

45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay On Covid-19: 100, 200 and 300 Words

- Updated on
- Apr 30, 2024

COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to many countries, causing widespread illness and impacting our lives in numerous ways. This blog talks about the details of this virus and also drafts an essay on COVID-19 in 100, 200 and 300 words for students and professionals.
Table of Contents
- 1 Essay On COVID-19 in English 100 Words
- 2 Essay On COVID-19 in 200 Words
- 3 Essay On COVID-19 in 300 Words
- 4 Short Essay on Covid-19
Essay On COVID-19 in English 100 Words
COVID-19, also known as the coronavirus, is a global pandemic. It started in late 2019 and has affected people all around the world. The virus spreads very quickly through someone’s sneeze and respiratory issues.
COVID-19 has had a significant impact on our lives, with lockdowns, travel restrictions, and changes in daily routines. To prevent the spread of COVID-19, we should wear masks, practice social distancing, and wash our hands frequently.
People should follow social distancing and other safety guidelines and also learn the tricks to be safe stay healthy and work the whole challenging time.
Also Read: National Safe Motherhood Day 2023
Essay On COVID-19 in 200 Words
COVID-19 also known as coronavirus, became a global health crisis in early 2020 and impacted mankind around the world. This virus is said to have originated in Wuhan, China in late 2019. It belongs to the coronavirus family and causes flu-like symptoms. It impacted the healthcare systems, economies and the daily lives of people all over the world.
The most crucial aspect of COVID-19 is its highly spreadable nature. It is a communicable disease that spreads through various means such as coughs from infected persons, sneezes and communication. Due to its easy transmission leading to its outbreaks, there were many measures taken by the government from all over the world such as Lockdowns, Social Distancing, and wearing masks.
There are many changes throughout the economic systems, and also in daily routines. Other measures such as schools opting for Online schooling, Remote work options available and restrictions on travel throughout the country and internationally. Subsequently, to cure and top its outbreak, the government started its vaccine campaigns, and other preventive measures.
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness.
Also Read : Essay on My Best Friend
Essay On COVID-19 in 300 Words
COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide. It was first discovered in late 2019 in Cina and then got spread in the whole world. It had a major impact on people’s life, their school, work and daily lives.
COVID-19 is primarily transmitted from person to person through respiratory droplets produced and through sneezes, and coughs of an infected person. It can spread to thousands of people because of its highly contagious nature. To cure the widespread of this virus, there are thousands of steps taken by the people and the government.
Wearing masks is one of the essential precautions to prevent the virus from spreading. Social distancing is another vital practice, which involves maintaining a safe distance from others to minimize close contact.
Very frequent handwashing is also very important to stop the spread of this virus. Proper hand hygiene can help remove any potential virus particles from our hands, reducing the risk of infection.
In conclusion, the Coronavirus has changed people’s perspective on living. It has also changed people’s way of interacting and how to live. To deal with this virus, it is very important to follow the important guidelines such as masks, social distancing and techniques to wash your hands. Getting vaccinated is also very important to go back to normal life and cure this virus completely.
Also Read: Essay on Abortion in English in 650 Words
Short Essay on Covid-19
Please find below a sample of a short essay on Covid-19 for school students:
Also Read: Essay on Women’s Day in 200 and 500 words
to write an essay on COVID-19, understand your word limit and make sure to cover all the stages and symptoms of this disease. You need to highlight all the challenges and impacts of COVID-19. Do not forget to conclude your essay with positive precautionary measures.
Writing an essay on COVID-19 in 200 words requires you to cover all the challenges, impacts and precautions of this disease. You don’t need to describe all of these factors in brief, but make sure to add as many options as your word limit allows.
The full form for COVID-19 is Corona Virus Disease of 2019.
Related Reads
Hence, we hope that this blog has assisted you in comprehending with an essay on COVID-19. For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Simran Popli
An avid writer and a creative person. With an experience of 1.5 years content writing, Simran has worked with different areas. From medical to working in a marketing agency with different clients to Ed-tech company, the journey has been diverse. Creative, vivacious and patient are the words that describe her personality.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
Facts about coronavirus
What kids need to know
Coronavirus (or, as doctors and scientists call it, COVID-19) has been part of everyone’s life since mid-March 2020, when most schools, businesses, and communities quickly changed how they operated to prevent the spread of the virus. Because the disease infected a large number of people all over the world, experts call this a pandemic.
For over a year, many kids attended school at least partly from their houses; their parents might’ve worked from home, too. This was all to avoid catching the virus from other people outside the home.
Lots of people helped their neighbors throughout the pandemic. First responders, like healthcare workers, police officers, and firefighters, kept people healthy and safe; essential workers such as grocery store employees, delivery drivers, and postal workers worked in-person to make sure other folks had what they needed to live.
Nearly 190 million people in the world have been infected by COVID-19, and more than four million people have died. But the good news is that the number of people getting the virus in the United States is going way down, thanks to testing, vaccines, and other preventative measures, like wearing masks and social distancing.
Here are answers to some questions you might still have about coronavirus.
So … what is COVID-19? And what’s a "coronavirus?"
The term "coronavirus" actually refers to a family of viruses that causes many different types of diseases, including the common cold. COVID-19 is a "novel coronavirus," which means it’s a new disease unfamiliar to scientists and doctors. Its name is actually a mash-up of three words: CO stands for "corona," which means "crown" in Latin, and the viruses are named for the crown-like spikes on their surface; VI stands for "virus"; and D is for "disease." The "19" comes from the year 2019, when the disease was first detected.
How did COVID-19 start?
Scientists don’t know the exact origin of COVID -19, and they might never have all the answers. But they do know that some diseases start in animals before spreading to humans. These types of diseases are called zoonotic (pronounced zoh-uh-NAH-tik). Cows, bats, and camels are among the animals that have spread diseases to humans in the past. The COVID-19 disease is also zoonotic, with the first cases popping up in December 2019 in Wuhan, China. The affected humans were all connected to a nearby market that sold live animals.
How does someone catch COVID-19?
COVID-19 can be transmitted by little droplets from coughs or sneezes, which is why doctors say unvaccinated people should wear masks when they’re indoors or close to others. According to the Centers for Disease Control and Prevention (CDC), there's no evidence that a dog, cat, or any other pet can transmit COVID-19. But more studies are needed to understand how COVID-19 could affect different types of animals.
How can I protect myself?
Kids older than 12 can now get the Pfizer COVID-19 vaccine. For older kids who aren’t vaccinated, as well as kids 11 and younger, research shows that taking small steps—like staying six feet (about two arm lengths) from others, wearing face masks that cover the mouth and nose, washing hands often, and seeing friends outside—can make a big difference in stopping the spread of the virus. (Vaccines for kids under 12 are expected to be available later in 2021.)
Learn how vaccines work and why they’re so effective .
OK, but what happens if I do get it?
Most people—including kids— who catch COVID-19 get better, and their illness is usually mild. But if you do catch COVID-19, you might have a dry cough, a fever, and shortness of breath. But just like when you’ve had a cold, the best treatment is to stay in bed—and away from anyone who might catch it from you. (Like your grandparents! Older people are more at risk for catching and getting sick from COVID-19 .) You might also not even know you have it, so keep washing your hands and wearing a mask, just in case. Masks work best when everyone wears one.
Will it go away?
Researchers expect that as more people are vaccinated and become immune to COVID-19, the number of cases will continue to go down. Immunity to the virus means the body can fight it off and won’t spread it to another person. When enough people are immune to COVID-19 so that the illness is no longer a serious threat, that’s called herd immunity . Experts say that for herd immunity to work in a community, between 75 and 85 percent of people need to be vaccinated. Almost 60 percent of Americans are fully vaccinated, depending on where you live: Some places are higher, and others are lower.
The majority of new cases in the United States are in unvaccinated people. They can also transmit the coronavirus to others, which is why the CDC recommends they still wear masks indoors and at crowded outdoor events.
What about school?
The latest guidelines from the CDC say that students and teachers who are fully vaccinated—meaning it’s been two weeks since their second COVID-19 shot—can be in class without masks. For students too young to get the vaccine, the recommendation is to keep doing what you’ve been doing in school: wear masks and social distance. Scientists say that keeping just three feet indoors in school is enough to keep kids safe.
This story has been updated with new information about vaccines for children.
Read This Next
Coronavirus glossary, science lab, weird but true: humans, how things work.
- Terms of Use
- Privacy Policy
- Your California Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell My Info
- National Geographic
- National Geographic Education
- Shop Nat Geo
- Customer Service
- Manage Your Subscription
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved

Listen Live

Go behind the headlines: From the economy and healthcare to politics and the environment - and so much more - On Point talks with newsmakers and real people about the issues that matter most. On Point is produced by WBUR for NPR.
Coronavirus: The world has come together to flatten the curve. Can we stay united to tackle other crises?
Watching the world come together gives me hope for the future, writes mira patel, a high school junior..

Mira Patel and her sister Veda. (Courtesy of Dee Patel)
Related Content

This 24-year-old entrepreneur is helping Black-owned restaurants survive coronavirus
Black and Mobile is an online delivery service that caters to Black-owned restaurants. The coronavirus shutdown has increased demand for its service.
4 years ago

Home desks won’t replace Philly’s high-rise office towers anytime soon, analysts say
Philadelphia’s office market might fare better post-coronavirus than those of other U.S. cities, CBRE analysts said in a new report.
Before the pandemic, I had often heard adults say that young people would lose the ability to connect in-person with others due to our growing dependence on technology and social media. However, this stay-at-home experience has proven to me that our elders’ worry is unnecessary. Because isolation isn’t in human nature, and no advancement in technology could replace our need to meet in person, especially when it comes to learning.
As the weather gets warmer and we approach summertime, it’s going to be more and more tempting for us teenagers to go out and do what we have always done: hang out and have fun. Even though the decision-makers are adults, everyone has a role to play and we teens can help the world move forward by continuing to self-isolate. It’s incredibly important that in the coming weeks, we respect the government’s effort to contain the spread of the coronavirus.
In the meantime, we can find creative ways to stay connected and continue to do what we love. Personally, I see many 6-feet-apart bike rides and Zoom calls in my future.
If there is anything that this pandemic has made me realize, it’s how connected we all are. At first, the infamous coronavirus seemed to be a problem in China, which is worlds away. But slowly, it steadily made its way through various countries in Europe, and inevitably reached us in America. What was once framed as a foreign virus has now hit home.
Watching the global community come together, gives me hope, as a teenager, that in the future we can use this cooperation to combat climate change and other catastrophes.
As COVID-19 continues to creep its way into each of our communities and impact the way we live and communicate, I find solace in the fact that we face what comes next together, as humanity.
When the day comes that my generation is responsible for dealing with another crisis, I hope we can use this experience to remind us that moving forward requires a joint effort.
Mira Patel is a junior at Strath Haven High School and is an education intern at the Foreign Policy Research Institute in Philadelphia. Follow her on Instagram here.
Becoming a storyteller at WHYY, your local public media station, is easier than you might think. Text STORYTELLER to 267-494-9949 to learn more.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
Part of the series

Coronavirus Pandemic
You may also like.
Threats and violence suspend high school football games Friday night
Fight breaks out at a game between Pennsauken and Camden High Schools, threats suspend games in Chester and Northampton Counties.
3 years ago

Philly students get vaxxed at the zoo before heading back to school
The event is the first of its kind for the school district, but arrives after months of partnering with CHOP to organize other vaccination clinics around the city.

Montco high school senior reflects on missing experiences because of coronavirus
Grace Honeyman, a senior at Harriton High School, talks with her father about how she’s dealing with missing milestones due to coronavirus.
Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The Effect of COVID-19 on Education
Jacob hoofman.
a Wayne State University School of Medicine, 540 East Canfield, Detroit, MI 48201, USA
Elizabeth Secord
b Department of Pediatrics, Wayne Pediatrics, School of Medicine, Pediatrics Wayne State University, 400 Mack Avenue, Detroit, MI 48201, USA
COVID-19 has changed education for learners of all ages. Preliminary data project educational losses at many levels and verify the increased anxiety and depression associated with the changes, but there are not yet data on long-term outcomes. Guidance from oversight organizations regarding the safety and efficacy of new delivery modalities for education have been quickly forged. It is no surprise that the socioeconomic gaps and gaps for special learners have widened. The medical profession and other professions that teach by incrementally graduated internships are also severely affected and have had to make drastic changes.
- • Virtual learning has become a norm during COVID-19.
- • Children requiring special learning services, those living in poverty, and those speaking English as a second language have lost more from the pandemic educational changes.
- • For children with attention deficit disorder and no comorbidities, virtual learning has sometimes been advantageous.
- • Math learning scores are more likely to be affected than language arts scores by pandemic changes.
- • School meals, access to friends, and organized activities have also been lost with the closing of in-person school.
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic class. At this time, we have few data on outcomes, but many oversight organizations have tried to establish guidelines, expressed concerns, and extrapolated from previous experiences.
General educational losses and disparities
Many researchers are examining how the new environment affects learners’ mental, physical, and social health to help compensate for any losses incurred by this pandemic and to better prepare for future pandemics. There is a paucity of data at this juncture, but some investigators have extrapolated from earlier school shutdowns owing to hurricanes and other natural disasters. 1
Inclement weather closures are estimated in some studies to lower middle school math grades by 0.013 to 0.039 standard deviations and natural disaster closures by up to 0.10 standard deviation decreases in overall achievement scores. 2 The data from inclement weather closures did show a more significant decrease for children dependent on school meals, but generally the data were not stratified by socioeconomic differences. 3 , 4 Math scores are impacted overall more negatively by school absences than English language scores for all school closures. 4 , 5
The Northwest Evaluation Association is a global nonprofit organization that provides research-based assessments and professional development for educators. A team of researchers at Stanford University evaluated Northwest Evaluation Association test scores for students in 17 states and the District of Columbia in the Fall of 2020 and estimated that the average student had lost one-third of a year to a full year's worth of learning in reading, and about three-quarters of a year to more than 1 year in math since schools closed in March 2020. 5
With school shifted from traditional attendance at a school building to attendance via the Internet, families have come under new stressors. It is increasingly clear that families depended on schools for much more than math and reading. Shelter, food, health care, and social well-being are all part of what children and adolescents, as well as their parents or guardians, depend on schools to provide. 5 , 6
Many families have been impacted negatively by the loss of wages, leading to food insecurity and housing insecurity; some of loss this is a consequence of the need for parents to be at home with young children who cannot attend in-person school. 6 There is evidence that this economic instability is leading to an increase in depression and anxiety. 7 In 1 survey, 34.71% of parents reported behavioral problems in their children that they attributed to the pandemic and virtual schooling. 8
Children have been infected with and affected by coronavirus. In the United States, 93,605 students tested positive for COVID-19, and it was reported that 42% were Hispanic/Latino, 32% were non-Hispanic White, and 17% were non-Hispanic Black, emphasizing a disproportionate effect for children of color. 9 COVID infection itself is not the only issue that affects children’s health during the pandemic. School-based health care and school-based meals are lost when school goes virtual and children of lower socioeconomic class are more severely affected by these losses. Although some districts were able to deliver school meals, school-based health care is a primary source of health care for many children and has left some chronic conditions unchecked during the pandemic. 10
Many families report that the stress of the pandemic has led to a poorer diet in children with an increase in the consumption of sweet and fried foods. 11 , 12 Shelter at home orders and online education have led to fewer exercise opportunities. Research carried out by Ammar and colleagues 12 found that daily sitting had increased from 5 to 8 hours a day and binge eating, snacking, and the number of meals were all significantly increased owing to lockdown conditions and stay-at-home initiatives. There is growing evidence in both animal and human models that diets high in sugar and fat can play a detrimental role in cognition and should be of increased concern in light of the pandemic. 13
The family stress elicited by the COVID-19 shutdown is a particular concern because of compiled evidence that adverse life experiences at an early age are associated with an increased likelihood of mental health issues as an adult. 14 There is early evidence that children ages 6 to 18 years of age experienced a significant increase in their expression of “clinginess, irritability, and fear” during the early pandemic school shutdowns. 15 These emotions associated with anxiety may have a negative impact on the family unit, which was already stressed owing to the pandemic.
Another major concern is the length of isolation many children have had to endure since the pandemic began and what effects it might have on their ability to socialize. The school, for many children, is the agent for forming their social connections as well as where early social development occurs. 16 Noting that academic performance is also declining the pandemic may be creating a snowball effect, setting back children without access to resources from which they may never recover, even into adulthood.
Predictions from data analysis of school absenteeism, summer breaks, and natural disaster occurrences are imperfect for the current situation, but all indications are that we should not expect all children and adolescents to be affected equally. 4 , 5 Although some children and adolescents will likely suffer no long-term consequences, COVID-19 is expected to widen the already existing educational gap from socioeconomic differences, and children with learning differences are expected to suffer more losses than neurotypical children. 4 , 5
Special education and the COVID-19 pandemic
Although COVID-19 has affected all levels of education reception and delivery, children with special needs have been more profoundly impacted. Children in the United States who have special needs have legal protection for appropriate education by the Individuals with Disabilities Education Act and Section 504 of the Rehabilitation Act of 1973. 17 , 18 Collectively, this legislation is meant to allow for appropriate accommodations, services, modifications, and specialized academic instruction to ensure that “every child receives a free appropriate public education . . . in the least restrictive environment.” 17
Children with autism usually have applied behavioral analysis (ABA) as part of their individualized educational plan. ABA therapists for autism use a technique of discrete trial training that shapes and rewards incremental changes toward new behaviors. 19 Discrete trial training involves breaking behaviors into small steps and repetition of rewards for small advances in the steps toward those behaviors. It is an intensive one-on-one therapy that puts a child and therapist in close contact for many hours at a time, often 20 to 40 hours a week. This therapy works best when initiated at a young age in children with autism and is often initiated in the home. 19
Because ABA workers were considered essential workers from the early days of the pandemic, organizations providing this service had the responsibility and the freedom to develop safety protocols for delivery of this necessary service and did so in conjunction with certifying boards. 20
Early in the pandemic, there were interruptions in ABA followed by virtual visits, and finally by in-home therapy with COVID-19 isolation precautions. 21 Although the efficacy of virtual visits for ABA therapy would empirically seem to be inferior, there are few outcomes data available. The balance of safety versus efficacy quite early turned to in-home services with interruptions owing to illness and decreased therapist availability owing to the pandemic. 21 An overarching concern for children with autism is the possible loss of a window of opportunity to intervene early. Families of children and adolescents with autism spectrum disorder report increased stress compared with families of children with other disabilities before the pandemic, and during the pandemic this burden has increased with the added responsibility of monitoring in-home schooling. 20
Early data on virtual schooling children with attention deficit disorder (ADD) and attention deficit with hyperactivity (ADHD) shows that adolescents with ADD/ADHD found the switch to virtual learning more anxiety producing and more challenging than their peers. 22 However, according to a study in Ireland, younger children with ADD/ADHD and no other neurologic or psychiatric diagnoses who were stable on medication tended to report less anxiety with at-home schooling and their parents and caregivers reported improved behavior during the pandemic. 23 An unexpected benefit of shelter in home versus shelter in place may be to identify these stressors in face-to-face school for children with ADD/ADHD. If children with ADD/ADHD had an additional diagnosis of autism or depression, they reported increased anxiety with the school shutdown. 23 , 24
Much of the available literature is anticipatory guidance for in-home schooling of children with disabilities rather than data about schooling during the pandemic. The American Academy of Pediatrics published guidance advising that, because 70% of students with ADHD have other conditions, such as learning differences, oppositional defiant disorder, or depression, they may have very different responses to in home schooling which are a result of the non-ADHD diagnosis, for example, refusal to attempt work for children with oppositional defiant disorder, severe anxiety for those with depression and or anxiety disorders, and anxiety and perseveration for children with autism. 25 Children and families already stressed with learning differences have had substantial challenges during the COVID-19 school closures.
High school, depression, and COVID-19
High schoolers have lost a great deal during this pandemic. What should have been a time of establishing more independence has been hampered by shelter-in-place recommendations. Graduations, proms, athletic events, college visits, and many other social and educational events have been altered or lost and cannot be recaptured.
Adolescents reported higher rates of depression and anxiety associated with the pandemic, and in 1 study 14.4% of teenagers report post-traumatic stress disorder, whereas 40.4% report having depression and anxiety. 26 In another survey adolescent boys reported a significant decrease in life satisfaction from 92% before COVID to 72% during lockdown conditions. For adolescent girls, the decrease in life satisfaction was from 81% before COVID to 62% during the pandemic, with the oldest teenage girls reporting the lowest life satisfaction values during COVID-19 restrictions. 27 During the school shutdown for COVID-19, 21% of boys and 27% of girls reported an increase in family arguments. 26 Combine all of these reports with decreasing access to mental health services owing to pandemic restrictions and it becomes a complicated matter for parents to address their children's mental health needs as well as their educational needs. 28
A study conducted in Norway measured aspects of socialization and mood changes in adolescents during the pandemic. The opportunity for prosocial action was rated on a scale of 1 (not at all) to 6 (very much) based on how well certain phrases applied to them, for example, “I comforted a friend yesterday,” “Yesterday I did my best to care for a friend,” and “Yesterday I sent a message to a friend.” They also ranked mood by rating items on a scale of 1 (not at all) to 5 (very well) as items reflected their mood. 29 They found that adolescents showed an overall decrease in empathic concern and opportunity for prosocial actions, as well as a decrease in mood ratings during the pandemic. 29
A survey of 24,155 residents of Michigan projected an escalation of suicide risk for lesbian, gay, bisexual, transgender youth as well as those youth questioning their sexual orientation (LGBTQ) associated with increased social isolation. There was also a 66% increase in domestic violence for LGBTQ youth during shelter in place. 30 LGBTQ youth are yet another example of those already at increased risk having disproportionate effects of the pandemic.
Increased social media use during COVID-19, along with traditional forms of education moving to digital platforms, has led to the majority of adolescents spending significantly more time in front of screens. Excessive screen time is well-known to be associated with poor sleep, sedentary habits, mental health problems, and physical health issues. 31 With decreased access to physical activity, especially in crowded inner-city areas, and increased dependence on screen time for schooling, it is more difficult to craft easy solutions to the screen time issue.
During these times, it is more important than ever for pediatricians to check in on the mental health of patients with queries about how school is going, how patients are keeping contact with peers, and how are they processing social issues related to violence. Queries to families about the need for assistance with food insecurity, housing insecurity, and access to mental health services are necessary during this time of public emergency.
Medical school and COVID-19
Although medical school is an adult schooling experience, it affects not only the medical profession and our junior colleagues, but, by extrapolation, all education that requires hands-on experience or interning, and has been included for those reasons.
In the new COVID-19 era, medical schools have been forced to make drastic and quick changes to multiple levels of their curriculum to ensure both student and patient safety during the pandemic. Students entering their clinical rotations have had the most drastic alteration to their experience.
COVID-19 has led to some of the same changes high schools and colleges have adopted, specifically, replacement of large in-person lectures with small group activities small group discussion and virtual lectures. 32 The transition to an online format for medical education has been rapid and impacted both students and faculty. 33 , 34 In a survey by Singh and colleagues, 33 of the 192 students reporting 43.9% found online lectures to be poorer than physical classrooms during the pandemic. In another report by Shahrvini and colleagues, 35 of 104 students surveyed, 74.5% students felt disconnected from their medical school and their peers and 43.3% felt that they were unprepared for their clerkships. Although there are no pre-COVID-19 data for comparison, it is expected that the COVID-19 changes will lead to increased insecurity and feelings of poor preparation for clinical work.
Gross anatomy is a well-established tradition within the medical school curriculum and one that is conducted almost entirely in person and in close quarters around a cadaver. Harmon and colleagues 36 surveyed 67 gross anatomy educators and found that 8% were still holding in-person sessions and 34 ± 43% transitioned to using cadaver images and dissecting videos that could be accessed through the Internet.
Many third- and fourth-year medical students have seen periods of cancellation for clinical rotations and supplementation with online learning, telemedicine, or virtual rounds owing to the COVID-19 pandemic. 37 A study from Shahrvini and colleagues 38 found that an unofficial document from Reddit (a widely used social network platform with a subgroup for medical students and residents) reported that 75% of medical schools had canceled clinical activities for third- and fourth-year students for some part of 2020. In another survey by Harries and colleagues, 39 of the 741 students who responded, 93.7% were not involved in clinical rotations with in-person patient contact. The reactions of students varied, with 75.8% admitting to agreeing with the decision, 34.7% feeling guilty, and 27.0% feeling relieved. 39 In the same survey, 74.7% of students felt that their medical education had been disrupted, 84.1% said they felt increased anxiety, and 83.4% would accept the risk of COVID-19 infection if they were able to return to the clinical setting. 39
Since the start of the pandemic, medical schools have had to find new and innovative ways to continue teaching and exposing students to clinical settings. The use of electronic conferencing services has been critical to continuing education. One approach has been to turn to online applications like Google Hangouts, which come at no cost and offer a wide variety of tools to form an integrative learning environment. 32 , 37 , 40 Schools have also adopted a hybrid model of teaching where lectures can be prerecorded then viewed by the student asynchronously on their own time followed by live virtual lectures where faculty can offer question-and-answer sessions related to the material. By offering this new format, students have been given more flexibility in terms of creating a schedule that suits their needs and may decrease stress. 37
Although these changes can be a hurdle to students and faculty, it might prove to be beneficial for the future of medical training in some ways. Telemedicine is a growing field, and the American Medical Association and other programs have endorsed its value. 41 Telemedicine visits can still be used to take a history, conduct a basic visual physical examination, and build rapport, as well as performing other aspects of the clinical examination during a pandemic, and will continue to be useful for patients unable to attend regular visits at remote locations. Learning effectively now how to communicate professionally and carry out telemedicine visits may better prepare students for a future where telemedicine is an expectation and allow students to learn the limitations as well as the advantages of this modality. 41
Pandemic changes have strongly impacted the process of college applications, medical school applications, and residency applications. 32 For US medical residencies, 72% of applicants will, if the pattern from 2016 to 2019 continues, move between states or countries. 42 This level of movement is increasingly dangerous given the spread of COVID-19 and the lack of currently accepted procedures to carry out such a mass migration safely. The same follows for medical schools and universities.
We need to accept and prepare for the fact that medial students as well as other learners who require in-person training may lack some skills when they enter their profession. These skills will have to be acquired during a later phase of training. We may have less skilled entry-level resident physicians and nurses in our hospitals and in other clinical professions as well.
The COVID-19 pandemic has affected and will continue to affect the delivery of knowledge and skills at all levels of education. Although many children and adult learners will likely compensate for this interruption of traditional educational services and adapt to new modalities, some will struggle. The widening of the gap for those whose families cannot absorb the teaching and supervision of education required for in-home education because they lack the time and skills necessary are not addressed currently. The gap for those already at a disadvantage because of socioeconomic class, language, and special needs are most severely affected by the COVID-19 pandemic school closures and will have the hardest time compensating. As pediatricians, it is critical that we continue to check in with our young patients about how they are coping and what assistance we can guide them toward in our communities.
Clinics care points
- • Learners and educators at all levels of education have been affected by COVID-19 restrictions with rapid adaptations to virtual learning platforms.
- • The impact of COVID-19 on learners is not evenly distributed and children of racial minorities, those who live in poverty, those requiring special education, and children who speak English as a second language are more negatively affected by the need for remote learning.
- • Math scores are more impacted than language arts scores by previous school closures and thus far by these shutdowns for COVID-19.
- • Anxiety and depression have increased in children and particularly in adolescents as a result of COVID-19 itself and as a consequence of school changes.
- • Pediatricians should regularly screen for unmet needs in their patients during the pandemic, such as food insecurity with the loss of school meals, an inability to adapt to remote learning and increased computer time, and heightened anxiety and depression as results of school changes.
The authors have nothing to disclose.
We need your support today
Independent journalism is more important than ever. Vox is here to explain this unprecedented election cycle and help you understand the larger stakes. We will break down where the candidates stand on major issues, from economic policy to immigration, foreign policy, criminal justice, and abortion. We’ll answer your biggest questions, and we’ll explain what matters — and why. This timely and essential task, however, is expensive to produce.
We rely on readers like you to fund our journalism. Will you support our work and become a Vox Member today?
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
- Recommendations
Most Popular
- America isn’t ready for another war — because it doesn’t have the troops
- Take a mental break with the newest Vox crossword
- Your guide to the Brittany Mahomes-Donald Trump drama, such as it is
- The Trump Arlington National Cemetery controversy, explained
- Democrats’ vibes are excellent. Can they turn that into votes?
Today, Explained
Understand the world with a daily explainer plus the most compelling stories of the day.
This is the title for the native ad
More in Culture

The back-and-forth over a wildly rare appeal is a win for victim’s rights.

Why everyone suddenly cares about Brittany Mahomes’s politics.

The second season of the series has huge news for fans of Tom Bombadil.

A newsletter about kids, for everyone.

How the once-maligned retailer quietly became a closet staple — and a stock market giant — once again.

My generation was taught to change the system. That lesson came at a cost.
The pandemic has had devastating impacts on learning. What will it take to help students catch up?
Subscribe to the brown center on education policy newsletter, megan kuhfeld , megan kuhfeld senior research scientist - nwea jim soland , jim soland assistant professor, school of education and human development - university of virginia, affiliated research fellow - nwea karyn lewis , and karyn lewis director, center for school and student progress - nwea emily morton emily morton research scientist - nwea.
March 3, 2022
As we reach the two-year mark of the initial wave of pandemic-induced school shutdowns, academic normalcy remains out of reach for many students, educators, and parents. In addition to surging COVID-19 cases at the end of 2021, schools have faced severe staff shortages , high rates of absenteeism and quarantines , and rolling school closures . Furthermore, students and educators continue to struggle with mental health challenges , higher rates of violence and misbehavior , and concerns about lost instructional time .
As we outline in our new research study released in January, the cumulative impact of the COVID-19 pandemic on students’ academic achievement has been large. We tracked changes in math and reading test scores across the first two years of the pandemic using data from 5.4 million U.S. students in grades 3-8. We focused on test scores from immediately before the pandemic (fall 2019), following the initial onset (fall 2020), and more than one year into pandemic disruptions (fall 2021).
Average fall 2021 math test scores in grades 3-8 were 0.20-0.27 standard deviations (SDs) lower relative to same-grade peers in fall 2019, while reading test scores were 0.09-0.18 SDs lower. This is a sizable drop. For context, the math drops are significantly larger than estimated impacts from other large-scale school disruptions, such as after Hurricane Katrina—math scores dropped 0.17 SDs in one year for New Orleans evacuees .
Even more concerning, test-score gaps between students in low-poverty and high-poverty elementary schools grew by approximately 20% in math (corresponding to 0.20 SDs) and 15% in reading (0.13 SDs), primarily during the 2020-21 school year. Further, achievement tended to drop more between fall 2020 and 2021 than between fall 2019 and 2020 (both overall and differentially by school poverty), indicating that disruptions to learning have continued to negatively impact students well past the initial hits following the spring 2020 school closures.
These numbers are alarming and potentially demoralizing, especially given the heroic efforts of students to learn and educators to teach in incredibly trying times. From our perspective, these test-score drops in no way indicate that these students represent a “ lost generation ” or that we should give up hope. Most of us have never lived through a pandemic, and there is so much we don’t know about students’ capacity for resiliency in these circumstances and what a timeline for recovery will look like. Nor are we suggesting that teachers are somehow at fault given the achievement drops that occurred between 2020 and 2021; rather, educators had difficult jobs before the pandemic, and now are contending with huge new challenges, many outside their control.
Clearly, however, there’s work to do. School districts and states are currently making important decisions about which interventions and strategies to implement to mitigate the learning declines during the last two years. Elementary and Secondary School Emergency Relief (ESSER) investments from the American Rescue Plan provided nearly $200 billion to public schools to spend on COVID-19-related needs. Of that sum, $22 billion is dedicated specifically to addressing learning loss using “evidence-based interventions” focused on the “ disproportionate impact of COVID-19 on underrepresented student subgroups. ” Reviews of district and state spending plans (see Future Ed , EduRecoveryHub , and RAND’s American School District Panel for more details) indicate that districts are spending their ESSER dollars designated for academic recovery on a wide variety of strategies, with summer learning, tutoring, after-school programs, and extended school-day and school-year initiatives rising to the top.
Comparing the negative impacts from learning disruptions to the positive impacts from interventions
To help contextualize the magnitude of the impacts of COVID-19, we situate test-score drops during the pandemic relative to the test-score gains associated with common interventions being employed by districts as part of pandemic recovery efforts. If we assume that such interventions will continue to be as successful in a COVID-19 school environment, can we expect that these strategies will be effective enough to help students catch up? To answer this question, we draw from recent reviews of research on high-dosage tutoring , summer learning programs , reductions in class size , and extending the school day (specifically for literacy instruction) . We report effect sizes for each intervention specific to a grade span and subject wherever possible (e.g., tutoring has been found to have larger effects in elementary math than in reading).
Figure 1 shows the standardized drops in math test scores between students testing in fall 2019 and fall 2021 (separately by elementary and middle school grades) relative to the average effect size of various educational interventions. The average effect size for math tutoring matches or exceeds the average COVID-19 score drop in math. Research on tutoring indicates that it often works best in younger grades, and when provided by a teacher rather than, say, a parent. Further, some of the tutoring programs that produce the biggest effects can be quite intensive (and likely expensive), including having full-time tutors supporting all students (not just those needing remediation) in one-on-one settings during the school day. Meanwhile, the average effect of reducing class size is negative but not significant, with high variability in the impact across different studies. Summer programs in math have been found to be effective (average effect size of .10 SDs), though these programs in isolation likely would not eliminate the COVID-19 test-score drops.
Figure 1: Math COVID-19 test-score drops compared to the effect sizes of various educational interventions

Source: COVID-19 score drops are pulled from Kuhfeld et al. (2022) Table 5; reduction-in-class-size results are from pg. 10 of Figles et al. (2018) Table 2; summer program results are pulled from Lynch et al (2021) Table 2; and tutoring estimates are pulled from Nictow et al (2020) Table 3B. Ninety-five percent confidence intervals are shown with vertical lines on each bar.
Notes: Kuhfeld et al. and Nictow et al. reported effect sizes separately by grade span; Figles et al. and Lynch et al. report an overall effect size across elementary and middle grades. We were unable to find a rigorous study that reported effect sizes for extending the school day/year on math performance. Nictow et al. and Kraft & Falken (2021) also note large variations in tutoring effects depending on the type of tutor, with larger effects for teacher and paraprofessional tutoring programs than for nonprofessional and parent tutoring. Class-size reductions included in the Figles meta-analysis ranged from a minimum of one to minimum of eight students per class.
Figure 2 displays a similar comparison using effect sizes from reading interventions. The average effect of tutoring programs on reading achievement is larger than the effects found for the other interventions, though summer reading programs and class size reduction both produced average effect sizes in the ballpark of the COVID-19 reading score drops.
Figure 2: Reading COVID-19 test-score drops compared to the effect sizes of various educational interventions

Source: COVID-19 score drops are pulled from Kuhfeld et al. (2022) Table 5; extended-school-day results are from Figlio et al. (2018) Table 2; reduction-in-class-size results are from pg. 10 of Figles et al. (2018) ; summer program results are pulled from Kim & Quinn (2013) Table 3; and tutoring estimates are pulled from Nictow et al (2020) Table 3B. Ninety-five percent confidence intervals are shown with vertical lines on each bar.
Notes: While Kuhfeld et al. and Nictow et al. reported effect sizes separately by grade span, Figlio et al. and Kim & Quinn report an overall effect size across elementary and middle grades. Class-size reductions included in the Figles meta-analysis ranged from a minimum of one to minimum of eight students per class.
There are some limitations of drawing on research conducted prior to the pandemic to understand our ability to address the COVID-19 test-score drops. First, these studies were conducted under conditions that are very different from what schools currently face, and it is an open question whether the effectiveness of these interventions during the pandemic will be as consistent as they were before the pandemic. Second, we have little evidence and guidance about the efficacy of these interventions at the unprecedented scale that they are now being considered. For example, many school districts are expanding summer learning programs, but school districts have struggled to find staff interested in teaching summer school to meet the increased demand. Finally, given the widening test-score gaps between low- and high-poverty schools, it’s uncertain whether these interventions can actually combat the range of new challenges educators are facing in order to narrow these gaps. That is, students could catch up overall, yet the pandemic might still have lasting, negative effects on educational equality in this country.
Given that the current initiatives are unlikely to be implemented consistently across (and sometimes within) districts, timely feedback on the effects of initiatives and any needed adjustments will be crucial to districts’ success. The Road to COVID Recovery project and the National Student Support Accelerator are two such large-scale evaluation studies that aim to produce this type of evidence while providing resources for districts to track and evaluate their own programming. Additionally, a growing number of resources have been produced with recommendations on how to best implement recovery programs, including scaling up tutoring , summer learning programs , and expanded learning time .
Ultimately, there is much work to be done, and the challenges for students, educators, and parents are considerable. But this may be a moment when decades of educational reform, intervention, and research pay off. Relying on what we have learned could show the way forward.
Related Content
Megan Kuhfeld, Jim Soland, Beth Tarasawa, Angela Johnson, Erik Ruzek, Karyn Lewis
December 3, 2020
Lindsay Dworkin, Karyn Lewis
October 13, 2021
Early Childhood Education Education Access & Equity Education Policy K-12 Education
Governance Studies
U.S. States and Territories
Brown Center on Education Policy
Lydia Wilbard
August 29, 2024
Zachary Billot, Annie Vong, Nicole Dias Del Valle, Emily Markovich Morris
August 26, 2024
Brian A. Jacob, Cristina Stanojevich
Writing about COVID-19 in a college admission essay
by: Venkates Swaminathan | Updated: September 14, 2020
Print article

For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic’s impact. The different sections have differing goals. You must understand how to use each section for its appropriate use.
The CommonApp COVID-19 question
First, the CommonApp this year has an additional question specifically about COVID-19 :
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces. Please use this space to describe how these events have impacted you.
This question seeks to understand the adversity that students may have had to face due to the pandemic, the move to online education, or the shelter-in-place rules. You don’t have to answer this question if the impact on you wasn’t particularly severe. Some examples of things students should discuss include:
- The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic.
- The candidate had to deal with personal or family issues, such as abusive living situations or other safety concerns
- The student suffered from a lack of internet access and other online learning challenges.
- Students who dealt with problems registering for or taking standardized tests and AP exams.
Jeff Schiffman of the Tulane University admissions office has a blog about this section. He recommends students ask themselves several questions as they go about answering this section:
- Are my experiences different from others’?
- Are there noticeable changes on my transcript?
- Am I aware of my privilege?
- Am I specific? Am I explaining rather than complaining?
- Is this information being included elsewhere on my application?
If you do answer this section, be brief and to-the-point.
Counselor recommendations and school profiles
Second, counselors will, in their counselor forms and school profiles on the CommonApp, address how the school handled the pandemic and how it might have affected students, specifically as it relates to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
Students don’t have to mention these matters in their application unless something unusual happened.
Writing about COVID-19 in your main essay
Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. That you had to stay home and study online isn’t sufficient, as millions of other students faced the same situation. But sometimes, it can be appropriate and helpful to write about something related to the pandemic in your essay. For example:
- One student developed a website for a local comic book store. The store might not have survived without the ability for people to order comic books online. The student had a long-standing relationship with the store, and it was an institution that created a community for students who otherwise felt left out.
- One student started a YouTube channel to help other students with academic subjects he was very familiar with and began tutoring others.
- Some students used their extra time that was the result of the stay-at-home orders to take online courses pursuing topics they are genuinely interested in or developing new interests, like a foreign language or music.
Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely important about the student. For many students whose lives have been shaped by this pandemic, it can be a critical part of their college application.
Want more? Read 6 ways to improve a college essay , What the &%$! should I write about in my college essay , and Just how important is a college admissions essay? .

Homes Nearby
Homes for rent and sale near schools

How our schools are (and aren't) addressing race

The truth about homework in America

What should I write my college essay about?
What the #%@!& should I write about in my college essay?
Yes! Sign me up for updates relevant to my child's grade.
Please enter a valid email address
Thank you for signing up!
Server Issue: Please try again later. Sorry for the inconvenience
I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads from TIME
- Breaking Down the 2024 Election Calendar
- How Nayib Bukele’s ‘Iron Fist’ Has Transformed El Salvador
- What if Ultra-Processed Foods Aren’t as Bad as You Think?
- How Ukraine Beat Russia in the Battle of the Black Sea
- Long COVID Looks Different in Kids
- How Project 2025 Would Jeopardize Americans’ Health
- What a $129 Frying Pan Says About America’s Eating Habits
- The 32 Most Anticipated Books of Fall 2024
Contact us at [email protected]
- Patient Care & Health Information
- Diseases & Conditions
- Coronavirus disease 2019 (COVID-19)
COVID-19, also called coronavirus disease 2019, is an illness caused by a virus. The virus is called severe acute respiratory syndrome coronavirus 2, or more commonly, SARS-CoV-2. It started spreading at the end of 2019 and became a pandemic disease in 2020.
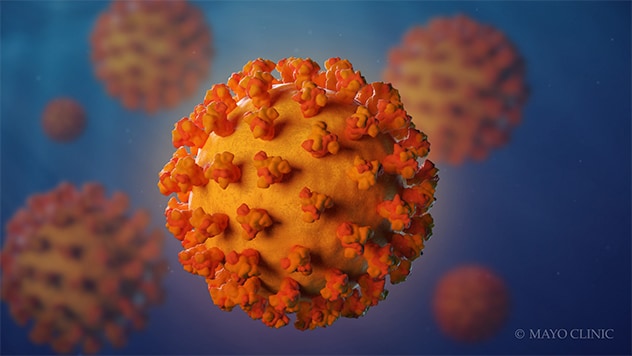
- Coronavirus
Coronaviruses are a family of viruses. These viruses cause illnesses such as the common cold, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads most commonly through the air in tiny droplets of fluid between people in close contact. Many people with COVID-19 have no symptoms or mild illness. But for older adults and people with certain medical conditions, COVID-19 can lead to the need for care in the hospital or death.
Staying up to date on your COVID-19 vaccine helps prevent serious illness, the need for hospital care due to COVID-19 and death from COVID-19 . Other ways that may help prevent the spread of this coronavirus includes good indoor air flow, physical distancing, wearing a mask in the right setting and good hygiene.
Medicine can limit the seriousness of the viral infection. Most people recover without long-term effects, but some people have symptoms that continue for months.
Typical COVID-19 symptoms often show up 2 to 14 days after contact with the virus.
Symptoms can include:
- Shortness of breath.
- Loss of taste or smell.
- Extreme tiredness, called fatigue.
- Digestive symptoms such as upset stomach, vomiting or loose stools, called diarrhea.
- Pain, such as headaches and body or muscle aches.
- Fever or chills.
- Cold-like symptoms such as congestion, runny nose or sore throat.
People may only have a few symptoms or none. People who have no symptoms but test positive for COVID-19 are called asymptomatic. For example, many children who test positive don't have symptoms of COVID-19 illness. People who go on to have symptoms are considered presymptomatic. Both groups can still spread COVID-19 to others.
Some people may have symptoms that get worse about 7 to 14 days after symptoms start.
Most people with COVID-19 have mild to moderate symptoms. But COVID-19 can cause serious medical complications and lead to death. Older adults or people who already have medical conditions are at greater risk of serious illness.
COVID-19 may be a mild, moderate, severe or critical illness.
- In broad terms, mild COVID-19 doesn't affect the ability of the lungs to get oxygen to the body.
- In moderate COVID-19 illness, the lungs also work properly but there are signs that the infection is deep in the lungs.
- Severe COVID-19 means that the lungs don't work correctly, and the person needs oxygen and other medical help in the hospital.
- Critical COVID-19 illness means the lung and breathing system, called the respiratory system, has failed and there is damage throughout the body.
Rarely, people who catch the coronavirus can develop a group of symptoms linked to inflamed organs or tissues. The illness is called multisystem inflammatory syndrome. When children have this illness, it is called multisystem inflammatory syndrome in children, shortened to MIS -C. In adults, the name is MIS -A.
When to see a doctor
Contact a healthcare professional if you test positive for COVID-19 . If you have symptoms and need to test for COVID-19 , or you've been exposed to someone with COVID-19 , a healthcare professional can help.
People who are at high risk of serious illness may get medicine to block the spread of the COVID-19 virus in the body. Or your healthcare team may plan regular checks to monitor your health.
Get emergency help right away for any of these symptoms:
- Can't catch your breath or have problems breathing.
- Skin, lips or nail beds that are pale, gray or blue.
- New confusion.
- Trouble staying awake or waking up.
- Chest pain or pressure that is constant.
This list doesn't include every emergency symptom. If you or a person you're taking care of has symptoms that worry you, get help. Let the healthcare team know about a positive test for COVID-19 or symptoms of the illness.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.

Sorry something went wrong with your subscription
Please, try again in a couple of minutes
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2, also called SARS-CoV-2.
The coronavirus spreads mainly from person to person, even from someone who is infected but has no symptoms. When people with COVID-19 cough, sneeze, breathe, sing or talk, their breath may be infected with the COVID-19 virus.
The coronavirus carried by a person's breath can land directly on the face of a nearby person, after a sneeze or cough, for example. The droplets or particles the infected person breathes out could possibly be breathed in by other people if they are close together or in areas with low air flow. And a person may touch a surface that has respiratory droplets and then touch their face with hands that have the coronavirus on them.
It's possible to get COVID-19 more than once.
- Over time, the body's defense against the COVID-19 virus can fade.
- A person may be exposed to so much of the virus that it breaks through their immune defense.
- As a virus infects a group of people, the virus copies itself. During this process, the genetic code can randomly change in each copy. The changes are called mutations. If the coronavirus that causes COVID-19 changes in ways that make previous infections or vaccination less effective at preventing infection, people can get sick again.
The virus that causes COVID-19 can infect some pets. Cats, dogs, hamsters and ferrets have caught this coronavirus and had symptoms. It's rare for a person to get COVID-19 from a pet.
Risk factors
The main risk factors for COVID-19 are:
- If someone you live with has COVID-19 .
- If you spend time in places with poor air flow and a higher number of people when the virus is spreading.
- If you spend more than 30 minutes in close contact with someone who has COVID-19 .
Many factors affect your risk of catching the virus that causes COVID-19 . How long you are in contact, if the space has good air flow and your activities all affect the risk. Also, if you or others wear masks, if someone has COVID-19 symptoms and how close you are affects your risk. Close contact includes sitting and talking next to one another, for example, or sharing a car or bedroom.
It seems to be rare for people to catch the virus that causes COVID-19 from an infected surface. While the virus is shed in waste, called stool, COVID-19 infection from places such as a public bathroom is not common.
Serious COVID-19 illness risk factors
Some people are at a higher risk of serious COVID-19 illness than others. This includes people age 65 and older as well as babies younger than 6 months. Those age groups have the highest risk of needing hospital care for COVID-19 .
Not every risk factor for serious COVID-19 illness is known. People of all ages who have no other medical issues have needed hospital care for COVID-19 .
Known risk factors for serious illness include people who have not gotten a COVID-19 vaccine. Serious illness also is a higher risk for people who have:
- Sickle cell disease or thalassemia.
- Serious heart diseases and possibly high blood pressure.
- Chronic kidney, liver or lung diseases.
People with dementia or Alzheimer's also are at higher risk, as are people with brain and nervous system conditions such as stroke. Smoking increases the risk of serious COVID-19 illness. And people with a body mass index in the overweight category or obese category may have a higher risk as well.
Other medical conditions that may raise the risk of serious illness from COVID-19 include:
- Cancer or a history of cancer.
- Type 1 or type 2 diabetes.
- Weakened immune system from solid organ transplants or bone marrow transplants, some medicines, or HIV .
This list is not complete. Factors linked to a health issue may raise the risk of serious COVID-19 illness too. Examples are a medical condition where people live in a group home, or lack of access to medical care. Also, people with more than one health issue, or people of older age who also have health issues have a higher chance of severe illness.
Related information
- COVID-19: Who's at higher risk of serious symptoms? - Related information COVID-19: Who's at higher risk of serious symptoms?
Complications
Complications of COVID-19 include long-term loss of taste and smell, skin rashes, and sores. The illness can cause trouble breathing or pneumonia. Medical issues a person already manages may get worse.
Complications of severe COVID-19 illness can include:
- Acute respiratory distress syndrome, when the body's organs do not get enough oxygen.
- Shock caused by the infection or heart problems.
- Overreaction of the immune system, called the inflammatory response.
- Blood clots.
- Kidney injury.
Post-COVID-19 syndrome
After a COVID-19 infection, some people report that symptoms continue for months, or they develop new symptoms. This syndrome has often been called long COVID, or post- COVID-19 . You might hear it called long haul COVID-19 , post-COVID conditions or PASC. That's short for post-acute sequelae of SARS -CoV-2.
Other infections, such as the flu and polio, can lead to long-term illness. But the virus that causes COVID-19 has only been studied since it began to spread in 2019. So, research into the specific effects of long-term COVID-19 symptoms continues.
Researchers do think that post- COVID-19 syndrome can happen after an illness of any severity.
Getting a COVID-19 vaccine may help prevent post- COVID-19 syndrome.
The Centers for Disease Control and Prevention (CDC) recommends a COVID-19 vaccine for everyone age 6 months and older. The COVID-19 vaccine can lower the risk of death or serious illness caused by COVID-19.
The COVID-19 vaccines available in the United States are:
2023-2024 Pfizer-BioNTech COVID-19 vaccine. This vaccine is available for people age 6 months and older.
Among people with a typical immune system:
- Children age 6 months up to age 4 years are up to date after three doses of a Pfizer-BioNTech COVID-19 vaccine.
- People age 5 and older are up to date after one Pfizer-BioNTech COVID-19 vaccine.
- For people who have not had a 2023-2024 COVID-19 vaccination, the CDC recommends getting an additional shot of that updated vaccine.
2023-2024 Moderna COVID-19 vaccine. This vaccine is available for people age 6 months and older.
- Children ages 6 months up to age 4 are up to date if they've had two doses of a Moderna COVID-19 vaccine.
- People age 5 and older are up to date with one Moderna COVID-19 vaccine.
2023-2024 Novavax COVID-19 vaccine. This vaccine is available for people age 12 years and older.
- People age 12 years and older are up to date if they've had two doses of a Novavax COVID-19 vaccine.
In general, people age 5 and older with typical immune systems can get any vaccine approved or authorized for their age. They usually don't need to get the same vaccine each time.
Some people should get all their vaccine doses from the same vaccine maker, including:
- Children ages 6 months to 4 years.
- People age 5 years and older with weakened immune systems.
- People age 12 and older who have had one shot of the Novavax vaccine should get the second Novavax shot in the two-dose series.
Talk to your healthcare professional if you have any questions about the vaccines for you or your child. Your healthcare team can help you if:
- The vaccine you or your child got earlier isn't available.
- You don't know which vaccine you or your child received.
- You or your child started a vaccine series but couldn't finish it due to side effects.
People with weakened immune systems
Your healthcare team may suggest added doses of COVID-19 vaccine if you have a moderately or seriously weakened immune system. The FDA has also authorized the monoclonal antibody pemivibart (Pemgarda) to prevent COVID-19 in some people with weakened immune systems.
Control the spread of infection
In addition to vaccination, there are other ways to stop the spread of the virus that causes COVID-19 .
If you are at a higher risk of serious illness, talk to your healthcare professional about how best to protect yourself. Know what to do if you get sick so you can quickly start treatment.
If you feel ill or have COVID-19 , stay home and away from others, including pets, if possible. Avoid sharing household items such as dishes or towels if you're sick.
In general, make it a habit to:
- Test for COVID-19 . If you have symptoms of COVID-19 test for the infection. Or test five days after you came in contact with the virus.
- Help from afar. Avoid close contact with anyone who is sick or has symptoms, if possible.
- Wash your hands. Wash your hands well and often with soap and water for at least 20 seconds. Or use an alcohol-based hand sanitizer with at least 60% alcohol.
- Cover your coughs and sneezes. Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Clean and disinfect high-touch surfaces. For example, clean doorknobs, light switches, electronics and counters regularly.
Try to spread out in crowded public areas, especially in places with poor airflow. This is important if you have a higher risk of serious illness.
The CDC recommends that people wear a mask in indoor public spaces if you're in an area with a high number of people with COVID-19 in the hospital. They suggest wearing the most protective mask possible that you'll wear regularly, that fits well and is comfortable.
- COVID-19 vaccines: Get the facts - Related information COVID-19 vaccines: Get the facts
- Comparing the differences between COVID-19 vaccines - Related information Comparing the differences between COVID-19 vaccines
- Different types of COVID-19 vaccines: How they work - Related information Different types of COVID-19 vaccines: How they work
- Debunking COVID-19 myths - Related information Debunking COVID-19 myths
Travel and COVID-19
Travel brings people together from areas where illnesses may be at higher levels. Masks can help slow the spread of respiratory diseases in general, including COVID-19 . Masks help the most in places with low air flow and where you are in close contact with other people. Also, masks can help if the places you travel to or through have a high level of illness.
Masking is especially important if you or a companion have a high risk of serious illness from COVID-19 .
- Goldman L, et al., eds. COVID-19: Epidemiology, clinical manifestations, diagnosis, community prevention, and prognosis. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Dec. 17, 2023.
- Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/. Accessed Dec. 18, 2023.
- AskMayoExpert. COVID-19: Testing, symptoms. Mayo Clinic; Nov. 2, 2023.
- Symptoms of COVID-19. Centers for Disease Control and Preventions. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed Dec. 20, 2023.
- AskMayoExpert. COVID-19: Outpatient management. Mayo Clinic; Oct. 10, 2023.
- Morris SB, et al. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection — United Kingdom and United States, March-August 2020. MMWR. Morbidity and Mortality Weekly Report 2020;69:1450. DOI: http://dx.doi.org/10.15585/mmwr.mm6940e1external icon.
- COVID-19 testing: What you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html. Accessed Dec. 20, 2023.
- SARS-CoV-2 in animals. American Veterinary Medical Association. https://www.avma.org/resources-tools/one-health/covid-19/sars-cov-2-animals-including-pets. Accessed Jan. 17, 2024.
- Understanding exposure risk. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-exposure.html. Accessed Jan. 10, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Jan. 10, 2024.
- Factors that affect your risk of getting very sick from COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-getting-very-sick.html. Accessed Jan. 10, 2024.
- Regan JJ, et al. Use of Updated COVID-19 Vaccines 2023-2024 Formula for Persons Aged ≥6 Months: Recommendations of the Advisory Committee on Immunization Practices—United States, September 2023. MMWR. Morbidity and Mortality Weekly Report 2023; 72:1140–1146. DOI: http://dx.doi.org/10.15585/mmwr.mm7242e1.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed Jan. 10, 2024.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Jan. 10, 2024.
- Interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html#CoV-19-vaccination. Accessed Jan. 10, 2024.
- Use and care of masks. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed Jan. 10, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Jan. 10, 2024.
- People who are immunocompromised. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html. Accessed Jan. 10, 2024.
- Masking during travel. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/masks. Accessed Jan. 10, 2024.
- AskMayoExpert. COVID-19: Testing. Mayo Clinic. 2023.
- COVID-19 test basics. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/covid-19-test-basics. Accessed Jan. 11, 2024.
- At-home COVID-19 antigen tests — Take steps to reduce your risk of false negative results: FDA safety communication. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/safety-communications/home-covid-19-antigen-tests-take-steps-reduce-your-risk-false-negative-results-fda-safety. Accessed Jan. 11, 2024.
- Interim clinical considerations for COVID-19 treatment in outpatients. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/outpatient-treatment-overview.html. Accessed Jan. 11, 2024.
- Know your treatment options for COVID-19. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/know-your-treatment-options-covid-19. Accessed Jan. 11, 2024.
- AskMayoExpert. COVID:19 Drug regimens and other treatment options. Mayo Clinic. 2023.
- Preventing spread of respiratory viruses when you're sick. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick.html. Accessed March 5, 2024.
- AskMayoExpert. COVID-19: Quarantine and isolation. Mayo Clinic. 2023.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed Jan. 11, 2024.
- COVID-19 overview and infection prevention and control priorities in non-U.S. healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html. Accessed Jan. 16, 2024.
- Kim AY, et al. COVID-19: Management in hospitalized adults. https://www.uptodate.com/contents/search. Accessed Jan. 17, 2024.
- O'Horo JC, et al. Outcomes of COVID-19 with the Mayo Clinic Model of Care and Research. Mayo Clinic Proceedings. 2021; doi:10.1016/j.mayocp.2020.12.006.
- At-home OTC COVID-19 diagnostic tests. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/home-otc-covid-19-diagnostic-tests. Accessed Jan. 22, 2024.
- Emergency use authorizations for drugs and non-vaccine biological products. U.S. Food and Drug Association. https://www.fda.gov/drugs/emergency-preparedness-drugs/emergency-use-authorizations-drugs-and-non-vaccine-biological-products. Accessed March 25, 2024.
- Coronavirus infection by race
- COVID-19 and pets
- COVID-19 and vitamin D
- COVID-19 and your mental health
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- COVID-19 travel advice
- COVID-19 vaccines
- COVID-19 vaccines for kids: What you need to know
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19, cold, allergies and the flu
- COVID-19: How can I protect myself?
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Fight coronavirus (COVID-19) transmission at home
- Herd immunity and coronavirus
- How do COVID-19 antibody tests differ from diagnostic tests?
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Long-term effects of COVID-19
- Mayo Clinic Minute: How dirty are common surfaces?
- Mayo Clinic Minute: You're washing your hands all wrong
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
Associated Procedures
- Convalescent plasma therapy
- COVID-19 antibody testing
- COVID-19 tests
- Extracorporeal membrane oxygenation (ECMO)
News from Mayo Clinic
- A Mayo Clinic virologist explains FLiRT and why you may need a new COVID-19 vaccination May 30, 2024, 02:30 p.m. CDT
- Mayo Clinic Q and A: Who should get the latest COVID-19 vaccine? Nov. 21, 2023, 01:30 p.m. CDT
- Can you get COVID-19 and the flu at the same time? A Mayo Clinic expert weighs in Oct. 16, 2023, 04:30 p.m. CDT
- At-home COVID-19 tests: A Mayo Clinic expert answers questions on expiration dates and the new variants Sept. 18, 2023, 04:00 p.m. CDT
- Mayo Clinic expert answers questions about the new COVID-19 vaccine Sept. 13, 2023, 04:15 p.m. CDT
- Study identifies risk factors for long-haul COVID disease in adults Sept. 13, 2023, 02:00 p.m. CDT
- Mayo researchers find vaccine may reduce severity of long-haul COVID symptoms Aug. 23, 2023, 04:34 p.m. CDT
- Corticosteroids lower the likelihood of in-hospital mortality from COVID-19 Aug. 04, 2023, 03:00 p.m. CDT
- COVID-19 vaccine administration simplified April 21, 2023, 07:00 p.m. CDT
- Science Saturday: COVID-19 -- the pandemic that's forever changed laboratory testing April 15, 2023, 11:00 a.m. CDT
- Mayo Clinic expert talks about the new omicron variant April 13, 2023, 02:13 p.m. CDT
- Mayo Clinic to ease universal face mask requirement April 04, 2023, 03:05 p.m. CDT
- 'Deaths of Despair' contribute to 17% rise in Minnesota's death rate during COVID-19 pandemic March 13, 2023, 12:00 p.m. CDT
- Rising cases of COVID-19 variant, XBB.1.5 Jan. 09, 2023, 05:15 p.m. CDT
- Bivalent COVID-19 booster approved for children 6 months and older Dec. 09, 2022, 09:33 p.m. CDT
- Mayo Clinic Minute: How to self-care at home when you have COVID-19 Dec. 06, 2022, 05:00 p.m. CDT
- Halloween safety tips from a Mayo Clinic infectious diseases expert Oct. 27, 2022, 02:00 p.m. CDT
- COVID-19, RSV and flu--season of respiratory infections Oct. 26, 2022, 04:30 p.m. CDT
- COVID-19 bivalent booster vaccines for kids 5-11 approved, Mayo Clinic awaits supply Oct. 13, 2022, 04:54 p.m. CDT
- Questions answered about the COVID-19 bivalent booster vaccines Oct. 12, 2022, 03:30 p.m. CDT
- Will the COVID-19 booster be like an annual flu shot? Sept. 12, 2022, 04:30 p.m. CDT
- Mayo Clinic Q and A: Who needs back-to-school COVID-19 vaccinations and boosters? Sept. 04, 2022, 11:00 a.m. CDT
- Q&A podcast: Updated COVID-19 boosters target omicron variants Sept. 02, 2022, 12:30 p.m. CDT
Products & Services
- A Book: Endemic - A Post-Pandemic Playbook
- A Book: Future Care
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- COVID-19 vaccines: Get the facts
- How well do face masks protect against coronavirus?
- Post-COVID Recovery
News on coronavirus disease 2019 (COVID-19)
Learn the latest medical news about COVID-19 on Mayo Clinic News Network.
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
- Share full article
Advertisement
Supported by
‘When Normal Life Stopped’: College Essays Reflect a Turbulent Year
This year’s admissions essays became a platform for high school seniors to reflect on the pandemic, race and loss.

By Anemona Hartocollis
This year perhaps more than ever before, the college essay has served as a canvas for high school seniors to reflect on a turbulent and, for many, sorrowful year. It has been a psychiatrist’s couch, a road map to a more hopeful future, a chance to pour out intimate feelings about loneliness and injustice.
In response to a request from The New York Times, more than 900 seniors submitted the personal essays they wrote for their college applications. Reading them is like a trip through two of the biggest news events of recent decades: the devastation wrought by the coronavirus, and the rise of a new civil rights movement.
In the wake of the high-profile deaths of Black people like George Floyd and Breonna Taylor at the hands of police officers, students shared how they had wrestled with racism in their own lives. Many dipped their feet into the politics of protest, finding themselves strengthened by their activism, yet sometimes conflicted.
And in the midst of the most far-reaching pandemic in a century, they described the isolation and loss that have pervaded every aspect of their lives since schools suddenly shut down a year ago. They sought to articulate how they have managed while cut off from friends and activities they had cultivated for years.
To some degree, the students were responding to prompts on the applications, with their essays taking on even more weight in a year when many colleges waived standardized test scores and when extracurricular activities were wiped out.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Open access
- Published: 02 September 2024
Clinical supervisor’s experiences of peer group clinical supervision during COVID-19: a mixed methods study
- Owen Doody ORCID: orcid.org/0000-0002-3708-1647 1 ,
- Kathleen Markey ORCID: orcid.org/0000-0002-3024-0828 1 ,
- James Turner ORCID: orcid.org/0000-0002-8360-1420 2 ,
- Claire O. Donnell ORCID: orcid.org/0000-0003-2386-7048 1 &
- Louise Murphy ORCID: orcid.org/0000-0003-2381-3963 1
BMC Nursing volume 23 , Article number: 612 ( 2024 ) Cite this article
Metrics details
Providing positive and supportive environments for nurses and midwives working in ever-changing and complex healthcare services is paramount. Clinical supervision is one approach that nurtures and supports professional guidance, ethical practice, and personal development, which impacts positively on staff morale and standards of care delivery. In the context of this study, peer group clinical supervision provides allocated time to reflect and discuss care provided and facilitated by clinical supervisors who are at the same grade/level as the supervisees.
To explore the clinical supervisor’s experiences of peer group clinical supervision a mixed methods study design was utilised within Irish health services (midwifery, intellectual disability, general, mental health). The Manchester Clinical Supervision Scale was used to survey clinical supervisors ( n = 36) and semi-structured interviews ( n = 10) with clinical supervisors were conducted. Survey data were analysed through SPSS and interview data were analysed utilising content analysis. The qualitative and quantitative data’s reporting rigour was guided by the CROSS and SRQR guidelines.
Participants generally had a positive encounter when providing clinical supervision. They highly appreciated the value of clinical supervision and expressed a considerable degree of contentment with the supervision they provided to supervisees. The advantages of peer group clinical supervision encompass aspects related to self (such as confidence, leadership, personal development, and resilience), service and organisation (including a positive working environment, employee retention, and safety), and patient care (involving critical thinking and evaluation, patient safety, adherence to quality standards, and elevated levels of care).
There are many benefits of peer group clinical supervision at an individual, service, organisation, and patient level. Nevertheless, there is a need to address a lack of awareness and misconceptions surrounding clinical supervision to create an environment and culture conducive to realising its full potential. It is crucial that clinical supervision be accessible to nurses and midwives of all grades across all healthcare services, with national planning to address capacity and sustainability.
Peer Review reports
Within a dynamic healthcare system, nurses and midwives face growing demands, underscoring the necessity for ongoing personal and professional development. This is essential to improve the effectiveness and efficiency of care delivery for patients, families, and societies. Despite the increased emphasis on increasing the quality and safety of healthcare services and delivery, there is evidence highlighting declining standards of nursing and midwifery care [ 1 ]. The recent focus on re-affirming and re-committing to core values guiding nursing and midwifery practice is encouraging such as compassion, care and commitment [ 2 ], competence, communication, and courage [ 3 ]. However, imposing value statements in isolation is unlikely to change behaviours and greater consideration needs to be given to ways in which compassion, care, and commitment are nurtured and ultimately applied in daily practice. Furthermore, concerns have been raised about global staff shortages [ 4 ], the evidence suggesting several contributing factors such as poor workforce planning [ 5 ], job dissatisfaction [ 6 ], and healthcare migration [ 7 ]. Without adequate resources and staffing, compromising standards of care and threats to patient safety will be imminent therefore the importance of developing effective strategies for retaining competent registered nurses and midwives is paramount in today’s climate of increased staff shortages [ 4 ]. Clinical supervision serves as a means to facilitate these advancements and has been linked to heightened job satisfaction, enhanced staff retention, improved staff effectiveness, and effective clinical governance, by aiding in quality improvements, risk management, and heightened accountability [ 8 ].
Clinical supervision is a key component of professional practice and while the aim is largely known, there is no universally accepted definition of clinical supervision [ 8 ]. Clinical supervision is a structured process where clinicians are allowed protected time to reflect on their practice within a supportive environment and with the purpose of developing high-quality clinical care [ 9 ]. Recent literature published on clinical supervision [ 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ] highlights the advantages and merits of clinical supervision. However, there are challenges also identified such as a lack of consensus regarding the meaning and goal, implementation issues, variations in approaches in its operationalisation, and an absence of research evidence on its effectiveness. Duration and experience in clinical supervision link to positive benefits [ 8 ], but there is little evidence of how clinical supervision altered individual behaviours and practices. This is reinforced by Kuhne et al., [ 15 ] who emphasise that satisfaction rather than effectiveness is more commonly examined. It is crucial to emphasise that reviews have pinpointed that clinical supervision lowers the risks of adverse patient outcomes [ 9 ] and demonstrates enhancements in the execution of certain care processes. Peer group clinical supervision is a form of clinical supervision whereby two or more practitioners engage in a supervision or consultation process to improve their professional practice [ 17 ]. There is limited evidence regarding peer group clinical supervision and research on the experiences of peer clinical supervision and stakeholders is needed [ 13 ]. In Ireland, peer group clinical supervision has been recommended and guidelines have been developed [ 18 ]. In the Irish context, peer clinical supervision is where both clinical supervisees and clinical supervisors are peers at the same level/grade. However, greater evidence is required to inform future decisions on the implementation of peer group clinical supervision and the purpose of this study is to explore clinical supervisors’ experiences of peer group clinical supervision. As the focus is on peer group supervisors and utilising mixed methods the experiences of the other stakeholders were investigated and reported separately.
A mixed methods approach was used (survey and semi-structured interviews) to capture clinical supervisor’s experiences of clinical supervision. The study adhered to the Consensus-Based Checklist for Reporting of Survey Studies guidelines [ 19 ] (Supplementary File S1 ) and Standards for Reporting Qualitative Research guidelines [ 20 ] (Supplementary File S2 ).
Participants
This study was conducted with participants who successfully completed a professionally credited award: clinical supervision module run by a university in Ireland (74 clinical supervisors across 5 programmes over 3 years). The specific selection criteria for participants were that they were registered nurses/midwives delivering peer group clinical supervision within the West region of Ireland. The specific exclusion criteria were as follows: (1) nurses and midwives who haven’t finished the clinical supervision module at the University, (2) newly appointed peer group clinical supervisors who have yet to establish their groups and initiate the delivery of peer group clinical supervision.
Measures and procedures
The Manchester Clinical Supervision Scale-26 was used to survey participants in February/March 2022 and measure the peer group clinical supervisors’ overall experiences of facilitating peer group clinical supervision. The Manchester Clinical Supervision Scale-26 is a validated 26-item self-report questionnaire with a Likert-type (1–5) scale ranging from strongly disagree (1) to strongly agree (5) [ 21 ]. The Manchester Clinical Supervision Scale-26 measures the efficiency of and satisfaction with supervision, to investigate the skills acquisition aspect of clinical supervision and its effect on the quality of clinical care [ 21 ]. The instrument consists of two main sections to measure three (normative, restorative, and formative) dimensions of clinical supervision utilising six sub-scales: (1) trust and rapport, (2) supervisor advice/support, (3) improved care/skills, (4) importance/value of clinical supervision, (5) finding time, (6) personal issues/reflections and a total score for the Manchester Clinical Supervision Scale-26 is also calculated. Section two consisted of the demographic section of the questionnaire and was tailored to include eight demographic questions concerning the supervisor’s demographics, supervisee characteristics, and characteristics of clinical supervision sessions. There were also two open field questions on the Manchester Clinical Supervision Scale-26 (model of clinical supervision used and any other comments about experience of peer group clinical supervision). The main question about participants’ experiences with peer clinical supervision was “What was your experience of peer clinical supervision?” This was gathered through individual semi-structured interviews lasting between 20 and 45 min, in March/April 2022 (Supplementary file 3 ).
Ethical considerations
Health service institutional review boards of two University hospitals approved this study (Ref: 091/19 and Ref: C.A. 2199). Participants were recruited after receiving a full explanation of the study’s purpose and procedure and all relevant information. Participants were aware of potential risks and benefits and could withdraw from the study, or the survey could be stopped at any time. Informed consent was recorded, and participant identities were protected by using a pseudonym to protect anonymity.
Data analysis method
Survey data was analysed using the data analysis software package Statistical Package for the Social Sciences, version 26 (SPSS Inc., Chicago, Il, USA). Descriptive analysis was undertaken to summarise responses to all items and categorical variables (nominal and ordinal) were analysed using frequencies to detail the number and percentage of responses to each question. Scores on the Manchester Clinical Supervision Scale-26 were reverse scored for 9 items (Q1-Q6, Q8, Q20,21) and total scores for each of the six sub-scales were calculated by adding the scores for each item. Raw scores for the individual sub-scales varied in range from 0 to 20 and these raw scores were then converted to percentages which were used in addition to the raw scores for each sub-scale to describe and summarise the results of the Manchester Clinical Supervision Scale-26. Cronbach’s alpha coefficient was undertaken with the 26 questions included within the Manchester Clinical Supervision Scale-26 and more importantly with each of the dimensions in the Manchester Clinical Supervision Scale-26. The open-ended questions on the Manchester Clinical Supervision Scale-26 and interviews were analysed using content analysis guided by Colorafi and Evans [ 22 ] and categories were generated using their eight steps, (1) creating a coding framework, (2) adding codes and memos, (3) applying the first level of coding, (4) categorising codes and applying the second level of coding, (5) revising and redefining the codes, (6) adding memos, (7) visualising data and (8) representing the data.
Research rigour
To ensure the validity and rigour of this study the researchers utilised the Manchester Clinical Supervision Scale-26 a recognised clinical supervision tool with good reliability and wide usage. Interviews were recorded, transcribed, and verified by four participants, data were collected until no new components appeared, data collection methods and analysis procedures were described, and the authors’ biases were minimised throughout the research process. The Manchester Clinical Supervision Scale-26 instrument internal consistency reliability was assessed which was overall good (α = 0.878) with individual subscale also good e.g., normative domain 0.765, restorative domain 0.864, and formative domain 0.900. Reporting rigour was demonstrated using the Consensus-Based Checklist for Reporting of Survey Studies guidelines [ 19 ] and Standards for Reporting Qualitative Research guidelines [ 20 ].
Quantitative data
Participant and clinical supervision characteristics.
Thirty-six of the fifty-two (69.2%) peer group clinical supervisors working across a particular region of Ireland responded to the Manchester Clinical Supervision Scale-26 survey online via Qualtrics. Table 1 identifies the demographics of the sample who were predominantly female (94.4%) with a mean age of 44.7 years (SD. 7.63).
Peer group clinical supervision session characteristics (Table 2 ) highlight over half of peer group clinical supervisors ( n = 20, 55.6%) had been delivering peer group clinical supervision for less than one year and were mainly delivered to female supervisees ( n = 28, 77.8%). Most peer group clinical supervision sessions took place monthly ( n = 32, 88.9%) for 31–60 min ( n = 27, 75%).
Manchester Clinical Supervision Scale-26 results
Participants generally viewed peer group clinical supervision as effective (Table 3 ), the total mean Manchester Clinical Supervision Scale-26 score among all peer group clinical supervisors was 76.47 (SD. 12.801) out of 104, Surpassing the clinical supervision threshold score of 73, which was established by the developers of the Manchester Clinical Supervision Scale-26 as the benchmark indicating proficient clinical supervision provision [ 21 ]. Of the three domains; normative, formative, and restorative, the restorative domain scored the highest (mean 28.56, SD. 6.67). The mean scores compare favourably to that of the Manchester Clinical Supervision Scale-26 benchmark data and suggest that the peer group clinical supervisors were satisfied with both the level of support, encouragement, and guidance they provided and the level of trust/rapport they had developed during the peer group clinical supervision sessions. 83.3% ( n = 30) of peer group clinical supervisors reported being either very satisfied ( n = 12, 33.3%) or moderately satisfied ( n = 18, 50%) with the peer group clinical supervision they currently delivered. Within the peer group clinical supervisor’s supervisee related issues ( n = 17, 47.2%), work environment-related issues ( n = 16, 44.4%), staff-related issues ( n = 15, 41.7%) were reported as the most frequent issues, with patient/client related issues being less frequent ( n = 8, 22.2%). The most identified model used to facilitate peer group clinical supervision was the Proctors model ( n = 8, 22.22%), which was followed by group ( n = 2, 5.55%), peer ( n = 2, 5.55%), and a combination of the seven-eyed model of clinical supervision and Proctors model ( n = 1, 2.77%) with some not sure what model they used ( n = 2, 5.553%) and 58.33% ( n = 21) did not report what model they used.
Survey open-ended question
‘Please enter any additional comments , which are related to your current experience of delivering Peer Group Clinical Supervision.’ There were 22 response comments to this question, which represented 61.1% of the 36 survey respondents, which were analysed using content analysis guided by Colorafi & Evans [ 22 ]. Three categories were generated. These included: personal value/benefit of peer group clinical supervision, challenges with facilitating peer group clinical supervision, and new to peer group clinical supervision.
The first category ‘personal value/benefit of peer group clinical supervision’ highlighted positive experiences of both receiving and providing peer group clinical supervision. Peer group clinical supervisors reported that they enjoyed the sessions and found them both worthwhile and beneficial for both the group and them as peer group clinical supervisors in terms of creating a trusted supportive group environment and motivation to develop. Peer group clinical supervision was highlighted as very important for the peer group clinical supervisors working lives and they hoped that there would be more uptake from all staff. One peer group clinical supervisor expressed that external clinical supervision was a ‘lifeline’ to shaping their supervisory journey to date.
The second category ‘challenges with facilitating peer group clinical supervision’, identified time constraints, lack of buy-in/support from management, staff shortages, lack of commitment by supervisees, and COVID-19 pandemic restrictions and related sick leave, as potential barriers to facilitating peer group clinical supervision. COVID-19 was perceived to have a negative impact on peer group clinical supervision sessions due to staff shortages, which resulted in difficulties for supervisees attending the sessions during work time. Peer group clinical supervisors felt that peer group clinical supervision was not supported by management and there was limited ‘buy-in’ at times. There was also a feeling expressed that peer group clinical supervision was in its infancy, as COVID-19 and its related restrictions impacted on this by either slowing down the process of commencing peer group clinical supervision in certain areas or having to move online. However, more recently improvements in managerial support and supervisee engagement with the peer group clinical supervision process are noted.
The final category ‘new to peer group clinical supervision’ highlighted that some peer group clinical supervisors were new to the process of providing peer group clinical supervision and some felt that this survey was not a true reflection of their experience of delivering peer group clinical supervision, as they were not fully established yet as clinical supervisors due to the impact of COVID-19. Peer group clinical supervisors identified that while they were new to providing peer group clinical supervision, they were enjoying it and that it was a learning curve for them.
Qualitative data
The qualitative phase explored peer group clinical supervisors’ ( n = 10) own experiences of preparation received and experiences of being a peer group clinical supervisor. Three themes were identified through data analysis, building the foundations, enacting engagement and actions, and realities (Table 4 ).
Building the foundations
This theme highlights the importance of prior knowledge, awareness, and training but also the recruitment process and education in preparing peer group clinical supervisors.
Knowledge and awareness
Participant’s prior knowledge and awareness of peer group clinical supervision was mixed with some reporting having little or no knowledge of clinical supervision.
I’m 20 years plus trained as a nurse , and I had no awareness of clinical supervision beforehand , I really hadn’t got a clue what all of this was about , so it was a very new concept to me (Bernie) .
Others were excited about peer group clinical supervision and while they could see the need they were aware that there may be limited awareness of the value and process of clinical supervision among peers.
I find that there’s great enthusiasm and passion for clinical supervision as it’s a great support mechanism for staff in practice , however , there’s a lack of awareness of clinical supervision (Jane) .
Recruitment
Some participants highlighted that the recruitment process to become a peer group clinical supervisor was vague in some organisations with an unclear and non-transparent process evident where people were chosen by the organisation’s management rather than self-selecting interested parties.
It was just the way the training was put to the people , they were kind of nominated and told they were going and there was a lot of upset over that , so they ended up in some not going at all (Ailbhe) .
In addition, the recruitment process was seen as top loaded where senior grades of staff were chosen, and this limited staff nurse grade opportunities where there was a clear need for peer group clinical supervisors and support.
We haven’t got down to the ground level like you know we’ve done the directors , we’ve done the CNM3s the CNM2s we are at the CNM1s , so we need to get down to the staff nurse level so the nurses at the direct frontline are left out and aren’t receiving supervision because we don’t have them trained (Bernie) .
Training and education
Participants valued the training and education provided but there was a clear sense of ‘imposter syndrome’ for some peer group clinical supervisors starting out. Participants questioned their qualifications, training duration, and confidence to undertake the role of peer group clinical supervisor.
Because it is group supervision and I know that you know they say that we are qualified to do supervision and you know we’re now qualified clinical supervisors but I’m not sure that a three-month module qualifies you to be at the top of your game (Maria) .
Participants when engaged in the peer group clinical supervisor educational programme did find it beneficial and the true benefit was the actual re-engagement in education and published evidence along with the mix of nursing and midwifery practice areas.
I found it very beneficial , I mean I hadn’t been engaged in education here in a while , so it was great to be back in that field and you know with the literature that’s big (Claire) .
Enacting engagement and actions
This theme highlights the importance of forming the groups, getting a clear message out, setting the scene, and grounding the group.
Forming the groups
Recruitment for the group was of key importance to the peer group clinical supervisor and they all sent out a general invitation to form their group. Some supervisors used invitation letters or posters in addition to a general email and this was effective in recruiting supervisees.
You’re reaching out to people , I linked in with the ADoN and I put together a poster and circulated that I wasn’t ‘cherry picking , and I set up a meeting through Webex so people could get a sense of what it was if they were on the fence about it or unsure if it was for them (Karen) .
In forming the peer clinical supervision groups consideration needs to be given to the actual number of supervisees and participants reported four to six supervisees as ideal but that number can alter due to attendance.
The ideal is having five or six consistent people and that they all come on board and that you get the dynamics of the group and everything working (Claire) .
Getting a clear message out
Within the recruitment process, it was evident that there was a limited and often misguided understanding or perception of peer group clinical supervision.
Greater awareness of what actually clinical supervision is , people misjudge it as a supervision where someone is appraising you , when in fact it is more of a support mechanism , I think peer support is the key element that needs to be brought out (Jane) .
Given the lack of clarity and understanding regarding peer group clinical supervision, the participants felt strongly that further clarity is needed and that the focus needs to be on the support it offers to self, practice, and the profession.
Clinical supervision to me is clinical leadership (Jane) .
Setting the scene and grounding the group
In the initial phase of the group coming together the aspect of setting the scene and grounding the group was seen as important. A key aspect of this process was establishing the ground rules which not only set the boundaries and gave structure but also ensured the adoption of principles of trust, confidentiality, and safety.
We start with the ground rules , they give us structure it’s our contract setting out the commitment the expectation for us all , and the confidentiality as that’s so important to the trust and safety and building the relationships (Brid) .
Awareness of group dynamics is important in this process along with awareness of the group members (supervisees) as to their role and expectations.
I reiterate the role of each person in relation to confidentiality and the relationship that they would have with each other within the group and the group is very much aware that it is based on respect for each person’s point of view people may have a fear of contributing to the group and setting the ground rules is important (Jane) .
To ground the group, peer group clinical supervisors saw the importance of being present and allowing oneself to be in the room. This was evident in the time allocated at the start of each session to allow ‘grounding’ to occur in the form of techniques such as a short meditation, relaxation, or deep breathing.
At the start , I do a bit of relaxation and deep breathing , and I saw that with our own external supervisor how she settled us into place so very much about connecting with your body and you’ve arrived , then always come in with the contract in my first sentence , remember today you know we’re in a confidential space , of course , you can take away information , but the only information you will take from today is your own information and then the respect aspect (Mary Rose) .
This settling in and grounding was seen as necessary for people to feel comfortable and engage in the peer group clinical supervision process where they could focus, be open, converse, and be aware of their role and the role of peer group clinical supervision.
People have to be open, open about their practice and be willing to learn and this can only occur by sharing, clinical supervision gives us the space to do it in a space where we know we will be respected, and we can trust (Claire) .
This theme highlights the importance of the peer group clinical supervisors’ past experiences, delivering peer group clinical supervision sessions, responding to COVID-19, personal and professional development, and future opportunities.
Past experiences
Past experiences of peer group clinical supervisors were not always positive and for one participant this related to the lack of ground rules or focus of the sessions and the fact it was facilitated by a non-nurse.
In the past , I suppose I would have found it very frustrating as a participant because I just found that it was going round in circles , people moaning and you know it wasn’t very solution focused so I came from my situation where I was very frustrated with clinical supervision , it was facilitated by somebody that was non-nursing then it wasn’t very , there wasn’t the ground rules , it was very loose (Caroline) .
However, many did not have prior experience of peer group clinical supervision. Nonetheless, through the education and preparation received, there was a sense of commitment to embrace the concept, practice, and philosophy.
I did not really have any exposure or really much information on clinical supervision , but it has opened my eyes , and as one might say I am now a believer (Brid) .
Delivering peer group clinical supervision
In delivering peer group clinical supervision, participants felt supervisees were wary, as they did not know what peer group clinical supervision was, and they had focused more on the word supervision which was misleading to them. Nonetheless, the process was challenging, and buy-in was questioned at an individual and managerial level.
Buy-in wasn’t great I think now of course people will blame the pandemic , but this all happened before the pandemic , there didn’t seem to be you know , the same support from management that I would have expected so I kind of understood it in a way because then there wasn’t the same real respect from the practitioners either (Mary Rose) .
From the peer group clinical supervisor’s perspective, they were all novices in delivering/facilitating peer group clinical supervision sessions, and the support of the external clinical supervisors, and their own peer group clinical supervision sessions were invaluable along with a clinical supervision model.
Having supervision myself was key and something that is vital and needed , we all need to look at our practice and how we work it’s no good just facilitating others without being part of the process yourself but for me I would say the three principles of clinical supervision , you know the normative , formative and restorative , I keep hammering that home and bring that in regularly and revisit the contract and I have to do that often you know (Claire) .
All peer group clinical supervisors commented on the preparation for their peer group clinical supervision sessions and the importance of them having the right frame of mind and that often they needed to read over their course work and published evidence.
I want everybody to have a shared voice and you know that if one person , there is something that somebody feels very strongly and wants to talk about it that they e-mail in advance like we don’t have a set agenda but that’s agreed from the participant at the start (Caroline) .
To assist this, the peer group clinical supervisors noted the importance of their own peer group clinical supervision, the support of their peers, and external clinical supervisors. This preparation in an unpredictable situation can be difficult but drawing on one’s experience and the experience within the group can assist in navigating beyond unexpected situations.
I utilise the models of clinical supervision and this helps guide me , I am more of a facilitator of the group we are experts in our own area and our own role but you can only be an expert if you take the time to examine your practice and how you operate in your role (Brid) .
All clinical supervisors noted that the early sessions can be superficial, and the focus can be on other practice or management issues, but as time moves on and people become more engaged and involved it becomes easier as their understanding of supervision becomes clearer. In addition, there may be hesitancy and people may have difficulty opening up with certain people in the group and this is a reality that can put people off.
Initially there was so much managerial bashing and I think through supervision , I began to kind of think , I need the pillars of supervision , the governance , bringing more knowledge and it shifted everything in the room , trying to marry it with all the tensions that people have (Mary Rose) .
For some clinical supervisors, there were expected and unexpected challenges for them as clinical supervisors in terms of the discussions veering off course and expectations of their own ability.
The other big challenge is when they go off , how do you bring him back , you know when they veer off and you’re expected to be a peer , but you have to try and recoil that you have to get the balance with that right (Mary Rose) .
While peer group clinical supervision is accepted and seen as a valuable process by the peer group clinical supervisors, facilitating peer group supervision with people known to you can be difficult and may affect the process.
I’d love to supervise a group where I actually don’t know the people , I don’t know the dynamics within the group , and I’d love to see what it would be like in a group (Bernie) .
Of concern to clinical supervisors was the aspect of non-attendance and while there may be valid reasons such as COVID-19 the absence of a supervisee for several sessions can affect the group dynamics, especially if the supervisee has only engaged with early group sessions.
One of the ones that couldn’t attend because of COVID and whatever , but she’s coming to the next one and I just feel there’s a lot of issues in her area and I suppose I’m mindful that I don’t want that sort of thing to seep in , so I suppose it’s just for me just to keep reiterating the ground rules and the boundaries , that’s something I just have to manage as a facilitator , but what if they don’t attend how far will the group have progressed before she attends (Caroline) .
Responding to COVID-19
The advent of COVID-19 forced peer group clinical supervisors to find alternative means of providing peer group clinical supervision sessions which saw the move from face-to-face to online sessions. The online transition was seen as seamless for many established groups while others struggled to deliver sessions.
With COVID we did online for us it was fine because we were already formed (Corina) .
While the transition may have been positive many clinical supervisors came across issues because they were using an online format that would not be present in the face-to-face session.
We did have a session where somebody was in the main office and they have a really loud booming voice and they were saying stuff that was not appropriate to say outside of clinical supervision and I was like are you in the office can you lower it down a bit can you put your headphones on (Maria) .
However, two peer group clinical supervisors ceased or hasted the progress of rolling out peer group clinical supervision sessions mainly due to redeployment and staff availability.
With COVID it just had to be canceled here , it’s just the whole thing was canceled so it was very , very difficult for people (Mary Rose) .
It was clear from clinical supervisors that online sessions were appropriate but that they felt they were only appropriate for existing established groups that have had the opportunity to build relationships, develop trust, embed the ground rules, and create the space for open communication and once established a combined approach would be appropriate.
Since we weren’t as established as a group , not everybody knew each other it would be difficult to establish that so we would hold off/reschedule , obviously COVID is a major one but also I suppose if you have an established group now , and again , you could go to a remote one , but I felt like since we weren’t established as a group it would be difficult to develop it in that way (Karen) .
Within practice COVID-19 took priority and other aspects such as peer group clinical supervision moved lower down on the priority list for managers but not for the clinical supervisors even where redeployment occurred.
With COVID all the practical side , if one of the managers is dealing with an outbreak , they won’t be attending clinical supervision , because that has to be prioritised , whereas we’ve prioritised clinical supervision (Maria) .
The valuing of peer group clinical supervision was seen as important by clinical supervisors, and they saw it as particularly needed during COVID-19 as staff were dealing with many personal and professional issues.
During the height of COVID , we had to take a bit of a break for four months as things were so demanding at work for people but then I realised that clinical supervision was needed and started back up and they all wanted to come back (Brid) .
Having peer group clinical supervision during COVID-19 supported staff and enabled the group to form supportive relationships.
COVID has impacted over the last two years in every shape and they needed the supervision and the opportunity to have a safe supportive space and it gelled the group I think as we all were there for each other (Claire) .
While COVID-19 posed many challenges it also afforded clinical supervisors and supervisees the opportunity for change and to consider alternative means of running peer group clinical supervision sessions. This change resulted in online delivery and in reflecting on both forms of delivery (face-to-face and online) clinical supervisors saw the benefit in both. Face-to-face was seen as being needed to form the group and then the group could move online once the group was established with an occasional periodic face-to-face session to maintain motivation commitment and reinforce relationships and support.
Online formats can be effective if the group is already established or the group has gone through the storming and forming phase and the ground rules have been set and trust built , then I don’t see any problem with a blended online version of clinical supervision , and I think it will be effective (Jane) .
Personal and professional development
Growth and development were evident from peer group clinical supervisors’ experiences and this growth and development occurred at a personal, professional, and patient/client level. This development also produced an awakening and valuing of one’s passion for self and their profession.
I suppose clinical supervision is about development I can see a lot of development for me and my supervisees , you know personally and professionally , it’s the support really , clinical supervision can reinvigorate it’s very exciting and a great opportunity for nursing to support each other and in care provision (Claire) .
A key to the peer group clinical supervisor’s development was the aspect of transferable skills and the confidence they gained in fulfilling their role.
All of these skills that you learn are transferable and I am a better manager because of clinical supervision (Maria) .
The confidence and skills gained translated into the clinical supervisor’s own practice as a clinical practitioner and clinical supervisor but they were also realistic in predicting the impact on others.
I have empowered my staff , I empower them to use their voice and I give my supervisees a voice and hope they take that with them (Corina) .
Fundamental to the development process was the impact on care itself and while this cannot always be measured or identified, the clinical supervisors could see that care and support of the individual practitioner (supervisee) translated into better care for the patient/client.
Care is only as good as the person delivering it and what they know , how they function and what energy and passion they have , and clinical supervision gives the person support to begin to understand their practice and how and why they do things in a certain way and when they do that they can begin to question and even change their way of doing something (Brid) .
Future opportunities
Based on the clinical supervisor’s experiences there was a clear need identified regarding valuing and embedded peer group clinical supervision within nursing/midwifery practice.
There has to be an emphasis placed on supervision it needs to be part of the fabric of a service and valued by all in that service , we should be asking why is it not available if it’s not there but there is some work first on promoting it and people knowing what it actually is and address the misconceptions (Claire) .
While such valuing and buy-in are important, it is not to say that all staff need to have peer group clinical supervision so as to allow for personal choice. In addition, to value peer group clinical supervision it needs to be evident across all staffing grades and one could question where the best starting point is.
While we should not mandate that all staff do clinical supervision it should become embedded within practice more and I suppose really to become part of our custom and practice and be across all levels of staff (Brid) .
When peer group clinical supervision is embedded within practice then it should be custom and practice, where it is included in all staff orientations and is nationally driven.
I suppose we need to be driving it forward at the coal face at induction , at orientation and any development for the future will have to be driven by the NMPDUs or nationally (Ailbhe) .
A formalised process needs to address the release of peer group clinical supervisors but also the necessity to consider the number of peer group clinical supervisors at a particular grade.
The issue is release and the timeframe as they have a group but they also have their external supervision so you have to really work out how much time you’re talking about (Maria) .
Vital within the process of peer group clinical supervision is receiving peer group clinical supervision and peer support and this needs to underpin good peer group clinical supervision practice.
Receiving peer group supervision helps me , there are times where I would doubt myself , it’s good to have the other group that I can go to and put it out there to my own group and say , look at this , this is what we did , or this is what came up and this is how (Bernie) .
For future roll out to staff nurse/midwife grade resourcing needs to be considered as peer group clinical supervisors who were managers could see the impact of having several peer group clinical supervisors in their practice area may have on care delivery.
Facilitating groups is an issue and needs to be looked at in terms of the bigger picture because while I might be able to do a second group the question is how I would be supported and released to do so (Maria) .
While there was ambiguity regarding peer group clinical supervision there was an awareness of other disciplines availing of peer group clinical supervision, raising questions about the equality of supports available for all disciplines.
I always heard other disciplines like social workers would always have been very good saying I can’t meet you I have supervision that day and I used to think my God what’s this fabulous hour that these disciplines are getting and as a nursing staff it just wasn’t there and available (Bernie) .
To address this equity issue and the aspect of low numbers of certain grades an interdisciplinary approach within nursing and midwifery could be used or a broader interdisciplinary approach across all healthcare professionals. An interdisciplinary or across-services approach was seen as potentially fruitful.
I think the value of interprofessional or interdisciplinary learning is key it addresses problem-solving from different perspectives that mix within the group is important for cross-fertilisation and embedding the learning and developing the experience for each participant within the group (Jane) .
As we move beyond COVID-19 and into the future there is a need to actively promote peer group clinical supervision and this would clarify what peer group clinical supervision actually is, its uptake and stimulate interest.
I’d say it’s like promoting vaccinations if you could do a roadshow with people , I think that would be very beneficial , and to launch it , like you have a launch an official launch behind it (Mary Rose) .
The advantages of peer group clinical supervision highlighted in this study pertain to self-enhancement (confidence, leadership, personal development, resilience), organisational and service-related aspects (positive work environment, staff retention, safety), and professional patient care (critical thinking and evaluation, patient safety, adherence to quality standards, elevated care standards). These findings align with broader literature that acknowledges various areas, including self-confidence and facilitation [ 23 ], leadership [ 24 ], personal development [ 25 ], resilience [ 26 ], positive/supportive working environment [ 27 ], staff retention [ 28 ], sense of safety [ 29 ], critical thinking and evaluation [ 30 ], patient safety [ 31 ], quality standards [ 32 ] and increased standards of care [ 33 ].
In this study, peer group clinical supervision appeared to contribute to the alleviation of stress and anxiety. Participants recognised the significance of these sessions, where they could openly discuss and reflect on professional situations both emotionally and rationally. Central to these discussions was the creation of a safe, trustworthy, and collegial environment, aligning with evidence in the literature [ 34 ]. Clinical supervision provided a platform to share resources (information, knowledge, and skills) and address issues while offering mutual support [ 35 ]. The emergence of COVID-19 has stressed the significance of peer group clinical supervision and support for the nursing/midwifery workforce [ 36 ], highlighting the need to help nurses/midwifes preserve their well-being and participate in collaborative problem-solving. COVID-19 impacted and disrupted clinical supervision frequency, duration and access [ 37 ]. What was evident during COVID-19 was the stress and need for support for staff and given the restorative or supportive functions of clinical supervision it is a mechanism of support. However, clinical supervisors need support themselves to be able to better meet the supervisee’s needs [ 38 ].
The value of peer group clinical supervision in nurturing a conducive working environment cannot be overstated, as it indorses the understanding and adherence to workplace policies by empowering supervisees to understand the importance and rationale behind these policies [ 39 ]. This becomes vital in a continuously changing healthcare landscape, where guidelines and policies may be subject to change, especially in response to situations such as COVID-19. In an era characterised by international workforce mobility and a shortage of healthcare professionals, a supportive and positive working environment through the provision of peer group clinical supervision can positively influence staff retention [ 40 ], enhance job satisfaction [ 41 ], and mitigate burnout [ 42 ]. A critical aspect of the peer group clinical supervision process concerns providing staff the opportunity to reflect, step back, problem-solve and generate solutions. This, in turn, ensures critical thinking and evaluation within clinical supervision, focusing on understanding the issues and context, and problem-solving to draw constructive lessons for the future [ 30 ]. Research has determined a link between clinical supervision and improvements in the quality and standards of care [ 31 ]. Therefore, peer group clinical supervision plays a critical role in enhancing patient safety by nurturing improved communication among staff, facilitating reflection, promoting greater self-awareness, promoting the exchange of ideas, problem-solving, and facilitating collective learning from shared experiences.
Starting a group arose as a foundational aspect emphasised in this study. The creation of the environment through establishing ground rules, building relationships, fostering trust, displaying respect, and upholding confidentiality was evident. Vital to this process is the recruitment of clinical supervisees and deciding the suitable group size, with a specific emphasis on addressing individuals’ inclination to engage, their knowledge and understanding of peer group clinical supervision, and dissipating any lack of awareness or misconceptions regarding peer group supervision. Furthermore, the educational training of peer group clinical supervisors and the support from external clinical supervisors played a vital role in the rollout and formation of peer group clinical supervision. The evidence stresses the significance of an open and safe environment, wherein supervisees feel secure and trust their supervisor. In such an environment, they can effectively reflect on practice and related issues [ 41 ]. This study emphasises that the effectiveness of peer group supervision is more influenced by the process than the content. Clinical supervisors utilised the process to structure their sessions, fostering energy and interest to support their peers and cultivate new insights. For peer group clinical supervision to be effective, regularity is essential. Meetings should be scheduled in advance, allocate protected time, and take place in a private space [ 35 ]. While it is widely acknowledged that clinical supervisors need to be experts in their professional field to be credible, this study highlights that the crucial aspects of supervision lie in the quality of the relationship with the supervisor. The clinical supervisor should be supportive, caring, open, collaborative, sensitive, flexible, helpful, non-judgmental, and focused on tacit knowledge, experiential learning, and providing real-time feedback.
Critical to the success of peer group clinical supervision is the endorsement and support from management, considering the organisational culture and attitudes towards the practice of clinical supervision as an essential factor [ 43 ]. This support and buy-in are necessary at both the management and individual levels [ 28 ]. The primary obstacles to effective supervision often revolve around a lack of time and heavy workloads [ 44 ]. Clinical supervisors frequently struggle to find time amidst busy environments, impacting the flexibility and quality of the sessions [ 45 ]. Time constraints also limit the opportunity for reflection within clinical supervision sessions, leaving supervisees feeling compelled to resolve issues on their own without adequate support [ 45 ]. Nevertheless, time-related challenges are not unexpected, prompting a crucial question about the value placed on clinical supervision and its integration into the culture and fabric of the organisation or profession to make it a customary practice. Learning from experiences like those during the COVID-19 pandemic has introduced alternative ways of working, and the use of technology (such as Zoom, Microsoft Teams, Skype) may serve as a means to address time, resource, and travel issues associated with clinical supervision.
Despite clinical supervision having a long international history, persistent misconceptions require attention. Some of these include not considering clinical supervision a priority [ 46 ], perceiving it as a luxury [ 41 ], deeming it self-indulgent [ 47 ], or viewing it as mere casual conversation during work hours [ 48 ]. A significant challenge lies in the lack of a shared understanding regarding the role and purpose of clinical supervision, with past perceptions associating it with surveillance and being monitored [ 48 ]. These negative connotations often result in a lack of engagement [ 41 ]. Without encouragement and recognition of the importance of clinical supervision from management or the organisation, it is unlikely to become embedded in the organisational culture, impeding its normalisation [ 39 ].
In this study, some peer group clinical supervisors expressed feelings of being impostors and believed they lacked the knowledge, skills, and training to effectively fulfil their roles. While a deficiency in skills and competence are possible obstacles to providing effective clinical supervision [ 49 ], the peer group clinical supervisors in this study did not report such issues. Instead, their concerns were more about questioning their ability to function in the role of a peer group clinical supervisor, especially after a brief training program. The literature acknowledges a lack of training where clinical supervisors may feel unprepared and ill-equipped for their role [ 41 ]. To address these challenges, clinical supervisors need to be well-versed in professional guidelines and ethical standards, have clear roles, and understand the scope of practice and responsibilities associated with being a clinical supervisor [ 41 ].
The support provided by external clinical supervisors and the peer group clinical supervision sessions played a pivotal role in helping peer group clinical supervisors ease into their roles, gain experiential learning, and enhance their facilitation skills within a supportive structure. Educating clinical supervisors is an investment, but it should not be a one-time occurrence. Ongoing external clinical supervision for clinical supervisors [ 50 ] and continuous professional development [ 51 ] are crucial, as they contribute to the likelihood of clinical supervisors remaining in their roles. However, it is important to interpret the results of this study with caution due to the small sample size in the survey. Generalising the study results should be approached with care, particularly as the study was limited to two regions in Ireland. However, the addition of qualitative data in this mixed-methods study may have helped offset this limitation.
This study highlights the numerous advantages of peer group clinical supervision at individual, service, organisational, and patient/client levels. Success hinges on addressing the initial lack of awareness and misconceptions about peer group clinical supervision by creating the right environment and establishing ground rules. To unlock the full potential of peer group clinical supervision, it is imperative to secure management and organisational support for staff release. More crucially, there is a need for valuing and integrating peer group clinical supervision into nursing and midwifery education and practice. Making peer group clinical supervision accessible to all grades of nurses and midwives across various healthcare services is essential, necessitating strategic planning to tackle capacity and sustainability challenges.
Data availability
Data are available from the corresponding author upon request owing to privacy or ethical restrictions.
Zelenikova R, Gurkova E, Friganovic A, Uchmanowicz I, Jarosova D, Ziakova K, Plevova I, Papastavrou E. Unfinished nursing care in four central European countries. J Nurs Manage. 2020;28(8):1888–900. https://doi.org/10.1111/jonm.12896 .
Article Google Scholar
Department of Health, Office of the Chief Nursing Officer. Position paper 1: values for nurses and midwives in Ireland. Dublin: The Stationery Office; 2016.
Google Scholar
Cummings J, Bennett V. Developing the culture of compassionate care: creating a new vision for nurses, midwives and care-givers. London: Department of Health; 2012.
Both-Nwabuwe JM, Dijkstra MT, Klink A, Beersma B. Maldistribution or scarcity of nurses: the devil is in the detail. J Nurs Manage. 2018;26(2):86–93. https://doi.org/10.1111/jonm.12531 .
Squires A, Jylha V, Jun J, Ensio A, Kinnunen J. A scoping review of nursing workforce planning and forecasting research. J Nurs Manage. 2017;25:587–96. https://doi.org/10.1111/jonm.12510 .
Sasso L, Bagnasco A, Catania G, Zanini M, Aleo G, Watson R. Push and pull factors of nurses’ intention to leave. J Nurs Manage. 2019;27:946–54. https://doi.org/10.1111/jonm.12745 .
Gea-Caballero V, Castro-Sánchez E, Díaz‐Herrera MA, Sarabia‐Cobo C, Juárez‐Vela R, Zabaleta‐Del Olmo E. Motivations, beliefs, and expectations of Spanish nurses planning migration for economic reasons: a cross‐sectional, web‐based survey. J Nurs Scholarsh. 2019;51(2):178–86. https://doi.org/10.1111/jnu.12455 .
Article PubMed Google Scholar
Cutcliffe J, Sloan G, Bashaw M. A systematic review of clinical supervision evaluation studies in nursing. Int J Ment Health Nurs. 2018;27:1344–63. https://doi.org/10.1111/inm.12443 .
Snowdon DA, Hau R, Leggat SG, Taylor NF. Does clinical supervision of health professionals improve patient safety? A systematic review and meta-analysis. Int J Qual Health C. 2016;28(4):447–55. https://doi.org/10.1093/intqhc/mzw059 .
Turner J, Hill A. Implementing clinical supervision (part 1): a review of the literature. Ment Health Nurs. 2011;31(3):8–12.
Dilworth S, Higgins I, Parker V, Kelly B, Turner J. Finding a way forward: a literature review on the current debates around clinical supervision. Contemp Nurse. 2013;45(1):22–32. https://doi.org/10.5172/conu.2013.45.1.22 .
Buss N, Gonge H. Empirical studies of clinical supervision in psychiatric nursing: a systematic literature review and methodological critique. Int J Ment Health Nurs. 2009;18(4):250–64. https://doi.org/10.1111/j.1447-0349.2009.00612.x .
Pollock A, Campbell P, Deery R, Fleming M, Rankin J, Sloan G, Cheyne H. A systematic review of evidence relating to clinical supervision for nurses, midwives and allied health professionals. J Adv Nurs. 2017;73(8):1825–37. https://doi.org/10.1111/jan.13253 .
Snowdon DA, Leggat SG, Taylor NF. Does clinical supervision of healthcare professionals improve effectiveness of care and patient experience: a systematic review. BMC Health Serv Res. 2017;17(1):1–11. https://doi.org/10.1186/s12913-017-2739-5 .
Kühne F, Maas J, Wiesenthal S, Weck F. Empirical research in clinical supervision: a systematic review and suggestions for future studies. BMC Psychol. 2019;7(1):1–11. https://doi.org/10.1186/s40359-019-0327-7 .
Snowdon DA, Sargent M, Williams CM, Maloney S, Caspers K, Taylor NF. Effective clinical supervision of allied health professionals: a mixed methods study. BMC Health Serv Res. 2020;20(1):1–11. https://doi.org/10.1186/s12913-019-4873-8 .
Borders LD. Dyadic, triadic, and group models of peer supervision/consultation: what are their components, and is there evidence of their effectiveness? Clin Psychol. 2012;16(2):59–71.
Health Service Executive. Guidance document on peer group clinical supervision. Mayo: Nursing and Midwifery Planning and Development Unit Health Service Executive West Mid West; 2023.
Sharma A, Minh Duc NT, Lam Thang L, Nam T, Ng NH, Abbas SJ, Huy KS, Marušić NT, Paul A, Kwok CL. Karamouzian, M. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med. 2021;36(10):3179–87. https://doi.org/10.1007/s11606-021-06737-1 .
Article PubMed PubMed Central Google Scholar
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;899:1245–51. https://doi.org/10.1097/ACM.0000000000000388 .
Winstanley J, White E. The MCSS-26©: revision of the Manchester Clinical Supervision Scale© using the Rasch Measurement Model. J Nurs Meas. 2011;193(2011):160–78. https://doi.org/10.1891/1061-3749.19.3.160 .
Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. HERD-Health Env Res. 2016;9:16–25. https://doi.org/10.1177/1937586715614171 .
Agnew T, Vaught CC, Getz HG, Fortune J. Peer group clinical supervision program fosters confidence and professionalism. Prof Sch Couns. 2000;4(1):6–12.
Mc Carthy V, Goodwin J, Saab MM, Kilty C, Meehan E, Connaire S, O’Donovan A. Nurses and midwives’ experiences with peer-group clinical supervision intervention: a pilot study. J Nurs Manage. 2021;29:2523–33. https://doi.org/10.1111/jonm.13404 .
Rothwell C, Kehoe A, Farook SF, Illing J. Enablers and barriers to effective clinical supervision in the workplace: a rapid evidence review. BMJ Open. 2021;119:e052929. https://doi.org/10.1136/bmjopen-2021-052929 .
Francis A, Bulman C. In what ways might group clinical supervision affect the development of resilience in hospice nurses. Int J Palliat Nurs. 2019;25:387–96. https://doi.org/10.12968/ijpn.2019.25.8.387 .
Chircop Coleiro A, Creaner M, Timulak L. The good, the bad, and the less than ideal in clinical supervision: a qualitative meta-analysis of supervisee experiences. Couns Psychol Quart. 2023;36(2):189–210. https://doi.org/10.1080/09515070.2021.2023098 .
Stacey G, Cook G, Aubeeluck A, Stranks B, Long L, Krepa M, Lucre K. The implementation of resilience based clinical supervision to support transition to practice in newly qualified healthcare professionals. Nurs Educ Today. 2020;94:104564. https://doi.org/10.1016/j.nedt.2020.104564 .
Feerick A, Doyle L, Keogh B. Forensic mental health nurses’ perceptions of clinical supervision: a qualitative descriptive study. Issues Ment Health Nurs. 2021;42:682–9. https://doi.org/10.1080/01612840.2020.1843095 .
Corey G, Haynes RH, Moulton P, Muratori M. Clinical supervision in the helping professions: a practical guide. Alexandria, VA: American Counseling Association; 2021.
Sturman N, Parker M, Jorm C. Clinical supervision in general practice training: the interweaving of supervisor, trainee and patient entrustment with clinical oversight, patient safety and trainee learning. Adv Health Sci Educ. 2021;26:297–311. https://doi.org/10.1007/s10459-020-09986-7 .
Alfonsson S, Parling T, Spännargård Å, Andersson G, Lundgren T. The effects of clinical supervision on supervisees and patients in cognitive behavioral therapy: a systematic review. Cogn Behav Therapy. 2018;47(3):206–28. https://doi.org/10.1080/16506073.2017.1369559 .
Coelho M, Esteves I, Mota M, Pestana-Santos M, Santos MR, Pires R. Clinical supervision of the nurse in the community to promote quality of care provided by the caregiver: scoping review protocol. Millenium J Educ Technol Health. 2022;2:83–9. https://doi.org/10.29352/mill0218.26656 .
Toros K, Falch-Eriksen A. Structured peer group supervision: systematic case reflection for constructing new perspectives and solutions. Int Soc Work. 2022;65:1160–5. https://doi.org/10.1177/0020872820969774 .
Bifarin O, Stonehouse D. Clinical supervision: an important part of every nurse’s practice. Brit J Nurs. 2017;26(6):331–5. https://doi.org/10.12968/bjon.2017.26.6.331 .
Turner J, Simbani N, Doody O, Wagstaff C, McCarthy-Grunwald S. Clinical supervision in difficult times and at all times. Ment Health Nurs. 2022;42(1):10–3.
Martin P, Tian E, Kumar S, Lizarondo L. A rapid review of the impact of COVID-19 on clinical supervision practices of healthcare workers and students in healthcare settings. J Adv Nurs. 2022;78:3531–9. https://doi.org/10.1111/jan.15360 .
van Dam M, van Hamersvelt H, Schoonhoven L, Hoff RG, Cate OT, Marije P. Hennus. Clinical supervision under pressure: a qualitative study amongst health care professionals working on the ICU during COVID-19. Med Edu Online. 2023;28:1. https://doi.org/10.1080/10872981.2023.2231614 .
Martin P, Lizarondo L, Kumar S, Snowdon D. Impact of clinical supervision on healthcare organisational outcomes: a mixed methods systematic review. PLoS ONE. 2021;1611:e0260156. https://doi.org/10.1371/journal.pone.0260156 .
Article CAS Google Scholar
Hussein R, Salamonson Y, Hu W, Everett B. Clinical supervision and ward orientation predict new graduate nurses’ intention to work in critical care: findings from a prospective observational study. Aust Crit Care. 2019;325:397–402. https://doi.org/10.1016/j.aucc.2018.09.003 .
Love B, Sidebotham M, Fenwick J, Harvey S, Fairbrother G. Unscrambling what’s in your head: a mixed method evaluation of clinical supervision for midwives. Women Birth. 2017;30:271–81. https://doi.org/10.1016/j.wombi.2016.11.002 .
Berry S, Robertson N. Burnout within forensic psychiatric nursing: its relationship with ward environment and effective clinical supervision? J Psychiatr Ment Health Nurs. 2019;26:7–8. https://doi.org/10.1111/jpm.12538 .
Markey K, Murphy L, O’Donnell C, Turner J, Doody O. Clinical supervision: a panacea for missed care. J Nurs Manage. 2020;28:2113–7. https://doi.org/10.1111/jonm.13001 .
Brody AA, Edelman L, Siegel EO, Foster V, Bailey DE Jr., Bryant AL, Bond SM. Evaluation of a peer mentoring program for early career gerontological nursing faculty and its potential for application to other fields in nursing and health sciences. Nurs Outlook. 2016;64(4):332–8. https://doi.org/10.1016/j.outlook.2016.03.004 .
Bulman C, Forde-Johnson C, Griffiths A, Hallworth S, Kerry A, Khan S, Mills K, Sharp P. The development of peer reflective supervision amongst nurse educator colleagues: an action research project. Nurs Educ Today. 2016;45:148–55. https://doi.org/10.1016/j.nedt.2016.07.010 .
Pack M. Unsticking the stuckness’: a qualitative study of the clinical supervisory needs of early-career health social workers. Brit J Soc Work. 2015;45:1821–36. https://doi.org/10.1093/bjsw/bcu069 .
Bayliss J. Clinical supervision for palliative care. London: Quay Books; 2006.
Kenny A, Allenby A. Implementing clinical supervision for Australian rural nurses. Nurs Educ Pract. 2013;13(3):165–9. https://doi.org/10.1016/j.nepr.2012.08.009 .
MacLaren J, Stenhouse R, Ritchie D. Mental health nurses’ experiences of managing work-related emotions through supervision. J Adv Nurs. 2016;72:2423–34. https://doi.org/10.1111/jan.12995 .
Wilson HM, Davies JS, Weatherhead S. Trainee therapists’ experiences of supervision during training: a meta-synthesis. Clinl Psychol Psychother. 2016;23:340–51. https://doi.org/10.1002/cpp.1957 .
Noelker LS, Ejaz FK, Menne HL, Bagaka’s JG. Factors affecting frontline workers’ satisfaction with supervision. J Aging Health. 2009;21(1):85–101. https://doi.org/10.1177/0898264308328641 .
Download references
Acknowledgements
The research team would like to thank all participants for their collaboration, the HSE steering group members and Carmel Hoey, NMPDU Director, HSE West Mid West, Dr Patrick Glackin, NMPD Area Director, HSE West, Annette Cuddy, Director, Centre of Nurse and Midwifery Education Mayo/Roscommon; Ms Ruth Hoban, Assistant Director of Nursing and Midwifery (Prescribing), HSE West; Ms Annette Connolly, NMPD Officer, NMPDU HSE West Mid West.
The authors declare that there are no sources of funding associated with this paper.
Author information
Authors and affiliations.
Department of Nursing and Midwifery, Health Research Institute, University of Limerick, Limerick, Ireland
Owen Doody, Kathleen Markey, Claire O. Donnell & Louise Murphy
Department of Nursing and Midwifery, Sheffield Hallam University, Sheffield, UK
James Turner
You can also search for this author in PubMed Google Scholar
Contributions
OD: Conceptualization, Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Project administration, Funding acquisition. COD: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition. KM: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition. JT: Methodology, Formal analysis, Writing - Original Draft, Writing - Review & Editing. LM: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition.
Corresponding author
Correspondence to Owen Doody .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by two health service institutional review boards University Hospital Limerick (Ref: 091/19) and Galway University Hospitals (Ref: C.A. 2199). The study was conducted in accordance with the principles of the Declaration of Helsinki and all study details were fully disclosed to participants, who were assured of the voluntary nature of participation and withdrawal. The study questionnaires were coded, and identities were not disclosed to guarantee participants’ anonymity and all participants provided written informed consent before interviews.
Consent for publication
No identifying images or other personal or clinical details of participants are presented in this paper that would compromise anonymity and all participants were aware and informed through the Participant Information Leaflet that the data collected may be reported through article and/or conference publications and this was reiterated during the qualitative data collection stage.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Doody, O., Markey, K., Turner, J. et al. Clinical supervisor’s experiences of peer group clinical supervision during COVID-19: a mixed methods study. BMC Nurs 23 , 612 (2024). https://doi.org/10.1186/s12912-024-02283-3
Download citation
Received : 04 January 2024
Accepted : 22 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12912-024-02283-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical supervision
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Startup guru Paul Graham eviscerates Silicon Valley’s conventional wisdom about founders

Y Combinator cofounder Paul Graham generated buzz on Sunday as the startup guru sought to dismantle some conventional wisdom in Silicon Valley about founders running the companies they started.
In an essay posted to his website, he recalled a talk that Airbnb cofounder and CEO Brian Chesky gave last week that many attendees told him was the best they had ever heard.
“The theme of Brian’s talk was that the conventional wisdom about how to run larger companies is mistaken,” Graham wrote. “As Airbnb grew, well-meaning people advised him that he had to run the company in a certain way for it to scale. Their advice could be optimistically summarized as ‘hire good people and give them room to do their jobs.’ He followed this advice and the results were disastrous.”
So instead, Chesky studied what the late Apple cofounder Steve Jobs did when he was running his company, he added.
The talk was attended by many of the founders that Y Combinator supported, and they told Graham that they received the same conventional wisdom with similar results.
“Why was everyone telling these founders the wrong thing? That was the big mystery to me,” he wrote. “And after mulling it over for a bit I figured out the answer: what they were being told was how to run a company you hadn’t founded—how to run a company if you’re merely a professional manager.”
Graham argued you can run a company either in manager mode or founder mode. Most people in Silicon Valley have assumed that scaling up a startup required the former. But founders can do things that managers can’t, he added, so this advice feels “broken” to founders.
Meanwhile, founder mode isn’t taught in books or business schools. But he said some of its principles can be inferred from the problems that founders have encountered while in manager mode, which preaches telling direct reports what to do and not getting involved in details so as to avoid looking like a micromanager.
While that sounds fine on paper, manager mode often results in “professional fakers” driving companies into the ground, according to Graham. As a result, founders feel like they’re being gaslit by advisers and employees urging manager mode.
“VCs who haven’t been founders themselves don’t know how founders should run companies, and C-level execs, as a class, include some of the most skillful liars in the world,” he said.
While the exact outlines of founder mode aren’t totally clear right now, Graham offered some predictions, including that skip-level meetings—where top execs meet employees without their direct supervisors—become the norm.
To be sure, founders will have to delegate some duties as their companies get bigger, and he acknowledged that founder mode will be more complicated than manager mode as the amount of autonomy varies.
But founder mode will work better, he added. “Indeed, another prediction I’ll make about founder mode is that once we figure out what it is, we’ll find that a number of individual founders were already most of the way there—except that in doing what they did they were regarded by many as eccentric or worse.”
Airbnb and Y Combinator didn’t immediately respond to requests for comment. But Chesky reposted Graham’s tweet that linked to his essay. In 2013, Chesky recalled having a “ CEO council ” to help him and more recently revealed that he has an informal practice of creating work duos for employees at Airbnb.
Meanwhile, serial entrepreneur Howard Lerman posted on X that many founders were “absolutely fired up” by the essay.
“I know I am. Building a company is all I know how to do, and all I ever want to do,” he wrote.
Latest in Leadership

Behind the scenes of how ‘effective altruism’ went to die in Sam Bankman-Fried’s Bahamas penthouse

People trying to access Elon Musk’s X in Brazil face daily fines greater than their annual wage

Most American workers want a union—and it may be the only way to save the middle class

Kurt Geiger’s CEO went from cleaning toilets to running a $432 million fashion brand—he says he got promoted by making his boss look brilliant

A 42-year-old Chinese heiress known as the ‘princess of Wahaha’ takes over father’s beverage empire
Most popular.

Staying fit as you age isn’t just about exercise. Experts say to prioritize these 4 habits

Warren Buffett turns 94 today. His secret to longevity? Coca-Cola, candy, and a life of joy

IMAGES
VIDEO
COMMENTS
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness. Also Read: Essay on My Best Friend. Essay On COVID-19 in 300 Words. COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide.
Published July 21, 2021. Coronavirus (or, as doctors and scientists call it, COVID-19) has been part of everyone's life since mid-March 2020, when most schools, businesses, and communities quickly changed how they operated to prevent the spread of the virus. Because the disease infected a large number of people all over the world, experts ...
Here are over 40 coronavirus-related Student Opinion writing prompts that cover an array of topics, like family life, dealing with anxiety, life without sports, voting during a time of social ...
DOI: 10.1001/JAMA.2020.7308. The author discusses the economic and healthcare crisis the COVID-19 pandemic created. The projections drawn in the paper predict a 10 to 25% contraction of the US economy in the second quarter. The writer asserts that the United States has entered a COVID-19 recession.
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
Coronavirus disease (COVID-19) Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention.
Becoming a storyteller at WHYY, your local public media station, is easier than you might think. Text STORYTELLER to 267-494-9949 to learn more. WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic ...
Paragraph Writing on Covid-19 in 100 Words. Coronavirus is an infectious disease and is commonly called Covid-19. It affects the human respiratory system causing difficulty in breathing. It is a contagious disease and has been spreading across the world like wildfire. The virus was first identified in 2019 in Wuhan, China.
For example, 79% of students switching from 3 rd to 4 th grade made academic gains between winter 2019 and fall 2019, relative to 57% of students in the same grade range in 2020.
experienced an average decrease of 11.5 hours of work per week and a 21% decrease in weekly earnings, arnings for 52% of the sample, which again re ects s. variation in the e ects of COVID-19 across students. In terms of labor market expectations, on average, students foresee a 13 percentage points decrease in.
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
A student wearing a protective mask, attends class on the first day of school, amid the coronavirus disease (COVID-19) pandemic, at St. Lawrence Catholic School in North Miami Beach, Florida, U.S ...
The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic. The student suffered from a lack of internet access and other online learning challenges. Students who dealt with problems registering for or taking standardized tests and AP exams. Jeff Schiffman of the Tulane University admissions ...
COVID-19 Coronavirus. Abstract. First appearing in China in late 2019, the novel Coronavirus COVID-19 has become the most significant global pandemic event in a century. As of October 28, 2020 the total number of cases worldwide was 44 million with 1.17 million deaths. The United States has had an extremely politicized response to the virus ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
Here's what Addie Muller from San Jose, Calif., had to say about the Opinion essay "I'm 26. Coronavirus Sent Me to the Hospital": ... I either walked or biked a mile to attend class. I ...
covering mouth and nose with flexed elbow or tissue when coughing or sneezing. Dispose of used tissue immediately; washing hands often with soap and water; and. cleaning frequently touched surfaces and objects. As we learn more about COVID-19 public health officials may recommend additional actions. II.
COVID-19, also called coronavirus disease 2019, is an illness caused by a virus. The virus is called severe acute respiratory syndrome coronavirus 2, or more commonly, SARS-CoV-2. It started spreading at the end of 2019 and became a pandemic disease in 2020. Coronavirus Enlarge image.
Sept. 8, 2020, he fell victim to Covid-19. To many, he's just a statistic — one of the "inevitable" deaths. But to me, he was, and continues to be, an inspiration.
Responding to COVID-19. The advent of COVID-19 forced peer group clinical supervisors to find alternative means of providing peer group clinical supervision sessions which saw the move from face-to-face to online sessions. The online transition was seen as seamless for many established groups while others struggled to deliver sessions.
Y Combinator cofounder Paul Graham generated buzz on Sunday as the startup guru sought to dismantle some conventional wisdom in Silicon Valley about founders running the companies they started.