant to this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nawi, A.M., Ismail, R., Ibrahim, F. et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 21 , 2088 (2021). https://doi.org/10.1186/s12889-021-11906-2
Download citation
Received : 10 June 2021
Accepted : 22 September 2021
Published : 13 November 2021
DOI : https://doi.org/10.1186/s12889-021-11906-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug abuse, substance, adolescent
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 30 August 2023
Police seizure of drugs without arrest among people who use drugs in Vancouver, Canada, before provincial ‘decriminalization’ of simple possession: a cohort study
- Kanna Hayashi 1 , 2 ,
- Tyson Singh Kelsall 1 , 2 ,
- Caitlin Shane 3 ,
- Zishan Cui 1 , 4 ,
- Vancouver Area Network of Drug Users ,
- M.-J. Milloy 1 , 6 ,
- Kora DeBeck 1 , 7 &
- Thomas Kerr 1 , 6
Harm Reduction Journal volume 20 , Article number: 117 ( 2023 ) Cite this article
3407 Accesses
3 Citations
59 Altmetric
Metrics details
Several jurisdictions in Canada have recently considered decriminalizing possession of illicit drugs for personal use (henceforth, simple possession) as part of their responses to the ongoing drug toxicity/overdose crisis. In this context, we sought to examine an early implementation case of a de facto depenalization policy of simple possession offences in Vancouver, Canada, that was enacted in 2006. Specifically, we characterized experiences of people who use drugs (PWUD) whose drugs were discretionally seized by police without arrest.
Data were derived from three prospective cohorts of community-recruited PWUD in Vancouver over 16 months in 2019–2021. We conducted multivariable generalized estimating equations analyses to determine the prevalence of and factors associated with drug seizure. Sub-analyses used data collected in 2009–2012 and examined the trends over time.
Among 995 participants who were interviewed in 2019–2021, 63 (6.3%) had their drugs seized by police at least once in the past 6 months. In multivariable analyses, factors significantly associated with drug seizure included: homelessness (adjusted odds ratio [AOR]: 1.98; 95% confidence interval [CI] 1.09–3.61), working in the unregulated drug market (AOR: 4.93; 95% CI 2.87–8.49), and naloxone administration (AOR: 2.15; 95% CI 1.23–3.76). In 2009–2012, 67.8% reported having obtained new drugs immediately after having their drugs seized by police. Odds of drug seizure were not significantly different between the two time periods (2019–2021 vs. 2009–2012) (AOR: 0.93; 95% CI: 0.64–1.35).
Conclusions
Despite the depenalization policy, the Vancouver Police Department has continued to seize illicit drugs from PWUD, even in cases where no arrest occurred. This policing practice may create health and safety risks for PWUD as it forces PWUD to increase the engagement with the unregulated illicit drug market. Our findings support calls for abolishing this often-undocumented discretionary policing practice that may exacerbate ongoing health inequities and interfere with peer-based overdose prevention efforts.
Over the past two decades, growing recognition of the negative consequences of punitive, prohibition-based drug policies has led to increased support for alternative approaches worldwide [ 1 , 2 ]. In this context, commonly discussed approaches include both de jure and de facto initiatives aimed at reducing criminal sanctions for the possession of illicit drugs for personal use (henceforth, simple possession). These initiatives can take various forms and produce different outcomes across different settings [ 3 , 4 ]. According to Stevens et al. [ 3 ], decriminalization involves the de jure removal of criminal sanctions for simple possession, while depenalization is a de facto (non-legislative) approach intended to reduce the use of existing criminal sanctions for simple possession. Police policies instructing officers to not arrest people for simple possession are an example of depenalization. In recent years, several jurisdictions in Canada have considered ‘decriminalizing’ simple possession via a temporary legal exemption under the federal drug law (i.e. in-between de jure and de facto initiatives) as part of their responses to the ongoing drug toxicity/overdose crisis.
In 2006, the Vancouver Police Department (VPD), the police force within the city of Vancouver in British Columbia (BC), Canada, formalized its drug policy and endorsed harm reduction as a core pillar of its strategy, alongside prevention, treatment, and law enforcement [ 5 ]. The policy encouraged the de facto depenalization of simple possession by restricting enforcement to circumstances where people are engaged in public drug use or other behaviour that the VPD believed may harm others [ 5 ], which would notably sustain roles for policing in the lives of PWUD. Similarly, in August 2020, the Public Prosecution Service of Canada released guidelines that direct prosecutors to limit the criminal prosecution of simple possession offences to the most serious manifestations of the offence (e.g. where there is a safety risk to others) [ 6 ]. Although the VPD’s published data are limited, available data indeed indicate low and declining levels of enforcement between 2016 and 2019, with recommended charges for simple possession having decreased by 67% from 109 to 36 cases [ 7 ].
Despite VPD’s depenalization policy regarding simple possession, officers are still afforded broad enforcement discretion, including with respect to drug possession [ 5 ]. For example officers may use their ‘professional judgement’ to enforce drug seizures with or without making an arrest [ 5 ]. While anecdotal reports suggest that the police practice of drug seizure is commonplace and a driver of harm among people who use drugs (PWUD) [ 8 ], such discretionary practice is not fully captured in the VPD’s published data [ 9 ], limiting our understanding of how VPD’s policy of depenalization has been implemented at the street level.
To date, one study has quantified the extent of the discretionary police seizure of drugs without arrest in the Greater Vancouver region (mostly within the VPD jurisdiction but also including an area beyond that), showing that 9% of 465 people who injected drugs had their drugs seized by the police without arrest in the past 6 months in 2005 [ 10 ]. However, that study predated the launch of VPD’s current drug policy. In the wake of recent policy efforts towards ‘decriminalization’ in Canada and also given that drug seizures by police can greatly affect drug acquisition behaviour among PWUD and subsequently their risk of overdose and other drug-related harm [ 11 ], we sought to characterize the prevalence and associated factors of experiencing police seizure of drugs without arrest among people who used drugs at least on a daily basis (i.e. a particularly high-risk population) in Vancouver between 2019 and 2021, a period coinciding with the ongoing drug poisoning crisis [ 12 ]. We also used data collected between 2009 and 2012 to explore historical trends as well as to examine PWUD’s behaviour immediately following the drug seizures by police because this particular set of behavioural data was not collected in 2019–2021.
Study setting, design, and participants
Data were derived from three ongoing prospective cohort studies of PWUD in Vancouver: the Vancouver Injection Drug Users Study (VIDUS), the AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS), and the At-Risk Youth Study (ARYS). Detailed descriptions of these cohorts have been previously published elsewhere [ 13 , 14 ]. In brief, VIDUS enrols HIV-seronegative adults (≥ 18 years of age) who injected drugs in the month before enrolment. ACCESS enrols HIV-seropositive adults, and ARYS enrols street-involved youth aged 14–26 who used unregulated drugs in the month before enrolment. Other common eligibility criteria across the cohorts include residing in the Greater Vancouver region and providing written informed consent. All cohorts recruit participants through word-of-mouth and street outreach primarily in two neighbourhoods in Vancouver: Downtown Eastside (DTES; an area characterized by high prevalence of marginalization and unregulated drug use) for VIDUS and ACCESS and Downtown South for ARYS. The studies use harmonized data collection procedures to allow for pooled analyses. Participants receive a CAD $40 honorarium upon completion of each study visit.
At baseline and semi-annually thereafter, participants complete an interviewer-administered questionnaire, which elicits a range of information including demographic data, substance use, health care access, and experiences with law enforcement. On 16 March 2020, data collection was suspended due to the COVID-19 pandemic on the orders of our host institutions. We resumed remote follow-up interviews (via phone) that included questions about drug seizure by police in June 2021. Options for in-person follow-up interviews were resumed in March 2022. All cohorts have received approvals from the University of British Columbia/Providence Health Care Research Ethics Board.
The cohort study survey is updated every follow-up. Survey questions related to drug seizure were only included on the questionnaire during the following periods: June 2009–November 2012; June 2019–March 2020; and June–November 2021. For the primary analysis, sample eligibility criteria included: completing a study interview at least once between June 2019 and November 2021, and reporting having resided within the city of Vancouver (i.e. within the VPD jurisdiction) and used drugs at least daily in the past 6 months. For the secondary analysis, the follow-up period from June 2009 to November 2012 was added to the eligibility while the other eligibility criteria were kept constant.
The primary outcome was self-reported drug seizure by police without arrest in the past 6 months (yes vs. no; henceforth, drug seizure), which was derived from a question: ‘In the last 6 months, did the police take away your drugs without arresting or pressing charges against you?’ This question was asked to participants who answered yes to a previous question: ‘In the last 6 months, have you had direct contact with the police?’ Participants who reported having their drugs seized were also asked how many times they had their drugs seized within the same 6-month period. Between 2009 and 2012, another sub-question about what they did immediately afterwards was also asked. Between 2019 and 2021, participants were not asked about their immediate responses to police seizure of drugs. However, they were asked a different sub-question about which neighbourhood they were in when drugs were seized. The cases that were reported to have occurred outside the VPD jurisdiction were excluded from the analyses.
The selection of explanatory variables that we hypothesized to be associated with drug seizures by police was informed by the lived and observational experiences of the authors and the previous literature about drug seizures by police in our study setting [ 5 , 10 , 11 , 15 ]. Additionally, the risk environment framework that has been used in the previous research characterizing PWUD–police interactions [ 16 , 17 , 18 , 19 , 20 ] prompted us to consider a range of social, structural, and environmental factors that may shape people’s experiences with drug seizures by police. Demographic variables included: age (continuous, per year increase); self-identified gender (man vs. woman, transgender or other); and self-identified ethnicity/ancestry (white vs. Indigenous or other persons of colour). Substance use-related variables referring to the past 6 months included: ≥ daily use of unregulated opioids (i.e. heroin, fentanyl, or down [a colloquial term locally used to refer to unregulated opioids]), unregulated stimulants (i.e. crystal methamphetamine or powder/crack cocaine), or cannabis, respectively; self-reported experience of opioid withdrawal, defined by answering yes to a question: ‘In the last 6 months, have you gone through opioid withdrawal (gotten dopesick)?’; always or usually (i.e. at least 75% of the time) injected drugs in public places (yes vs. < 75% of the time or not injected drugs); non-fatal overdose; and having administered naloxone to someone for overdose reversal. Social and structural exposures in the past 6 months included: homeless, sex work, working in unregulated drug markets (e.g. direct selling, middling, steering, holding, enforcing, cooking/packaging/producing, and supplying as defined in a previous study [ 21 ]), street-based income generation activities (e.g. recycling, panhandling, etc.), incarceration, and self-reported inability to access health and/or social services. The calendar year of interviews (2021 vs. 2019–2020) was also included to account for potential differences before and during the COVID-19 pandemic. Unless otherwise stated, all variables were dichotomized as yes vs. no. Missing responses were less than 3% (maximum 2.1%) per variable and were treated as missing in variable categorization and statistical analyses.
Primary analysis: factors associated with drug seizure by police in 2019–2021
We first examined the sample characteristics stratified by ever-reporting drug seizure during the study period, using the Wilcoxon rank-sum test (for age) and the Pearson’s Chi-squared test (for all other variables). Next, to account for the repeated measures, we used generalized estimating equations (GEE) with logit link to examine associations with drug seizure. We built a multivariable model by using an a priori-defined backward model selection procedure based on examination of Akaike Information Criterion and including all variables that were associated with the outcome at p < 0.10 in bivariable analyses in the initial full model [ 22 ]. The multicollinearity was assessed by checking the variance inflation factor with a cutoff of 5.0 [ 23 ].
Secondary analysis: trends of drug seizure between 2009–2012 and 2019–2021
We sought to examine whether the annual prevalence of drug seizure was significantly different between the two time periods (2009–2012 vs. 2019–2021) after accounting for potential differences in the sample characteristics. As a first step, we employed GEE with logit link to compare the characteristics of the participants in the two periods. We used all the variables used for the primary analysis as covariates, except for naloxone administration and opioid withdrawal because the questions for these two variables were not consistently asked during the 2009–2012 period. The calendar year of interviews used for the primary analysis (2021 vs. 2019–2020) was replaced with 2009–2012 vs. 2019–2021. We also added cohort designation (VIDUS vs. ACCESS vs. ARYS) as a covariate to account for potential differences across cohorts. Next, we included all variables that were associated with the variable comparing the two periods at p < 0.05 in bivariable analyses as covariates in a multivariable GEE model where drug seizure was the dependent variable, and the variable comparing the two periods was the primary independent variable. All p -values were two-sided. All statistical analyses were performed using SAS 9.4 (Cary, North Carolina, USA).
Factors associated with drug seizure during 2019–2021
A total of 995 participants were eligible for the primary analysis and contributed 1696 observations. Between 2019 and 2021, 63 (6.3%) participants had at least one report of drugs being seized, with a total of 68 reports (35 reports in 2019, 10 in 2020, and 23 in 2021). Of the 68 reports, 55 (80.9%) mentioned that it occurred in the DTES neighbourhood. Further, 42 (61.8%) reports also included the number of occurrences in the past 6 months, with 23 (54.8%) reporting once, 11 (26.2%) twice, and 8 (19.0%) more than twice. Table 1 shows some sample characteristics at their most recent study visit. As shown, the median age was 41 (1st and 3rd quartiles: 31 and 54) years, 588 (59.1%) self-identified as a man, and 540 (55.1%) self-identified as white, 382 (38.9%) as Indigenous, and 59 (6.0%) as other persons of colour. The prevalence of experiencing non-fatal overdose in the past 6 months was significantly higher among those who reported having their drugs seized compared to those who did not (30.2% vs. 18.3%, p = 0.020) as was the prevalence of experiencing opioid withdrawal in the past 6 months (71.4% vs. 48.8%, p = 0.001).
Table 2 presents the results of bivariable and multivariable GEE analyses. Following our modelling procedures, five variables remained in the final multivariable model, and all of them remained significantly associated with having one’s drugs seized: older age (adjusted odds ratio [AOR]: 0.97; 95% confidence interval [CI] 0.94–0.99), self-identifying as a man (AOR: 1.98; 95% CI 1.10–3.56), naloxone administration (AOR: 2.15; 95% CI 1.23–3.76), homelessness (AOR: 1.98; 95% CI 1.09–3.61), and working in the unregulated drug market (AOR: 4.93; 95% CI 2.87–8.49). We did not detect any collinearity.
Trends of drug seizure between 2009–2012 and 2019–2021
In total, 1894 VIDUS/ACCESS/ARYS participants were eligible for the secondary analysis and contributed 4607 observations. Of these individuals, 410 (21.7%) contributed at least one observation in each of the two time periods (2019–2021 and 2009–2012), 911 (48.1%) in 2009–2012 only, and 584 (30.8%) in 2019–2021 only. A total of 1266 (66.8%) participants completed more than one interview during the study period and were followed up for a median of 2.4 (1st and 3rd quartiles: 1.7 and 9.8) years. The median age at their most recent observation was 42 (1st and 3rd quartiles: 30 and 52) years, 1188 (63.2%) self-identified as a man, and 1080 (57.6%) self-identified as white, 679 (36.2%) as Indigenous, and 117 (6.2%) as other persons of colour.
Overall, 214 (11.3%) individuals reported having their drugs seized at least once with a total of 259 reports. Among the 214 participants, 149 (69.6%) were interviewed between 2009 and 2012 and answered the sub-question about what they did immediately afterwards. The most common response was acquiring more drugs (67.8%), followed by doing nothing (20.8%), got fronted drugs or money (5.4%), borrowed drugs or money (2.7%), and sold drugs (2.7%). The annual prevalence of drug seizure is shown in Table 3 . An average annual prevalence was 5.6%. In the GEE analyses, the variable comparing the two time periods (2019–2021 vs. 2009–2012) was not significantly associated with drug seizure in either the unadjusted (odds ratio: 0.85; 95% CI 0.64–1.15) or adjusted analysis (AOR: 0.93; 95% CI 0.64–1.35).
During the 16-month study period between June 2019 and November 2021 (June 2019–mid-March 2020 and June 2021–November 2021), 6% of our sample of people who used drugs daily in Vancouver reported having had their drugs seized by police without arrest at least once in the past 6 months. When examining the historical trends of annual prevalence, we found a declining trend in reports of drug seizure from 7% in 2009 to 3% in 2012, while the prevalence between June 2019 and mid-March 2020 and between June and November of 2021 (4–5%) remained essentially the same as the annual prevalence in 2011–2012. However, overall, the odds of drug seizure were not significantly different between the two time periods (2019–2021 vs. 2009–2012).
The low documented numbers of recommended charges for simple possession by the VPD are often cited to indicate success of VPD’s de facto depenalization policy [ 24 ]. Certainly, recommended charges for simple possession and drug seizure without arrest are two distinct practices and not directly comparable; however, given that statistics regarding the former are almost the only data used to assess the extent of depenalization, it is worth examining the potential discrepancy between the two to deepen our understanding of street-level drug law enforcement activities. For example, in 2019, VPD recommended 36 charges for simple possession to Crown Counsel [ 7 ]. In contrast, in our study, participants reported experiencing at least 35 drug seizures by police during the 6 months prior to their interview date between June and December 2019. The number of unique events was much higher than 35 given that a substantial portion of participants (approx. 45% of those who reported the number of occurrences of police seizure of drugs) experienced having their drugs seized more than once during the same 6-month period. These findings corroborate previous anecdotal reports [ 8 ] and show that drug seizure without arrest occurs more frequently than the VPD’s recommended charges for simple possession.
Some negative consequences of criminal justice involvement may be avoided by police not recommending charges for simple possession. However, we found that more than two-thirds of PWUD who were interviewed in 2009–2012 obtained more drugs immediately after police seized their drugs. These findings suggest that this policing practice may still lead to health and safety harms for PWUD. For example a previous qualitative study that interviewed PWUD in 2017 described that police seizure of drugs inadvertently promoted the creation of drug debts and increased the risk of drug market violence among PWUD [ 11 ]. Some PWUD were also forced to refill their drug supply hastily from an unknown unregulated drug market worker especially when experiencing withdrawal [ 11 , 25 ]. Each time an individual has to return to the unregulated market, especially if accessing drugs from an unknown source, they are increasing their risk of fatal or non-fatal overdose. In this regard, drug seizure essentially ‘mimics the health and safety harms associated with criminalization’ [ 15 ], undermining the intended benefits of the VPD’s depenalization policy. Of concern, a previous qualitative study reported that some police officers in BC believed that seizure of drugs is ‘beneficial for preventing harms, including overdose’, though it was not made clear whether it referred to VPD officers or other officers in BC or both [ 26 ].
When examining the data collected in 2019–2021, we also found that participants who administered naloxone to reverse someone’s overdose were more likely to have their drugs seized. As we did not directly ask our participants whether naloxone administration and police seizure of drugs occurred at the same time, future research needs to investigate this association in more depth. The VPD has a policy of non-attendance at overdose events unless requested by emergency health services [ 27 ]. However, a previous ethnographic study documented regular police presence in the DTES neighbourhood [ 28 ], which may mean that police officers are incidentally present near overdose events in public spaces. Even when police officers attend an overdose event, the Good Samaritan Drug Overdose Act (enacted in Canada in 2017) provides that no person who experiences or witnesses an overdose shall be charged or convicted for simple possession [ 29 ]. But if police is seizing drugs from PWUD who administered naloxone for overdose reversal at an overdose scene, the purpose of the Good Samaritan Drug Overdose Act is arguably undermined even in the absence of charges, because fear of police engagement at overdose events would persist among PWUD [ 29 ]. Indeed, a recent qualitative study based on interviews with PWUD in BC indicated that police seizure of drugs at overdose scenes was common, though it was not clear how common it was specifically in Vancouver [ 30 ]. Alternatively, PWUD who administered naloxone may have had their drugs seized by police at locations other than overdose scenes. Naloxone kits carried by these PWUD might ‘mark’ them as a person who uses drugs, thereby attracting police attention and resulting in drug seizures. Again, more research is needed to investigate detailed contexts around this finding.
Our results from the 2019–2021 data also demonstrated that those who were experiencing greater marginalization (e.g. homelessness and working in the unregulated drug market) were more likely to have their drugs seized. Overall, our research findings indicate that police seizure of drugs without arrest has potential to exacerbate ongoing health inequities and potentially undermine peer-based overdose prevention efforts. Therefore, the findings support calls for formally abolishing this discretionary policing practice. The efforts to achieve this goal may include Health Canada issuing a guidance about the harms of the practice to discourage police from engaging in it.
Our study results come at a crucial moment as BC will begin a trial period of ‘decriminalization’ respecting the simple possession of a cumulative quantity of 2.5 g of certain illicit drugs in January 2023, via a legal exemption under the federal drug law [ 31 ]. While in principle, the move could have public health benefits, unfortunately, feedback from PWUD communities and others indicates that the threshold quantity of drugs that defined simple possession is too low to be beneficial [ 32 , 33 , 34 ]. According to Health Canada, those who possess less than 2.5-g total of certain drugs for personal consumption will typically not be charged for simple possession and police will not seize those drugs [ 35 ]. Their approach to drug seizures (namely that ‘the drugs will not be seized’ if below 2.5 g [ 35 ]) was developed by BC’s Ministry of Mental Health and Addictions and Health Canada and would thus seem to suggest acknowledgement of the public health harms associated with the practice. However, it is unknown how BC’s ‘decriminalization’ model will influence drug seizures when people possess more than 2.5 g of drugs—or even when people possess less than that amount, given oft-noted discrepancies between policies and street-level practices [ 36 ]. Our findings suggest that it is important to evaluate the impacts of BC’s emerging policy on the police practice of seizing drugs without arrest particularly among PWUD who are socioeconomically more disadvantaged and more visible to police, including those who are homeless or working in the unregulated drug market for subsistence [ 21 ].
This study has limitations. First, a non-random sample limits the generalizability of our findings. Second, self-reported data may be influenced by some reporting bias, although reasonable validity of self-reports has been demonstrated in a similar population [ 37 ]. Third, data were not consistently collected between June 2009 and November 2021 (i.e. no data collection between December 2012 and May 2019 or between mid-March 2020 and May 2021), which made it challenging to determine the longitudinal patterns of drug seizure. Also, while we restricted the sample to those residing in the VPD jurisdiction and the cases of drug seizure between 2019 and 2021 to those reported to have occurred in the VPD jurisdiction, the outcome measure may still have included cases occurring outside the VPD jurisdiction due to potential self-report errors or missing responses to the locations of police drug seizures. Lastly, overall rates of police seizure of drugs ( with and without arrest) would be much higher than those identified in the present study, which focused on cases without arrest. Notably, in relation to their drug seizures data in 2019–2020, the VPD’s Director of Public Affairs also commented that smaller drug seizures often involved an arrest for another offence [ 9 , 38 ]. While the present study is limited in this regard, its unique strength is that it elucidated the extent to which police seizure of drugs occurred, even when PWUD were presumably not engaged in any serious offences that necessitated an arrest.
In sum, we found that 6% of our sample of PWUD in Vancouver had their drugs seized by police without arrest over a 16-month period in 2019–2021. In 2019, police seizure of drugs without arrest appeared to have occurred more frequently than simple possession charges recommended by the VPD. Drug seizures without arrest were concentrated among socioeconomically more marginalized PWUD and those who administered naloxone to others for overdose reversal. In addition, our data collected in 2009–2012 showed that the majority of PWUD who had their drugs seized acquired new drugs immediately following said seizure. This finding indicates that the police seizure of drugs without arrest can lead to more frequent interactions with the unregulated drug market, sometimes with direct impacts on their health and safety, including but not limited to fatal overdose. These findings call for abolishing this harmful discretionary policing practice that may aggravate ongoing health inequities and interfere with peer-based overdose responses.
Availability of data and materials
The data used for this study are not publicly available due to the way informed consent was obtained from study participants.
Abbreviations
AIDS Care Cohort to evaluate Exposure to Survival Services
Adjusted odds ratio
At-risk youth study
British Columbia
Confidence interval
Downtown eastside
Generalized estimating equations
People who use drugs
Vancouver Injection Drug Users Study
Vancouver Police Department
Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, et al. Public health and international drug policy. Lancet. 2016;387(10026):1427–80.
Article PubMed PubMed Central Google Scholar
Global Commission on Drug Policy. The war on drugs. 2011. https://www.globalcommissionondrugs.org/reports/the-war-on-drugs
Stevens A, Hughes CE, Hulme S, Cassidy R. Depenalization, diversion and decriminalization: a realist review and programme theory of alternatives to criminalization for simple drug possession. Eur J Criminol. 2022;19(1):29–54.
Article Google Scholar
Greer A, Bonn M, Shane C, Stevens A, Tousenard N, Ritter A. The details of decriminalization: designing a non-criminal response to the possession of drugs for personal use. Int J Drug Policy. 2022;102:103605.
Article PubMed Google Scholar
Vancouver Police Department. Vancouver Police Department drug policy. 2006 Sep. https://vpd.ca/wp-content/uploads/2021/06/vpd-policy-drug.pdf
Public Prosecution Service of Canada. 5.13 Prosecution of possession of controlled substances contrary to s.4(1) of the Controlled Drugs and Substances Act. 2020 August. https://www.ppsc-sppc.gc.ca/eng/pub/fpsd-sfpg/fps-sfp/tpd/p5/ch13.html
Vancouver Police Department. Records access request: 20-0484A. Vancouver, BC: Vancouver Police Department; 2020 July. https://vpd.ca/wp-content/uploads/2021/06/cleared-drug-charges-january-2014-to-present.pdf
Lupick T. Vancouver police stats suggest a softer touch on drugs but users say it’s a different story on the streets. The Georgia Straight. 2019 March 12. https://www.straight.com/news/1213101/vancouver-police-stats-suggest-softer-touch-drugs-users-say-its-different-story-streets
Vancouver Police Department. Records access request: 20-0493A. Vancouver, BC: Vancouver Police Department; 2020 July. https://vpd.ca/wp-content/uploads/2021/06/seized-illicit-substances-may-17-2019-to-june-9-20.pdf
Werb D, Wood E, Small W, Strathdee S, Li K, Montaner J, et al. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Int J Drug Policy. 2008;19(4):332–8.
Bennett D, Larkin D. Project inclusion: confronting anti-homeless and anti-substance user stigma in British Columbia. Vancouver, BC: PIVOT Legal Society; 2018. https://www.pivotlegal.org/project_inclusion_full
British Columbia Coroners Service. Illicit drug toxicity deaths in BC: January 1, 2012–June 30, 2022. Burnaby, BC: Ministry of Public Safety and Solicitor General; 2022 August. https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/illicit-drug.pdf
Wood E, Kerr T, Marshall BD, Li K, Zhang R, Hogg RS, et al. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. BMJ. 2009;338:b1649.
Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: the ARYS study. Harm Reduct J. 2006;3:18.
Shane C. Act now! Decriminalizing drugs in Vancouver. Vancouver, BC: Pivot Legal Society; 2021 September. https://d3n8a8pro7vhmx.cloudfront.net/pivotlegal/pages/3494/attachments/original/1639066365/Decriminalization_Report_Final_Revised.pdf
Rhodes T. The, “risk environment”: a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13(2):85–94.
Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy. 2009;20(3):193–201.
Hayashi K, Ti L, Csete J, Kaplan K, Suwannawong P, Wood E, et al. Reports of police beating and associated harms among people who inject drugs in Bangkok, Thailand: a serial cross-sectional study. BMC Public Health. 2013;13(1):733.
Hayashi K, Ti L, Buxton JA, Kaplan K, Suwannawong P, Wood E, et al. Experiences with urine drug testing by police among people who inject drugs in Bangkok, Thailand. Int J Drug Policy. 2014;25(2):297–302.
Chiu J, Burris S. Punitive drug law and the risk environment for injecting drug users: understanding the connections. In: The third meeting of the technical advisory group of the global commission on HIV and the law. 2012. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2102841
Kerr T, Small W, Johnston C, Li K, Montaner JS, Wood E. Characteristics of injection drug users who participate in drug dealing: implications for drug policy. J Psychoact Drugs. 2008;40(2):147–52.
Burnham KP, Anderson DR. Model selection and multimodel inference: a practical information-theoretic approach. 2nd ed. New York: Springer; 2002.
Google Scholar
James G, Witten D, Hastie T, Tibshirani R. Linear regression. In: An introduction to statistical learning: with applications in R. New York: Springer; 2013. p. 59–120.
Griffiths N. Drug possession charges vary widely by police. Vancouver Sun. 2020 December 25. https://vancouversun.com/news/drug-possession-charges-vary-widely-by-police
Bardwell G, Boyd J, Arredondo J, McNeil R, Kerr T. Trusting the source: the potential role of drug dealers in reducing drug-related harms via drug checking. Drug Alcohol Depend. 2019;198:1–6.
Greer A, Zakimi N, Butler A, Ferencz S. Simple possession as a “tool”: drug law enforcement practices among police officers in the context of depenalization in British Columbia, Canada. Int J Drug Policy. 2022;99:103471.
Vancouver Police Department. 1.6.28 guidelines for police attending illicit drug overdoses. In: Vancouver police department regulations and procedures manual. Vancouver, BC; 2006. https://vpd.ca/wp-content/uploads/2022/01/vpd-manual-regulations-procedures-p158.pdf
Collins AB, Boyd J, Mayer S, Fowler A, Kennedy MC, Bluthenthal RN, et al. Policing space in the overdose crisis: a rapid ethnographic study of the impact of law enforcement practices on the effectiveness of overdose prevention sites. Int J Drug Policy. 2019;73:199–207.
Government of Canada. About the Good Samaritan Drug Overdose Act. 2021. https://www.canada.ca/en/health-canada/services/substance-use/problematic-prescription-drug-use/opioids/about-good-samaritan-drug-overdose-act.html
Xavier J, Greer A, Pauly B, Loyal J, Mamdani Z, Ackermann E, et al. “There are solutions and I think we’re still working in the problem”: the limitations of decriminalization under the good Samaritan drug overdose act and lessons from an evaluation in British Columbia, Canada. Int J Drug Policy. 2022;105:103714.
British Columbia Government News. B.C. receives exemption to decriminalize possession of some illegal drugs for personal use. Victoria, BC; 2022 May. https://news.gov.bc.ca/releases/2022MMHA0029-000850
Ibrahim E. B.C.’s drug decriminalization threshold based on police input: Bennett. Vancouver Sun. 2022 Jun 2. https://vancouversun.com/news/local-news/bcs-drug-decriminalization-threshold-based-on-police-input-bennett
Canadian Drug Policy Coalition. Letter to Ministers Bennett and Duclos re: proposed cumulative threshold of 4.5 grams in B.C. 2022. https://drugpolicy.ca/letter-to-ministers-bennett-and-duclos-re-proposed-cumulative-threshold-of-4-5-grams-in-b-c/
Bardwell G, Mansoor M, Van Zwietering A, Cleveland E, Snell D, Kerr T. The, “goldfish bowl”: a qualitative study of the effects of heightened surveillance on people who use drugs in a rural and coastal Canadian setting. Harm Reduct J. 2022;19(1):136.
Government of Canada. Exemption from controlled drugs and substances act: personal possession of small amounts of certain illegal drugs in British Columbia (January 31, 2023–January 31, 2026). 2022. https://www.canada.ca/en/health-canada/services/health-concerns/controlled-substances-precursor-chemicals/policy-regulations/policy-documents/exemption-personal-possession-small-amounts-certain-illegal-drugs-british-columbia.html
Burris S, Blankenship KM, Donoghoe M, Sherman S, Vernick JS, Case P, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82(1):125–56.
Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–63.
Article CAS PubMed Google Scholar
Denis JS. How police drug seizures are making life worse on the Downtown Eastside. The Tyee. 2020 Sep 18. https://thetyee.ca/News/2020/09/18/Police-Drug-Seizures-DTES/
Download references
Acknowledgements
The VIDUS, ARYS, and ACCESS studies take place on the unceded territory of the Coast Salish Peoples, including the territories of the xwməθkwəy̓əm (Musqueam), Skwxwú7mesh (Squamish), Stó:lō, and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations. The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff.
The VIDUS, ARYS, and ACCESS studies were supported by the US National Institutes of Health (NIH) (U01DA038886 and U01DA021525). This study was undertaken, in part, thanks to funding from the William and Ada Isabelle Steel Fund through Simon Fraser University. KH holds the St. Paul’s Hospital Chair in Substance Use Research and is supported in part by the NIH (U01DA038886), a Michael Smith Foundation for Health Research (MSFHR) Scholar Award, and the St. Paul’s Foundation. TSK is supported by the Canada Graduate Scholarships Doctoral program award. MJM is supported by the NIH (U01DA0251525). KD is supported by a MSFHR/St. Paul’s Hospital Foundation–Providence Health Care Career Scholar Award. These funders did not have any role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Author information
Authors and affiliations.
British Columbia Centre On Substance Use, 400-1045 Howe Street, Vancouver, BC, V6Z 2A9, Canada
Kanna Hayashi, Tyson Singh Kelsall, Zishan Cui, M.-J. Milloy, Kora DeBeck & Thomas Kerr
Faculty of Health Sciences, Simon Fraser University, 8888 University Drive, Burnaby, BC, V5A 1S6, Canada
Kanna Hayashi & Tyson Singh Kelsall
Pivot Legal Society, 121 Heatley Avenue, Vancouver, BC, V6A 3E9, Canada
Caitlin Shane
School of Population and Public Health, University of British Columbia, 2206 East Mall, Vancouver, BC, V6T 1Z3, Canada
Department of Medicine, University of British Columbia, 2775 Laurel Street, 10th Floor, Vancouver, BC, V5Z 1M9, Canada
M.-J. Milloy & Thomas Kerr
School of Public Policy, Simon Fraser University, 515 West Hastings Street, Office 3269, Vancouver, BC, V6B 5K3, Canada
Kora DeBeck
You can also search for this author in PubMed Google Scholar
Vancouver Area Network of Drug Users
Contributions.
KH, KD, MJM, and TK obtained funding for, designed and managed the three cohort studies that the present study is built on. KH, TSK, and CS conceived and designed the present study. ZC conducted the statistical analyses. Several VANDU members provided feedback on the initial results and study design and validated the interpretation. KH wrote the first draft manuscript and incorporated the other co-authors’ input in the revised manuscript. All authors made significant contributions to the conceptions of the analyses, interpretation of the data, and writing and reviewing the manuscript. All authors (including the VANDU board) approved the final manuscript.
Corresponding author
Correspondence to Kanna Hayashi .
Ethics declarations
Ethics approval and consent to participate.
All three cohort studies (VIDUS, ACCESS, and ARYS) received ethics approval from the Providence Health Care/University of British Columbia Research Ethics Board (H14-01396 and H05-50233). Additionally, the Simon Fraser University Research Ethics Board (20190503) approved the present study. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
MJM’s institution has received an unstructured gift from NG Biomed, Ltd., to support his research. MJM is the Canopy Growth professor of cannabis science at the University of British Columbia, a position created by unstructured gifts to the university from Canopy Growth, a licenced producer of cannabis, and the Government of British Columbia’s Ministry of Mental Health and Addictions. The funder that supports MJM did not have any role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication. All authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hayashi, K., Singh Kelsall, T., Shane, C. et al. Police seizure of drugs without arrest among people who use drugs in Vancouver, Canada, before provincial ‘decriminalization’ of simple possession: a cohort study. Harm Reduct J 20 , 117 (2023). https://doi.org/10.1186/s12954-023-00833-7
Download citation
Received : 03 April 2023
Accepted : 17 July 2023
Published : 30 August 2023
DOI : https://doi.org/10.1186/s12954-023-00833-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Harm reduction
- Substance abuse
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
United Nations
Office on drugs and crime, press release , unodc world drug report 2021: pandemic effects ramp up drug risks, as youth underestimate cannabis dangers, 24 june 2021.
VIENNA, 24 June 2021 – Around 275 million people used drugs worldwide in the last year, while over 36 million people suffered from drug use disorders, according to the 2021 World Drug Report, released today by the United Nations Office on Drugs and Crime (UNODC).
The Report further noted that in the last 24 years cannabis potency had increased by as much as four times in parts of the world, even as the percentage of adolescents who perceived the drug as harmful fell by as much as 40 per cent, despite evidence that cannabis use is associated with a variety of health and other harms, especially among regular long-term users.
"Lower perception of drug use risks has been linked to higher rates of drug use, and the findings of UNODC’s 2021 World Drug Report highlight the need to close the gap between perception and reality to educate young people and safeguard public health,” said UNODC Executive Director Ghada Waly.
“The theme of this year’s International Day against Drug Abuse and Illicit Trafficking is “Share facts on drugs. Save lives”, emphasizing the importance of strengthening the evidence base and raising public awareness, so that the international community, governments, civil society, families and youth can make informed decisions, better target efforts to prevent and treat drug use, and tackle world drug challenges .”
According to the Report, the percentage of Δ9-THC – the main psychoactive component in cannabis - has risen from around six per cent to more than 11 per cent in Europe between 2002-2019, and around four per cent to 16 per cent in the United States between 1995-2019, while the percentage of adolescents that perceived cannabis as harmful declined by 40 per cent in the United States and by 25 per cent in Europe.
Moreover, most countries have reported a rise in the use of cannabis during the pandemic. In surveys of health professionals across 77 countries, 42 per cent asserted that cannabis use had increased. A rise in the non-medical use of pharmaceutical drugs has also been observed in the same period.
Drug Use Rising, but Science-Based Treatment More Available
Between 2010-2019 the number of people using drugs increased by 22 per cent, owing in part to global population growth. Based on demographic changes alone, current projections suggest an 11 per cent rise in the number of people who use drugs globally by 2030 -- and a marked increase of 40 per cent in Africa, due to its rapidly growing and young population.
According to the latest global estimates, about 5.5 per cent of the population aged between 15 and 64 years have used drugs at least once in the past year, while 36.3 million people, or 13 per cent of the total number of persons who use drugs, suffer from drug use disorders.
Globally, over 11 million people are estimated to inject drugs, half of whom are living with Hepatitis C. Opioids continue to account for the largest burden of disease attributed to drug use.
The two pharmaceutical opioids most commonly used to treat people with opioid use disorders, methadone and buprenorphine, have become increasingly accessible over the past two decades. The amount available for medical use has increased six-fold since 1999, from 557 million daily doses to 3,317 million by 2019, indicating that science-based pharmacological treatment is more available now than in the past.
The Dark Web
Drug markets on the dark web only emerged a decade ago but major ones are now worth at least US$ 315 million in annual sales. Although this is just a fraction of overall drug sales, the trend is upwards with a fourfold increase between 2011 to mid-2017 and mid-2017 to 2020.
Rapid technological innovation, combined with the agility and adaptability of those using new platforms to sell drugs and other substances, is likely to usher in a globalized market where all drugs are more available and accessible everywhere. This, in turn, could trigger accelerated changes in patterns of drug use and entail public health implications, according to the Report.
The Drug Market Rebounds and Shifts
The new report shows that drug markets have swiftly resumed operations after the initial disruption at the onset of the pandemic; a burst that has triggered or accelerated certain pre-existing trafficking dynamics across the global drug market. Among these are: increasingly larger shipments of illicit drugs, a rise in the frequency of overland and water-way routes used for trafficking, greater use of private planes for the purpose of drug trafficking, and an upsurge in the use of contactless methods to deliver drugs to end-consumers.
The resilience of drug markets during the pandemic has demonstrated once again traffickers’ ability to adapt quickly to changed environments and circumstances.
The Report also noted that cocaine supply chains to Europe are diversifying, pushing prices down and quality up and thereby threatening Europe with a further expansion of the cocaine market. This is likely to widen the potential harm caused by the drug in the region.
The number of new psychoactive substances (NPS) emerging on the global market fell from 163 in 2013 to 71 in 2019. This reflects trends in North America, Europe and Asia. The findings suggest national and international control systems have succeeded in limiting the spread of NPS in high income countries,where NPS first emerged a decade ago.
Drug Risks, New Developments Spurred by Pandemic
COVID-19 has triggered innovation and adaptation in drug prevention and treatment services through more flexible models of service delivery. Many countries have introduced or expanded telemedicine services due to the pandemic, which for drug users means that healthcare workers can now offer counselling or initial assessments over the telephone and use electronic systems to prescribe controlled substances.
While the impact of COVID-19 on drug challenges is not yet fully known, the analysis suggests that the pandemic has brought increasing economic hardship that is likely to make illicit drug cultivation more appealing to fragile rural communities. The social impact of the pandemic – driving a rise in inequality, poverty, and mental health conditions particularly among already vulnerable populations – represent factors that could push more people into drug use.
The World Drug Report and further content is available here: https://wdr.unodc.org/
The 2021 World Drug Report provides a global overview of the supply and demand of opiates, cocaine, cannabis, amphetamine-type stimulants and new psychoactive substances (NPS), as well as their impact on health, taking into account the possible effects of the COVID-19 pandemic.
For further information and interview requests, please contact:
- Fraud Alert
- Legal Notice
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Glob Health
- v.85(1); 2019

The Manila Declaration on the Drug Problem in the Philippines
Nymia simbulan.
1 University of Southern California, US
Leonardo Estacio
Carissa dioquino-maligaso, teodoro herbosa, mellissa withers.
2 University of the Philippines, PH
When Philippine President Rodrigo R. Duterte assumed office in 2016, his government launched an unprecedented campaign against illegal drugs. The drug problem in the Philippines has primarily been viewed as an issue of law enforcement and criminality, and the government has focused on implementing a policy of criminalization and punishment. The escalation of human rights violations has caught the attention of groups in the Philippines as well as the international community. The Global Health Program of the Association of Pacific Rim Universities (APRU), a non-profit network of 50 universities in the Pacific Rim, held its 2017 annual conference in Manila. A special half-day workshop was held on illicit drug abuse in the Philippines which convened 167 participants from 10 economies and 21 disciplines. The goal of the workshop was to collaboratively develop a policy statement describing the best way to address the drug problem in the Philippines, taking into consideration a public health and human rights approach to the issue. The policy statement is presented here.
When Philippine President Rodrigo R. Duterte assumed office on June 30, 2016, his government launched an unprecedented campaign against illegal drugs. He promised to solve the illegal drug problem in the country, which, according to him, was wreaking havoc on the lives of many Filipino families and destroying the future of the Filipino youth. He declared a “war on drugs” targeting users, peddlers, producers and suppliers, and called for the Philippine criminal justice system to put an end to the drug menace [ 1 ].
According to the Dangerous Drugs Board (DDB) (the government agency mandated to formulate policies on illegal drugs in the Philippines), there are 1.8 million current drug users in the Philippines, and 4.8 million Filipinos report having used illegal drugs at least once in their lives [ 2 ]. More than three-quarters of drug users are adults (91%), males (87%), and have reached high school (80%). More than two-thirds (67%) are employed [ 2 ]. The most commonly used drug in the Philippines is a variant of methamphetamine called shabu or “poor man’s cocaine.” According to a 2012 United Nations report, the Philippines had the highest rate of methamphetamine abuse among countries in East Asia; about 2.2% of Filipinos between the ages 16–64 years were methamphetamines users.
The drug problem in the Philippines has primarily been viewed as an issue of law enforcement and criminality, and the government has focused on implementing a policy of criminalization and punishment. This is evidenced by the fact that since the start of the “war on drugs,” the Duterte government has utilized punitive measures and has mobilized the Philippine National Police (PNP) and local government units nationwide. With orders from the President, law enforcement agents have engaged in extensive door-to-door operations. One such operation in Manila in August 2017 aimed to “shock and awe” drug dealers and resulted in the killing of 32 people by police in one night [ 3 ].
On the basis of mere suspicion of drug use and/or drug dealing, and criminal record, police forces have arrested, detained, and even killed men, women and children in the course of these operations. Male urban poor residents in Metro Manila and other key cities of the country have been especially targeted [ 4 ]. During the first six months of the Duterte Presidency (July 2016–January 2017), the PNP conducted 43,593 operations that covered 5.6 million houses, resulting in the arrest of 53,025 “drug personalities,” and a reported 1,189,462 persons “surrendering” to authorities, including 79,349 drug dealers and 1,110,113 drug users [ 5 ]. Government figures show that during the first six months of Duterte’s presidency, more than 7,000 individuals accused of drug dealing or drug use were killed in the Philippines, both from legitimate police and vigilante-style operations. Almost 2,555, or a little over a third of people suspected to be involved in drugs, have been killed in gun battles with police in anti-drug operations [ 5 , 6 ]. Community activists estimate that the death toll has now reached 13,000 [ 7 ]. The killings by police are widely believed to be staged in order to qualify for the cash rewards offered to policeman for killing suspected drug dealers. Apart from the killings, the recorded number of “surrenderees” resulting in mass incarceration has overwhelmed the Philippine penal system, which does not have sufficient facilities to cope with the population upsurge. Consequently, detainees have to stay in overcrowded, unhygienic conditions unfit for humans [ 8 ].
The escalation of human rights violations, particularly the increase in killings, both state-perpetrated and vigilante-style, has caught the attention of various groups and sectors in society including the international community. Both police officers and community members have reported fear of being targeted if they fail to support the state-sanctioned killings [ 9 ]. After widespread protests by human rights groups, Duterte called for police to shoot human rights activists who are “obstructing justice.” Human Rights organizations, such as Human Rights Watch and Amnesty International, have said that Duterte’s instigation of unlawful police violence and the incitement of vigilante killings may amount to crimes against humanity, violating international law [ 10 , 11 ]. The European Union found that human rights have deteriorated significantly since Duterte assumed power, saying “The Philippine government needs to ensure that the fight against drug crimes is conducted within the law, including the right to due process and safeguarding of the basic human rights of citizens of the Philippines, including the right to life, and that it respects the proportionality principle [ 12 ].” Despite the fact that, in October 2017, Duterte ordered the police to end all operations in the war on drugs, doubts remain as to whether the state-sanctioned killings will stop [ 13 ]. Duterte assigned the Philippine Drug Enforcement Agency (PDEA) to be the sole anti-drug enforcement agency.
Duterte’s war on drugs is morally and legally unjustifiable and has created large-scale human rights violations; and is also counterproductive in addressing the drug problem. International human rights groups and even the United Nations have acknowledged that the country’s drug problem cannot be resolved using a punitive approach, and the imposition of criminal sanctions and that drug users should not be viewed and treated as criminals [ 14 ]. Those critical of the government’s policy towards the illegal drug problem have emphasized that the drug issue should be viewed as a public health problem using a rights-based approach (RBA). This was affirmed by UN Secretary General Ban Ki Moon on the 2015 International Day Against Drug Abuse and Illegal Trafficking when he stated, “…We should increase the focus on public health, prevention, treatment and care, as well as on economic, social and cultural strategies [ 15 ].” The United Nations Human Rights Council released a joint statement in September 2017, which states that the human rights situation in the Philippines continued to cause serious concern. The Council urged the government of the Philippines to “take all necessary measures to bring these killings to an end and cooperate with the international community to pursue appropriate investigations into these incidents, in keeping with the universal principles of democratic accountability and the rule of law [ 16 ].” In October 2017, the Philippines Dangerous Drug Board (DDB) released a new proposal for an anti-drug approach that protects the life of the people. The declaration includes an implicit recognition of the public health aspect of illegal drug use, “which recognizes that the drug problem as both social and psychological [ 16 ].”
Workshop on Illicit Drug Abuse in the Philippines
The Association of Pacific Rim Universities (APRU) is a non-profit network of 50 leading research universities in the Pacific Rim region, representing 16 economies, 120,000 faculty members and approximately two million students. Launched in 2007, the APRU Global Health Program (GHP) includes approximately 1,000 faculty, students, and researchers who are actively engaged in global health work. The main objective of the GHP is to advance global health research, education and training in the Pacific Rim, as APRU member institutions respond to global and regional health challenges. Each year, about 300 APRU GHP members gather at the annual global health conference, which is hosted by a rotating member university. In 2017, the University of the Philippines in Manila hosted the conference and included a special half-day workshop on illicit drug abuse in the Philippines.
Held on the first day of the annual APRU GHP conference, the workshop convened 167 university professors, students, university administrators, government officials, and employees of non-governmental organizations (NGO), from 21 disciplines, including anthropology, Asian studies, communication, dentistry, development, education, environmental health, ethics, international relations, law, library and information science, medicine, nutrition, nursing, occupational health, pharmaceutical science, physical therapy, political science, psychology, public health, and women’s studies. The participants came from 10 economies: Australia, China, Hong Kong, Indonesia, Japan, Mexico, Nepal, the Philippines, Thailand, and the US. The special workshop was intended to provide a venue for health professionals and workers, academics, researchers, students, health rights advocates, and policy makers to: 1) give an overview on the character and state of the drug problem in the Philippines, including the social and public health implications of the problem and the approaches being used by the government in the Philippines; 2) learn from the experiences of other countries in the handling of the drug and substance abuse problem; and 3) identify appropriate methods and strategies, and the role of the health sector in addressing the problem in the country. The overall goal of the workshop was to collaboratively develop a policy statement describing the best way to address this problem in a matnner that could be disseminated to all the participants and key policymakers both in the Philippines, as well as globally.
The workshop included presentations from three speakers and was moderated by Dr. Carissa Paz Dioquino-Maligaso, head of the National Poison Management and Control Center in the Philippines. The first speaker was Dr. Benjamin P. Reyes, Undersecretary of the Philippine Dangerous Drugs Board, who spoke about “the State of the Philippine Drug and Substance Abuse Problem in the Philippines.” The second speaker was Dr. Joselito Pascual, a medical specialist from the Department of Psychiatry and Behavioral Medicine, at the University of the Philippines General Hospital in Manila. His talk was titled “Psychotropic Drugs and Mental Health.” The final speaker was Patrick Loius B. Angeles, a Policy and Research Officer of the NoBox Transitions Foundation, whose talk was titled “Approaches to Addressing the Drug and Substance Abuse Problem: Learning from the Experiences of Other Countries.” Based on the presentations, a draft of the Manila Declaration on the Drug Problem in the Philippines was drafted by the co-authors of this paper. The statement was then sent to the workshop participants for review and comments. The comments were reviewed and incorporated into the final version, which is presented below.
Declaration
“Manila Statement on the Drug Problem in the Philippines”
Gathering in this workshop with a common issue and concern – the drug problem in the Philippines and its consequences and how it can be addressed and solved in the best way possible;
Recognizing that the drug problem in the Philippines is a complex and multi-faceted problem that includes not only criminal justice issues but also public health issues and with various approaches that can be used in order to solve such;
We call for drug control policies and strategies that incorporate evidence-based, socially acceptable, cost-effective, and rights-based approaches that are designed to minimize, if not to eliminate, the adverse health, psychological, social, economic and criminal justice consequences of drug abuse towards the goal of attaining a society that is free from crime and drug and substance abuse;
Recognizing, further, that drug dependency and co-dependency, as consequences of drug abuse, are mental and behavioral health problems, and that in some areas in the Philippines injecting drug use comorbidities such as the spread of HIV and AIDS are also apparent, and that current prevention and treatment interventions are not quite adequate to prevent mental disorders, HIV/AIDS and other co-morbid diseases among people who use drugs;
Affirming that the primacy of the sanctity/value of human life and the value of human dignity, social protection of the victims of drug abuse and illegal drugs trade must be our primary concern;
And that all health, psycho-social, socio-economic and rights-related interventions leading to the reduction or elimination of the adverse health, economic and social consequences of drug abuse and other related co-morbidities such as HIV/AIDS should be considered in all plans and actions toward the control, prevention and treatment of drug and substance abuse;
As a community of health professionals, experts, academics, researchers, students and health advocates, we call on the Philippine government to address the root causes of the illegal drug problem in the Philippines utilizing the aforementioned affirmations . We assert that the drug problem in the country is but a symptom of deeper structural ills rooted in social inequality and injustice, lack of economic and social opportunities, and powerlessness among the Filipino people. Genuine solutions to the drug problem will only be realized with the fulfillment and enjoyment of human rights, allowing them to live in dignity deserving of human beings. As members of educational, scientific and health institutions of the country, being rich and valuable sources of human, material and technological resources, we affirm our commitment to contribute to solving this social ill that the Philippine government has considered to be a major obstacle in the attainment of national development.
The statement of insights and affirmations on the drug problem in the Philippines is a declaration that is readily applicable to other countries in Asia where approaches to the problem of drug abuse are largely harsh, violent and punitive.
As a community of scholars, health professionals, academics, and researchers, we reiterate our conviction that the drug problem in the Philippines is multi-dimensional in character and deeply rooted in the structural causes of poverty, inequality and powerlessness of the Filipino people. Contrary to the government’s position of treating the issues as a problem of criminality and lawlessness, the drug problem must be addressed using a holistic and rights-based approach, requiring the mobilization and involvement of all stakeholders. This is the message and the challenge which we, as members of the Association of Pacific Rim Universities, want to relay to the leaders, policymakers, healthcare professionals, and human rights advocates in the region; we must all work together to protect and promote health and well being of all populations in our region.
Competing Interests
The authors have no competing interests to declare.

COMMENTS
Teen Cocaine Addiction Case Study: Chloe's Story This case study of drug addiction can affect anyone - it doesn't discriminate on the basis of age, gender or background. At Serenity Addiction Centres, our drug detox clinic is open to everyone, and our friendly and welcoming approach is changing the way rehab clinics are helping clients recover from addiction.
A case study is provided to illustrate the high level of scrutiny of study protocols involving the participation of illicit drug users and the effect of such scrutiny on recruitment of participants. The article concludes with a discussion of the effects of the current political climate on the recruitment of illicit drug users in research.
Researchers at RAND recently published the most comprehensive study to date on what's driving the crisis, how it could play out in the future, and what may be done to save more lives. Among their findings: Fentanyl is unlike any other drug problem in modern history. It's more useful to think of it as a mass poisoning than as a traditional drug epidemic. The crisis is likely to get worse ...
Illegal drug use increases the likelihood of continued involvement in criminal activity, with high rates of relapse and recidivism found among drug-involved offenders; 68% of drug offenders are rearrested within 3 years of release from prison [ 12 ].
According to research studies, marijuana use causes aggressive behavior, causes or exacerbates psychosis, and produces paranoia. These effects have been illustrated through case studies of highly publicized incidents and heightened political profiles.
A report from the National Drug Intelligence Center 14 estimated that the cost to society for drug use was $193 billion in 2007, a substantial portion of which—$113 billion—was associated with drug related crime, including criminal justice system costs and costs borne by victims of crime. The same report showed that the cost of treating ...
Substance Use Disorder in the U.S. 11.7% of Americans 12 and over use illegal drugs. 53 million or 19.4% of people 12 and over have used illegal drugs or misused prescription drugs within the last year. If alcohol and tobacco are included, 165 million, or 60.2% of Americans ages 12 years or older currently abuse drugs.
Using overdose Good Samaritan Laws (GSLs) as a case study, we argue that public health-oriented policy changes made in some states are undercut by the broader enduring environment of a structurally racist drug criminalization agenda that continues to permeate and constrict most attempts at change.
A case study is provided to illustrate the high level of scrutiny of study protocols involving the participation of illicit drug users and the effect of such scrutiny on recruitment of participants. The article concludes with a discussion of the effects of the current political climate on the recruitment of illicit drug users in research.
NIDA uses multiple sources to monitor the prevalence and trends regarding drug use in the United States. The resources cover a variety of drug-related issues, including information on drug use, emergency room data, prevention and treatment programs, and other research findings.
The purpose is to help the patient understand the trajectory and modifiable contextual factors associated with drug use, challenge unhelpful positive drug use expectancies, identify possible skills deficiencies as well as seeking functionally equivalent non- drug using behaviours so as to reduce the probability of future drug use.
This report describes different routes of drug use observed in drug overdose deaths.
Studies by the Centers for Disease Control and Prevention and the Mayo Clinic also found healthcare workers who steal drugs frequently tamper with medications, leaving them contaminated.
There has been advocacy for legalization of abusable substances, but systematic data on societal beliefs regarding such legalization are limited. People who use substances may have unique beliefs about legalization, and this study assessed whether they ...
The world's drug problem remains an urgent challenge that threatens to exacerbate COVID-19 pandemic impacts and hinder a healthy and inclusive recovery, warned the UN Secretary General ahead of The International Day Against Drug Abuse and Illicit Trafficking.
Cocaine and heroin were also significant contributors, found in 41.6% and 29.6% of cases, respectively. Nearly 80% of overdose deaths involved the use of multiple substances. Despite the presence of bystanders in more than half the cases, most victims (74.9%) were using drugs alone at the time of their fatal overdose, mainly at home.
Background Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Methods Preferred Reporting Items for Systematic Reviews and ...
Background Several jurisdictions in Canada have recently considered decriminalizing possession of illicit drugs for personal use (henceforth, simple possession) as part of their responses to the ongoing drug toxicity/overdose crisis. In this context, we sought to examine an early implementation case of a de facto depenalization policy of simple possession offences in Vancouver, Canada, that ...
We focus on illicit drug use while admitted to hospital and how PWUD and health care providers describe, respond, and attempt to manage its use.
A study investigating the relationship between the influence of the family and behaviors among adolescents that put their health at risk reported that family connectedness was significantly inversely associated with alcohol and drug use [ 9 ].
How did the pandemic affect drug use and risks? Find out in the UNODC World Drug Report 2021, a comprehensive analysis of global drug trends.
Drug trafficking is the phrase used to describe the smuggling of narcotics including marijuan. a, cocaine, heroin, and other illicit substances over state lines and into other nations. While ...
Abstract This paper investigates options available to policy makers responding to the challenges of drug use in modern society, focussing on the UK. It investigates the failings of prohibition policy that has driven historic reactions to drugs, drug use and drug users globally, nationally and locally.
Conclusion. The statement of insights and affirmations on the drug problem in the Philippines is a declaration that is readily applicable to other countries in Asia where approaches to the problem of drug abuse are largely harsh, violent and punitive. As a community of scholars, health professionals, academics, and researchers, we reiterate our ...