- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Advances in the...
Advances in the management of chronic kidney disease
- Related content
- Peer review
- Teresa K Chen , assistant professor 1 ,
- Melanie P Hoenig , associate professor 2 ,
- Dorothea Nitsch , professor 3 ,
- Morgan E Grams , professor 4
- 1 Kidney Health Research Collaborative and Division of Nephrology, Department of Medicine, University of California San Francisco; and San Francisco VA Health Care System, San Francisco, CA, USA
- 2 Division of Nephrology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
- 3 Department of Non-Communicable Disease Epidemiology, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, UK
- 4 Department of Medicine, New York University Langone School of Medicine, New York, NY, USA
- Correspondence to: M E Grams Morgan.Grams{at}nyulangone.org
Chronic kidney disease (CKD) represents a global public health crisis, but awareness by patients and providers is poor. Defined as persistent abnormalities in kidney structure or function for more than three months, manifested as either low glomerular filtration rate or presence of a marker of kidney damage such as albuminuria, CKD can be identified through readily available blood and urine tests. Early recognition of CKD is crucial for harnessing major advances in staging, prognosis, and treatment. This review discusses the evidence behind the general principles of CKD management, such as blood pressure and glucose control, renin-angiotensin-aldosterone system blockade, statin therapy, and dietary management. It additionally describes individualized approaches to treatment based on risk of kidney failure and cause of CKD. Finally, it reviews novel classes of kidney protective agents including sodium-glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, non-steroidal selective mineralocorticoid receptor antagonists, and endothelin receptor antagonists. Appropriate, widespread implementation of these highly effective therapies should improve the lives of people with CKD and decrease the worldwide incidence of kidney failure.
Introduction
Chronic kidney disease (CKD) affects approximately 10% of the world’s population and is associated with substantial morbidity and mortality. 1 Risks of kidney failure, acute kidney injury, heart failure, cardiovascular disease, and hospital admissions are all heightened in people with CKD. 2 The Global Burden of Disease Consortium projects that CKD will be in the top five conditions contributing to years of life lost by 2040. 3 However, CKD remains under-recognized by both patients and providers. 1 A diverse entity, CKD is most commonly attributed to diabetes or high blood pressure, but many other causes exist, from genetic causes to adverse effects of drugs to autoimmune processes. 2 In this review, we summarize the evidence for current paradigms of disease identification and classification, discuss new equations developed for estimating glomerular filtration rate (GFR) and harmonizing different measures of albuminuria, report major progress in individualized risk estimation of kidney failure and other adverse outcomes both for CKD in general and within specific disease entities, and describe longstanding and novel treatment strategies. Notable advances have been made in both general and cause specific therapies, including sodium-glucose cotransporter-2 (SGLT-2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, non-steroidal selective mineralocorticoid receptor antagonists (MRA), and endothelin receptor antagonists. Finally, we describe major guidelines in CKD and highlight common themes as well as differences in their recommendations.
Sources and selection criteria
We searched PubMed for peer reviewed articles in the English language from 1 January 2010 to 14 July 2023 using the keywords listed in the web appendix. We additionally reviewed reference lists of selected articles, prioritizing randomized controlled trials, systematic reviews, and meta-analyses when possible but also including observational studies and reviews that were of high quality. We included older articles if we deemed them to be of high importance. Finally, we reviewed guidelines from websites of professional societies and advisory committees (for example, the National Institute for Health and Care Excellence (NICE), Kidney Disease: Improving Global Outcomes (KDIGO), US Centers for Disease Control and Prevention, US Department of Health and Human Services, and International Society of Hypertension).
Epidemiology
CKD is a global public health crisis. Recent estimates suggest that more than 700 million people have CKD, with greater burdens in low income and middle income countries. 1 4 Determining the global, regional, and national burden of disease is challenging owing to inconsistent use of estimating equations for GFR, laboratory assay standardization, and albuminuria testing. Despite this, some important observations can still be made. The prevalence of CKD increases with age and is greatest in people over 70 years. 2 In the US, compared with White people, Black people have substantially higher rates of kidney failure, followed by Native Americans, people of Hispanic ethnicity, and people of Asian descent. 5
The most commonly reported risk factors for CKD are diabetes mellitus and hypertension. 6 7 Social determinants of health are also important and likely contribute to racial disparities in kidney disease. Specific genetic variants increase risk of CKD, including variants in the APOL1 and HBB genes that are present in far greater proportions among people of African ancestry. 8 9 10 11 In Central America, Sri Lanka, Egypt, and Central India, defined geographic areas exist where many cases of CKD of unknown cause have been identified. 12 Some experts postulate that heat stress or pesticides may contribute.
Whereas the incidence of CKD is difficult to estimate, reliant as it is on testing for GFR and albuminuria, the incidence of kidney failure with the receipt of replacement therapy (KFRT) is more readily captured. Many countries have developed national registries of patients with kidney failure, allowing comparison of incidence across ages and countries. 13 For example, the countries with the highest incidence of treated kidney failure in 2020 were Taiwan, the US, and Singapore, whereas the countries with the highest prevalence were Taiwan, the Republic of Korea, and Japan. 5
Definition and classification of CKD: cause, GFR, and albuminuria staging
CKD is defined as persistent abnormalities in kidney structure or function for more than three months, manifest as either low GFR or presence of a marker of kidney damage. 2 Specifically, diagnosis requires one or more of the following: albuminuria, defined as an albumin-to-creatinine ratio (ACR) ≥30 mg per gram of creatinine (approximately ≥3 mg/mmol) or albumin excretion of ≥30 mg/day; GFR <60 mL/min/1.73 m 2 ; abnormalities on urine sediment, histology, or imaging; electrolyte or other abnormalities attributed to tubular disorders; or history of kidney transplantation. The KDIGO heat map helps with understanding of overall risk (low, moderately increased, high, and very high) of patients according to level of albuminuria (A category), level of GFR (G category), and cause of disease ( fig 1 ), such that people with normal estimated GFR but higher albuminuria have a similar risk to people with moderately reduced estimated GFR and no albuminuria.

Kidney Disease: Improving Global Outcomes heat map with guidance on monitoring. 2 Numbers in boxes indicate recommended frequency of monitoring (number of times per year). Colors denote risk as follows: green (low risk), yellow (moderately increased risk), orange (high risk), and red (very high risk). CKD=chronic kidney disease; GFR=glomerular filtration rate
- Download figure
- Open in new tab
- Download powerpoint
Clinical manifestations of CKD
Albuminuria.
Albuminuria is often the first sign of kidney damage, and its detection drives many treatment decisions. 2 The prevalence of albuminuria in people with diabetes or hypertension is estimated to be 32% and 22%, respectively. 14 However, only a minority of patients receive urine screening tests. 14 15 For example, the mean albuminuria screening rates across health systems in the US were 35% among adults with diabetes and 4% among adults with hypertension. 14
The gold standard for assessing albuminuria is either a sample collected mid-stream from an early morning urine void or a 24 hour urine collection; however, in situations where this is not possible, a spot collection is reasonable. 2 Quantification of albumin is preferred over that of total protein. 2 16 This preference is because the sensitivity of the total protein assay to different protein components can vary by laboratory, as well as the fact that proteinuria assessments do not easily discriminate A1 and A2 categories. Both urine albumin and urine protein are typically indexed to urine creatinine to account for differences in dilution, as urine ACR or urine protein-to-creatinine ratio (PCR). Dipstick protein assessment is generally more economical than both methods; however, like PCR, dipstick assessment can be insensitive in A1 and A2 categories. Although conversion calculators exist to aid in the harmonization of ACR and PCR measures; they do not work well at lower ranges of albuminuria. 17 18
The second axis for CKD classification focuses on GFR. 2 The gold standard for assessing GFR is direct measurement from clearance of an exogenous filtration marker such as iohexol or iothalamate; however, this is relatively cumbersome and rarely done in clinical practice. Instead, GFR is usually estimated by using plasma or serum concentrations of endogenous filtration markers, such as creatinine and cystatin C, and demographic variables. Early equations for adults, such as Modification of Diet in Renal Disease (MDRD) and CKD Epidemiology Collaboration (CKD-EPI) 2009 equations, used filtration markers along with age, sex, and race (Black versus non-Black) to estimate GFR. 19 20 21 The newer European Kidney Function Consortium equation, which allows for seamless GFR evaluation from infancy to old age, uses a population specific divisor to adjust creatinine values (for example, separate values for Black European and White European populations). 22 However, the use of race in GFR estimation has faced strong criticism and, in 2021, the US based American Society of Nephrology-National Kidney Foundation Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease recommended immediate adoption of the race-free CKD-EPI 2021 estimating equations, which exist for creatinine alone (eGFRcr) as well as for creatinine and cystatin C (eGFRcr-cys). 23 24 25 Cystatin C has distinct confounders (non-GFR determinants) of its relation with GFR compared with creatinine ( fig 2 ). 2 26 Thus, eGFRcr-cys is a more accurate estimate of GFR than eGFRcr alone, irrespective of equation used, in most scenarios, including those in which large differences exist between eGFRcr and that estimated solely using cystatin C (eGFRcys). 25 27 28 However, the newest GFR estimating equations have not been tested extensively in Asian populations. 29 30

Common non-glomerular filtration rate (GFR) determinants of blood concentrations of creatinine and cystatin C. 2 26 eGFR=estimated glomerular filtration rate
The third axis for classification is cause of CKD, which is generally ascertained through imaging, assessment of extrarenal manifestations and biomarkers, or kidney biopsy. 2 Classification of cause typically hinges on the presence or absence of systemic disease (for example, obesity, diabetes, hypertension, systemic autoimmune disease) and the specific location of the kidney pathology (for example, glomeruli, tubulointerstitium, vasculature, or cystic/congenital abnormality). Unfortunately, the cause of CKD is often unknown, limiting its utility. Molecular phenotyping and genetic testing are increasingly being used to assign cause of disease. Targeted gene panels offered commercially may have high diagnostic yields in select populations, such as patients with glomerular disease, nephrotic syndrome, or congenital anomalies of the kidney and urinary tract. 31 One study suggested that for appropriately selected patients, 34% had disease either reclassified or assigned on the basis of genetic testing, thus changing clinical management. 32 The European Renal Association and the European Rare Kidney Disease Reference Network have issued a joint statement providing recommendations for how to provide genetic testing, including specific settings in which it may be considered ( box 1 ). 33
European Renal Association and European Rare Kidney Disease Reference Network recommendations for settings in which genetic testing might be considered 33
Most tubulopathies
Glomerulopathies:
Congenital nephrotic syndrome
Nephrotic syndrome refractory to standard steroid therapy
Multi-organ phenotypes suggestive of syndromic steroid resistant nephrotic syndrome
Complement disorders:
Immune complex mediated membranoproliferative glomerulonephritis
C3 glomerulopathy
Atypical hemolytic uremic syndrome
Renal ciliopathies
Congenital anomalies of the kidney and urinary tract
Patients aged <50 years with severe CKD of unknown cause
Patients aged >50 years with adult onset CKD and family history of CKD
CKD=chronic kidney disease
Individualized prognosis and treatment
Identifying the cause of CKD is critical as different causes of CKD carry different prognoses and can have distinct treatments. 2 For example, autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic cause of CKD and is typically associated with faster progression than other disease entities. 32 34 Individualized prognosis is often determined by using disease specific risk classification or calculators (for example, the Mayo classification or the ADPKD Prognostic Tool), and screening and treatment recommendations such as increased fluid intake and tolvaptan are unique to this entity. 35 36 37 38 IgA nephropathy, the most common type of glomerulonephritis worldwide, particularly in East Asian and Pacific Asian countries, 39 has its own prognostic aids, such as the International IgA Nephropathy Prediction Tool, 40 41 and treatments specific to IgA nephropathy are in various stages of development. 42 The APOL1 high risk genotypes confer about twofold higher risk of kidney failure in the general population and are common in people of African ancestry. 8 43 44 45 A recently published phase 2A study of targeted therapy for APOL1 related disease showed promising reductions in albuminuria; the phase 3 study is ongoing. 46 Other disease specific therapies are increasingly available, such as belimumab in lupus nephritis and lumasiran for primary hyperoxaluria type 1. 47 48
Individualized risk prediction is also available for more general populations of patients with CKD. The most widely known and validated is the kidney failure risk equation (KFRE), which is used in patients with GFR <60 mL/min/1.73 m 2 . 49 Tested in more than 30 countries and 700 000 people, the tool provides probabilities of kidney failure at two years and five years based on age, sex, and estimated GFR and albuminuria levels. 50 Like all risk equations, the KFRE may perform better with recalibration to absolute risk levels of local populations, but the discriminatory ability (that is, distinguishing people at high risk from those at low risk) has been extremely consistent across all studies. The KFRE has also been validated in recipients of kidney transplants. 51 52 Although the KFRE does not explicitly take into account the competing risk of death, estimates are quite accurate except among the members of the oldest segments of the population at the highest risk. 53 One study suggested that the KFRE provides more accurate prediction of kidney failure than both patients and providers. 54 Even within categories of GFR and urine ACR, the KFRE provides a wide estimate of risk prediction, which can be helpful in the counseling and referral of patients ( fig 3 ). Some centers will refer patients with a two year risk of kidney failure greater than 20-40% for vascular access and kidney transplantation evaluation, on the basis that tools that incorporate albuminuria provide more accurate and unbiased time to kidney failure than does estimated GFR alone. 55 Studies suggest that the KFRE is robust to different GFR equations (specifically, CKD-EPI 2009 and CKD-EPI 2021) and that many patients value being counseled using this information. 53 56

Range of predicted risk of kidney failure using the kidney failure risk equation (KFRE) within G and A categories of chronic kidney disease (CKD). The KFRE ( ckdpcrisk.org/kidneyfailurerisk ) was used to estimate two year risk of kidney failure in 350 232 patients with estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m 2 from the Optum Laboratories Data Warehouse (OLDW). OLDW is a longitudinal, real world data asset with deidentified administrative claims and electronic health record data. Patients with eGFR and albuminuria (urine albumin-to-creatinine ratio (ACR), protein-to-creatinine ratio, or dipstick protein) within a two year window were included in this analysis. Different measures of albuminuria were harmonized to ACR levels for A categories ( ckdpcrisk.org/pcr2acr )
Other risk equations exist to predict the risk of cardiovascular disease and death in CKD; some of these do consider the competing risk of death ( www.ckdpcrisk.org ). For example, the advanced CKD risk tool provides simultaneous estimates of kidney failure, cardiovascular disease, and death for patients with estimated GFR <30 mL/min/1.73 m 2 , which can inform decisions on access placement and reinforce the importance of cardiovascular risk reduction. 57 Estimating risks of cardiovascular disease is particularly relevant given that many more patients with CKD have cardiovascular disease events than need KFRT. 58 Other efforts incorporate estimated GFR and albuminuria into existing tools, such as SCORE2 and the pooled cohort equation for the prediction of cardiovascular disease. 59 60
Patient specific prognostic clues may stem from discrepant estimated GFR values between eGFRcr and eGFRcys. 61 62 63 When eGFRcys is substantially lower than eGFRcr, the risk for kidney related laboratory abnormalities (for example, anemia, hyperuricemia, and hyperphosphatemia) and subsequent adverse outcomes (for example, kidney failure, heart failure, and mortality) is higher. 61 64 65 By contrast, having a lower eGFRcr than eGFRcys is associated with lower risk of adverse outcomes. 66 Risk factors for having a discrepancy between eGFRcr and eGFRcys include older age, female sex, higher body mass index, recent weight loss, and smoking.
General principles of management
The mainstays of therapy for patients with CKD include treating the underlying cause if known, and correcting risk factors (for example, albuminuria) for CKD progression and other CKD related complications ( fig 4 ). 2

Comprehensive care of patients with chronic kidney disease (CKD), irrespective of cause
Blood pressure targets
The three major studies for evaluating the optimal blood pressure target in CKD were the Modification of Diet in Renal Disease Study (MDRD), African American Study of Kidney Disease and Hypertension (AASK), and Systolic Blood Pressure Intervention Trial (SPRINT). 67 68 69 In both MDRD and AASK, intensive blood pressure control did not slow GFR decline overall. 67 68 However, in MDRD, participants with baseline proteinuria of ≥3 g/day seemed to benefit from intensive blood pressure control, with slower mean rates of GFR decline compared with their counterparts in the usual blood pressure control group. 67 Among SPRINT participants with baseline CKD (n=2646), aiming for a systolic blood pressure goal of <120 mm Hg versus <140 mm Hg did not significantly reduce the risk for a composite kidney outcome that included a ≥50% reduction in estimated GFR, long term dialysis, or kidney transplant. 69 70 However, benefits of intensive blood pressure control were seen with respect to prevention of the composite cardiovascular outcome (defined as myocardial infarction, acute coronary syndrome, stroke, heart failure, or death from cardiovascular causes—hazard ratio 0.75, 95% confidence interval 0.64 to 0.89) and all cause mortality (hazard ratio 0.73, 0.60 to 0.90), regardless of CKD status. 69 Blood pressure control can also reduce albuminuria, as shown in the Chlorthalidone in Chronic Kidney Disease (CLICK) trial of chlorthalidone in advanced CKD. 71
Glycemic targets
Among patients with diabetes and CKD, glycemic control is an important component of comprehensive care. 72 The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) was the largest trial of intensive glucose control to enroll patients with CKD. 73 Among the 11 140 trial participants, 19% had an estimated GFR <60 mL/min/1.73 m 2 and 31% had albuminuria at baseline. 74 Compared with standard glucose control, intensive glucose control was associated with 9% (hazard ratio 0.91, 0.85 to 0.98), 30% (0.70, 0.57 to 0.85), and 65% (0.35, 0.15 to 0.83) lower risks of developing new onset ACR 30-300 mg/g, ACR >300 mg/g, and end stage kidney disease (ESKD), respectively.
Specific classes of therapy
Angiotensin converting enzyme inhibitors and angiotensin receptor blockers.
When choosing antihypertensive agents, those that act by inhibiting the renin-angiotensin-aldosterone system (RAAS) have particular relevance in CKD. A 2001 meta-analysis of 11 studies suggested that, for non-diabetic CKD, the use of angiotensin converting enzyme (ACE) inhibitors resulted in a 30% reduction in risk of KFRT or doubling of serum creatinine. 75 Clinical trials in populations with CKD and diabetes (for example, IDNT, RENAAL) have also shown benefit of angiotensin receptor blockers (ARB) in preventing CKD progression ( table 1 ). 77 78 RAAS inhibition also plays a role in prevention of cardiovascular disease. The Heart Outcomes Prevention Evaluation (HOPE) study showed that ACE inhibitors reduced the risks of myocardial infarction, stroke, and cardiovascular death in populations at high risk for cardiovascular disease, including those with diabetes and albuminuria. 80 The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) showed that ACE inhibitors and ARB were generally equivalent in the prevention of cardiovascular events. 81 Because of the increased risk of hyperkalemia and acute kidney injury, dual therapy with both an ACE inhibitor and an ARB is typically avoided. 82
Landmark randomized clinical trials on angiotensin converting enzyme inhibitors or angiotensin receptor blockers in chronic kidney disease
- View inline
When GFR declines, providers often grapple with whether RAAS inhibitors should be continued. The Benazepril in Advanced CKD study showed that benazepril reduced the risk of the primary composite kidney endpoint by 43% compared with placebo, thus suggesting that RAAS inhibitors are beneficial even in advanced CKD (baseline serum creatinine 3.1-5.0 mg/dL). 79 Three recent reports further explored this question, also examining the benefits in prevention of death and cardiovascular events associated with continuation of RAAS inhibitors. 83 84 85 A retrospective, propensity score matched study of patients with estimated GFR <30 mL/min/1.73 m 2 showed higher risk of all cause mortality and major adverse cardiovascular events in those who stopped RAAS inhibitors compared with those who continued them, 83 as did a Swedish trial emulation study. 84 The risk of kidney replacement therapy associated with cessation of RAAS inhibitors was not statistically significant in the first study and lower in the second study. 83 84 In an open label randomized trial, cessation of RAAS inhibitors did not show significant between group differences in long term decline in estimated GFR or initiation of kidney replacement therapy, providing reassurance that RAAS inhibitors can be safely continued as GFR declines. 85
SGLT-2 inhibitors
One of the biggest advancements in CKD management over the past decade was the discovery that SGLT-2 inhibitors have robust protective effects on the heart and kidneys in patients with and without diabetes. Recent trials showed an approximate 30% reduction in risk for diverse kidney outcomes among patients with baseline estimated GFR values as low as 20 mL/min/1.73 m 2 ( table 2 ). 86 88 89 91 Importantly, the three trials designed with primary kidney outcomes (Canagliflozin and Renal Events in Diabetes and Established Nephropathy Clinical Evaluation (CREDENCE), Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD), and Study of Heart and Kidney Protection with Empagliflozin (EMPA-KIDNEY)) were terminated early because pre-specified efficacy criteria were met, with median follow-up times ranging from 2.0 to 2.6 years. 88 89 91 The overwhelming majority of trial participants were taking an ACE inhibitor or ARB before randomization, showing that the benefits of SGLT-2 inhibitors on slowing CKD progression are additive to those of RAAS inhibitors. One simulation study estimated that a 50 year old adult with non-diabetic albuminuric CKD would have seven extra years free from doubling of serum creatinine, kidney failure, or all cause mortality if treated with an SGLT-2 inhibitor and RAAS inhibitor. 92
Landmark randomized clinical trials on sodium-glucose co-transporter 2 inhibitors in chronic kidney disease (CKD)
Subgroup analyses of the DAPA-CKD and EMPA-KIDNEY trials have provided additional insights on the wide range of patients who are likely to benefit from SGLT-2 inhibitors. 89 91 In DAPA-CKD, dapagliflozin was favored over placebo in all pre-specified subgroups by baseline age, sex, race, diabetes status, systolic blood pressure, estimated GFR (<45 v ≥45 mL/min/1.73 m 2 ), and ACR (≤1000 v >1000 mg/g or ≤113 v >113 mg/mmol). 89 Similarly, in EMPA-KIDNEY, empagliflozin was associated with lower risk of the primary composite outcome compared with placebo regardless of baseline diabetes status or estimated GFR (<30 v ≥30 mL/min/1.73 m 2 to <45 v ≥45 mL/min/1.73 m 2 ). 91 The risk of the primary outcome was not lower among patients with ACR ≤300 mg/g (approximately ≤30 mg/mmol). In exploratory analyses, however, empagliflozin was associated with slower annual rates of decline in estimated GFR compared with placebo among participants with ACR between 30 and 300 mg/g (approximately 3-30 mg/mmol) and slower chronic slope (from two months to the final follow-up visit) among all ACR subgroups.
The DAPA-CKD trial also showed that the kidney protective effects of SGLT-2 inhibitors extend to patients with IgA nephropathy and perhaps also those with focal segmental glomerulosclerosis (FSGS). 93 94 Among 270 participants with IgA nephropathy (mean estimated GFR 44 mL/min/1.73 m 2 ; median ACR 900 mg/g (102 mg/mmol)), dapagliflozin was associated with a 71% lower risk of developing the primary outcome and a 70% lower risk of ESKD compared with placebo. 93 Among the 104 participants with FSGS (mean estimated GFR 42 mL/min/1.73 m 2 ; median ACR 1248 mg/g (141 mg/mmol)), dapagliflozin was not associated with a lower risk of the primary composite outcome, although this analysis was limited in power (only 11 events). 94 In exploratory analyses, dapagliflozin was associated with slower chronic decline in estimated GFR in the FSGS population. Investigations on the use of SGLT-2 inhibitors in other patient populations, such as those with polycystic kidney disease and kidney transplant recipients, are ongoing (clinicaltrials.gov).
SGLT-2 inhibitors, which act at the level of the proximal tubule to block the reabsorption of glucose and sodium, 95 are generally safe to use in patients with CKD. Early signals of heightened risks of volume depletion, serious genital infections, bone fractures, and need for limb amputation in the Canagliflozin Cardiovascular Assessment Study (CANVAS) were not observed in subsequent studies—CREDENCE, DAPA-CKD, and EMPA-KIDNEY—thus assuaging these concerns ( table 3 ). 86 88 89 91 A pooled analysis of 15 081 participants with type 2 diabetes and CKD G3-4 showed similar rates of serious adverse events for empagliflozin versus placebo, with a higher rate only of mild genital infections with the SGLT-2 inhibitor. 96 A real world study of patients receiving SGLT-2 inhibitors compared with dipeptidyl peptidase-4 (DPP-4) inhibitors found no increased risk of outpatient urinary tract infections or severe urinary tract infection events requiring hospital admission. 97
Adverse effects of SGLT-2 inhibitors * in CANVAS, CREDENCE, DAPA-CKD, and EMPA-KIDNEY trials
GLP-1 receptor agonists
GLP-1 receptor agonists have also been shown to improve kidney outcomes among patients with type 2 diabetes, albeit in trials that were designed for primary cardiac outcomes ( table 4 ). 98 99 100 101 102 103 104 105 106 107 108 109 The reduction in risk of kidney outcomes, which included albuminuria, ranged from 15% to 36%. A large meta-analysis of approximately 44 000 participants from the six trials in table 4 reported that use of GLP-1 receptor agonists was associated with a 21% lower risk of developing the composite kidney outcome, defined as new onset albuminuria >300 mg/g, doubling of serum creatinine, ≥40% decline in estimated GFR, kidney replacement therapy, or death due to kidney causes, compared with placebo. 100 This risk reduction seemed to be driven by the reduction in incident albuminuria >300 mg/g; associations between GLP-1 receptor agonists and CKD progression and kidney failure were not statistically significant. However, results were more promising in A Study Comparing Dulaglutide with Insulin Glargine on Glycemic Control in Participants with Type 2 Diabetes and Moderate or Severe Chronic Kidney Disease (AWARD-7), a clinical trial designed to evaluate change in glycated hemoglobin. 110 Among 577 adults with type 2 diabetes and CKD G3-4 randomized to open label dulaglutide 1.5 mg once weekly, dulaglutide 0.75 mg once weekly, or insulin glargine daily, both dulaglutide groups had slower estimated GFR declines compared with the insulin glargine group; among participants with baseline albuminuria >300 mg/g, dulaglutide was associated with greater ACR reductions in a dose dependent manner over the one year follow-up.
Landmark randomized clinical trials on associations of glucagon-like peptide-1 (GLP-1) receptor agonists with secondary kidney outcomes among patients with type 2 diabetes mellitus
Exact mechanisms by which the GLP-1 receptor agonists slow decline in estimated GFR and/or reduce albuminuria are not entirely clear, but proposed mechanisms include improved glycemic control, weight loss, increased natriuresis, and reduced inflammation and oxidative stress. 111 112 113 Adverse effects observed with this class of drugs have included diarrhea, nausea, and vomiting. 103 104 107 109 110
Mineralocorticoid receptor antagonists
Several MRAs are available and can be useful adjuncts to RAAS inhibitors, particularly among populations with albuminuria and/or diabetes. Two common steroidal non-selective MRAs, spironolactone and eplerenone, both lower albuminuria. 72 In a meta-analysis of 372 participants from seven trials, combination therapy with a non-selective MRA and an ACE inhibitor and/or ARB was associated with a significant reduction in proteinuria, albeit with a higher risk of hyperkalemia. 114 Finerenone, a non-steroidal selective MRA, was also recently approved. 115 Compared with the steroidal non-selective MRAs, finerenone has a stronger selectivity for the mineralocorticoid receptor, a shorter half life, less of a blood pressure lowering effect, and a more favorable side effect profile, as well as potentially greater anti-inflammatory and antifibrotic effects. 115 116 117 The Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease (FIDELIO-DKD) trial and the Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease (FIGARO-DKD) trial were two complementary phase 3 clinical trials designed to investigate the kidney and cardiovascular benefits of finerenone, respectively, in people with albuminuria levels ≥30 mg/g and type 2 diabetes ( table 5 ). 116 118 Both trials included patients taking maximally tolerated ACE inhibitor or ARB, with participants in FIDELIO-DKD generally having more severe baseline CKD. In a pooled analysis of the two trials, finerenone was associated with a 15-23% lower risk of developing the kidney composite outcomes and a 32% lower mean change in ACR from baseline to four months. 119 Hyperkalemia was more frequent among patients randomized to finerenone (14%) compared with placebo (7%). In pre-specified analyses, baseline SGLT-2 inhibitor use (n=877) or GLP-1 receptor agonist use (n=944) did not modify the beneficial effect of finerenone on the kidney composite outcome, thus suggesting a potential role for dual therapy (for example, finerenone plus SGLT-2 inhibitor or GLP-1 receptor agonist) among patients with type 2 diabetes and CKD.
Landmark randomized clinical trials on finerenone in chronic kidney disease
Endothelin receptor antagonists
Endothelin receptor antagonists have emerged as novel treatments for a variety of kidney diseases. The Study of Diabetic Nephropathy with Atrasentan (SONAR) evaluated the effect of atrasentan on a composite kidney outcome (defined as a doubling of serum creatinine or ESKD) among adults with type 2 diabetes, estimated GFR 25-75 mL/min/1.73 m 2 , and urine ACR 300-5000 mg/g taking a stable dose of ACE inhibitor or ARB. 120 After a six week enrichment period during which all participants received atrasentan 0.75 mg daily (n=5517), those who responded (defined as a ≥30% reduction in urine ACR without the development of substantial fluid retention or increase in serum creatinine by >0.5 mg/dL and 20% from baseline; n=2648) were randomized to receive atrasentan or placebo. Over a median follow-up of 2.2 years, the atrasentan group had a 35% lower risk of developing the composite kidney outcome compared with the placebo group, although fluid retention and anemia were more frequent in the former. Of note, the frequency of hyperkalemia was low (1%) in both treatment groups. Sparsentan, a dual endothelin and angiotensin II receptor antagonist, is also being investigated as a treatment for FSGS and IgA nephropathy. 121 122 In a phase 2, randomized, double blind, active control trial, 109 adults with biopsy proven FSGS (estimated GFR >30 mL/min/1.73 m 2 and urine PCR ≥1 g/g) received varying doses of sparsentan (200, 400, or 800 mg daily) or irbesartan 300 mg daily. 121 At eight weeks, participants receiving sparsentan had greater reductions in urine PCR compared with those receiving irbesartan. In an interim analysis of the PROTECT phase 3 trial, adults with biopsy proven IgA nephropathy (urine PCR ≥1 g/day) randomized to sparsentan 400 mg daily had a 41% greater reduction in urine PCR over 36 weeks and threefold higher odds of achieving complete remission of proteinuria at any point compared with their counterparts who were randomized to irbesartan 300 mg daily. 122 Based in part on the results of this study, the US Food and Drug Administration (FDA) granted accelerated approval for the use of this drug in adults with primary IgA nephropathy considered to be at risk of rapid disease progression. 123
Endothelin 1 has been implicated in the pathogenesis of kidney disease via various mechanisms including vasoconstriction, vascular hypertrophy, endothelial and podocyte injury, inflammation, cell proliferation, extracellular matrix accumulation, and fibrosis. 124 Systemic and local kidney production of endothelin 1 is augmented in CKD.
Other nephroprotective and cardiovascular risk reduction strategies
A bidirectional association exists between CKD and cardiovascular disease: cardiovascular disease is both a risk factor for CKD and a common outcome in patients with CKD. 125 126 Thus, patients with CKD are likely to benefit from efforts at cardiovascular risk reduction including administration of a statin as well as the gamut of lifestyle changes. 2 127
Lipid management
The Study of Heart and Renal Protection (SHARP) trial evaluated the efficacy of ezetimibe and simvastatin combination therapy in patients with moderate to severe CKD (33% on dialysis; 67% not on dialysis with mean estimated GFR of 27 mL/min/1.73 m 2 ). 128 Treatment with these low density lipoprotein (LDL) cholesterol lowering agents led to a 17% risk reduction for development of a first major atherosclerotic event compared with placebo, although this benefit was seen only in the patients not requiring maintenance dialysis. Those at very high risk (for example, with previous major atherosclerotic cardiovascular disease events) may benefit from additional therapies to lower LDL cholesterol, including evolocumab. 129 Evolocumab is a monoclonal antibody for proprotein convertase subtilisin/kexin type 9, which increases LDL cholesterol receptors and hence clearance of LDL; this novel therapy also seems to be safe and efficacious in patients with CKD. 129 130
Physical activity
Exercise has been shown to benefit patients with CKD. Several small, randomized trials have reported that exercise training programs in patients with moderate to severe CKD are safe, feasible, and effective in improving physical activity levels, cardiorespiratory fitness, and quality of life. 131 132 133 134 135 Whether these interventions also slow CKD progression remains to be determined, as many of these studies were underpowered for this outcome.
For patients with obesity, weight loss may reduce the risk of CKD progression, whether it comes from intensive lifestyle intervention such as in the Look AHEAD (Action for Health in Diabetes) trial or, as in observational studies, from bariatric surgery. 136 137 138 Micronutrient and macronutrient composition of diets may also matter. 139
Traditional recommendations about diet in the setting of CKD have focused on limiting protein and dietary acid intake. Experimental evidence suggests that protein intake can increase intraglomerular pressure and cause glomerular hyperfiltration. 140 141 142 Observational data from large cohort studies suggest that the type of protein may be important; a diet high in animal protein may increase risk, whereas protein from plant sources may be better tolerated. 143 144 For example, an observational study in Singapore found a strong correlation between red meat intake and risk of ESKD. 145 Little clinical trial evidence for protein restriction exists. The MDRD study randomized patients to different levels of protein restriction but found no statistically significant difference in the rate of GFR decline. 67
A second line of investigation has been into the benefits of increasing nutritional alkali intake, with a body of open label trials suggesting benefits on kidney function and prevention of starting dialysis. 146 A phase 3 double blinded, placebo controlled trial reported that veverimer (a potent acid binder that acts in the intestine) was effective in raising or normalizing serum bicarbonate among patients with CKD and chronic metabolic acidosis. 147 Other double blinded studies using veverimer suggested that treating acidosis in CKD improves quality of life and overall physical function. 148 However, a recent trial evaluating veverimer in slowing progression of CKD was negative. 149
Although patients with CKD are prone to hyperkalemia, potassium intake has a beneficial effect on blood pressure, cardiovascular disease, and death independent of and opposite to that of sodium intake. 150 151 152 153 One large randomized controlled trial suggested that substituting 25% of sodium chloride intake with potassium chloride reduced the risk of major adverse cardiovascular events by 13% in the general population. 154 Similarly, small studies suggest that diets rich in potassium may be beneficial in CKD. A feeding trial in people with CKD G3 observed that 100 mmol compared with 40 mmol of dietary potassium per day increased serum potassium by 0.21 mmol/L, 155 similar to the increase seen with finerenone. 156 Many dietary studies have evaluated patterns of diet rather than potassium alone: for example, plant based diets tend to be rich in not only potassium but also alkali and fiber. Observational data from prospective cohorts suggest that plant based diets are associated with less CKD progression. 143 157 158 Evidence is also emerging to suggest that increasing fiber intake benefits the gut microbiome, decreases inflammation, and possibly slows CKD progression. 159
Appropriate drug dosing and nephrotoxin avoidance
An important component of care for patients with CKD is avoidance of additional insults. Many drugs are cleared by glomerular filtration or tubular secretion by the kidney, and reduced GFR can lead to accumulation of the drug or its metabolites resulting in adverse effects. 160 Careful estimation of GFR is generally a first step in determining dosage for renally excreted drugs. 161 The US FDA guidance to industry suggests that estimated GFR based on serum creatinine may be used in pharmacokinetic studies. 162 If drugs are dosed on the basis of estimated GFR (rather than estimated creatinine clearance from the Cockcroft-Gault equation, an equation that is known to be flawed), estimated GFR must be “de-indexed” by multiplying the standardized estimated GFR by the individual’s calculated body surface area and dividing by 1.73 m 2 . 163 164 165 This is because drug clearance is thought to be proportional to a person’s GFR and not the GFR standardized to body surface area. Antibiotics and antiviral agents, direct oral anticoagulants, drugs for diabetes mellitus, and chemotherapeutic agents are the most common drugs that require attention to dosing in CKD. 2 160 164
Some drugs should be avoided or minimized in CKD because of their potential to worsen kidney function. For example, non-steroidal anti-inflammatory drugs (NSAIDs) can exacerbate hypertension, cause fluid retention, and contribute to the risk of acute kidney injury. 166 Particularly when used with RAAS inhibitors and diuretics, NSAIDs are ideally avoided. 167 In select patients with CKD, however, some clinicians will prescribe an abbreviated course of NSAIDs given that the most common alternative, opioids, also have significant adverse effects. 168 Proton pump inhibitors can lead to acute or chronic interstitial nephritis and have been associated with incident CKD, progression of CKD, and ESKD. 169 170 Although the mechanism by which proton pump inhibitors contribute to CKD remains unclear, most experts agree that these agents should be used judiciously.
Emerging treatments
Many phase 3-4 clinical trials are ongoing to evaluate emerging treatments for kidney disease (clinicaltrials.gov). These include, but are not limited to, investigations on the use of dapagliflozin in advanced CKD (for example, estimated GFR <25 mL/min/1.73 m 2 , on maintenance dialysis with residual daily urine output of >500 mL, and kidney transplant recipients with estimated GFR ≤45 mL/min/1.73 m 2 ; NCT05374291 ); finerenone in non-diabetic CKD ( NCT05047263 ); and monteluklast ( NCT05362474 ) and pentoxyifylline ( NCT03625648 ) in diabetic CKD. Several therapies are also being tested for rarer causes of kidney disease: obinutuzumab ( NCT04629248 ), zanubrutinib ( NCT05707377 ), and SNP-ACTH (1-39) gel ( NCT05696613 ) in membranous nephropathy; voclosporin ( NCT05288855 ), atacicept ( NCT05609812 ), anifrolumab ( NCT05138133 ), inanalumab ( NCT05126277 ), secukinumab ( NCT04181762 ), obinutuzumab ( NCT04221477 ), and ACTHar gel ( NCT02226341 ) in lupus nephritis; VX-147 in APOL1 related kidney disease ( NCT05312879 ); imlifidase in antiglomerular basement membrane disease ( NCT05679401 ); sparsentan in focal segmental glomerulosclerosis ( NCT03493685 ); and pegcetacoplan ( NCT05067127 ) in immune complex glomerulonephritis. IgA nephropathy, in particular, is an area of high interest, as recent work suggests that disease activity may be driven by the overproduction of galactose deficient IgA antibodies that are recognized as autoantigens, triggering glomerular deposition of immune complexes. 171 Monoclonal antibodies to signaling molecules that enhance IgA production are in phase 3 trials, as are immunosuppressive and non-immunosuppressive agents (for example, those acting on the endothelin-1 and angiotensin II pathways): budesonide ( NCT03643965 ), sparsentan ( NCT03762850 ), atrasentan ( NCT04573478 ), LNP023 ( NCT04578834 ), RO7434656 ( NCT05797610 ), atacicept ( NCT04716231 ), and sibeprenlimab ( NCT05248646 ; NCT05248659 ).
Major guidelines in CKD are issued by the international KDIGO group ( https://kdigo.org/ ), and locally in the UK by NICE ( www.nice.org.uk/guidance/ng28/chapter/Recommendations#chronic-kidney-disease ), with the most recent issuances primarily from 2023 (currently in public review) and 2021, respectively. KDIGO publishes guidelines on the evaluation and management of patients with CKD in general, as well as myriad other aspects (for example, diabetes, blood pressure, lipids, anemia, mineral and bone disease, hepatitis C, ADPKD, glomerular diseases). With the expansion of therapeutic options, both organizations are updating recommendations frequently. Other guideline producing organizations such as the American College of Cardiology, the American Heart Association, the European Society of Cardiology, the European Society of Hypertension, the International Society of Hypertension, and the American Diabetes Association (ADA) provide more limited statements of recommendation for the specific aspects of the management of patients with CKD. 172 173 174 175
Annual screening for CKD (including testing for albuminuria) is widely recommended in people with diabetes. 72 174 175 176 177 Guidelines in hypertension are less clear. 178 The 2020 Global Hypertension Practice Guideline from the International Society of Hypertension is a notable exception and now recommends routine assessment of albuminuria in addition to estimated GFR in people with hypertension. 173 KDIGO and NICE also recommend testing anyone who is at risk for CKD, which includes those with hypertension, cardiovascular disease, diabetes, and previous acute kidney injury, along with multiple other, less common conditions. 179 For CKD, the KDIGO guidelines recommend at least annual albuminuria testing with greater frequency in higher risk categories ( fig 1 ). 2 The NICE guidelines, on the other hand, recommend annual ACR testing with individualization based on clinical characteristics, risk of progression, and whether a change in ACR would lead to a change in management. 16
KDIGO guidelines and those from NICE differ slightly on staging CKD. KDIGO recommends using a validated equation for GFR estimation and suggests that using “race as a distinct variable in the computation of GFR” is not appropriate. 179 NICE recommends using the CKD-EPI 2009 equation, which did include race, but using the computed value for non-Black people for everyone, a position that is also endorsed by other European groups. 16 180 181 The KDIGO guidelines recommend staging CKD by eGFRcr-cys when cystatin C is available, as well as when precise estimates of GFR are needed for clinical decision making. 2 179 The NICE guidelines recommend direct measurement of GFR rather than the use of cystatin C in clinical situations requiring additional precision. 16
Both KDIGO and NICE emphasize the importance of risk assessment in patients with CKD. The NICE guidelines suggest that primary care providers should counsel patients using the KFRE five year risk estimate, with referral to a specialist if risk is greater than 5%. 16 KDIGO 2023 additionally suggests that the two year risk estimate can drive referral for multidisciplinary care (>10%) and preparation for kidney replacement therapy, including vascular access planning and referral for transplantation (>40%). 179 The KDIGO 2023 guidelines also emphasize the importance of cardiovascular risk assessment using equations developed in people with CKD or that encompasses estimated GFR and albuminuria and the use of disease specific tools in IgA nephropathy and ADPKD. 179
Multiple guidelines comment on target blood pressures in the setting of CKD. The NICE guidelines recommend a target of <140/90 mm Hg, or <130/80 mm Hg if ACR is ≥70 mg/mmol (approximately 700 mg/g). 16 Guidelines from the American College of Cardiology, American Heart Association, European Society of Cardiology, and European Society of Hypertension recommend a systolic blood pressure target of <130 mm Hg as a best practice target, with the European Society of Cardiology and European Society of Hypertension specifically advising against lower targets. 172 The KDIGO guidelines on hypertension in CKD advocate for a systolic blood pressure goal of <120 mm Hg, as assessed using standardized office measurements. 182 This recommendation is based largely on data from SPRINT and the observed benefits in cardiovascular endpoints and survival rather than benefits in kidney endpoints. 70
Of note, disparate guideline recommendations may reflect different emphasis on standardized blood pressure measurement techniques, which can result in measured blood pressure that is substantially lower than measurement in an uncontrolled setting. 183 Joint statements from several international groups including KDIGO stress the importance of proper technique when assessing blood pressure. 184 Both NICE and KDIGO recommend RAAS inhibitors (either ACE inhibitor or ARB) as first line antihypertensive treatment for people without diabetes but with albuminuria (NICE: urine ACR >70 mg/mmol; KDIGO: A3) as well as those with diabetes and CKD G1-G4, A2-A3. 16 182 KDIGO 2023 suggests continuation of RAAS inhibitors even when estimated GFR is <30 mL/min/1.73 m 2 . 179
For patients with diabetes and CKD not treated with dialysis, KDIGO recommends a hemoglobin A 1c target ranging from <6.5% to <8%. 72 NICE does not provide specific recommendations for people with CKD, instead emphasizing shared decision making but a general goal of hemoglobin A 1c <7% for people with diabetes treated with drugs associated with hypoglycemia and <6.5% for people with diabetes managed by lifestyle or a single drug not associated with hypoglycemia. 185
KDIGO and ADA guidelines recommend SGLT-2 inhibitors as first line drug therapy for all people with type 2 diabetes, CKD, and an estimated GFR ≥20 mL/min/1.73 m 2 ( fig 5 ). 72 174 175 179 The NICE guidelines recommend that an SGLT-2 inhibitor should be offered when ACR is >30 mg/mmol (approximately >300 mg/g) and considered when ACR is between 3 and 30 mg/mmol (approximately 30 to 300 mg/g) in patients with type 2 diabetes and CKD who are already taking an ACE inhibitor or ARB and meet estimated GFR thresholds. 185 The NICE guidelines further specify that dapagliflozin should also be considered in people with estimated GFR 25-75 mL/min/1.73 m 2 and ACR ≥22.6 mg/mmol (approximately 200 mg/g) regardless of diabetes status 186 ; KDIGO is broader and recommends SGLT-2 inhibitors in general in people with ACR ≥200 mg/g and estimated GFR ≥20 mL/min/1.73 m 2 , as well as in those with CKD and heart failure. 179 KDIGO further specifies that once started, a SGLT-2 inhibitor can be continued even if the estimated GFR drops below 20 mL/min/1.73 m 2 , as long as it is tolerated and kidney replacement therapy has not yet been started. 72 179 The KDIGO and ADA guidelines recommend the use of GLP-1 receptor agonists in patients with type 2 diabetes and CKD who are unable to tolerate metformin or an SGLT-2 inhibitor or do not meet their individualized glycemic target with these drugs. 72 174 175 179

Kidney Disease: Improving Global Outcomes/American Diabetes Association recommendations on the management of diabetes in populations with chronic kidney disease. 72 174 ACR=albumin-to-creatinine ratio; ASCVD=atherosclerotic cardiovascular disease; BP=blood pressure; CCB=calcium channel blocker; CVD=cardiovascular disease; eGFR=estimated glomerular filtration rate; GLP-1 RA=glucagon-like peptide-1 receptor agonist; HTN=hypertension; MRA=mineralocorticoid receptor antagonist; PCSK9i=proprotein convertase subtilisin/kexin type 9 inhibitor; RAS=renin-angiotensin system; SGLT2i=sodium-glucose cotransporter-2 inhibitor
In patients with diabetes and CKD, the KDIGO and ADA guidelines recommend that finerenone should be used as add-on therapy to maximally tolerated ACE inhibitor or ARB if ACR is ≥30 mg/g (approximately ≥3 mg/mmol) and potassium is within normal limits (that is, ≤4.8 mmol/L based on trial and ≤5.0 mmol/L as per FDA). 72 174 175 179 More specifically, the starting dose should be 10 mg daily when estimated GFR is 25-59 mL/min/1.73 m 2 and 20 mg daily when it is ≥60 mL/min/1.73 m 2 . The guidelines also recommend that potassium concentration should be checked at four weeks after starting treatment, with each dose change, and routinely during treatment. If potassium is >5.5 mmol/L, the drug should be stopped and restarted at the lower dose of 10 mg daily when potassium is ≤5.0 mmol/L. Additionally, finerenone need not be stopped when estimated GFR falls below 25 mL/min/1.73 m 2 as long as the patient is normokalemic. 174 175
With respect to cardiovascular risk reduction, the KDIGO guidelines suggest that all patients aged over 50 with CKD G3-G5 but not treated with chronic dialysis or kidney transplantation should be treated with a statin, irrespective of cholesterol concentrations or a statin/ezetimide combination. 179 187 The NICE recommendation is broader, recommending starting atorvastatin 20 mg for all people with CKD. 188 KDIGO recommends regular physical activity for people with CKD, for at least 150 minutes a week of moderate intensity exercise. 179 NICE simply suggests providing lifestyle advice, including encouragement of exercise, maintenance of healthy weight, and smoking cessation, and specifically recommends against offering low protein diets (defined as dietary protein intake <0.8 g/kg/day). 16 KDIGO recommends maintaining sodium intake <2 g/day and a protein intake of 0.8 g/kg/day but no higher than 1.3 g/kg/day. 179
People with CKD face high risks of many adverse outcomes, including requirement for kidney replacement therapy, cardiovascular events, and death. Fortunately, major advances have been made in the field of CKD over the past decade. Estimating equations for GFR and ACR have evolved for more precise classification of disease. Individualized risk prediction tools exist to assist in the counseling, referral, and treatment of patients. Novel therapies build on the fundamentals—a healthy lifestyle, blood pressure and glucose control, and statin therapy and RAAS blockade—to provide effective preventive strategies for CKD progression and cardiovascular events.
Glossary of abbreviations
ACE—angiotensin converting enzyme
ACR—albumin-to-creatinine ratio
ADA—American Diabetes Association
ADPKD—autosomal dominant polycystic kidney disease
ARB—angiotensin receptor blockers
CKD—chronic kidney disease
CKD-EPI—CKD Epidemiology Collaboration
DPP-4—dipeptidyl peptidase-4
eGFRcr—estimated glomerular filtration rate using creatinine
eGFRcr-cys—estimated glomerular filtration rate using creatinine and cystatin C
eGFRcys—estimated glomerular filtration rate using cystatin C
ESKD—end stage kidney disease
FDA—Food and Drug Administration
FSGS—focal segmental glomerulosclerosis
GFR—glomerular filtration rate
GLP-1—glucagon-like peptide-1
KDIGO—Kidney Disease: Improving Global Outcomes
KFRE—kidney failure risk equation
KFRT—kidney failure with replacement therapy
LDL—low density lipoprotein
MDRD—Modification of Diet in Renal Disease
MRA—mineralocorticoid receptor antagonists
NICE—National Institute for Health and Care Excellence
NSAID—non-steroidal anti-inflammatory drug
PCR—protein-to-creatinine ratio
RAAS—renin-angiotensin-aldosterone system
SGLT-2—sodium-glucose cotransporter-2
Questions for future research
How do the race-free estimating equations perform in global populations?
Where can genetic testing add value in patient care?
Can cause of chronic kidney disease be incorporated into risk prediction tools?
How can medical therapy be best tailored for the individual patient with chronic kidney disease?
Patient perspective
Increasing awareness of chronic kidney disease is key to empowering patients to make lifestyle changes and seek treatments to improve their health outcomes. We are pleased to offer our perspective as husband and wife, and as physicians, who have been affected by kidney disease. Roberta M Falke is a patient with autosomal dominant polycystic kidney disease (ADPKD), a kidney transplant recipient, and a retired hematologist-oncologist. Andrew S Levey is a kidney donor and a nephrologist. Our knowledge of Roberta’s family history enabled early diagnosis and treatment. 189 Although we have benefited from our training and positions in the healthcare system, all patients can benefit from early diagnosis.
RMF —My ADPKD was diagnosed when I developed pyelonephritis at age 22 years. Thereafter, I had prophylaxis and prompt treatment of recurrent urinary tract infections and, as the disease progressed, complications of kidney and liver cysts, hypertension, hyperparathyroidism, vitamin D deficiency, acidosis, hyperkalemia, and ultimately kidney failure, with fatigue, dietary restrictions, and a long list of medications to take every day. I had always known that living donor kidney transplantation would be the best treatment for my kidney failure. Over time, family members without ADPKD donated to others, and when I was ready at age 60 years no family members were available. Fortunately, Andy stepped up. I felt better immediately after the transplant, and in the 13 years since then I have continued to take medications daily but have had few complications. I am grateful to all those who have cared for me for many years and enabled me to make the best choices I could to help myself, and I’m especially grateful to Andy who gave me the gift of life.
ASL —I knew that Roberta would develop kidney failure and hoped that a living kidney donor would be available for her. I wanted to donate, but our blood group incompatibility was an obstacle, so it was exciting when paired donor exchange was conceived and implemented in our region. I believe that kidney donors benefit from donation, not only by fulfilling their spirit of altruism but by improving their own lives. In my case, donating has been life changing. Roberta and I have been able to have an active, fulfilling life for more than a decade after the transplant, without the demands and complications of kidney failure or dialysis. I hope that we will have many more years together. I am also grateful to all those who enabled me to achieve my goal and to Roberta, who always takes full responsibility for caring for her kidney disease.
Acknowledgments
We thank Andrew S Levey and Roberta M Falke for providing both their perspective as patients affected by kidney disease and their input on the manuscript itself. We also acknowledge Alix Rosenberg and Yingying Sang for their help with the boxes and figures.
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: All authors were involved in the conception, writing, and revision of the manuscript. MEG is the guarantor.
Funding: TKC is supported by NIH/NIDDK K08DK117068; MEG is supported by NIH/NIDDK R01DK108803, R01DK100446, R01DK115534, R01DK124399, and NIH/NHLBI K24HL155861.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: TKC and MEG received an honorarium from the American Society of Nephrology (nephSAP).
Patient involvement: We invited a husband and wife, Andrew S Levey and Roberta M Falke, who are affected by chronic kidney disease, to write a patient perspective together. They also reviewed and provided input on the penultimate draft of the paper.
Provenance and peer review: Commissioned; externally peer reviewed.
- GBD Chronic Kidney Disease Collaboration
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group
- Foreman KJ ,
- Marquez N ,
- Dolgert A ,
- Kovesdy C ,
- Langham R ,
- Rosenberg M ,
- ↵ United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. 2022. https://adr.usrds.org/2022 .
- Garcia-Garcia G ,
- Friedman DJ ,
- Derebail VK ,
- Genovese G ,
- Johnson RJ ,
- Wesseling C ,
- Johnson DW ,
- O’Shaughnessy MM ,
- CKD Prognosis Consortium
- Shlipak MG ,
- ↵ National Institute for Health and Care Excellence. NICE guideline [NG203]: Chronic kidney disease: assessment and management. 2021. www.nice.org.uk/guidance/ng203 .
- Nadkarni GN ,
- Chronic Kidney Disease Prognosis Consortium
- Weaver RG ,
- Modification of Diet in Renal Disease Study Group
- Chronic Kidney Disease Epidemiology Collaboration
- Stevens LA ,
- Schmid CH ,
- CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration)
- Delgado C ,
- Eneanya ND ,
- ↵ Chen DC, Potok OA, Rifkin D, Estrella MM. Advantages, Limitations, and Clinical Considerations in Using Cystatin C to Estimate GFR. Kidney360 2022;3:1807-1814.
- Khandpur S ,
- Awasthi A ,
- Behera MR ,
- Nestor JG ,
- Groopman EE ,
- Cameron-Christie S ,
- Antignac C ,
- Bergmann C ,
- Sexton DJ ,
- Collins AJ ,
- Torres VE ,
- Chapman AB ,
- Devuyst O ,
- TEMPO 3:4 Trial Investigators
- Müller RU ,
- Messchendorp AL ,
- Irazabal MV ,
- Rangel LJ ,
- Bergstralh EJ ,
- CRISP Investigators
- ↵ QxMD. Total Kidney Volume (height-adjusted) Calculator & ADPKD Prognostic Tool using Kidney Dimensions calculator. https://qxmd.com/calculate/calculator_490/total-kidney-volume-height-adjusted-calculator-adpkd-prognostic-tool-using-kidney-dimensions .
- Rodrigues JC ,
- ↵ QxMD. International IgAN Prediction Tool at biopsy - adults. https://qxmd.com/calculate/calculator_499/international-igan-prediction-tool-at-biopsy-adults .
- Barbour SJ ,
- International IgA Nephropathy Network
- Selvaskandan H ,
- Gonzalez-Martin G ,
- Barratt J ,
- Foster MC ,
- Fornage M ,
- AASK Study Investigators ,
- CRIC Study Investigators
- Zimmerman B ,
- VX19-147-101 Study Group
- Houssiau F ,
- Garrelfs SF ,
- Frishberg Y ,
- Hulton SA ,
- ILLUMINATE-A Collaborators
- Griffith J ,
- Ferguson TW ,
- Fallahzadeh MK ,
- McCulloch CE ,
- Brunskill NJ ,
- Ballew SH ,
- Nguyen HA ,
- Abdelmalek JA ,
- Woodell TB ,
- Greene TH ,
- Sparkes D ,
- Harasemiw O ,
- Thorsteinsdottir B ,
- Matsushita K ,
- Kaptoge S ,
- Hageman SHJ ,
- Jassal SK ,
- Scherzer R ,
- Farrington DK ,
- Surapaneni A ,
- Seegmiller JC ,
- Carrero JJ ,
- Wright JT Jr . ,
- African American Study of Kidney Disease and Hypertension Study Group
- Williamson JD ,
- Whelton PK ,
- SPRINT Research Group
- Agarwal R ,
- Cramer AE ,
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group
- MacMahon S ,
- Chalmers J ,
- ADVANCE Collaborative Group
- Perkovic V ,
- Heerspink HL ,
- The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia)
- Brenner BM ,
- Cooper ME ,
- de Zeeuw D ,
- RENAAL Study Investigators
- Hunsicker LG ,
- Clarke WR ,
- Collaborative Study Group
- Sleight P ,
- Dagenais G ,
- Heart Outcomes Prevention Evaluation Study Investigators
- ONTARGET Investigators
- Emanuele N ,
- VA NEPHRON-D Investigators
- Bhandari S ,
- STOP ACEi Trial Investigators
- Mahaffey KW ,
- CANVAS Program Collaborative Group
- Jardine MJ ,
- CREDENCE Trial Investigators
- Heerspink HJL ,
- Stefánsson BV ,
- Correa-Rotter R ,
- DAPA-CKD Trial Committees and Investigators
- Wheeler DC ,
- Stefansson BV ,
- Batiushin M ,
- Herrington WG ,
- Staplin N ,
- The EMPA-KIDNEY Collaborative Group
- Vaduganathan M ,
- DeFronzo RA ,
- Reeves WB ,
- Tuttle KR ,
- Nangaku M ,
- Schneeweiss S ,
- Fralick M ,
- Muskiet MHA ,
- Tonneijck L ,
- Pfeffer MA ,
- Claggett B ,
- ELIXA Investigators
- Kristensen SL ,
- Bentley-Lewis R ,
- Aguilar D ,
- Riddle MC ,
- Ørsted DD ,
- Brown-Frandsen K ,
- LEADER Steering Committee and Investigators
- Daniels GH ,
- LEADER Steering Committee ,
- LEADER Trial Investigators
- Consoli A ,
- SUSTAIN-6 Investigators
- Holman RR ,
- Bethel MA ,
- EXSCEL Study Group
- Merrill P ,
- Gerstein HC ,
- Colhoun HM ,
- Dagenais GR ,
- REWIND Investigators
- REWIND Trial Investigators
- Rosenstock J ,
- AMPLITUDE-O Trial Investigators
- Lakshmanan MC ,
- Dieter BP ,
- Alicic RZ ,
- O’Neil PM ,
- Birkenfeld AL ,
- McGowan B ,
- Pratley R ,
- PIONEER 4 investigators
- Navaneethan SD ,
- Nigwekar SU ,
- Sehgal AR ,
- Strippoli GF
- Epstein M ,
- Kovesdy CP ,
- Pecoits-Filho R
- Bakris GL ,
- FIDELIO-DKD Investigators
- Barrera-Chimal J ,
- Lima-Posada I ,
- Filippatos G ,
- FIGARO-DKD Investigators
- FIDELIO-DKD and FIGARO-DKD investigators
- Parving HH ,
- Andress DL ,
- SONAR Committees and Investigators
- Trachtman H ,
- DUET Study Group
- Radhakrishnan J ,
- Alpers CE ,
- PROTECT Investigators
- ↵ US Food and Drug Administration. Highlights of prescribing information: Filspari. 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/216403s000lbl.pdf .
- Kalyesubula R ,
- Schaeffner E ,
- Ishigami J ,
- Trevisan M ,
- Grundy SM ,
- Bailey AL ,
- Baigent C ,
- Landray MJ ,
- SHARP Investigators
- Lloyd-Jones DM ,
- Morris PB ,
- Ballantyne CM ,
- Writing Committee
- Charytan DM ,
- Sabatine MS ,
- Pedersen TR ,
- FOURIER Steering Committee and Investigators
- Weiner DE ,
- Uchiyama K ,
- Muraoka K ,
- Beetham KS ,
- Krishnasamy R ,
- Stanton T ,
- Howden EJ ,
- Coombes JS ,
- Douglas B ,
- Campbell KL ,
- Ikizler TA ,
- Robinson-Cohen C ,
- Look AHEAD Research Group
- Sadeghirad B ,
- Hostetter TH
- Caulfield LE ,
- Garcia-Larsen V ,
- Bushinsky DA
- Wesson DE ,
- Mathur VS ,
- ↵ Tangri N, Mathur VS, Bushinsky DA, Inker LA, et al. VALOR-CKD: A Multicenter, Randomized, Double-Blind Placebo-Controlled Trial Evaluating Veverimer in Slowing Progression of CKD in Patients With Metabolic Acidosis. 2022, Florida. https://www.asn-online.org/education/kidneyweek/2022/program-abstract.aspx?controlId=3801835 .
- Aburto NJ ,
- Gutierrez H ,
- Elliott P ,
- Cappuccio FP
- Narasaki Y ,
- O’Donnell M ,
- Rangarajan S ,
- PURE Investigators
- Juraschek SP ,
- Miller ER 3rd . ,
- Fioretto P ,
- Anderson CAM ,
- Whittaker CF ,
- Miklich MA ,
- Matzke GR ,
- Aronoff GR ,
- Atkinson AJ Jr . ,
- ↵ US Food and Drug Administration, Center for Drug Evaluation and Research. Pharmacokinetics in patients with impaired renal function - study design, data analysis, and impact on dosing. 2020. https://www.fda.gov/media/78573/download .
- Vondracek SF ,
- Teitelbaum I ,
- Hudson JQ ,
- Perazella MA
- Azoulay L ,
- Nessim SJ ,
- Doerfler RM ,
- Lazarus B ,
- Wilson FP ,
- Balasubramanian S ,
- Pattrapornpisut P ,
- Avila-Casado C ,
- Charchar F ,
- de Boer IH ,
- Sadusky T ,
- Tummalapalli SL ,
- Boulware LE ,
- Conference Participants
- American Diabetes Association Professional Practice Committee
- ↵ Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2023 Clinical Practice Guideline For the Evaluation and Management of Chronic Kidney Disease - Public Review Draft July 2023. 2023. https://kdigo.org/wp-content/uploads/2017/02/KDIGO-2023-CKD-Guideline-Public-Review-Draft_5-July-2023.pdf .
- Gansevoort RT ,
- Anders HJ ,
- Cozzolino M ,
- Delanaye P ,
- Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group
- Muntner P ,
- Einhorn PT ,
- Cushman WC ,
- 2017 National Heart, Lung, and Blood Institute Working Group
- Cheung AK ,
- ↵ National Institute for Health and Care Excellence. NICE guideline [NG28]: Type 2 diabetes in adults: management. 2022. https://www.nice.org.uk/guidance/ng28/chapter/Recommendations#chronic-kidney-disease .
- ↵ National Institute for Health and Care Excellence. Technology appraisal guidance [TA775]: Dapagliflozin for treating chronic kidney disease. 2022. https://www.nice.org.uk/guidance/ta775/chapter/1-Recommendations .
- Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group
- ↵ National Institute for Health and Care Excellence. NICE guideline [CG181]: Cardiovascular disease: risk assessment and reduction, including lipid modification. 2023. https://www.nice.org.uk/guidance/cg181/chapter/Recommendations#lipid-modification-therapy-for-the-primary-and-secondary-prevention-of-cardiovascular-disease .
- Introduction
- Conclusions
- Article Information
A, Unadjusted prevalence. B, Prevalence adjusted by age, sex, and race/ethnicity.
ACE indicates angiotensin-converting enzyme; ARB, angiotensin receptor blocker; NSAID, nonsteroidal anti-inflammatory drug; PPI, proton pump inhibitor; and SGLT2, sodium-glucose cotransporter 2.
eFigure. CURE-CKD STROBE Diagram, Participant Groups by CKD and At-Risk Categories
eTable 1. Inclusion Criteria for the CURE-CKD Registry
eTable 2. Characteristics of Adults at Risk of CKD in the CURE-CKD Registry
eTable 3. Characteristics of Adults With CKD and Diabetes or Prediabetes With or Without Hypertension in the CURE-CKD Registry
eTable 4. Characteristics of Adults at Risk of CKD With Diabetes or Prediabetes With or Without Hypertension in the CURE-CKD Registry
eTable 5. Medications Prescribed to Adults With CKD in the CURE-CKD Registry
eTable 6. Medications Prescribed to Adults at Risk of CKD in the CURE-CKD Registry
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Tuttle KR , Alicic RZ , Duru OK, et al. Clinical Characteristics of and Risk Factors for Chronic Kidney Disease Among Adults and Children : An Analysis of the CURE-CKD Registry . JAMA Netw Open. 2019;2(12):e1918169. doi:10.1001/jamanetworkopen.2019.18169
Manage citations:
© 2024
- Permissions
Clinical Characteristics of and Risk Factors for Chronic Kidney Disease Among Adults and Children : An Analysis of the CURE-CKD Registry
- 1 Providence St Joseph Health, Providence Medical Research Center, Spokane, Washington
- 2 University of Washington School of Medicine, Seattle
- 3 Division of General Internal Medicine, Department of Medicine, David Geffen School of Medicine, University of California, Los Angeles
- 4 Division of Nephrology, University of California, Los Angeles
- 5 Elson S. Floyd College of Medicine, Washington State University, Spokane
- 6 College of Pharmacy and Pharmaceutical Sciences, Washington State University, Spokane
Question What are the clinical characteristics of and major risk factors for chronic kidney disease among patients in 2 large US health care systems?
Findings In this cohort study of the Center for Kidney Research, Education, and Hope (CURE-CKD) registry, more than 2.6 million adults and children had chronic kidney disease or were at risk. Albuminuria or proteinuria was tested in approximately one-eighth of adults with chronic kidney disease, renin-angiotensin system inhibitors were prescribed to one-fifth, and nonsteroidal anti-inflammatory agents or proton pump inhibitors were prescribed to more than one-third.
Meaning Despite common occurrence of chronic kidney disease, rates of identification and use of kidney protective agents were low, while use of potential nephrotoxins was widespread.
Importance Chronic kidney disease (CKD) is serious and common, yet recognition and public health responses are limited.
Objective To describe clinical features of, prevalence of, major risk factors for, and care for CKD among patients treated in 2 large US health care systems.
Design, Setting, and Participants This cohort study collected data from the Center for Kidney Disease Research, Education, and Hope (CURE-CKD) registry, an electronic health record–based registry jointly curated and sponsored by Providence St Joseph Health and the University of California, Los Angeles. Patients were adults and children with CKD (excluding end-stage kidney disease) and adults at risk of CKD (ie, with diabetes, hypertension, or prediabetes) identified by laboratory values, vital signs, prescriptions, and administrative codes. Data were collected from January 2006 through December 2017, with analyses performed from March 2019 through November 2019.
Exposures Diabetes, hypertension, and prediabetes.
Main Outcomes and Measures Clinical and demographic characteristics, prevalence, and prescribed medications.
Results Of 2 625 963 adults and children in the sample, 606 064 adults (23.1%) with CKD had a median (interquartile range [IQR]) age of 70 (59-81) years, with 338 785 women (55.9%) and 434 474 non-Latino white individuals (71.7%). A total of 12 591 children (0.4%) with CKD had a median (IQR) age of 6 (1-13) years, with 7079 girls (56.2%) and 6653 non-Latino white children (52.8%). Median (IQR) estimated glomerular filtration rate was 53 (41-61) mL/min/1.73 m 2 among adults and 70 (50-95) mL/min/1.73 m 2 in children. Prevalence rates for CKD in adults were 4.8% overall (606 064 of 12 669 700) with 1.6% (93 644 of 6 011 129) during 2006 to 2009, 5.7% (393 455 of 6 903 084) during 2010 to 2013, and 8.4% (683 574 of 8 179 860) during 2014 to 2017 ( P < .001). A total of 226 693 patients (37.4%) had category 3a CKD; 100 239 (16.5%), category 3b CKD; 39 125 (6.5%), category 4 CKD; and 20 328 (3.4%), category 5 CKD. Among adults with CKD, albuminuria and proteinuria assessments were available in 52 551 (8.7%) and 25 035 (4.1%) patients, respectively. A renin-angiotensin system inhibitor was prescribed to 124 575 patients (20.6%), and 204 307 (33.7%) received nonsteroidal anti-inflammatory drugs or proton pump inhibitors. Of 1 973 258 adults (75.1%) at risk, one-quarter had diabetes or prediabetes (512 299 [26.0%]), nearly half had hypertension (955 812 [48.4%]), and one-quarter had both hypertension and diabetes or prediabetes (505 147 [25.6%]).
Conclusions and Relevance This registry-based cohort study revealed a burgeoning number of patients with CKD and its major risk factors. Rates of identification and use of kidney protective agents were low, while potential nephrotoxin use was widespread, underscoring the pressing need for practice-based improvements in CKD prevention, recognition, and treatment.
Chronic kidney disease (CKD) is a serious and common disease, and it eventuates in multiple complications, including premature mortality and end-stage kidney disease (ESKD). 1 - 3 An estimated 1 in 7 to 10 adults worldwide have CKD, with only approximately 10% surviving to ESKD and only half of survivors receiving dialysis or a kidney transplant because of lack of access or high costs. 3 From 1990 to 2016, the prevalence of CKD increased by 90%, and related deaths, mainly due to cardiovascular diseases and infections, nearly doubled in the United States and globally. 4 - 6 In high-income countries, 2% to 3% of annual health care costs are devoted to the 0.03% of the population with ESKD. 7
The increasing prevalence of CKD is closely tied to the increase of at-risk populations with diabetes, hypertension, and prediabetes. Indeed, diabetes is the leading cause of CKD and a global health emergency, with 425 million individuals affected worldwide in 2017 and a projected 629 million individuals affected by 2045. 8 - 10 Hypertension is the second most frequent cause of CKD, affecting nearly one-third of US adults and 1.13 billion people globally in 2015. 11 , 12 The estimated population size for prediabetes was 78.5 million among adults in the United States between 2011 and 2014, and nearly one-tenth have been reported with CKD. 13 Even so, awareness of CKD and its major risk factors remains strikingly low among health care professionals and patients alike. 14 - 16
The Advancing American Kidney Health initiative was recently launched by a US executive order calling for new approaches to prevent and treat CKD, with a goal of reducing ESKD incidence 25% by 2030. 17 Real-world data from electronic health records (EHRs) provide an ideal platform to answer this call by improving CKD detection, tracking, and public health responses. The Center for Kidney Disease Research, Education, and Hope (CURE-CKD) registry contains detailed patient-level EHR data from more than 2.6 million adults and children with CKD and at risk of CKD during 12 inclusive years. 18 The objective of this study was to describe baseline clinical features of, prevalence of, major risk factors for, and care for CKD based on data from the CURE-CKD registry.
The study was approved by Providence St Joseph Health (PSJH; Washington, Montana, Oregon, Alaska, and California) and the University of California, Los Angeles (UCLA; California) Health institutional review boards, which determined that written informed consent was not required for this limited data set. Data use agreements between PSJH and UCLA Health formed the framework for data sharing, stewardship, and security. This study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cohort studies. 19
Detailed methodology for CURE-CKD has been previously published. 18 The formation of CURE-CKD was supported by institutional funding from PSJH and UCLA Health. Both health care systems use Epic EHRs (Epic Systems). The first phase of CURE-CKD created a data repository with patient information from EHRs with at least 1 measure indicating CKD, diabetes, prediabetes, or hypertension based on patient-level laboratory values, vital signs, prescription medications, and administrative codes from January 1, 2006, to December 31, 2017. Electronic health record data for these patients were extracted from ambulatory and inpatient encounters. Unstructured data from the EHRs were not extracted. The total number of patients with encounters and serum creatinine measures for the health care systems was also recorded. Repository updates are performed annually.
The second phase crafted an EHR-based registry of participants with CKD and at risk for CKD derived from the repository. The first 90 days a patient was included in the registry were considered the baseline period. Registry criteria were based on established clinical practice guidelines for CKD (eTable 1 in the Supplement ). Adults (ie, aged ≥18 years) were included with 2 or more of the following laboratory measurements recorded at least 90 days apart: estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m 2 , calculated from serum creatinine levels using the Chronic Kidney Disease Epidemiology equation; urine albumin to creatinine ratio greater than 30 mg/g; and urine protein to creatinine ratio greater than 150 mg/g. 20 , 21 Children (ie, aged <18 years) with CKD were identified using the same criteria, except the bedside Schwartz equation was used to calculate eGFR from serum creatinine levels. 22 We identified CKD categories 1 and 2 by an administrative code, urine albumin to creatinine ratio greater than 30 mg/g, and/or urine protein to creatinine ratio greater than 150 mg/g. We identified CKD categories 3 to 5 based on eGFR and/or administrative code. Patients with ESKD treated with dialysis or kidney transplant were excluded. Participants with diabetes, prediabetes, and hypertension were identified by clinical practice guidelines and published criteria for EHR identification 23 - 25 (eTable 1 in the Supplement ).
Data analyses were performed from March 2019 through November 2019. Continuous variables are reported as mean and SD or as median and interquartile range (IQR) for skewed or kurtotic distributions. Categorical variables are reported as frequencies and percentages. The Pearson χ 2 test for independence was used to determine differences between categorical variables. Prevalence rates for CKD among adults are presented as a combined data set from PSJH and UCLA Health and by each system. To address sources of bias in CKD prevalence rates, data were analyzed as proportions based on the 3 following definitions for CKD: (1) CURE-CKD entry criteria, (2) 2 measurements of eGFR less than 60 mL/min/1.73 m 2 at least 90 days apart; and (3) 1 measurement of eGFR less than 60 mL/min/1.73 m 2 . Serial prevalence rates of CKD overall, by categories, and prescription medication use during 3 periods (ie, 2006-2009, 2010-2013, and 2014-2017) were analyzed by logistic regression models. Prevalence was adjusted for age, sex, and race/ethnicity in the models using repository data (ie, CKD by 1 or 2 eGFR measurements). Adjustments could not be made for CKD prevalence with the denominator based on the total number of patients with encounters because the institutional review board approvals did not include data extraction for age, sex, and race/ethnicity from the total populations in the health care system.
To reduce risk of type I error, a 2-tailed P < .001 was the a priori threshold for statistical significance because of the large sample size and resultant high level of statistical power. Because overall CKD participant characteristics, except distribution of geolocation, were similar between PSJH and UCLA Health, findings other than prevalence are presented from a jointly curated data set. Descriptive statistics and the Pearson χ 2 test were conducted with SQL Server Management Studio 2012 version 11.0.2100.60 (Microsoft Corp); tests for normality and logistic regression were completed using SPSS statistical software version 23 (IBM Corp).
A total of 2 625 963 adults and children were included in the sample. The cohort of adults with CKD included 606 064 individuals (23.1%), including 338 785 women (55.9%), 434 474 non-Latino white individuals (71.7%), 17 625 Latino individuals (2.9%), 29 974 black individuals (4.9%), 32 850 Asian individuals (5.4%), 5461 American Indian and Alaska Native individuals (0.9%), and 3899 Hawaiian and Pacific Islander individuals (0.6%) ( Table 1 ). The median (IQR) age among adults was 70 (59-81) years. The proportions with CKD were highest among those aged 60 to 89 years (401 541 [66.3%]). A total of 12 591 children (0.4%) with CKD included 7079 girls (56.2%) and 6653 non-Latino white children (52.8%) ( Table 2 ). The median (IQR) age of children with CKD was 6 (1-13) years, and CKD was comparably distributed across age groups (2545 [20.2%] aged <1 year; 2241 [17.8%], 1-3 years; 1515 [12.0%], 4-6 years; 1863 [14.8%], 7-10 years; 1916 [15.2%], 11-14 years; and 2511 [19.9%], 15-17 years). The cohort of participants at risk for CKD included 1 973 258 adults (75.1%). Among them, 955 812 (48.4%) had hypertension alone, while 505 147 (25.6%) had diabetes or prediabetes with hypertension, and 512 299 (26.0%) had diabetes or prediabetes alone. Those at risk for CKD included 1 014 847 women (51.4%), 1 308 036 non-Latino white individuals (66.3%), 60 201 Latino individuals (3.1%), 92 403 black individuals (4.9%), 114 400 Asian individuals (5.8%), 19 820 American Indian and Alaska Native individuals (1.0%), and 11 420 Hawaiian and Pacific Islander individuals (0.6%) (eTable 2 in the Supplement ). Proportions of participants at risk for CKD were highest among those aged 50 to 69 years (866 528 [43.9%]).
Comparing adults with CKD with those at risk for CKD, women were more frequently represented in the cohort with CKD than in the cohort at risk for CKD (338 785 [55.9%] vs 1 014 847 [51.4%]; P < .001). Non-Latino white individuals (434 474 [71.7%] vs 1 308 036 [66.3%]; P < .001) and individuals aged 70 years or older (315 397 [52.0%] vs 386 364 [19.6%]; P < .001) were also more common among participants with CKD vs those at risk. There was a higher proportion with rural geolocation within PSJH vs UCLA Health (287 622 [17.2%] vs 6918 [1.8%]; P < .001).
A total of 243 635 adults with CKD (40.2%) were identified by eGFR, 163 375 (27.0%) by administrative codes, and 151 794 (25.0%) by both eGFR and administrative codes. Various combinations of laboratory measurements and administrative codes accounted for the remainder of adult CKD identification. More than half of adults with CKD were in category 3 (3a, 226 693 [37.4%]; 3b, 100 239 [16.5%]) ( Table 1 ). Decreases in prevalence were observed for CKD category 4 (39 125 [6.5%]) and category 5, not dialyzed (20 328 [3.4%]). Median (IQR) eGFR was 53 (41-61) mL/min/1.73 m 2 , and measurements of albuminuria and proteinuria were recorded in 52 511 (8.7%) and 25 035 (4.1%) patients, respectively. Mean (SD) systolic and diastolic blood pressure values were 129 (18) mm Hg and 72 (11) mm Hg, respectively. When participants with CKD and diabetes or prediabetes were assessed separately, higher proportions of patients with diabetes than those with prediabetes had CKD category 4 or 5 (9790 [18.4%] vs 3724 [13.2%]; P < .001), and higher levels of albuminuria or proteinuria were present in the group with diabetes compared with the group with prediabetes (5555 [10.4%] vs 965 [3.4%]; P < .001) (eTable 3 in the Supplement ).
Most children (10 841 [86.1%]) were identified exclusively through CKD administrative codes. Among 8145 children (64.7%), CKD was not categorized ( Table 2 ). Median (IQR) eGFR was 70 (50-95) mL/min/1.73 m 2 . Mean (SD) systolic and diastolic blood pressure were 104 (16) mm Hg and 61 (11) mm Hg, respectively. Measurements of albuminuria and proteinuria were available in 520 (4.1%) and 798 (6.4%) children, respectively.
Median (IQR) eGFR in adults at risk of CKD was 90 (77-103) mL/min/1.73 m 2 , and albuminuria and proteinuria measurements were recorded in 51 470 (2.6%) and 10 285 (0.5%), respectively (eTable 2 in the Supplement ). Mean (SD) systolic and diastolic blood pressure values were 135 (18) mm Hg and 79 (12) mm Hg, respectively. When participants with diabetes or prediabetes who were at risk for CKD were analyzed separately, frequency of ascertainment for albuminuria or proteinuria was 7% or less in all groups (eg, among 317 648 patients with diabetes and hypertension, albumin to creatine ratio measurements were available for 21 697 patients [6.8%]; among 187 499 patients with prediabetes and hypertension, protein to creatine ratio measurements were available in 907 [0.5%]) (eTable 4 in the Supplement ).
A total of 12 669 700 patients received care at PSJH (10 793 550 [85.2%]) and UCLA Health (1 876 150 [14.8%]) between January 1, 2006, and December 31, 2017 (eFigure in the Supplement ). During this period, 606 064 adults (4.8%) met the CURE-CKD registry entry criteria for CKD. However, when CKD was determined by at least 2 eGFR measurements of less than 60 mL/min/1.73 m 2 at least 90 days apart, unadjusted prevalence among adults was 26.1% (420 678 of 1 612 737), and adjusted CKD prevalence was 22.6%. When determined by 1 eGFR measure, unadjusted CKD prevalence was 34.4% (873 642 of 2 542 393), and adjusted prevalence was 32.9% ( Table 3 ). Diagnostic coding for CKD was recorded among 171 011 patients (40.7%) with CKD determined by 2 eGFR measurements at least 90 days apart and among 240 630 patients (27.5%) with CKD determined by 1 eGFR measurement.
Temporal trends in CKD prevalence were determined for the 3 following periods: 2006 to 2009, 2010 to 2013, and 2014 to 2017. CKD prevalence rates by CURE-CKD registry criteria increased over time (2006-2009, 93 644 of 6 011 129 [1.6%]; 2010-2013, 393 455 of 6 903 084 [5.7%]; and 2014-2017, 683 574 of 8 179 860 [8.4%]). Prevalence rates adjusted for age, sex, and race/ethnicity and based on eGFR classification alone were higher and stable over time among patients with 2 or more eGFR measurements at least 90 days apart (20.8%, 22.6%, and 21.2%, respectively), while increasing adjusted prevalence was observed among patients with 1 eGFR measurement (22.3%, 27.8%, and 28.5%, respectively). Rates of administrative coding for CKD increased progressively at both PSJH and UCLA Health ( Table 3 ). For example, among patients with 2 eGFR measurements of less than 60 mL/min/1.73 m 2 at least 90 days apart, 2766 of 87 225 (3.2%) were identified by administrative code during 2006 to 2009 and 124 897 of 238 750 (52.3%) were identified by administrative code during 2014 to 2017. When CKD categories were analyzed by at least 2 eGFR measurements at least 90 days apart, unadjusted prevalence rates and prevalence rates adjusted by age, sex, and race/ethnicity showed progressive increases for categories 3a and 3b with declines in categories 4 and 5 (eg, category 3a: 2006-2009, 22 805 [prevalence, 26.1%; adjusted prevalence 26.1%]; 2014-2017, 96 449 [prevalence 40.4%; adjusted prevalence, 38.2%]; category 4: 2006-2009, 22 338 [prevalence, 25.7%, adjusted prevalence, 19.4%], 2014-2017, 42 065 [prevalence, 17.6%; adjusted prevalence, 16.1%]) ( Figure 1 ).
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) were prescribed to 127 574 adults (20.5%) with CKD, with slightly higher use of these agents among those with CKD and hypertension (112 449 of 434 657 [25.9%]) (eTable 5 in the Supplement ). By contrast, 204 307 participants (33.7%) with CKD had prescriptions for nonsteroidal anti-inflammatory drugs (NSAIDs) or proton pump inhibitors (PPIs). Statins and aspirin were prescribed to 107 445 (17.7%) and 110 335 (18.2%) individuals, respectively. The most commonly prescribed antihyperglycemic agents among patients with CKD and diabetes or prediabetes were insulin (38 278 [10.0%]), metformin (30 393 [7.9%]), and sulfonylureas (16 989 [4.4%]). Medications prescribed among the cohort of participants at risk of CKD were generally similar to the CKD cohort, except for more common use of insulin (83 363 [16.3%]) among those with diabetes and of NSAIDs (701 493 [35.5%]) and PPIs (295 804 (15.0%]) overall (eTable 6 in the Supplement ).
Temporal trends in prescription medications were determined for participants with CKD determined by 2 eGFR measurements of less than 60 mL/min/1.73 m 2 at least 90 days apart for the 3 periods. Use rates of ACE inhibitors, ARBs, NSAIDs, and PPIs across CKD categories 3a to 5 all increased (ACE inhibitors: 2006-2009, 5654 [2.0%]; 2010-2013, 46 921 [5.1%]; 2014-2017, 81 601 [7.6%]; ARBs: 2006-2009, 2461 [0.9%]; 2010-2013, 21 791 [2.4%]; 2014-2017, 47 233 [4.4%]; NSAIDs: 2006-2009, 7009 [2.4%]; 2010-2013, 57 705 [6.3%]; 2014-2017, 113 251 [11.0%]; PPIs: 2006-2009, 5331 [1.8%]; 2010-2013, 44 362 [4.9%]; 2014-2017, 83 340 [7.7%]) ( Figure 2 ). Sodium-glucose cotransporter 2 inhibitors were rarely prescribed, but use increased over time (2006-2009, 0; 2010-2013, 22 [0.002%]; 2014-2017, 1002 [0.093%]).
More than 2.6 million adults and children who received care at PSJH and UCLA Health from 2006 to 2017 had CKD or were at risk of CKD. Overall, CKD prevalence among adults in the health care systems was 4.8%, as determined by a combination of eGFR, albuminuria and proteinuria measures, and administrative code criteria. However, adult CKD prevalence adjusted for age, sex, and race/ethnicity was 22.6% based on persistently low eGFR alone. Adults with CKD were more likely to be older, women, and non-Latino white individuals. In this study, CKD category 3 was most frequent, with a clear drop-off in prevalence at more advanced categories. Kidney protective agents (ie, renin-angiotensin system inhibitors) were prescribed to approximately one-fifth of adults with CKD, while potential nephrotoxins (ie, NSAIDs and PPIs) were prescribed to more than one-third of adults with CKD. Albuminuria and proteinuria testing for CKD assessment was rarely reported.
The CURE-CKD registry is among the most comprehensive CKD registries worldwide. A unique feature is the extensive amount of patient-level data on laboratory measures, prescriptions, and vital signs, combined with administrative codes, to identify CKD and major risk factors according to guideline-based criteria. 21 , 24 , 25 Previous registries were restricted by containing primarily administrative data, ESKD, primary care practices, single health care systems, older adults, or men. 4 , 26 - 32 In contrast, CURE-CKD participants represent the life span, from children to adults, and include women and men and a wide spectrum of races and ethnicities across an expansive region of the western United States that has not been previously involved in large-scale epidemiologic studies of CKD. Moreover, PSJH and UCLA Health care for patients in a variety of settings that include academic, primary care, and specialty practices as well as community health and safety-net systems. Rural patients were well represented in the geography covered by PSJH. Thus, CURE-CKD provides in-depth identification of patients with and at risk for CKD in contemporary US health care systems.
In CURE-CKD, the progressive increase in adult CKD prevalence was largely driven by diagnostic coding. Among adults with persistently low eGFR, use of CKD administrative codes increased from 3.2% to 52.3% between the periods of 2006 to 2009 and 2014 to 2017, while overall CKD prevalence estimates, adjusted for age, sex, and race/ethnicity, were essentially stable between 20.8% and 22.6%. Although the upward trend in CKD recognition represents a clinically meaningful improvement, nearly one-half of patients with low eGFR remained undiagnosed in the most recent period. The present findings from CURE-CKD point to the critical need for quality improvement and research at the point of care.
Although nearly two-thirds of the adults with CKD had diabetes, hypertension, or prediabetes, rates of laboratory testing for albuminuria or proteinuria and of prescribing ACE inhibitors or ARBs were low. Potentially nephrotoxic agents (ie, NSAIDs and PPIs) were used more commonly than renin-angiotensin system inhibitors. Given the most common cause of death in CKD is cardiovascular disease, the low use of preventive agents, such as statins and aspirin, is also concerning. 33 , 34 Compared with participants in the National Health and Nutrition Examination Survey, patients with CKD in CURE-CKD received ACE inhibitors or ARBs much less often during approximately the same period. 35 Although CURE-CKD found an increase in uptake of renin-angiotensin system inhibitors in adults with CKD categories 3a to 5, NSAID and PPI use also increased over time. However, these prescription rates were lower than in the overall CKD cohort, perhaps because of concerns about adverse effects with more advanced CKD. While this may seem counterintuitive for renin-angiotensin system inhibitors, these agents may be avoided because of fear of complications such as hyperkalemia or acute kidney injury, especially in acute care settings. In Ontario, Canada, primary care practices reported ACE inhibitor or ARB use in three-fourths of patients with CKD, but the metric was confined to those with diabetes and albuminuria or adults older than 66 years. 30 , 31 Nevertheless, rates of albuminuria testing in the overall CKD population were comparably low, although avoidance of NSAIDs was better among patients in Canada than in CURE-CKD. 30 A recent Canada-wide study 32 from an EHR-based surveillance system in primary care found that only 4 of 12 quality indicators for CKD care were met, with ACE inhibitor or ARB use among approximately one-third of patients with diabetes or proteinuria. Contrasts exist between reports from health care systems, community screenings, primary care practices, and countries, but they consistently illuminate major gaps in CKD care and the need for more comprehensive surveillance to uncover actionable trends.
In comparison with patients treated at PSJH and UCLA Health, the Kidney Early Evaluation Program and the National Health and Nutrition Examination Survey have reported lower frequencies of individuals at risk for CKD in community screenings. 36 Moreover, associations between risk factors and CKD are remarkably complex. For example, although a primary contributor to CKD is diabetes, CKD in patients with diabetes greatly amplifies cardiovascular risks. 37 Additionally, nearly one-fifth of patients with CKD in the CURE-CKD registry had prediabetes. The prediabetes phenotype of CKD appears less severe than the diabetes phenotype of CKD, as reflected by fewer patients with advanced CKD categories, albuminuria, or proteinuria and prediabetes. Nevertheless, consistent with findings from the National Health and Nutrition Examination Survey, findings from CURE-CKD support the observation that subdiabetic hyperglycemia may contribute to kidney damage before overt diabetes ensues. 13 The CURE-CKD registry contains abundant longitudinal data that will be invaluable for elucidating CKD incidence among individuals at risk as well as progression and complications in those with CKD. Given its vast scope, CURE-CKD is also ideally suited to generate and validate CKD risk prediction models. 38
Strengths of the CURE-CKD registry include the large sample size, long observation duration, and curated patient-level data from 2 US health care systems. However, this study has limitations. First, CURE-CKD is limited by differences in documentation methods across and between health care systems and varying attrition rates based on insurance, socioeconomic factors, and geolocation. Variation in platforms even within a common EHR system also presents a limitation to the creation of interinstitutional registries, highlighting the importance of collaboration in identifying data elements, structures, and synchronization. Lack of information on over-the-counter medications underestimates the usage rates for NSAIDs, PPIs, and other potential nephrotoxins. Data in CURE-CKD on sodium-glucose cotransporter 2 inhibitor use, recently recommended for diabetes and CKD, came from an era before this new indication. It will be important to follow this trend to ensure sodium-glucose cotransporter 2 inhibitors are delivered to patients who may benefit. Another limitation of EHR-based registries is undercoding and miscoding. To mitigate this limitation, patient-level data for laboratory values, vital signs, and prescriptions were used to classify CURE-CKD registry participants and their care, which allowed for the use of guideline-based criteria for persistence of low eGFR or elevated albuminuria or proteinuria levels. Although CURE-CKD produced a lower range estimate of overall CKD prevalence compared with other US reports, this prevalence rate is similar to that found in Canadian primary care. 4 , 32 A higher range estimate for CKD based solely on eGFR could be because of more frequent testing in patients with higher risk who were treated by both specialty and primary care practices at PSJH and UCLA Health. Ascertainment bias is an inherent limitation of EHR-based registries, and information about CKD will also be missed from patients receiving care elsewhere or not receiving testing. The actual prevalence of overall CKD likely lies between the low (4.8%) and high (22.6%) range estimations from CURE-CKD. Nevertheless, these detailed prevalence estimates are strengths that represent the complexity and composition of patients treated in typical US health care systems.
In conclusion, the CURE-CKD registry reveals a burgeoning number of patients with CKD and major risk factors of diabetes, hypertension, and prediabetes. Rates of identification and use of kidney protective agents were low, while nephrotoxin use was widespread, underscoring the pressing need for practice-based improvement in CKD prevention, recognition, and treatment. These real-world data lay the groundwork for the development of more effective strategies to deliver care that enhances wellness and survival for patients with and at risk for CKD.
Accepted for Publication: November 4, 2019.
Published: December 20, 2019. doi:10.1001/jamanetworkopen.2019.18169
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2019 Tuttle KR et al. JAMA Network Open .
Corresponding Author: Katherine R. Tuttle, MD, Providence St Joseph Health, Providence Medical Research Center, 105 W Eighth Ave, Ste 6050 W, Spokane, WA 99204 ( [email protected] ).
Author Contributions: Dr Tuttle had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Tuttle, Jones, Daratha, Nicholas, McPherson, Bell, Mangione, Norris.
Acquisition, analysis, or interpretation of data: Tuttle, Alicic, Duru, Jones, Daratha, McPherson, Neumiller, Bell, Norris.
Drafting of the manuscript: Tuttle, Alicic, Jones, Nicholas, McPherson, Norris.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Tuttle, Jones, Daratha, McPherson, Bell.
Obtained funding: Tuttle, Magione, Norris.
Administrative, technical, or material support: Tuttle, Alicic, Daratha, McPherson, Neumiller, Bell, Norris.
Supervision: Tuttle, Magione, Norris.
Conflict of Interest Disclosures: Dr Tuttle reported receiving personal fees from Eli Lilly and Co, Boehringer Ingelheim, AstraZeneca, Gilead Sciences, Goldfinch Bio, and Novo Nordisk outside the submitted work. Dr Nicholas reported receiving grants from Goldfinch Bio, Bayer, the US Centers for Disease Control and Prevention, and Terasaki Research Institute; serving as national leader of a phase 3 clinical trial for the George Clinical Institute of Global Health; and receiving consulting fees from Janssen Pharmaceuticals and Amgen outside the submitted work. Dr McPherson reported receiving grants from the US Department of Health and Human Services and US Centers for Disease Control and Prevention during the conduct of the study. Dr Norris reported receiving grants from the National Institutes of Health during the conduct of the study. No other disclosures were reported.
Funding/Support: The CURE-CKD registry was supported by institutional funding from Providence St Joseph Health and the University of California, Los Angeles. Dr Tuttle is supported by grants 4UL1TR00426-10, 1U2CDK114886-01, 1U54DK083912, and 2UC4DK101108-02 from the National Institutes of Health. Drs Tuttle and Alicic are supported by grants 5UM1DK100846-03 and 2U01DK10086-07 from the National Institutes of Health. Drs Tuttle, Alicic, Jones, Daratha, and McPherson are supported by grant 75D301-19-Q-69877 from the US Centers for Disease Control and Prevention. Drs Duru, Bell, Mangione, and Norris are supported by grant UL1TR000124 from the National Institutes of Health. Drs Duru, Mangione, and Norris are supported by grant P30AG021684-15S2 from the National Institutes of Health. Dr Nicholas is supported by grant UL1TRR001881 from the National Center for Advancing Translational Science. Dr McPherson is supported by grants P20MD006871, UG1DA013714, R01EY027476, N44DA162246, R01AA022070, R01AA020248, P60AA026112, R41AA026793, N44DA171210, and R01AG042467 from the National Institutes of Health and grant I01HX002518 from the US Department of Veterans Affairs. Dr Mangione is supported by the Barbara A. Levey and Gerald S. Levey Endowed Chair.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: Carol Miceli, BS, Robert Follett, BS, and Theona Tacorda, MS (Providence St Joseph Health), extracted data from electronic health records, and Art Gongora (Providence St Joseph Health) provided administrative support. They were compensated for their time.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

- Previous Article
- Next Article
Introduction
Ada/kdigo consensus statements, screening and diagnosis, comprehensive care, treatment targets and pharmacotherapy, conclusions, article information, diabetes management in chronic kidney disease: a consensus report by the american diabetes association (ada) and kidney disease: improving global outcomes (kdigo).
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Ian H. de Boer , Kamlesh Khunti , Tami Sadusky , Katherine R. Tuttle , Joshua J. Neumiller , Connie M. Rhee , Sylvia E. Rosas , Peter Rossing , George Bakris; Diabetes Management in Chronic Kidney Disease: A Consensus Report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care 1 December 2022; 45 (12): 3075–3090. https://doi.org/10.2337/dci22-0027
Download citation file:
- Ris (Zotero)
- Reference Manager
People with diabetes and chronic kidney disease (CKD) are at high risk for kidney failure, atherosclerotic cardiovascular disease, heart failure, and premature mortality. Recent clinical trials support new approaches to treat diabetes and CKD. The 2022 American Diabetes Association (ADA) Standards of Medical Care in Diabetes and the Kidney Disease: Improving Global Outcomes (KDIGO) 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease each provide evidence-based recommendations for management. A joint group of ADA and KDIGO representatives reviewed and developed a series of consensus statements to guide clinical care from the ADA and KDIGO guidelines. The published guidelines are aligned in the areas of CKD screening and diagnosis, glycemia monitoring, lifestyle therapies, treatment goals, and pharmacologic management. Recommendations include comprehensive care in which pharmacotherapy that is proven to improve kidney and cardiovascular outcomes is layered on a foundation of healthy lifestyle. Consensus statements provide specific guidance on use of renin-angiotensin system inhibitors, metformin, sodium–glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and a nonsteroidal mineralocorticoid receptor antagonist. These areas of consensus provide clear direction for implementation of care to improve clinical outcomes of people with diabetes and CKD.
Clinicians and patients refer to clinical practice guidelines to synthesize data and provide expert direction on diagnosis and treatment. Guidelines must be evidence-based, systematic, transparent, and explicit to offer credibility and impact implementation. They must also allow adaptation to local circumstances and provide mechanisms for updates over time.
A rapidly expanding number of clinical trials are advancing clinical care in the field of diabetes and chronic kidney disease (CKD). The American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO) each follow structured processes to assess these data and develop rigorous, evidence-based guidelines for adults with diabetes and CKD ( 1 , 2 ). Areas of consensus between the two guidelines therefore represent independent agreement on high priority areas of care.
The goal of this consensus report was to identify and highlight shared recommendations from the ADA 2022 Standards of Medical Care in Diabetes (hereafter called Standards of Care) and KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease ( 1 , 2 ). A joint writing group of ADA and KDIGO representatives convened to compare and contrast ADA and KDIGO recommendations. A series of virtual meetings were held from March 2021 through February 2022 to define scope, review published guidelines and supportive evidence, and jointly write and revise the consensus report. Meetings were cochaired by an ADA representative (G.B.) and a KDIGO representative (I.H.d.B.) and supported by both ADA and KDIGO staff.
Consensus statements were drafted when recommendations from each organization were aligned and supported by high-quality evidence from randomized clinical trials ( ada/kdigo consensus statements ). These statements do not specify a level of evidence, which can be found in the individual ADA and KDIGO documents. However, all consensus statements were endorsed by both the ADA and KDIGO and represent broad agreement on evidence-based management of adults with diabetes and CKD.
All patients with type 1 diabetes (T1D) or type 2 diabetes (T2D) and CKD should be treated with a comprehensive plan, outlined and agreed by health care professionals and the patient together, to optimize nutrition, exercise, smoking cessation, and weight, upon which are layered evidence-based pharmacologic therapies aimed at preserving organ function and other therapies selected to attain intermediate targets for glycemia, blood pressure (BP), and lipids.
An ACE inhibitor (ACEi) or angiotensin II receptor blocker (ARB) is recommended for patients with T1D or T2D who have hypertension and albuminuria, titrated to the maximum antihypertensive or highest tolerated dose.
A statin is recommended for all patients with T1D or T2D and CKD, moderate intensity for primary prevention of atherosclerotic cardiovascular disease (ASCVD) or high intensity for patients with known ASCVD and some patients with multiple ASCVD risk factors.
Metformin is recommended for patients with T2D, CKD, and estimated glomerular filtration rate (eGFR) ≥30 mL/min/1.73 m 2 ; the dose should be reduced to 1,000 mg daily in patients with eGFR 30–44 mL/min/1.73 m 2 and in some patients with eGFR 45–59 mL/min/1.73 m 2 who are at high risk of lactic acidosis.
A sodium–glucose cotransporter 2 inhibitor (SGLT2i) with proven kidney or cardiovascular benefit is recommended for patients with T2D, CKD, and eGFR ≥20 mL/min/1.73 m 2 . Once initiated, the SGLT2i can be continued at lower levels of eGFR.
A glucagon-like peptide 1 (GLP-1) receptor agonist with proven cardiovascular benefit is recommended for patients with T2D and CKD who do not meet their individualized glycemic target with metformin and/or an SGLT2i or who are unable to use these drugs.
A nonsteroidal mineralocorticoid receptor antagonist (ns-MRA) with proven kidney and cardiovascular benefit is recommended for patients with T2D, eGFR ≥25 mL/min/1.73 m 2 , normal serum potassium concentration, and albuminuria (albumin-to-creatinine ratio [ACR] ≥30 mg/g) despite maximum tolerated dose of renin-angiotensin system (RAS) inhibitor.
CKD occurring among people with diabetes is common, morbid, and costly. The International Diabetes Federation estimates that 537 million people were living with diabetes in 2021, with an expected increase to 784 million by the year 2045 ( 3 ). The prevalence of CKD among people with diabetes is >25%, and it has been estimated that 40% of people with diabetes develop CKD during their lifetime ( 4 ). As the prevalence of diabetes has increased, the prevalence of CKD attributable to diabetes has grown proportionally ( 4 ).
Diabetes is the most common cause of kidney failure requiring kidney transplantation or dialysis worldwide ( 5 ). In the U.S., diabetes fueled a marked increase in the prevalence of kidney failure over the last 30 years and now accounts for half of all new cases of kidney failure ( 6 ). Moreover, CKD markedly amplifies risks of ASCVD, heart failure (HF), cardiovascular death, and all-cause mortality among people with diabetes ( 7 , 8 ).
In the U.S., one of every five adults with diabetes is not aware of their diagnosis ( 9 ). Awareness of CKD is even lower, with 9 of 10 individuals unaware of having underlying CKD, including 2 of 5 with severe CKD ( 6 , 10 ). In addition, both diabetes and CKD disproportionately affect racial and ethnic minorities and older adults. Insufficient screening, diagnosis, and awareness impair efforts to implement treatment and improve outcomes and exacerbate racial, socioeconomic, and ethnic disparities. Furthermore, recent population-based data uncovering disparities in access to glucose-lowering agents with proven kidney and cardiovascular benefits further highlight the need for interventions that ensure more equitable access to and use of these pharmacotherapies across racial and ethnic minorities ( 11 ).
In the U.S., the total estimated cost of diagnosed diabetes in 2017 was $327 billion, including $237 billion in direct medical costs and $90 billion in reduced productivity ( 12 ). The estimated global direct health expenditure on diabetes in 2019 was $760 billion ( 13 ). CKD, with and without kidney failure, is a major driver of the cost of diabetes care. Costs of CKD, stroke, and heart disease are additive ( 14 , 15 ).
CKD is defined as persistent eGFR <60 mL/min/1.73 m 2 , albuminuria (ACR ≥30 mg/g), or other markers of kidney damage, such as hematuria or structure abnormalities. Importantly, these measurements can vary within individuals over time, and persistence for at least 3 months is therefore required for diagnosis ( 16 ).
For most people, CKD is not identified as a result of symptoms; CKD is often diagnosed through routine screening. Both the ADA and KDIGO recommend annual screening of patients with diabetes for CKD ( 17 , 18 ) ( Fig. 1 ). CKD screening should start at diagnosis of T2D because evidence of CKD is often already apparent at this time. For T1D, screening is recommended commencing 5 years after diagnosis, prior to which CKD is uncommon. Screening is underutilized, particularly for albuminuria. In typical practice in the U.S., less than half of patients with T2D are screened for albuminuria in a given year ( 19 ).

CKD screening and diagnosis for people living with diabetes. Screening includes measurement of both urine albumin and eGFR. Abnormalities should be confirmed. Persistent abnormalities in either urine ACR or eGFR (or both) diagnose CKD and should lead to immediate initiation of evidence-based treatments. ACR, albumin-to-creatinine ratio; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; T1D, type 1 diabetes; T2D, type 2 diabetes.
Clinical laboratories routinely report eGFR calculated from serum creatinine and demographic data ( 20 – 22 ). The American Society of Nephrology and National Kidney Foundation advocate using the 2021 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, which was generated without inclusion of a term for race and calculates eGFR without regard to race, to estimate glomerular filtration rate (GFR) from creatinine, age, and sex ( 20 ). Another CKD-EPI equation that additionally incorporates serum cystatin C increases precision and reduces racial and ethnic bias, offering additional value in screening and for confirmation of low eGFR in appropriate cases ( 23 – 25 ).
Calculation of the ACR in single-voided “spot” urine samples is most convenient to measure albuminuria. Early morning urine specimens are ideal, although samples collected any time of day may be used. ACR has marked variability; therefore, a confirmatory urine sample within 3–6 months is recommended ( 26 , 27 ).
KDIGO has codified a CKD classification scheme based on eGFR and albuminuria that is endorsed by the ADA ( 26 ). In cohort studies, risks of progressive CKD, cardiovascular events, and mortality all increase with categories of increasing albuminuria or decreasing eGFR. Moreover, CKD stage and corresponding risk category can guide frequency of laboratory monitoring, treatment, and referral to nephrology care ( Fig. 2 ).
![research articles on kidney disease Risk of CKD progression, frequency of visits, and referral to nephrology according to GFR and albuminuria. The numbers in the boxes are a guide to the frequency of screening or monitoring (number of times per year). Green reflects no evidence of CKD by eGFR or albuminuria, with screening indicated once per year. For monitoring of prevalent CKD, suggested monitoring varies from once per year (yellow) to four times or more per year (i.e., every 1–3 months, [deep red]) according to risks of CKD progression and CKD complications. These are general parameters only, based on expert opinion, and underlying comorbid conditions and disease state must be taken into account, as well as the likelihood of impacting a change in management for any individual patient. CKD, chronic kidney disease; GFR, glomerular filtration rate.](https://ada.silverchair-cdn.com/ada/content_public/journal/care/45/12/10.2337_dci22-0027/6/m_dci220027f2.png?Expires=1725611264&Signature=PjFec6cgGt2FhXMZXCC7JPTp05FTDPJW3YN~ppwv33I8RdUnCKSSTG9kcZR0hEXoLaRJDO18mOX46tjhKL97~Ap4BiGsz9oF118lL~ydGJKGlQN8fRvBdGAxjSofIOkh7CEVlkj-lWRSeSexiYZW3M8vYFHMMIhh0lEZOBtWa4ORNxjUeKPsYJgTGrAAT8aM-YW11GwSmMzb4I8SXYqtRgHKjPvTdGT2nEvYu5mCwZwnnSl4cq9OYo5tvMB3RTNTGcn1MM2UZYU8hWYmq4uvXe3-DGUKTjWxCcsqe6HMeWib5qxlXpewn--b~U1i0XYzHvjwJaXBTqoUmNDbBL4Siw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Risk of CKD progression, frequency of visits, and referral to nephrology according to GFR and albuminuria. The numbers in the boxes are a guide to the frequency of screening or monitoring (number of times per year). Green reflects no evidence of CKD by eGFR or albuminuria, with screening indicated once per year. For monitoring of prevalent CKD, suggested monitoring varies from once per year (yellow) to four times or more per year (i.e., every 1–3 months, [deep red]) according to risks of CKD progression and CKD complications. These are general parameters only, based on expert opinion, and underlying comorbid conditions and disease state must be taken into account, as well as the likelihood of impacting a change in management for any individual patient. CKD, chronic kidney disease; GFR, glomerular filtration rate.
A cause of CKD other than diabetes should be considered in the presence of other systemic diseases that cause CKD, when retinopathy is not present (particularly in T1D), or with CKD signs not common to diabetes (e.g., glomerular hematuria, large and abrupt changes in eGFR or albuminuria, or abnormal serology tests). In the absence of such “red flags,” CKD is usually attributed to diabetes and treated accordingly. Ongoing research seeks to define CKD subtypes with more granularity and link novel subtypes to precision treatments ( 28 , 29 ).
Goals of Comprehensive Care
Multimorbidity is common in patients with diabetes and CKD, who are at high risk of CKD progression, cardiovascular events, and premature mortality. Therefore, both the ADA ( 1 ) and KDIGO ( 2 ) emphasize the importance of comprehensive, holistic, patient-centered medical care to improve overall patient outcomes.
The goals of comprehensive care are to treat the patient as a “whole” person and incorporate coordinated multidisciplinary treatment, structured education to promote self-management, shared-decision making, and primary and secondary prevention of diabetes-related complications, including CKD, ASCVD, and HF ( 2 ). This approach requires treatment directed to optimize lifestyle, pharmacological therapy aimed at preserving organ function, and additional therapies aimed at improving intermediate risk factors such as glycemia, BP, and lipids ( Fig. 3 ).

Holistic approach for improving outcomes in patients with diabetes and CKD. Icons presented indicate the following benefits: BP cuff, BP lowering; glucometer, glucose lowering; heart, cardioprotection; kidney, kidney protection; scale, weight management. eGFR is presented in units of mL/min/1.73 m 2 . *ACEi or ARB (at maximal tolerated doses) should be first-line therapy for hypertension when albuminuria is present. Otherwise, dihydropyridine calcium channel blocker or diuretic can also be considered; all three classes are often needed to attain BP targets. †Finerenone is currently the only ns-MRA with proven clinical kidney and cardiovascular benefits. ACEi, angiotensin-converting enzyme inhibitor; ACR, albumin-to-creatinine ratio; ARB, angiotensin II receptor blocker; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CCB, calcium channel blocker; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; GLP-1 RA, GLP-1 receptor agonist; HTN, hypertension; MRA, mineralocorticoid receptor antagonist; ns-MRA, nonsteroidal mineralocorticoid receptor antagonist; PCSK9i, proprotein convertase subtilisin/kexin type 9 inhibitor; RAS, renin-angiotensin system; SGLT2i, sodium–glucose cotransporter 2 inhibitor; T1D, type 1 diabetes; T2D, type 2 diabetes.
With multiple interventions ubiquitously needed to optimize the care of people with diabetes and CKD, it is crucial to avoid therapeutic inertia ( 30 ). Most patients with diabetes and CKD have high residual risks of CKD progression and cardiovascular disease despite treatment, and increasing options are available for risk mitigation. Patients may need to be seen frequently to identify and implement multiple therapies, some of which may interact. For example, RAS inhibitors, SGLT2i, and the ns-MRA finerenone all cause initial hemodynamic reductions in GFR. When indicated, such medications may need to be added and adjusted sequentially, with frequent assessments to institute and optimize care in a timely manner. Empowering patients and facilitating multidisciplinary care can help institute and titrate multiple treatments expeditiously.
Consensus Statement
All patients with T1D or T2D and CKD should be treated with a comprehensive plan, outlined and agreed by health care professionals and the patient together, to optimize nutrition, exercise, smoking cessation, and weight, upon which are layered evidence-based pharmacologic therapies aimed at preserving organ function and other therapies selected to attain intermediate targets for glycemia, BP, and lipids.
Education, Self-care, and Patient Empowerment
The ADA and KDIGO guidelines both advocate for patients to take an active role in managing their diabetes and kidney disease and to have a voice in decisions that affect their well-being ( 2 , 31 ). Education for patients and an integrated approach to treatment is an effective approach for both patients and clinicians.
Patients know themselves better than anyone else, and although health care professionals have the medical background, when a patient and health care professional become partners in developing a shared-decision treatment plan the lives of the patients will improve. In addition, the time required by the health care professional in managing the patients care will be reduced. Patient priorities often do not align with health care professional priorities. Ideally, health care professionals will question patients about their priorities and together they will establish an agreed upon care program ( 32 ).
Ways in which patients can work with their health care professionals to manage their diabetes and CKD include asking questions; becoming educated about diet, physical activity, smoking cessation, glycemic control, and medications; talking to peers and support groups in the diabetes and CKD community; becoming familiar with technology that is available to track progress; and understanding test results in preparation for health care appointments ( 33 ).
Multidisciplinary Team Care
Diabetes and CKD management is ideal when the health care system model of care includes a multidisciplinary team to assist patients including the patient, physician (or other care provider), and other health care professionals ( 2 , 34 ). Both the ADA and KDIGO guidelines emphasize the importance of a team-based integrated approach that engages diabetes care and education specialists, physicians, nurse practitioners, physician assistants, nurses, dietitians, exercise specialists, pharmacists, dentists, podiatrists, and/or mental health professionals in the care of the patient, with multidisciplinary care models representing a key strategy to overcome barriers to effective management of patients with diabetes and CKD ( Fig. 4 ).

Overcoming barriers to management of CKD in patients with diabetes. Barriers such as low CKD awareness, high complexity of care, difficulties with adhering to increasingly complex treatment regimens, and low recognition and application of guideline-directed management all contribute to suboptimal management of patients with diabetes and CKD. Proposed strategies that may contribute to improved management of patients with diabetes and CKD include implementation of multidisciplinary models of care, structured risk mitigation strategies and education, multidisciplinary educational initiatives, harmonization of clinical practice guidelines, and provision of self-management programs for patients with diabetes and CKD.
Health care systems should include team-based care for patients and focus on both short- and long-term treatment plans. Lifestyle interventions for the patient must be included in determining an overall plan of care to ensure individual preferences are addressed and goals are established by all team members, especially the patient.
Behavioral evaluation should be considered in the initial assessment for all patients with diabetes. In addition, it should be considered in patients who are unable to meet goals in order to determine potential psychosocial barriers to treatment and self-management.
Both the ADA and KDIGO guidelines underscore the integral role of medical nutritional therapy, including adequate access to nutritional management from a specialty-trained registered dietitian nutritionist (RD/RDN), for optimal diabetes management ( Supplementary Table 1 ). The ADA and KDIGO guidelines both recommend individualized and balanced diets that are high in vegetables, fruits, and whole grains but are low in refined carbohydrates and sugar-sweetened beverages ( 1 , 2 ). Both guidelines also recommend a low-sodium diet (KDIGO <2,000 mg/day, ADA 1,500 to <2,300 mg/day), largely to control BP and reduce cardiovascular risk.
The ADA and KDIGO guidelines also recommend targeting a dietary protein intake of 0.8 g/kg/day, the same intake recommended by the World Health Organization for the general population. Higher protein intakes confer theoretical risk of enhancing kidney function decline ( 35 ). KDIGO performed a systematic review of randomized trials and found no conclusive evidence that restriction of dietary protein to levels <0.8 g/kg/day improves kidney or other health outcomes among people with diabetes and CKD ( 2 ). While the ADA and KDIGO are aligned in this regard, the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) has somewhat different recommendations, including restricting dietary protein to 0.55–0.60 g/kg/day (or lower with keto acid analog supplementation) for metabolically stable CKD patients without diabetes and to 0.6–0.8 g/kg/day for patients with diabetes and CKD ( 36 ). All recommendations call for higher levels of protein intake for patients with kidney failure treated with maintenance dialysis, who are often catabolic or malnourished (e.g., 1.0–1.2 g/kg/day).
The ADA and KDIGO guidelines also advise moderate to intense/vigorous physical activity with a cumulative duration of ≥150 min/week and avoidance of sedentary activity ( 1 , 2 ). In overweight or obese patients with diabetes, ADA and KDIGO show overall agreement with respect to achieving and maintaining healthy weight through diet, physical activity, and behavioral therapy ( Supplementary Table 1 ). Though specific evidence is low, smoking cessation is also strongly advised.
Glycemic Control
Metrics and frequency.
Both the ADA and KDIGO recommend twice-yearly glycemic assessment using glycated hemoglobin (HbA 1c ) among stable patients with T2D who are meeting treatment goals and quarterly assessment among those who are intensively managed, whose therapy has changed, or whose treatment goals are not met ( Supplementary Table 1 ). While both ADA and KDIGO focus on HbA 1c as the primary tool for assessing long-term glycemic control, both guidelines acknowledge limitations in its accuracy and precision as an indirect metric of glycemic status, particularly in advanced CKD (i.e., CKD stages G4 and G5 without kidney replacement therapy [KRT]) and kidney failure treated by dialysis, and the inability of HbA 1c to adequately capture glycemic variability and hypoglycemic events. Consequently, both guidelines emphasize the concurrent use of 1 ) HbA 1c as a metric upon which therapeutic targets are defined based on randomized controlled trial (RCT) data, 2 ) continuous glucose monitoring (CGM) to assess effectiveness and safety of treatment among patients at risk for hypoglycemia or to assess overall glycemia when HbA 1c is inaccurate, and 3 ) self-monitoring of blood glucose as a tool to guide medication adjustment, particularly in patients treated with insulin ( 37 ).
Individualized Targets
Both the ADA and KDIGO emphasize use of individualized glycemic targets that take into consideration key patient characteristics that may modify risks and benefits of intensive glycemic control ( Supplementary Table 1 ). Based on RCT data, KDIGO recommends an individualized HbA 1c target of <6.5% to <8.0% for patients with diabetes and CKD, with targets in this range having been associated with improvements in survival, cardiovascular outcomes, and microvascular end points, as well as lower risk of CKD progression. The ADA recommends a starting HbA 1c target of <7% to reduce microvascular complications in most nonpregnant adult patients with T1D and T2D without hypoglycemia risk, although with higher goals (i.e., <8%) acceptable for patients with limited life expectancy and in whom the harms of treatment may outweigh the benefits.
CGM and Diabetes Technology
Diabetes technology refers to the hardware, devices, and software that patients with diabetes use to manage their chronic disease and encompasses 1 ) insulin administered with syringe, pen, or pump; 2 ) blood glucose monitoring with meter or CGM; and 3 ) hybrid devices that monitor glucose and deliver insulin. The ADA and KDIGO guidelines highlight the important role of CGM technology in improving diabetes management as a tool to identify and correct glycemic derangements, prevent hypoglycemia, direct medication management, and guide medical nutritional therapy and physical activity, as well as its rapid evolution in affordability and accuracy ( 2 , 37 ) ( Supplementary Table 1 ). Furthermore, ADA and KDIGO underscore that CGM may provide an advantage in glycemic control assessment among patients with T1D, as well as patients with T2D using glucose-lowering therapies associated with hypoglycemia. Other technologies supported by the ADA include sensor-augmented pumps that suspend insulin when glucose is low or predicted to become low, as well as automated insulin delivery systems that increase and decrease insulin delivery based on sensor-derived glucose levels and trends.
BP Management
BP management is universally accepted as a critical goal for prevention of CKD progression, ASCVD, and HF. The ADA includes BP recommendations in each annual Standards of Care and published a position statement on diabetes and hypertension in 2017 ( 38 ). BP control was highlighted as a key component of comprehensive care in the KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease and KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease and addressed in more detail in the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease ( 39 ).
The ADA and KDIGO BP recommendations share many similarities, including a focus on proper BP measurement techniques, individualization of BP targets, and preferred drugs for treatment. Considerations for individualization of BP targets include both anticipated benefits (e.g., higher absolute benefit for patients with higher underlying cardiovascular or kidney disease risk) and potential risks (e.g., ability to tolerate pharmacotherapy without experiencing adverse effects).
For patients with diabetes, hypertension, and high cardiovascular risk (i.e., 10-year ASCVD risk ≥15%), the ADA advises a BP target of <130/80 mmHg if this target can be safely attained. For patients with diabetes, hypertension, and low cardiovascular risk (defined as those with 10-year ASCVD risk <15%), the ADA recommends a BP target of <140/90 mmHg (grade A recommendation) ( 40 ). The KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease recommends a target systolic BP of <120 mmHg with assessment via standardized guideline-recommended office measurement in CKD patients (grade 2B recommendation), based largely on a single, high-quality RCT that was conducted exclusively in people without diabetes ( 39 ). However, the KDIGO Blood Pressure Work Group outlined certain caveats with respect to safety considerations and/or limited evidence for this threshold in certain populations, including those with diabetes and CKD. All of these thresholds are proposed as starting places for individualization of targets ( 41 ).
With respect to preferred antihypertensive pharmacotherapies, there is consensus that an RAS inhibitor, i.e., an ACEi or ARB, should be initiated in patients with concomitant diabetes, hypertension, and albuminuria, with titration to the highest tolerated approved dose. This recommendation is based on RCTs where findings demonstrated decreased risk of CKD progression, for which patients with albuminuria are at elevated risk, with a maximally dosed RAS inhibitor compared with placebo or an active antihypertensive drug comparator ( 42 – 44 ). In a recent study in almost three million patients, investigators found that both classes performed similarly; however, the ARB was better tolerated ( 45 ). Dihydropyridine calcium channel blockers and thiazide-like diuretics are also recommended for patients with hypertension who do not have albuminuria, for whom cardiovascular events and mortality are more common than kidney failure. Multiple drugs are often required to control BP, and an RAS inhibitor, dihydropyridine calcium channel blockers, and diuretics can be combined to attain individualized BP targets ( Fig. 3 ).
An ACEi or ARB is recommended for patients with T1D or T2D who have hypertension and albuminuria, titrated to the maximum antihypertensive or highest tolerated dose.
Lipid Management
Statin therapy is a cornerstone of therapy for the primary and secondary prevention of ASCVD among people with diabetes and CKD. The 2013 KDIGO Clinical Practice Guideline for Lipid Management in Chronic Kidney Disease recommended statin initiation for most adults with diabetes and CKD who are not treated with dialysis ( 46 , 47 ). Specifically, this included 1 ) adults ≥50 years old with CKD and eGFR ≥60 mL/min/1.73 m 2 (grade 1B recommendation) and 2 ) adults aged 18–49 years with CKD with diabetes, known coronary heart disease, prior ischemic stroke, or estimated 10-year incidence of coronary heart disease death or nonfatal myocardial infarction >10% (grade 2A recommendation). These recommendations are based largely on results of the Study of Heart and Renal Protection (SHARP) trial of CKD ( 48 ). Additional evidence from subsequent trials was incorporated into recommendations in the 2022 ADA Standards of Care, which are endorsed by this consensus statement.
For primary prevention of ASCVD, the ADA recommends a moderate-intensity statin for all adults with diabetes aged 40–75 years, those aged 20–39 years with additional ASCVD risk factors (such as CKD), and, with individualized decision-making, those aged >75 years (who are not well represented in completed trials). An exception may be patients with kidney failure treated with dialysis for whom primary prevention of ASCVD events with a statin has been generally ineffective ( 47 , 49 , 50 ). High-intensity statin is recommended for secondary prevention for all patients with known ASCVD. For some patients, intensification of statin therapy (for primary prevention), addition of ezetimibe, or addition of a PCSK-9 inhibitor is recommend based on ASCVD risk and attained LDL cholesterol concentrations. For patients with high triglyceride or low HDL levels, intensification of lifestyle intervention, optimization of glycemic control, and then consideration of icosapent ethyl are advised ( 51 ) ( Supplementary Table 1 ).
A statin is recommended for all patients with T1D or T2D and CKD, moderate intensity for primary prevention of ASCVD or high intensity for patients with known ASCVD and some patients with multiple ASCVD risk factors.
Glucose-Lowering Agents in T2D and CKD
The ADA 2022 Standards Care and the KDIGO 2022 guideline recommend early initiation of metformin plus an SGLT2 inhibitor in most patients with T2D and CKD ( 2 , 17 ) ( Table 1 ). Additional glucose-lowering agents can then be added as needed to meet individualized glycemic targets based on patient-specific considerations ( 2 , 17 ) ( Table 2 ). Prescription of glucose-lowering medications may be limited by eGFR ( Table 3 ). Appropriate dose adjustment based on eGFR is important for medications that increase risk of side effects with low eGFR or undergo elimination through the kidney ( Table 4 ). When needed, careful use and titration of insulin and sulfonylurea agents is recommended to avoid hypoglycemia.
Key glucose-lowering agent recommendations for patients with T2D and CKD from ADA and KDIGO ( 2 , 17 )
| Medication class . | ADA 2022 Standards of Medical Care in Diabetes . | KDIGO 2022 Guideline for Diabetes Management in Chronic Kidney Disease . |
|---|---|---|
| Metformin | • 9.4a First-line therapy depends on comorbidities, patient-centered treatment factors, and management needs and generally includes metformin and comprehensive lifestyle modification (A). | • Recommendation 4.1.1: We recommend treating patients with T2D, CKD, and an eGFR ≥30 mL/min per 1.73 m with metformin (1B). |
| • Practice Point 4.1.3: Adjust the dose of metformin when the eGFR is <45 mL/min per 1.73 m , and for some patients when the eGFR is 45–59 mL/min per 1.73 m . | ||
| SGLT2i | • Consider use of SGLT2i for organ protection independent of baseline HbA , individualized HbA target, or metformin use. | • Recommendation 1.3.1: We recommend treating patients with T2D, CKD, and an eGFR ≥20 mL/min per 1.73 m with an SGLT2i (1A). |
| • 10.42 Among patients with T2D who have established ASCVD or established kidney disease, an SGLT2i or GLP-1 receptor agonist with demonstrated cardiovascular disease benefit is recommended as part of the comprehensive cardiovascular risk reduction and/or glucose-lowering regimens (A). | ||
| • 10.42a In patients with T2D and established ASCVD, multiple ASCVD risk factors, or diabetic kidney disease, an SGLT2i with demonstrated cardiovascular benefit is recommended to reduce the risk of MACE and/or HF hospitalization (A). | ||
| • 11.3a For patients with T2D and diabetic kidney disease, use of an SGLT2i in patients with an eGFR ≥20 mL/min/1.73 m and urinary albumin ≥200 mg/g creatinine is recommended to reduce CKD progression and cardiovascular events (A). | ||
| • 11.3b For patients with T2D and diabetic kidney disease, use of an SGLT2i is recommended to reduce CKD progression and cardiovascular events in patients with an eGFR ≥20 mL/min/1.73 m and urine albumin ranging from normal to 200 mg/g creatinine (B). | ||
| GLP-1 receptor agonists | • 10.42 Among patients with T2D who have established ASCVD or established kidney disease, an SGLT2i or GLP-1 receptor agonist with demonstrated cardiovascular disease benefit is recommended as part of the comprehensive cardiovascular risk reduction and/or glucose-lowering regimens (A). | • Recommendation 4.2.1: In patients with T2D and CKD who have not achieved individualized glycemic targets despite use of metformin and SGLT2i treatment, or who are unable to use those medications, we recommend a long-acting GLP-1 receptor agonist (1B). |
| Medication class . | ADA 2022 Standards of Medical Care in Diabetes . | KDIGO 2022 Guideline for Diabetes Management in Chronic Kidney Disease . |
|---|---|---|
| Metformin | • 9.4a First-line therapy depends on comorbidities, patient-centered treatment factors, and management needs and generally includes metformin and comprehensive lifestyle modification (A). | • Recommendation 4.1.1: We recommend treating patients with T2D, CKD, and an eGFR ≥30 mL/min per 1.73 m with metformin (1B). |
| • Practice Point 4.1.3: Adjust the dose of metformin when the eGFR is <45 mL/min per 1.73 m , and for some patients when the eGFR is 45–59 mL/min per 1.73 m . | ||
| SGLT2i | • Consider use of SGLT2i for organ protection independent of baseline HbA , individualized HbA target, or metformin use. | • Recommendation 1.3.1: We recommend treating patients with T2D, CKD, and an eGFR ≥20 mL/min per 1.73 m with an SGLT2i (1A). |
| • 10.42 Among patients with T2D who have established ASCVD or established kidney disease, an SGLT2i or GLP-1 receptor agonist with demonstrated cardiovascular disease benefit is recommended as part of the comprehensive cardiovascular risk reduction and/or glucose-lowering regimens (A). | ||
| • 10.42a In patients with T2D and established ASCVD, multiple ASCVD risk factors, or diabetic kidney disease, an SGLT2i with demonstrated cardiovascular benefit is recommended to reduce the risk of MACE and/or HF hospitalization (A). | ||
| • 11.3a For patients with T2D and diabetic kidney disease, use of an SGLT2i in patients with an eGFR ≥20 mL/min/1.73 m and urinary albumin ≥200 mg/g creatinine is recommended to reduce CKD progression and cardiovascular events (A). | ||
| • 11.3b For patients with T2D and diabetic kidney disease, use of an SGLT2i is recommended to reduce CKD progression and cardiovascular events in patients with an eGFR ≥20 mL/min/1.73 m and urine albumin ranging from normal to 200 mg/g creatinine (B). | ||
| GLP-1 receptor agonists | • 10.42 Among patients with T2D who have established ASCVD or established kidney disease, an SGLT2i or GLP-1 receptor agonist with demonstrated cardiovascular disease benefit is recommended as part of the comprehensive cardiovascular risk reduction and/or glucose-lowering regimens (A). | • Recommendation 4.2.1: In patients with T2D and CKD who have not achieved individualized glycemic targets despite use of metformin and SGLT2i treatment, or who are unable to use those medications, we recommend a long-acting GLP-1 receptor agonist (1B). |
The ADA issues an A level of evidence for clear or supportive evidence from well-conducted, generalizable randomized control trials that are adequately powered and a B level of evidence for supportive evidence from well-conducted cohort or case-control studies. KDIGO uses the GRADE framework, with 1A indicating a strong recommendation based on high-quality evidence and 1B indicating a strong recommendation based on moderate-quality evidence.
ADA recommendations 11.3a and 11.3b include updates made in September 2022 through ADA’s living Standards of Care guideline update process.
Considerations for selecting glucose-lowering agents in patients with T2D and CKD ( 2 , 17 )

Benefit supported by primary and secondary outcome data.
Benefit supported by secondary outcome data.
Benefit or risk is agent specific.
ASCVD, atherosclerotic cardiovascular disease; CKD, chronic kidney disease; DPP-4, dipeptidyl peptidase 4; GLP-1, glucagon-like peptide 1; SGLT2, sodium–glucose cotransporter 2.
Key monitoring and risk mitigation strategies for preferred glucose-lowering agents
| Medication . | Consideration . | Monitoring and/or risk mitigation strategies . |
|---|---|---|
| Metformin | Metformin-associated lactic acidosis | • Monitor eGFR with increasing frequency as eGFR falls to <60 mL/min/1.73 m |
| • Adjust metformin dose as appropriate per eGFR (see ) | ||
| • Consider dose reduction in the presence of conditions that predispose patients to hypoperfusion and hypoxemia for eGFR 45–59 mL/min/1.73 m | ||
| • Discontinue for eGFR <30 mL/min/1.73 m | ||
| • Institute a sick day protocol | ||
| B malabsorption | • Monitor patients for vitamin B deficiency when treated with metformin for >4 years | |
| SGLT2i | Genital mycotic infections | • Counsel on genital hygiene |
| Volume depletion | • Monitor for hypovolemia and consider proactive dose reduction of diuretics in patients at high risk | |
| • Hold SGLT2i during illness | ||
| Diabetic ketoacidosis | • Educate about signs/symptoms to facilitate early recognition | |
| • Monitor blood or urine ketones in the case of very high risk | ||
| • Institute a sick day protocol | ||
| • Maintain at least low-dose insulin in insulin-requiring individuals | ||
| Hypoglycemia | • Adjust background glucose-lowering agents (e.g., insulin or sulfonylureas) as appropriate | |
| GLP-1 receptor agonists | Nausea/vomiting/diarrhea | • Educate on tolerability and symptom recognition |
| • Start at lowest recommended dose and titrate slowly | ||
| Hypoglycemia | • Adjust background glucose-lowering agents (e.g., insulin or sulfonylureas) as appropriate |
| Medication . | Consideration . | Monitoring and/or risk mitigation strategies . |
|---|---|---|
| Metformin | Metformin-associated lactic acidosis | • Monitor eGFR with increasing frequency as eGFR falls to <60 mL/min/1.73 m |
| • Adjust metformin dose as appropriate per eGFR (see ) | ||
| • Consider dose reduction in the presence of conditions that predispose patients to hypoperfusion and hypoxemia for eGFR 45–59 mL/min/1.73 m | ||
| • Discontinue for eGFR <30 mL/min/1.73 m | ||
| • Institute a sick day protocol | ||
| B malabsorption | • Monitor patients for vitamin B deficiency when treated with metformin for >4 years | |
| SGLT2i | Genital mycotic infections | • Counsel on genital hygiene |
| Volume depletion | • Monitor for hypovolemia and consider proactive dose reduction of diuretics in patients at high risk | |
| • Hold SGLT2i during illness | ||
| Diabetic ketoacidosis | • Educate about signs/symptoms to facilitate early recognition | |
| • Monitor blood or urine ketones in the case of very high risk | ||
| • Institute a sick day protocol | ||
| • Maintain at least low-dose insulin in insulin-requiring individuals | ||
| Hypoglycemia | • Adjust background glucose-lowering agents (e.g., insulin or sulfonylureas) as appropriate | |
| GLP-1 receptor agonists | Nausea/vomiting/diarrhea | • Educate on tolerability and symptom recognition |
| • Start at lowest recommended dose and titrate slowly | ||
| Hypoglycemia | • Adjust background glucose-lowering agents (e.g., insulin or sulfonylureas) as appropriate |
eGFR, estimated glomerular filtration rate; GLP-1, glucagon-like peptide 1; SGLT2i, sodium–glucose cotransporter 2 inhibitor.
Dose adjustments for eGFR <45 mL/min/1.73 m 2 (information presented reflects the package inserts rather than guidance from this consensus report)

Glucose-lowering efficacy is reduced with SGLT2i as eGFR declines, but kidney and cardiovascular benefits are preserved.
Dapagliflozin is approved for use at 10 mg once daily with an eGFR of 25 to <45 mL/min/1.73 m 2 .
Initiation not recommended with eGFR <30 mL/min/1.73 m 2 for glycemic control or <20 mL/min/1.73 m 2 for HF. Higher dose can be used but is not effective for glucose lowering and does not offer further clinical benefit in this range of eGFR.
Dulaglutide, liraglutide, and injectable semaglutide have demonstrated evidence of cardiovascular benefit in large cardiovascular outcome trials.
CV, cardiovascular; DPP-4, dipeptidyl peptidase 4; GFR, estimated glomerular filtration rate; GLP-1, glucagon-like peptide 1; SGLT2, sodium–glucose cotransporter 2.
Metformin is recommended for use in most patients with T2D and CKD who have eGFR ≥30 mL/min/1.73 m 2 , although careful patient selection and downward dose adjustment based on eGFR is recommended. Metformin has been proven to be a safe, effective, and affordable foundation for glycemic control in T2D. Metformin is excreted unchanged in urine, with the label including a boxed warning for increased risk of lactic acidosis in patients with CKD due to impaired metformin excretion ( 52 ). Evidence, however, suggests the overall risk for metformin-associated lactic acidosis is low ( 53 ), and the U.S. Food and Drug Administration has revised the U.S. label to reflect its safety in most patients with eGFR ≥30 mL/min/1.73 m 2 ( 52 ). In facilitating safe use, eGFR should be monitored at least annually in patients with CKD, with the recommended frequency of monitoring increased to every 3–6 months once eGFR falls <60 mL/min/1.73 m 2 ( 2 ) ( Fig. 1 ). It is recommended that the dose of metformin be reduced to 1,000 mg daily in patients with eGFR between 30 and 44 mL/min/1.73 m 2 , and a reduction should also be considered in patients with eGFR of 45–59 mL/min/1.73 m 2 if they have a comorbidity that places them at increased risk of lactic acidosis due to hypoperfusion and hypoxemia ( 2 ). Most episodes of metformin-associated lactic acidosis occur concurrent with other acute illness, often when acute kidney injury (AKI) contributes to reduced metformin clearance. Therefore, sick day protocols that specify holding metformin doses during acute illness may help reduce the risk of metformin-associated lactic acidosis.
Metformin is recommended for patients with T2D, CKD, and eGFR ≥30 mL/min/1.73 m 2 ; the dose should be reduced to 1,000 mg daily for patients with eGFR 30–44 mL/min/1.73 m 2 and for some patients with eGFR 45–59 mL/min/1.73 m 2 who are at high risk of lactic acidosis.
SGLT2i are recommended in most patients with T2D and CKD with eGFR ≥20 mL/min/1.73 m 2 independent of HbA 1c or the need for additional glucose lowering ( 2 , 17 ). This recommendation is based on strong evidence that SGLT2i reduce CKD progression, HF, and ASCVD risk in patients with T2D and CKD. These benefits are independent of glycemia, and an SGLT2i should be used for patients with T2D and CKD even if glycemic targets are already attained. While an SGLT2i will usually be added to lifestyle and metformin therapy, SGLT2i treatment without metformin may be reasonable for patients with eGFR too low for safe prescription of metformin, who do not tolerate metformin, or who do not need metformin to achieve glycemic targets.
To date, two clinical trials with primary kidney disease outcomes using canagliflozin and dapagliflozin (Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation [CREDENCE] and Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease [DAPA-CKD]) demonstrated significant benefit for composite outcomes including end points of substantial eGFR decline, kidney failure, and mortality ( 54 , 55 ). These trials enrolled participants with albuminuria (ACR ≥300 mg/g and ≥200 mg/g, respectively); therefore, current evidence is strongest in this population, as emphasized by ADA recommendations ( 17 ) ( Table 1 ). Evidence from combined major SGLT2i trials, however, suggests that kidney and cardiovascular benefits are consistent irrespective of baseline albuminuria ( 56 ), including in patients with normal albumin excretion, as reflected in the KDIGO recommendation and consensus statement supporting SGLT2i use in most patients with T2D and CKD ( 2 ).
The lower limit of eGFR for which initiation of SGLT2i is recommended has changed over time as new data have rapidly become available. The KDIGO 2022 guideline recommended initiation of an SGLT2i for patients with T2D and CKD who have eGFR ≥20 mL/min/1.73 m 2 (a change from ≥30 mL/min/1.73 m 2 in the 2020 guideline), and the ADA has also updated this threshold to ≥20 mL/min/1.73 m 2 in its living Standards of Care (from ≥25 mL/min/1.73 m 2 in the initial issue of the 2022 Standards of Care). These changes are driven largely by findings of new trials, including the DAPA-CKD trial (which provided clear evidence of efficacy and safety for dapagliflozin in patients with eGFR ≥25 mL/min/1.73 m 2 and ACR ≥200 mg/g) and the Empagliflozin Outcome Trial in Patients With Chronic Heart Failure (EMPEROR) trials (which provided clear evidence of efficacy and safety for empagliflozin among patients with eGFR ≥20 mL/min/1.73 m 2 and HF) ( 54 , 57 , 58 ). Additional support comes from subgroup analyses of participants in the CREDENCE and DAPA-CKD trials with baseline eGFR <30 mL/min/1.73 m 2 ( 59 , 60 ). Based on these results, direct evidence supporting initiation of an SGLT2i for patients with T2D and eGFR 20–29 mL/min/1.73 m 2 is strongest for patients with concomitant albuminuria or HF, though the efficacy and safety of SGLT2i are generally consistent among trial participants with or without these conditions ( 56 , 61 , 62 ). Moreover, SGLT2i have been observed to have consistent efficacy and safety across studied ranges of eGFR ( 56 ). Therefore, an SGLT2i can be initiated for most patients with T2D, CKD, and eGFR ≥20 mL/min/1.73 m 2 . Further data are anticipated from the EMPA-KIDNEY trial (EMPA-KIDNEY: The Study of Heart and Kidney Protection with Empagliflozin [clinical trial reg. no. NCT03594110, ClinicalTrials.gov ]), where entry criteria was expanded to include nonalbuminuric CKD with an eGFR initiation threshold ≥20 mL/min/1.73 m 2 , among >6,600 participants with or without T2D. Like CREDENCE and DAPA-CKD, EMPA-KIDNEY was stopped early for clear positive efficacy ( 63 ); corresponding expansion of the indications for use of an SGLT2i in CKD may be further supported based on these findings.
SGLT2i initiation is associated with a reversible decline in eGFR, but this generally does not require drug discontinuation. In fact, SGLT2i use appears to protect patients from AKI ( 56 ). Notably, protocols for both CREDENCE and DAPA-CKD specified continuation of study drug when eGFR fell below initiation thresholds. Therefore, it is reasonable to continue therapy if the eGFR falls below the initiation thresholds unless the patient is not tolerating treatment or KRT is initiated ( 2 ).
Hypovolemia and hypoglycemia may occur with SGLT2i, but absolute risks are low, especially at low eGFR. Therefore, adjustment of background therapies is generally not required when initiating an SGLT2i, but it may be prudent in some patients, and follow-up to reassess volume status and glycemia is important ( 64 ). Euglycemic ketoacidosis with minimal to no elevation in blood glucose may occur in patients taking SGLT2i. Patients with T2D requiring insulin are at particular risk. To mitigate risk, it is important to maintain at least low-dose insulin and consider pausing SGLT2i treatment during periods of acute illness or stressors. Blood or urine ketone monitoring may be used for ketosis detection. Patients with signs, symptoms, or biochemical evidence of ketoacidosis should discontinue SGLT2i therapy and seek immediate medical attention. Genital mycotic infections are a known complication of SGLT2i. A meta-analysis of clinical trials reported that genital mycotic infections occurred in 6% of participants assigned to an SGLT2i, compared with 1% of those assigned to placebo ( 65 ). The risk is higher for women than men. Daily hygienic measures may lessen this risk, and most genital mycotic infections are easily treated, but severe cases of Fournier gangrene have been reported. Additional research is needed to determine the role of SGLT2i in improving kidney outcomes in patients with T1D, among whom diabetic ketoacidosis is more common, and posttransplant, in which case immunosuppression may modify infection risks ( 66 ).
An SGLT2i with proven kidney or cardiovascular benefit is recommended for patients with T2D, CKD, and eGFR ≥20 mL/min/1.73 m 2 . Once initiated, the SGLT2i can be continued at lower levels of eGFR.
Use of Additional Glucose-Lowering Agents
For patients with T2D and CKD requiring additional glucose-lowering agents, selection should be made in consideration of patient- and medication-specific considerations ( Table 2 ). Addition of a long-acting GLP-1 receptor agonist is preferred as per KDIGO for patients not achieving individualized glycemic targets despite use of metformin and/or SGLT2i therapy or for individuals unable to take these medications ( 2 ). Similarly, the ADA gives strong support to use of GLP-1 receptor agonists in patients with T2D and CKD or ASCVD in consideration of their primary cardiovascular and secondary kidney benefits in large cardiovascular outcomes trials ( 17 ). Notably, GLP-1 receptor agonists retain glycemic efficacy and safety even in advanced CKD stages.
GLP-1 Receptor Agonists
GLP-1 receptor agonists reduce albuminuria and slow eGFR decline, as evidenced by secondary outcomes assessed in the cardiovascular outcomes trials and a clinical trial for glycemic efficacy and safety in patients with T2D and eGFR 15–59 mL/min/1.73 m 2 ( 2 ). In cardiovascular outcomes trials, GLP-1 receptor agonists reduced risk of major adverse cardiovascular events (MACE) in patients with T2D ( 67 – 70 ). Notably, the MACE risk reduction with liraglutide was significantly greater for those with eGFR <60 mL/min/1.73 m 2 than for those with eGFR ≥60 mL/min/1.73 m 2 ( 69 ). Although most participants in the cardiovascular outcomes trials of GLP-1 receptor agonists had established cardiovascular disease, the MACE reduction was similar between those with and without previous cardiovascular or kidney disease ( 71 ).
Although there has not been a completed kidney disease outcome trial for GLP-1 receptor agonists, the cardiovascular outcomes trials have included participants with eGFR as low as 15 mL/min/1.73 m 2 . The GLP-1 receptor agonists with favorable CKD outcomes include lixisenatide, exenatide (once weekly), liraglutide, semaglutide, albiglutide, dulaglutide, and efpeglenatide ( 67 , 68 , 70 , 72 – 76 ). In a meta-analysis of eight cardiovascular outcomes trials, GLP-1 receptor agonists significantly reduced risk for a composite kidney disease outcome (macroalbuminuria, eGFR decline, progression to kidney failure, or death from kidney disease) compared with placebo, largely driven by reduction in albuminuria ( 71 ). In a glycemic efficacy and safety trial in patients with moderate-to-severe CKD (CKD stages G3 and G4), dulaglutide was compared with insulin glargine as basal therapy ( 71 , 77 ). Dulaglutide produced similar glycemic control but resulted in significantly slower GFR decline. There is an ongoing clinical trial for a GLP-1 receptor agonist in T2D and CKD to evaluate whether semaglutide will prevent ≥50% eGFR decline, kidney failure, or death due to kidney or cardiovascular causes (clinical trial reg. no. NCT03819153, ClinicalTrials.gov ).
Nausea, vomiting, and diarrhea are the most common side effects of GLP-1 receptor agonists. These symptoms occur in 15–20% of patients with moderate-to-severe CKD (CKD stages G3 and G4) but usually are tolerable with dose titration and abate over several weeks to months ( 77 ). Injection site reactions are rare (<1%), and semaglutide is now available in an oral formulation. Heart rate typically increases by ∼5 bpm but has not been associated with higher BP or other adverse events. GLP-1 receptor agonist treatment is not recommended in patients at risk for thyroid C-cell tumors (e.g., multiple endocrine neoplasia), pancreatic cancer, or pancreatitis based on theoretical risks from preclinical models ( 1 ).
GLP-1 receptor agonists that have shown cardiovascular and CKD benefits (liraglutide, semaglutide, albiglutide [not currently available], and dulaglutide) are preferred agents. GLP-1 receptor agonists do not cause hypoglycemia per se but, when used with insulin or insulin secretagogues, doses of these drugs may be reduced to avoid hypoglycemia. However, in moderate-to-severe CKD (CKD stages G3 and G4), rates of hypoglycemia are reduced by one-half even with concurrent insulin therapy ( 77 ).
GLP-1 receptor agonist with proven cardiovascular benefit is recommended for patients with T2D and CKD who do not meet their individualized glycemic target with metformin and/or an SGLT2i or who are unable to use these drugs.
Glycemic Management in Advanced CKD (eGFR <30 mL/min/1.73 m 2 With or Without KRT)
Glycemic management is particularly challenging for patients with eGFR <30 mL/min/1.73 m 2 , including those treated with dialysis, because of restrictions on drug use ( Table 4 ) and lack of high-quality RCTs in this population.
For T1D, insulin remains the only approved therapy. Doses are titrated to achieve individualized glycemic goals but may need to be decreased in comparison with earlier stages of CKD due to reduced insulin clearance and other changes in metabolism with advanced CKD ( 78 ).
In T2D, advanced CKD is a risk factor for hypoglycemia ( 29 , 79 ) and, when possible, drugs that control glycemia without increasing risk of hypoglycemia are preferred. Metformin is contraindicated with eGFR<30 mL/min/1.73 m 2 and with dialysis treatment. SGLT2i can be initiated with eGFR 20–29 mL/min/1.73 m 2 and continued at lower eGFR if previously initiated and well tolerated. However, SGLT2i have minimal effects on glycemia in this range of eGFR and are of use mainly for kidney and cardiovascular benefits not mediated through glycemia.
GLP-1 receptor agonists have been studied with eGFR as low as 15 mL/min/1.73 m 2 and retain glucose-lowering potency across the range of eGFR and among dialysis patients. GLP-1 receptor agonists reduced ASCVD events and albuminuria in large RCTs and, thus, are theoretically appealing for people with T2D and CKD but have not been prospectively tested for cardiovascular efficacy or safety in this population. However, findings of a meta-analysis of the cardiovascular outcomes trials showed that ASCVD risk was reduced at least as much among individuals with eGFR <60 mL/min/1.73 m 2 compared with those with higher eGFR ( 71 ). GLP-1 receptor agonists induce weight loss and can cause nausea and vomiting, so caution is warranted among patients with or at risk for malnutrition. Notably, in people with T2D and advanced CKD who have obesity exceeding BMI limits required for kidney transplant listing, GLP-1 receptor agonists can be used to aid with weight loss that may facilitate qualification for transplant.
Selected dipeptidyl peptidase 4 inhibitors can be used with eGFR <30 mL/min/1.73 m 2 and in dialysis ( Table 4 ) and provide a safe and effective option for treatment of patients who are not treated with GLP-1 receptor agonists. Thiazolidinediones improve insulin sensitivity, a common abnormality in advanced CKD, and retain antihyperglycemic effects in this population. Fluid retention and HF are concerns with low eGFR and require careful monitoring. Insulin and short-acting sulfonylureas are often necessary to control glucose when medications with less propensity to cause hypoglycemia are contraindicated, not tolerated, unavailable, or insufficient.
Glycemic Management for Patients With a Kidney Transplant
Patients with a kidney transplant have been excluded from most clinical trials of glucose-lowering therapy. Therefore, data must be extrapolated from general populations with diabetes, with consideration of differences in diabetes pathophysiology (i.e., posttransplant diabetes) and unique aspects of treatment (such as immunosuppressive medications). High-quality trial data are needed for this population.
For T2D and posttransplant diabetes, it is reasonable to treat kidney transplant recipients with metformin according to eGFR, as for the broader population with T2D, because risks of metformin are related to kidney function ( 80 – 84 ). SGLT2i are promising drugs for kidney transplant recipients because they reduce intraglomerular pressure, which may be elevated in single functional kidneys, and may improve graft outcomes through this and other mechanisms. However, these benefits have not been confirmed in clinical trials, and there is a theoretical concern that infection risks (i.e., genital mycotic infections, urinary tract infections, Fournier gangrene) may be increased due to immunosuppression. Therefore, more data are needed prior to making recommendations for or against treatment with SGLT2i for kidney transplant recipients. Kidney transplantation and its treatments do not substantially modify the known risks and benefits of other glucose-lowering medications, other than restrictions associated with eGFR.
Renin-Angiotensin-Aldosterone System Inhibition
Ace inhibitors and arbs.
RAS inhibition with ACEi or ARBs has been standard of care in patients with T1D and T2D and CKD for decades. ACEi or ARBs are the preferred first-line agent for BP treatment among patients with diabetes, hypertension, and ACR ≥300 mg/g because of their proven benefits for prevention of CKD progression. In the setting of lower levels of albuminuria (30–299 mg/g), ACEi or ARB therapy has been demonstrated to reduce progression to more advanced albuminuria (≥300 mg/g) and cardiovascular events but not progression to kidney failure. Therefore, both KDIGO and the ADA recommend an ACEi or ARB for treatment of hypertension among people with T1D or T2D who have hypertension and ACR ≥30 mg/g ( 1 , 2 ).
Rarely, patients with albuminuria have normal BP, and in this situation, evidence for treatment with RAS inhibition is less strong. Although short-term studies demonstrated added benefit of the combination of ACEi and ARBs in albuminuria reduction, long-term studies showed no benefit and more adverse events, particularly hyperkalemia and AKI, and thus avoidance of this combination is recommended.
The steroidal mineralocorticoid receptor antagonist spironolactone is effective for management of resistant hypertension and treatment of primary hyperaldosteronism, in the setting of normal eGFR. Additionally, spironolactone reduces mortality in patients with HF with reduced ejection fraction. However, spironolactone causes hyperkalemia, particularly with reduced kidney function (i.e., eGFR <45 mL/min/1.73 m 2 ). There are no long-term kidney outcome studies with spironolactone, and only one study in heart failure with reduced ejection fraction with a mean follow-up of 2 years that showed benefit.
A novel class of ns-MRAs, including esaxerenone and finerenone, has recently been investigated among people with T2D and CKD, added to RAS inhibition. Esaxerenone lowered BP and albuminuria with limited changes in potassium, but long-term studies with clinical end points are lacking ( 85 ). Finerenone was investigated in two complementary phase 3 studies of patients with T2D, kidney disease (defined primarily as ACR ≥30 mg/g), and potassium <4.8 mmol/L and is the only ns-MRA approved in the world for slowing CKD progression and reducing cardiovascular events. In Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease (FIDELIO-DKD), both the primary kidney end point of progression of kidney disease (40% decline in eGFR or kidney failure) and the prespecified secondary composite cardiovascular end point (MACE or hospitalization for HF) were reduced with finerenone compared with placebo. Serum potassium was monitored regularly, and 2.6% of participants stopped treatment because of hyperkalemia with finerenone compared with 0.9% on placebo ( 86 ). In Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease (FIGARO-DKD), the primary composite cardiovascular end point (MACE or hospitalization for HF) was reduced with finerenone compared with placebo, with estimates of effect for kidney outcomes and hyperkalemia similar to those seen in FIDELIO-DKD ( 87 ).
Findings from the FIDELITY (Finerenone in Chronic Kidney Disease and Type 2 Diabetes: Combined FIDELIO-DKD and FIGARO-DKD Trial Programme Analysis) individual patient, prespecified combined analysis of both trials (13,191 total participants) demonstrated significant reductions of 18% for the composite cardiovascular outcome; 23% for a composite outcome of doubling of creatinine, kidney failure, or renal death; and 20% for dialysis initiation with a 22% reduction in HF hospitalizations ( 88 ). While <10% of participants were treated with an SGLT2i or a GLP-1 receptor agonist, results of subgroup analyses suggested that benefits of finerenone were similar with and without concomitant SGLT2i or GLP-1 receptor agonist treatment. Moreover, the risk of hyperkalemia was significantly reduced by the presence of an SGLT2i ( 89 ).
In summary, FIDELIO-DKD and FIGARO-DKD demonstrated cardiovascular and kidney benefits for finerenone among people with T2D who were treated with standard of care (including an RAS inhibitor at maximally tolerated doses and good control of glycemia and BP) who were at high residual risk, based largely on albuminuria (ACR ≥30 mg/g). These effects appear to be additive, based on preclinical studies, to those of SGLT2i and GLP-1 receptor agonists, though further clinical research on these combinations is needed. Therefore, it is reasonable to add finerenone to the treatment regimen of patients with T2D who have any level of persistent albuminuria despite current standard of care treatment with glucose-lowering and antihypertensive medications ( Fig. 3 ).
Finerenone can be initiated with eGFR ≥25 mL/min/1.73 m 2 (as per trial eligibility) and serum potassium 4.8 mmol/L (per trial eligibility criteria) or ≤5.0 mmol/L (as per U.S. Food and Drug Administration label). As per trial protocols, finerenone should be started at a dose of 20 mg daily for eGFR >60 mL/min/1.73 m 2 and 10 mg for eGFR 25–60 mL/min/1.73 m 2 and uptitrated to 20 mg daily if possible. Potassium should be followed 4 weeks after dose change and regularly during treatment. With potassium <4.8 mmol/L, dose can be uptitrated to 20 mg and continued with potassium ≤5.5 mmol/L. If potassium increases to >5.5 mmol/L, finerenone should be withheld and can be restarted at 10 mg daily when potassium is ≤5.0 mmol/L. Finerenone can be continued with eGFR <25 mL/min/1.73 m 2 as long as potassium is acceptable and the drug is otherwise tolerated.
An ns-MRA with proven kidney and cardiovascular benefit is recommended for patients with T2D, eGFR ≥25 mL/min/1.73 m 2 , normal serum potassium concentration, and albuminuria (ACR ≥30 mg/g) despite maximum tolerated dose of RAS inhibitor.
The 2022 ADA Standards of Care and KDIGO 2022 guideline are aligned on issues of CKD screening and diagnosis, glycemia monitoring, lifestyle therapies, treatment goals, and pharmacologic management ( 1 , 2 ). Both recommend comprehensive care in which pharmacotherapy that is proven to improve clinical kidney and cardiovascular outcomes is layered upon a foundation of healthy lifestyle approaches. This consensus approach to management is based on high-quality evidence. Randomized clinical trial data are most abundant for drug therapies, and other professional societies have also made similar recommendations for use of these agents.
Implementation of proven therapies is paramount to improving health outcomes. There is a critical need for patients with diabetes and CKD to be treated in accord with the most up-to-date recommendations. The ADA and KDIGO, individually and now in combination, offer clear guidance on applying and prioritizing interventions. High cost, limited workforce, and other resource constraints in health care systems will limit implementation of some recommendations among individuals and populations, and efforts to improve accessibility are essential to maximizing benefit and minimizing disparities.
Investigation remains active in the fields of diabetes, CKD, and cardiovascular disease, and additional data on existing and novel approaches are anticipated. Clinical practice guidelines will continue to evolve. When possible, consensus approaches to diagnosis and management will help interpret new data in context and translate discoveries to improved outcomes for patients.
This article contains supplementary material online at https://doi.org/10.2337/figshare.20272404 .
This article is featured in a podcast available at diabetesjournals.org/journals/pages/diabetes-core-update-podcasts .
This article is being simultaneously published in Diabetes Care and Kidney International . The articles are identical except for stylistic changes in keeping with each journal’s style. Either of these versions may be used in citing this article.
A consensus report of a particular topic contains a comprehensive examination and is authored by an expert panel (i.e., consensus panel) and represents the panel’s collective analysis, evaluation, and opinion. The need for a consensus report arises when clinicians, scientists, regulators, and/or policy makers desire guidance and/or clarity on a medical or scientific issue related to diabetes for which the evidence is contradictory, emerging, or incomplete. Consensus reports may also highlight gaps in evidence and propose areas of future research to address these gaps. A consensus report is not an American Diabetes Association (ADA) position but represents expert opinion only and is produced under the auspices of the ADA by invited experts. A consensus report may be developed after an ADA Clinical Conference or Research Symposium.
Duality of Interest. I.H.d.B.’s employer receives research support from Dexcom, and he has received honoraria from the ADA. He is a consultant to or advisory board member of AstraZeneca, Bayer, Boehringer Ingelheim, Cyclerion Therapeutics, George Clinical, Goldfinch Bio, and Ironwood Pharmaceuticals. He is also deputy editor for the Clinical Journal of the American Society of Nephrology . K.K.’s institution has received research grants from Boehringer Ingelheim, AstraZeneca, Novartis, Novo Nordisk, Sanofi, Lilly, and Merck Sharp & Dohme, and he is a consultant to Novo Nordisk, AstraZeneca, Sanofi, Servier, Merck Sharp & Dohme, Novartis, Abbott, Amgen, Bayer, Lilly, Roche, Berlin-Chemie AG/Menarini Group, and Boehringer Ingelheim. T.S.’s employer receives research support from Transplant House, and she has received honoraria from AstraZeneca. K.R.T. has received research grants from Goldfinch Bio, Bayer, and Travere Therapeutics. She is a consultant to or advisory board member of Eli Lilly, AstraZeneca, Boehringer Ingelheim, Gilead Sciences, Goldfinch Bio, Novo Nordisk, Bayer, and Travere Therapeutics. J.J.N. is an advisory board member for Novo Nordisk and Sanofi and is on Dexcom’s speakers bureau. C.M.R. has received a research grant from Dexcom and honoraria from AstraZeneca. She has also received funding from Fresenius Medical Care and ReCor Medical. S.E.R.’s employer receives research grants from Bayer, and she is a consultant to or advisory board member of Bayer, Relypsa, and Reata Pharmaceuticals. She is the president-elect of the National Kidney Foundation. P.R. has received research support from Novo Nordisk, AstraZeneca, Bayer, Gilead Sciences, Boehringer Ingelheim, Vifor Pharma, Mundipharma, Sanofi, Astellas Pharma, and Merck Sharp & Dohme. G.B. is a consultant to or advisory board member of Merck, Bayer, KBP Biosciences, Ionis Pharmaceuticals, Alnylam Pharmaceuticals, AstraZeneca, Quantum Genomics, Horizon Therapeutics, Novo Nordisk, DiaMedica Therapuetics, and inRegen. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. I.H.d.B. and G.B. were co-chairs for the consensus report writing group. J.J.N., C.M.R., and S.E.R. were the writing group members for the ADA. K.K., T.S., K.R.T., and P.R. were the writing group members for the KDIGO. All authors were responsible for drafting the report and revising it critically for important intellectual content. All authors approved the version to be published.
Email alerts
- Online ISSN 1935-5548
- Print ISSN 0149-5992
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Wednesday, July 19, 2023
New atlas of human kidney cells to help unlock kidney disease research
NIH-funded effort provides interactive resource for global research community.
In a major breakthrough toward understanding and treating kidney disease, a nationwide research team funded by the National Institutes of Health has created the most comprehensive atlas of the human kidney. Data from the Kidney Tissue Atlas will allow the comparison of healthy kidney cells to those injured by kidney disease, helping investigators understand the factors that contribute to the progression of kidney disease and kidney failure or recovery from injury. The atlas, part of the Kidney Precision Medicine Project (KPMP), was supported by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), as published in Nature .
Due to the complexity of the kidney, scientists have struggled to develop kidney models that accurately represent human kidney structures and function. The lack of human kidney models has limited the ability to develop new drugs to treat or prevent kidney disease.
The Kidney Tissue Atlas comprises maps of 51 main kidney cell types that include rare and novel cell populations, 28 kidney cellular states that represent injury or disease, a repository of raw gene data, and interactive 3D models of cells and microenvironment relationships created from 45 healthy donor kidneys and 48 kidney disease biopsies. The atlas thus establishes a critical foundation for KPMP’s overall goal to help discover new treatments for chronic kidney disease (CKD) and acute kidney injury (AKI), medical conditions that present a significant global health burden. The publicly available data created by KPMP, including all 3D renderings and analytical tools, can be accessed at atlas.kpmp.org .
“KPMP’s new atlas represents open, public science at its best,” said Dr. Eric Brunskill, KPMP program director in NIDDK’s Division of Kidney, Urologic, and Hematologic Diseases. “With the atlas, we’ve created an interactive, hypothesis-generating resource for kidney disease investigators and clinicians around the world.”
While CKD and AKI have historically been described as single, uniform diseases, KPMP builds on growing consensus that kidney disease can have several different root causes and disease pathways leading to subgroups of CKD and AKI. Instead of a “one size fits all” approach to treating kidney disease, precision medicine explores more personalized treatments. KPMP’s kidney atlas is intended to help identify disease subgroups within CKD and AKI, leading to the discovery of new, and possibly individualized, ways to treat CKD and AKI.
The study also received support from the Human Cell Atlas initiative, an international research effort to gather information on at least 10 billion human cells, and NIH’s Human BioMolecular Atlas Program (HuBMAP). HuBMAP’s goal is to develop an open and global platform to map healthy cells in the human body; the KPMP and HuBMAP teams worked closely to align the outputs of this molecular atlas as an example of cross-consortia collaborations.
“KPMP brings together the best of new technology, patient engagement, and partnership, and represents an evolution in the way we think about kidney disease,” said NIDDK Director Dr. Griffin P. Rodgers. “We’re confident the Kidney Tissue Atlas will help us discover new ways to get the right kidney disease treatment to the right patient at the right time.”
Data related to this research are available for request at the NIDDK Central Repository .
Research reported in this study was funded by NIDDK (grants U2C DK114886, UH3 DK114861, UH3 DK114866, UH3 DK114870, UH3 DK114908, UH3 DK114915, UH3 DK114926, UH3 DK114907, UH3 DK114923 and UH3 DK114933). The research was also supported by National Institute of Health (S10 OD026929), National Cancer Institute (P30 CA91842), and National Center for Advancing Translational Sciences (UL1 TR002345). HuBMAP is supported by NIH (OT2 D033760), National Heart, Lung, and Blood Institute (U54 HL145608), and NIDDK (U54 DK134301). Additional NIH support was provided by NIDDK (K08 DK107864, R01 DK111651, P01 DK056788, U2C DK114886, U54 DK083912, P30 DK081943, K23 DK125529, and U54 DK083912), National Institute of Mental Health (U01 MH114828), and National Cancer Institute (UH3 CA246632).
About the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): The NIDDK, a component of the National Institutes of Health (NIH), conducts and supports research on diabetes and other endocrine and metabolic diseases; digestive diseases, nutrition and obesity; and kidney, urologic and hematologic diseases. Spanning the full spectrum of medicine and afflicting people of all ages and ethnic groups, these diseases encompass some of the most common, severe, and disabling conditions affecting Americans. For more information about the NIDDK and its programs, see www.niddk.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Lake BB, et al. An atlas of healthy and injured cell states and niches in the human kidney . Nature. 2023.
Connect with Us
- More Social Media from NIH
- Frontiers in Nephrology
- Clinical Research in Nephrology
- Research Topics
New Advances and Updates in Inherited Cystic Diseases of the Kidney
Total Downloads
Total Views and Downloads
About this Research Topic
Understanding the genetic basis of kidney disease is important for identifying individuals at higher risk, implementing early interventions, and developing targeted therapies. Genetic testing and family history assessments can provide valuable information for assessing the genetic risk of kidney disease in certain individuals. Additionally, ongoing research in genomics and personalized medicine may lead to more effective strategies for the prevention and treatment of kidney diseases with a genetic component. To describe the genetic landscape of cystic kidney diseases and the recent advances in the identification of genetic disorders of the kidney. The focus will be on monogenic kidney disease, but a consideration of genetic modifiers of kidney disease and risk alleles will be given. To describe how personalised medicine approaches have led to novel therapies for genetic cystic kidney diseases. The scope includes summaries and reviews of different genetic disorders of the kidney including monogenic cystic disorders (autosomal dominant and recessive) as well as ciliopathy syndromes such as Bardet Biedl syndrome. The type of manuscripts will include case reports with literature reviews, reviews, commentary and basic research articles.
Keywords : cystic kidney disease, ciliopathies, genomic, genetic, personalised medicine
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines.
| Manuscript Summary | |
| Manuscript |
Participating Journals
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Effectiveness of educational interventions for nurses caring for patients with chronic kidney disease in improving nurse outcomes: A systematic review
Affiliations.
- 1 Nursing Division, Singapore General Hospital, Singapore, Singapore.
- 2 Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- PMID: 37953494
- DOI: 10.1111/jocn.16929
Aim: The aim of the study was to evaluate the effectiveness of educational interventions for nurses caring for patients with chronic kidney disease in improving knowledge, nurse-patient interaction, performance, skills competence and clinical decision-making.
Design: Systematic review.
Methods: Search of literature for randomised controlled trials, quasi-experimental studies and pre-experimental studies on chronic kidney disease-related educational interventions for nurses was conducted across 10 databases. Two reviewers independently screened articles, appraised studies and extracted data.
Data sources: PubMed, Cochrane, Embase, CINAHL Complete, ERIC, Social Science Database, ASSIA, Scopus, Web of Science and ProQuest Thesis and Dissertations Global databases were searched from date of inception to 21 December 2022.
Results: Three randomised controlled trials and eight pre-experimental studies were included in this review. Synthesis without meta-analysis was conducted due to high heterogeneity among studies. Interventions with teaching sessions, learning activities, self-study modules, discussion and a web-based training system were effective in improving nurses' knowledge, nurse-patient interaction, performance, skills competence and clinical decision-making. Patients experienced an improvement in nurse-patient interaction and no significant decrease in overall quality of life.
Conclusion: This review has shown the effectiveness of educational interventions for nurses caring for people with chronic kidney disease in improving outcomes for both nurses and patients, with sustained improvements up to a period of 1 year.
Implications for the profession and/or patient care: Study findings can guide the scope of future training for nurses caring for patients with chronic kidney disease.
Impact: Nurses often lack in-service training on how to improve care for patients with chronic kidney disease. This study found that training nurses on how to care for such patients can improve outcomes for nurses, which can translate to higher quality of patient care.
Reporting method: This paper adhered to the synthesis without meta-analysis (SWiM) reporting guideline.
Keywords: chronic kidney failure; nurse education; nurses; systematic review; training.
© 2023 John Wiley & Sons Ltd.
PubMed Disclaimer

Similar articles
- Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. Rees S, Williams A. Rees S, et al. JBI Libr Syst Rev. 2009;7(13):492-582. doi: 10.11124/01938924-200907130-00001. JBI Libr Syst Rev. 2009. PMID: 27819974
- Beyond the black stump: rapid reviews of health research issues affecting regional, rural and remote Australia. Osborne SR, Alston LV, Bolton KA, Whelan J, Reeve E, Wong Shee A, Browne J, Walker T, Versace VL, Allender S, Nichols M, Backholer K, Goodwin N, Lewis S, Dalton H, Prael G, Curtin M, Brooks R, Verdon S, Crockett J, Hodgins G, Walsh S, Lyle DM, Thompson SC, Browne LJ, Knight S, Pit SW, Jones M, Gillam MH, Leach MJ, Gonzalez-Chica DA, Muyambi K, Eshetie T, Tran K, May E, Lieschke G, Parker V, Smith A, Hayes C, Dunlop AJ, Rajappa H, White R, Oakley P, Holliday S. Osborne SR, et al. Med J Aust. 2020 Dec;213 Suppl 11:S3-S32.e1. doi: 10.5694/mja2.50881. Med J Aust. 2020. PMID: 33314144
- The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: a systematic review protocol. Sinclair P, Kable A, Levett-Jones T. Sinclair P, et al. JBI Database System Rev Implement Rep. 2015 Jan;13(1):52-64. doi: 10.11124/jbisrir-2015-1919. JBI Database System Rev Implement Rep. 2015. PMID: 26447007
- Education support services for improving school engagement and academic performance of children and adolescents with a chronic health condition. Barnett T, Tollit M, Ratnapalan S, Sawyer SM, Kelaher M. Barnett T, et al. Cochrane Database Syst Rev. 2023 Feb 8;2(2):CD011538. doi: 10.1002/14651858.CD011538.pub2. Cochrane Database Syst Rev. 2023. PMID: 36752365 Free PMC article. Review.
- Cultural competence education for health professionals. Horvat L, Horey D, Romios P, Kis-Rigo J. Horvat L, et al. Cochrane Database Syst Rev. 2014 May 5;2014(5):CD009405. doi: 10.1002/14651858.CD009405.pub2. Cochrane Database Syst Rev. 2014. PMID: 24793445 Free PMC article. Review.
- Andrade, C. (2019). The p value and statistical significance: Misunderstandings, explanations, challenges, and alternatives. Indian Journal of Psychological Medicine, 41(3), 210-215. https://doi.org/10.4103/ijpsym.ijpsym_193_19
- Antonini, M., Bellier-Teichmann, T., O'Reilly, L., Cara, C., Brousseau, S., Weidmann, J., Roulet-Schwab, D., Ledoux, I., Konishi, M., Pasquier, J., & Delmas, P. (2021). Effects of an educational intervention to strengthen humanistic practice on haemodialysis nurses' caring attitudes and behaviours and quality of working life: A cluster randomised controlled trial. BMC Nursing, 20, 255. https://doi.org/10.1186/s12912-021-00729-6
- Arsat, N., Chua, B. S., Wider, W., & Dasan, N. (2022). The impact of working environment on nurses' caring behavior in Sabah, Malaysia. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.858144
- Blue, C., Isringhausen, K., & Dils, E. (2011). Raising oral health awareness among nephrology nurses. Journal of Dental Hygiene, 85(2), 151-157.
- Bristol, T. J., Hagler, D., McMillian-Bohler, J., Wermers, R., Hatch, D., & Oermann, M. H. (2019). Nurse educators' use of lecture and active learning. Teaching and Learning in Nursing, 14(2), 94-96. https://doi.org/10.1016/j.teln.2018.12.003
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 06 August 2024
Impaired sensitivity to thyroid hormone correlates to all-cause mortality in euthyroid individuals with chronic kidney disease
- Qichao Yang 1 , 2 na1 ,
- Ru Dong 1 , 2 na1 ,
- Han Yan 1 , 2 ,
- Ruijun Xu 1 , 2 ,
- Yi Xue 1 , 2 ,
- Yong Yin 1 , 2 ,
- Zhiyong Zhao 1 , 2 &
- Zhaoxiang Wang 3
BMC Public Health volume 24 , Article number: 2134 ( 2024 ) Cite this article
Metrics details
This study aimed to investigate the association between central sensitivity to thyroid hormones and all-cause mortality in euthyroid patients with chronic kidney disease (CKD).
Data on thyroid function indicators and all-cause mortality for CKD patients were extracted from the NHANES database (2007–2012). Central sensitivities to thyroid hormones were mainly evaluated by Thyroid Feedback Quantile-based Index (TFQI). The Kaplan–Meier method, Cox proportional hazards regression model and subgroup analysis were performed to explore the potential associations between thyroid hormone sensitivity and all-cause mortality.
A total of 1303 euthyroid CKD patients were enrolled in this study. After a median follow-up of 115 months, 503 participants died. The Kaplan-Meier analysis demonstrated significant variations in survival rates among different levels of TFQI ( P = 0.0015). Cox regression analysis showed that increased levels of TFQI were independent risk factors for all-cause mortality after adjusting for multiple confounding factors (HR = 1.40, 95% CI 1.10–1.79, P = 0.007). Subgroup analysis did not reveal any significant variation in the association between TFQI and all-cause mortality between the subgroups assessed ( P for interaction > 0.05).
Our study suggests that impaired thyroid hormone sensitivity might be linked to increased mortality in euthyroid CKD patients. Further research is needed to confirm and explore this association.
Peer Review reports
Introduction
As one of the leading causes of death and suffering in the 21st century, chronic kidney disease (CKD) affects more than 10% of the general population worldwide, placing enormous economic and social pressure on the world [ 1 ]. Previous studies have shown that here is a bi-directional link between kidney and thyroid function [ 2 , 3 ]. Thyroid hormones directly or indirectly affect renal development, structure, hemodynamics, glomerular filtration rate, and water and electrolyte homeostasis [ 4 ]. The high burden of thyroid dysfunction, whether subclinical or overt, is closely associated with survival prognosis and adverse outcomes in patients with CKD [ 3 , 5 , 6 ]. Studies have shown that TSH levels in the abnormal range are associated with a higher risk of death for non-dialysis and dialysis-dependent CKD patients [ 6 , 7 ].
However, whether this risk extends to CKD patients with normal thyroid function remains controversial. One previous study suggested that a mild form of acquired thyroid hormone resistance may occur in the general population and accordingly proposed a new central thyroid hormone resistance index (Thyroid Feedback Quantile-based Index, TFQI) that focuses on deviations in the average pituitary inhibition to thyroid hormone in the population [ 8 ]. Thyroid hormone resistance can be systematically divided into central resistance which influences the feedback loop set point in the central nervous system and peripheral resistance which reduces hormone metabolism [ 9 , 10 ]. Compared to the latter, the former is easier to evaluate and can be quantified by looking at thyroid hormone and TSH concentrations or indicators derived from them [ 8 , 11 , 12 ]. One retrospective study found that decreased thyroid hormone sensitivity is associated with decreased renal function in normal thyroid function population, and that the composite index composed of TSH and free thyroxine (FT4) correlates more strongly to renal function than TSH or FT4 alone [ 13 ].
At present, it is uncertain whether changes in thyroid hormone sensitivity affect survival outcomes in patients with CKD. Therefore, we analyzed data from the National Health and Nutrition Examination Survey (NHANES) database (2007–2012) to explore the association between central thyroid hormone resistance index and the risk of all-cause death in CKD patients.
Study population
Data were obtained from NHANES, which is a periodic program designed to assess the health and nutrition status of adults and children in the United States administered by the National Center for Health Statistics (NCHS) [ 14 ]. NHANES is a stratified, multi-stage survey with good national representation and participants are selected at random through a complex statistical process each year. Our analysis finally comprised of a total of 1303 eligible participants, obtained by merging data from the NHANES cycles: 2007–2008, 2009–2010, and 2011–2012 (30,442 participants) (Fig. 1 ). All included participants were CKD (Stage 1–4) patients aged 20 and above, with complete thyroid function indicators and death data, and no history of pregnancy. The laboratory normality reference ranges were 7.74 − 20.64 pmol/L for FT4 and 0.34 − 5.60 mIU/L for TSH [ 15 ]. Those with abnormal TSH and FT4 levels were also excluded. Additionally, participants undergoing thyroid hormone replacement therapy (levothyroxine, thyroxine, thyroid desiccated, or other) and those with a history of thyroid disease were also excluded from the study.

Flow chart for participant identification and exclusion
Assessment of CKD
Age, gender, race, and serum creatinine (SCr) were used to evaluate estimated glomerular filtration rate (eGFR, ml/min/1.73 m 2 ) for each participant, according to the computational equations of the CKD Epidemiology Society (CKD-EPI) [ 16 ]. CKD was defined as eGFR < 60 mL/min/1.73 m 2 and/or urinary albumin to urinary creatinine ratio (UACR) ≥ 30 mg/g. The corresponding CKD stages were defined as: Stage 1, eGFR ≥ 90 mL/min/1.73 m 2 , along with UACR ≥ 30 mg/g; Stage 2, eGFR 60–89 mL/min/1.73 m 2 , along with UACR ≥ 30 mg/g; Stage 3, eGFR 30–59 mL/min/ 1.73m 2 ; Stage 4, eGFR 15–29 mL/min/ 1.73m 2 ; and Stage 5, eGFR < 15 mL/min/ 1.73m 2 [ 17 ]. We excluded these participants with CKD Stage 5 because it was not clear whether they were on dialysis.
Calculation of thyroid hormone sensitivity
The index reflecting thyroid central sensitivity were TSH T4 resistance index (TT4RI), TSH index (TSHI), and TFQI. TT4RI was calculated as FT4 (pmol/L) ⋅ TSH (mIU/L) [ 11 ]. TSHI = ln TSH (mIU/L) + 0.1345 ⋅ FT4 (pmol/L) [ 12 ]. The formula for calculating TFQI was cumulative distribution function (cdfFT4) – (1 – cdfTSH) [ 8 ]. FT4 and TSH concentrations were measured at the University of Washington using the two-step enzyme immunoassay and two-site immunoenzymatic (“sandwich”) assay, respectively.
Other variables
Data on other potential covariates employed in the statistical analyses included information on age, gender, race, smoking status, physical activity, annual household income, diabetes, hypertension, cardiovascular disease, body mass index (BMI, kg/m 2 ), alanine transaminase (ALT, U/L), aspartate transaminase (AST, U/L), gamma-glutamyl transferase (GGT, U/L), and glycohemoglobin. BMI is categorized into three groups: <25 kg/m 2 for normal weight, 25–29.9 kg/m 2 for overweight, and ≥ 30 kg/m 2 for obesity. Smokers are classified as current or former. Self-reported diabetes and hypertension are also defined, and the presence of cardiovascular disease is determined based on self-reported history of heart attack, stroke, congestive heart failure, coronary artery disease, or angina. Detailed measurement procedures for all variables in this study are publicly available in the NHANES database [ 15 ].
We utilized the NHANES Public-Use Linked Mortality File up to 31 December 2019, which employs a probabilistic algorithm to match with National Death Index (NDI) data for ascertaining mortality status [ 18 ]. The duration of follow-up for each participant was determined as the difference between the baseline examination date and the last known date alive or censored from the mortality file. The outcome of this study was all-cause mortality, encompassing deaths from all diseases, accidental incidents, and various other factors.
Statistical analysis
All statistical analyses were performed in accordance with Centers for Disease Control and Prevention (CDC) guidelines. A complex multistage cluster survey design was fully considered, and the corresponding weight values were applied. Continuous variables were presented as mean ± standard error and categorical variables were presented as proportions (standard error). Weighted Student’s t-test and chi-squared test were used to compare continuous and categorical variables in multiple groups, respectably. The Kaplan–Meier method was employed to estimate the survival among different TFQI levels, and the differences were evaluated with a stratified log-rank test. Cox regression model was employed to analyze the independent effects of various thyroid resistance indices (FT3/FT4, TT4RI, TSHI, and TFQI) on all-cause mortality in patients with CKD, using both unadjusted and fully adjusted models. The fully adjusted model accounted for multiple covariates, including age, gender, race, annual income, moderate physical activity, smokers, hypertension, diabetes, cardiovascular diseases, CKD stages, BMI, ALT, AST, GGT, and glycohemoglobin. Based on adjusted model, a restrictive cubic spline analysis was conducted to assess the relationship between the TFQI index and all-cause mortality risk in CKD patients, using the median values of the TFQI as the reference (HR = 1). Time-dependent Receiver Operating Characteristic (ROC) analyses using an unadjusted model were employed to evaluate clinical applicability. Subgroup analyses were performed on a priori basis, stratified by age, gender, race, BMI, hypertension, diabetes, cardiovascular diseases, and CKD stages. The Empower software ( http://www.empowerstats.com ) and R version 4.1.2 ( http://www.R-project.org ) were employed for all analyses. A P value ≤ 0.05 was considered statistically significant.
Characteristics of study population
The median follow-up period was 115 months. By December 31, 2019, 503 participants had died (Table 1 ). The deceased group was generally older, more often male, had lower annual income, were smokers, engaged in less moderate physical activity, and had higher levels of SCr, eGFR, UACR, FT4, TSH, and higher CKD stages ( P < 0.05). They also had a higher prevalence of hypertension, diabetes, and cardiovascular diseases ( P < 0.001). There were also significant differences in the distribution of race between the groups ( P = 0.001). The deceased group exhibited significantly lower FT3 levels ( P < 0.001). No significant differences in BMI, ALT, AST, and GGT were observed between the deceased and surviving groups ( P > 0.05). Importantly, the deceased group had higher TT4RI, TSHI, and TFQI levels compared to the surviving group ( P < 0.001).
Clinical features of the participants according to the tertiles of TFQI index
The weighted baseline characteristics based on the TFQI tertiles were also presented in Table 2 . Participants with higher TFQI levels exhibited significantly higher age, prevalence of obesity, diabetes, hypertension, cardiovascular disease, SCr, eGFR, CKD stages, FT4, TSH, TT4RI, and TSHI ( P < 0.05). FT3 levels were significantly lower ( P < 0.001). Notably, all-cause mortality was significantly higher with elevated TFQI tertiles, increasing from 26.61% in Tertile 1 to 40.89% in Tertile 3 ( P = 0.001). It was observed that TFQI values were associated with CKD stage, with more advanced stages of CKD associated with higher TFQI ( P < 0.001) (Fig. 2 ).

The levels of TFQI in different CKD stages
Survival analysis results based on TFQI tertiles
As shown in Fig. 3 , the Kaplan-Meier analysis revealed statistically significant differences in survival probability across the three TFQI levels. The analysis indicated the lowest survival in participants with high level of TFQI ( P = 0.0015).

Kaplan-Meier analysis results based on TFQI tertiles
The association between central thyroid hormone resistance index and all-cause death
Cox proportional hazards regression analysis confirmed that thyroid hormone indices were positively related with all-cause mortality among CKD patients (Table 3 ). In both fully adjusted and non-adjusted models, we found that TT4RI, TSHI and TFQI were positively associated with the risk of all-cause mortality. In fully adjusted models, the results indicated a 40% increased risk of death per unit increase in TFQI index (HR = 1.40, 95% CI 1.10–1.79, P = 0.007). Consistent with previous studies, we also discovered in CKD patients that peripheral thyroid hormone sensitivity (FT3/FT4) is associated with all-cause mortality (HR = 0.69, 95% CI 0.57–0.84, P < 0.001) [ 19 ]. Additionally, classification of TFQI into tertiles showed that higher TFQI teritles levels were associated with a higher prevalence of death ( P for trend = 0.050). Results of restrictive cubic strip analysis showed a positive relationship between TFQI and all-cause mortality among participants with CKD, with no significant threshold effect observed (Fig. 4 ). In the ROC analyses, TFQI in patients of 150 months follow-up duration showed a higher AUC (0.61) for predicting all-cause mortality compared to 120 months (0.58) and 60 months (0.58) (Fig. 5 ). Additionally, compared to TSHI and TT4RI, TFQI performed better at predicting mortality ( Attachment 1 ).

Restrictive cubic strip analysis results of TFQI and all-cause mortality

ROC curve analysis of TFQI in assessing death risk
Subgroup stratification analyses
The subgroup analyses in Fig. 6 demonstrated that the association of TFQI level and all-cause mortality is consistent after being stratified by age, gender, race, BMI, hypertension, diabetes, cardiovascular diseases, and CKD ( P for interaction > 0.05).

Subgroup analysis results based on age, gender, BMI, hypertension, diabetes, cardiovascular diseases, and CKD
We noted a strong association between TFQI and all-cause mortality among patients with stage 1–4 CKD in a representative sample of US adults on the NHANES 2007–2010 data. In this cohort study, we discovered a linear relationship between TFQI levels and all-cause mortality in CKD patients. After fully adjusting for confounding factors, increased levels of TFQI were independent risk factors for all-cause mortality (HR = 1.40, 95% CI 1.10–1.79, P = 0.007).
Previous studies have also revealed an association between FT4 levels within the normal range and the risk of all-cause mortality [ 19 , 20 ]. However, some studies have indicated that both the high-normal and low-normal TSH groups have a significantly higher risk of all-cause mortality compared to the mid-normal TSH group [ 21 , 22 ]. Based on negative feedback regulation, it seems difficult to fully explain this phenomenon, especially for the high-normal TSH. Hence, we attempted to elucidate this association from the perspective of central thyroid resistance. In individuals with normal thyroid function, the correlation between the assessment index based on thyroid hormone sensitivity and the risk of death is stronger than the assessment of individual indices alone [ 23 ]. This finding might partly explain the inconsistencies observed in previous studies, such as the nonlinear relationship between TSH levels and the risk of death and helps establish the link between thyroid function and all-cause mortality risk in CKD patients with normal thyroid function. Among the three indices for evaluating thyroid hormone central sensitivity, we found that TFQI has a stronger correlation with the risk of death. Previous studies have also indicated that in assessing abnormal response ranges of the thyroid to TSH, TFQI is more closely related to diabetes risk compared to TT4RI and TSHI [ 8 ]. We observed that in the time-dependent ROC analysis, the AUC for TFQI alone ranges from 0.58 to 0.61. Evaluating the predictive ability of TFQI in isolation may underestimate its true effect. A more comprehensive assessment of TFQI’s contribution can be achieved through multivariable analysis, which considers the incremental value of combining TFQI with other variables. Furthermore, the specific impact of TFQI should be evaluated within different clinical contexts and subjected to repeated validation across diverse populations to assess its value more objectively in predicting mortality.
The association between thyroid resistance index and mortality also has some reasonable biological mechanisms. Higher levels of FT4 within the reference range are associated with many adverse cardiac events, including heart failure, atrial fibrillation, and cardiac sudden death [ 24 , 25 , 26 ]. Elevated FT4 levels in the general population are also associated with an increased risk of solid tumors, including breast, prostate, lung, and ovarian cancers [ 23 , 27 ]. Despite the results of interaction tests not identifying specific populations, patients without hypertension, diabetes, or cardiovascular diseases appear to have a greater risk. Previous findings also indicated that reduced sensitivity to thyroid hormones serves as a risk factor for hypertension, diabetes, and cardiovascular diseases [ 8 , 28 , 29 ]. Therefore, we speculate that these diseases might partially mediate the link between thyroid hormone sensitivity and the risk of all-cause mortality. Additionally, the relatively small sample sizes in subgroups might also contribute to potential biases in the results. We also found that the impaired central sensitivity of the thyroid is related to the CKD stage, indicating that the impaired central sensitivity of the thyroid may itself be involved in the exacerbation of CKD. Thyroid hormones can directly participate in vascular and endothelial dysfunction and contribute to the formation of albuminuria [ 30 , 31 ]. Thyroid resistance may also induce changes in the immune microenvironment of kidney disease, thereby enhancing immune inflammatory responses, ultimately leading to kidney damage [ 32 ].
Our study has several limitations. First, the relatively small sample size and limited number of events available for analysis restrict the precision of the estimates and have prevented us from exploring specific analyses by causes of mortality that should be assessed in larger studies. Second, thyroid function was measured only at baseline, with no data on the changes in thyroid function over time. Thyroid-related antibodies, metabolic syndrome, and nonalcoholic fatty liver disease, as possible confounding factors, were not included in the study. Third, the mortality data we used was sourced from Public-use-files. Synthetic data were substituted for follow-up time or underlying cause of death, which to some extent hindered more in-depth analysis. Additionally, our study also did not consider the history of medication use that might affect thyroid function, such as beta blockers, steroids, and amiodarone. Finally, as our research used samples from people in the United States, the universal applicability of our results requires further validation.
Our study demonstrates that impaired sensitivity to thyroid hormone might be associated with all-cause mortality in CKD patients with normal thyroid function, independent of other traditional risk factors and comorbidities. The nature of this association is currently unclear and requires further research to confirm and explore.
Data availability
Data was collected from the NHANES database ( https://www.cdc.gov/nchs/nhanes/ ). Summary data supporting the study’s findings are available upon request from the corresponding author.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12(1):7–11. https://doi.org/10.1016/j.kisu.2021.11.003 .
Article PubMed Google Scholar
Rhee CM. The interaction between thyroid and kidney disease: an overview of the evidence. Curr Opin Endocrinol Diabetes Obes. 2016;23(5):407–15. https://doi.org/10.1097/med.0000000000000275 .
Article CAS PubMed PubMed Central Google Scholar
Narasaki Y, Sohn P, Rhee CM. The interplay between thyroid dysfunction and kidney disease. Semin Nephrol. 2021;41(2):133–43. https://doi.org/10.1016/j.semnephrol.2021.03.008 .
Article PubMed PubMed Central Google Scholar
Mariani LH, Berns JS. The renal manifestations of thyroid disease. J Am Soc Nephrol. 2012;23(1):22–6. https://doi.org/10.1681/asn.2010070766 .
Article CAS PubMed Google Scholar
Kang EW, Nam JY, Yoo TH, Shin SK, Kang SW, Han DS, Han SH. Clinical implications of subclinical hypothyroidism in continuous ambulatory peritoneal dialysis patients. Am J Nephrol. 2008;28(6):908–13. https://doi.org/10.1159/000141933 .
Rhee CM, Ravel VA, Streja E, Mehrotra R, Kim S, Wang J, Nguyen DV, Kovesdy CP, Brent GA, Kalantar-Zadeh K. Thyroid functional disease and mortality in a National Peritoneal Dialysis Cohort. J Clin Endocrinol Metab. 2016;101(11):4054–61. https://doi.org/10.1210/jc.2016-1691 .
Rhee CM, Kalantar-Zadeh K, Ravel V, Streja E, You AS, Brunelli SM, Nguyen DV, Brent GA, Kovesdy CP. Thyroid status and death risk in US Veterans with chronic kidney disease. Mayo Clin Proc. 2018;93(5):573–85. https://doi.org/10.1016/j.mayocp.2018.01.024 .
Laclaustra M, Moreno-Franco B, Lou-Bonafonte JM, Mateo-Gallego R, Casasnovas JA, Guallar-Castillon P, Cenarro A, Civeira F. Impaired sensitivity to thyroid hormones is Associated with Diabetes and metabolic syndrome. Diabetes Care. 2019;42(2):303–10. https://doi.org/10.2337/dc18-1410 .
Refetoff S, Weiss RE, Usala SJ. (1993) The syndromes of resistance to thyroid hormone. Endocr Rev 14(3): 348 – 99. https://doi.org/10.1210/edrv-14-3-348
Corica D, Licenziati MR, Calcaterra V, Currò M, Di Mento C, Curatola S, Zuccotti G, Alibrandi A, Ientile R, Aversa T, Wasniewska M. Central and peripheral sensitivity to thyroid hormones and glucose metabolism in prepubertal children with obesity: pilot multicenter evaluation. Endocrine. 2023;80(2):308–11. https://doi.org/10.1007/s12020-022-03276-5 .
Yagi H, Pohlenz J, Hayashi Y, Sakurai A, Refetoff S. Resistance to thyroid hormone caused by two mutant thyroid hormone receptors beta, R243Q and R243W, with marked impairment of function that cannot be explained by altered in vitro 3,5,3’-triiodothyroinine binding affinity. J Clin Endocrinol Metab. 1997;82(5):1608–14. https://doi.org/10.1210/jcem.82.5.3945 .
Jostel A, Ryder WD, Shalet SM. The use of thyroid function tests in the diagnosis of hypopituitarism: definition and evaluation of the TSH Index. Clin Endocrinol (Oxf). 2009;71(4):529–34. https://doi.org/10.1111/j.1365-2265.2009.03534.x .
Yang S, Lai S, Wang Z, Liu A, Wang W, Guan H. Thyroid feedback quantile-based Index correlates strongly to renal function in euthyroid individuals. Ann Med. 2021;53(1):1945–55. https://doi.org/10.1080/07853890.2021.1993324 .
Fain JA. NHANES Diabetes Educ. 2017;43(2):151. https://doi.org/10.1177/0145721717698651 .
The National Health and Nutrition Examination. Survey (NHANES) database. https://www.cdc.gov/nchs/nhanes/ . Accessed 10 Jan 2024.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006 .
Whaley-Connell AT, Sowers JR, Stevens LA, McFarlane SI, Shlipak MG, Norris KC, Chen SC, Qiu Y, Wang C, Li S, Vassalotti JA, Collins AJ. CKD in the United States: kidney early evaluation program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 Suppl 2):S13–20. https://doi.org/10.1053/j.ajkd.2007.12.016 .
The NHANES Public-Use Linked Mortality Database. https://www.cdc.gov/nchs/data-linkage/mortality-public.htm . Accessed 10 Jan 2024.
Lang X, Li Y, Zhang D, Zhang Y, Wu N, Zhang Y. FT3/FT4 ratio is correlated with all-cause mortality, cardiovascular mortality, and cardiovascular disease risk: NHANES 2007–2012. Front Endocrinol (Lausanne). 2022;13964822. https://doi.org/10.3389/fendo.2022.964822 .
Yuan D, Jia S, Zhu P, Zhang C, Liu Y, Liu R, Xu J, Tang X, Zhao X, Gao R, Yang Y, Xu B, Gao Z, Yuan J. Usefulness of FT3 to FT4 ratio to Predict Mortality in Euthyroid patients with Prior Cardiovascular events undergoing PCI: five-year findings from a large single-Center Cohort Study. Front Endocrinol (Lausanne). 2021;12700349. https://doi.org/10.3389/fendo.2021.700349 .
Zhu P, Lao G, Chen C, Luo L, Gu J, Ran J. TSH levels within the normal range and risk of cardiovascular and all-cause mortality among individuals with diabetes. Cardiovasc Diabetol. 2022;21(1):254. https://doi.org/10.1186/s12933-022-01698-z .
Inoue K, Tsujimoto T, Saito J, Sugiyama T. Association between serum thyrotropin levels and mortality among euthyroid adults in the United States. Thyroid. 2016;26(10):1457–65. https://doi.org/10.1089/thy.2016.0156 .
Alonso SP, Valdés S, Maldonado-Araque C, Lago A, Ocon P, Calle A, Castaño L, Delgado E, Menéndez E, Franch-Nadal J, Gaztambide S, Girbés J, Chaves F, Garcia-Serrano S, Garcia-Escobar E, Fernandez-García JC, Olveira G, Colomo N, Rojo-Martínez G. Thyroid hormone resistance index and mortality in euthyroid subjects: [email protected] study. Eur J Endocrinol. 2021;186(1):95–103. https://doi.org/10.1530/eje-21-0640 .
Cappola AR, Arnold AM, Wulczyn K, Carlson M, Robbins J, Psaty BM. Thyroid function in the euthyroid range and adverse outcomes in older adults. J Clin Endocrinol Metab. 2015;100(3):1088–96. https://doi.org/10.1210/jc.2014-3586 .
Chaker L, Heeringa J, Dehghan A, Medici M, Visser WE, Baumgartner C, Hofman A, Rodondi N, Peeters RP, Franco OH. Normal thyroid function and the risk of Atrial Fibrillation: the Rotterdam Study. J Clin Endocrinol Metab. 2015;100(10):3718–24. https://doi.org/10.1210/jc.2015-2480 .
Chaker L, van den Berg ME, Niemeijer MN, Franco OH, Dehghan A, Hofman A, Rijnbeek PR, Deckers JW, Eijgelsheim M, Stricker BH, Peeters RP. Thyroid function and sudden Cardiac death: a prospective Population-based Cohort Study. Circulation. 2016;134(10):713–22. https://doi.org/10.1161/circulationaha.115.020789 .
Krashin E, Piekiełko-Witkowska A, Ellis M, Ashur-Fabian O. Thyroid hormones and Cancer: a Comprehensive Review of Preclinical and Clinical studies. Front Endocrinol (Lausanne). 2019;1059. https://doi.org/10.3389/fendo.2019.00059 .
Mehran L, Delbari N, Amouzegar A, Hasheminia M, Tohidi M, Azizi F. Reduced sensitivity to thyroid hormone is Associated with Diabetes and Hypertension. J Clin Endocrinol Metab. 2022;107(1):167–76. https://doi.org/10.1210/clinem/dgab646 .
Sun Y, Teng D, Zhao L, Shi X, Li Y, Shan Z, Teng W. Impaired sensitivity to thyroid hormones is Associated with Hyperuricemia, obesity, and Cardiovascular Disease risk in subjects with subclinical hypothyroidism. Thyroid. 2022;32(4):376–84. https://doi.org/10.1089/thy.2021.0500 .
Yang Z, Duan P, Li W, Nie R, Lou X, Wang L, Wu K, Liu J, Tu P, Lai X. The correlation between thyroid hormone levels and the kidney disease progression risk in patients with type 2 diabetes. Diabetes Metab Syndr Obes. 2022;1559–67. https://doi.org/10.2147/dmso.S347862 .
Liu X, Li Y, Chai Y, Zhang Y, Zhang L, Zhang H. Thyroid function and thyroid homeostasis parameters are associated with increased urinary albumin excretion in euthyroid individuals over 60 years old from NHANES. Front Endocrinol (Lausanne). 2023;141285249. https://doi.org/10.3389/fendo.2023.1285249 .
Han Z, Chen L, Peng H, Zheng H, Lin Y, Peng F, Fan Y, Xie X, Yang S, Wang Z, Yuan L, Wei X, Chen H. The role of thyroid hormone in the renal immune microenvironment. Int Immunopharmacol. 2023;119110172. https://doi.org/10.1016/j.intimp.2023.110172 .
Download references
Acknowledgements
We want to acknowledge all participants of this study and the support provided by the Jiangsu University.
This study was funded by the Science and Technology Project of Changzhou Health Commission (WZ202226) and the Young Talent Development Plan of Changzhou Health Commission (CZQM2022029).
Author information
Qichao Yang and Ru Dong contributed equally to this work.
Authors and Affiliations
Department of Endocrinology, Affiliated Wujin Hospital of Jiangsu University, Changzhou, 213017, Jiangsu, China
Qichao Yang, Ru Dong, Han Yan, Ruijun Xu, Yi Xue, Yong Yin & Zhiyong Zhao
Department of Endocrinology, Wujin Clinical College of Xuzhou Medical University, Changzhou, 213017, Jiangsu, China
Department of Endocrinology, Affiliated Kunshan Hospital of Jiangsu University, Kunshan, 215300, Jiangsu, China
Zhaoxiang Wang
You can also search for this author in PubMed Google Scholar
Contributions
Q.Y. R.D. and Z.W. wrote the main manuscript text, H.Y. and R. X. prepared figures and tables. Y.X. and Y.Y. analyzed the data. All authors reviewed the manuscript.
Corresponding authors
Correspondence to Zhiyong Zhao or Zhaoxiang Wang .
Ethics declarations
Ethics approval and consent to participate.
The studies involving humans were approved by the Ethics Review Board of the National Center for Health Statistics. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: ROC analysis results
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Yang, Q., Dong, R., Yan, H. et al. Impaired sensitivity to thyroid hormone correlates to all-cause mortality in euthyroid individuals with chronic kidney disease. BMC Public Health 24 , 2134 (2024). https://doi.org/10.1186/s12889-024-19660-x
Download citation
Received : 19 December 2023
Accepted : 31 July 2024
Published : 06 August 2024
DOI : https://doi.org/10.1186/s12889-024-19660-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic kidney disease
- All-cause mortality
- Sensitivity to thyroid hormone
- Thyroid feedback quantile-based index
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Nephrol
- v.2023; 2023

The Growing Challenge of Chronic Kidney Disease: An Overview of Current Knowledge
1 Department of Nephrology, Zealand University Hospital Roskilde, Roskilde, Denmark
2 Institute of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Nicholas Carlson
3 Department of Nephrology, Rigshospitalet, Copenhagen, Denmark
4 Department of Research, The Danish Heart Foundation, Copenhagen, Denmark
Jens Søndergaard
5 Research Unit for General Practice, Department of Public Health, University of Southern Denmark, Odense, Denmark
Frederik Persson
6 Steno Diabetes Center Copenhagen, Herlev, Denmark
Associated Data
No data are available for this review.
Chronic kidney disease (CKD) is becoming one of the world's most prevalent noncommunicable chronic diseases. The World Health Organization projects CKD to become the 5th most common chronic disease in 2040. Causes of CKD are multifactorial and diverse, but early-stage symptoms are often few and silent. Progression rates are highly variable, but patients encounter both an increased risk for end-stage kidney disease (ESKD) as well as increased cardiovascular risk. End-stage kidney disease incidence is generally low, but every single case carries a significant burden of illness and healthcare costs, making prevention by early intervention both desirable and worthwhile. This review focuses on the prevalence, diagnosis, and causes of CKD. In addition, we discuss the developments in the general treatment of CKD, with particular attention to what can be initiated in general practice. With the addition of recent landmark findings and the expansion of the indication for using sodium–glucose cotransporter 2 inhibitors, there are now new effective treatments to add to standard therapy. This will also be relevant for primary care physicians as many patients with CKD have their family physician as their primary health care professional handling kidney function preservation. In the future, more precise and less invasive diagnostic methods may not only improve the determination of the underlying cause of CKD but may also carry information regarding which treatment to use (i.e. personalized medicine). This could lead to a reduced number of preventive treatments per individual, while at the same time improving the prognosis. This review summarizes ongoing efforts in this area.
1. Introduction
With this paper, we aim to provide an overview of chronic kidney disease with a focus on recent developments in treatment possibilities and the need for collaboration across healthcare sectors to improve detection, treatment, and prognosis.
The prevalence of chronic kidney disease (CKD) is increasing globally, with CKD projected to become the fifth most prevalent chronic condition by 2040 [ 1 ]. Global incidence and prevalence of CKD vary depending on divergent definitions of disease, different health care systems, social distributions, and risk factors for CKD, with the current standardized prevalence of CKD (eGFR < 60 ml/min/1.73 m 2 ) estimated to be 10–15% [ 2 – 4 ].
The impact of CKD is multifold. Progression towards end-stage kidney disease (ESKD) (the final stage of kidney failure, requiring either chronic dialysis or kidney transplantation) entails a concurrent substantial increase in the risk of cardiovascular disease. An analysis of the Kaiser Permanente Renal Registry ( n = 1,120,295) [ 5 ] found a marked increase in the age-standardized risk of death, cardiovascular events, and hospitalizations in individuals with an eGFR below 45 ml/min/1.73 m 2 . The risk of death from any cause was 0.76 per 100 person-years in individuals with eGFR above 60 ml/min/1.73 m 2 but was 4.76 per 100 person-years in individuals with eGFR between 30 and 44 ml/min/1.73 m 2 . In parallel, the risk of cardiovascular events was 2.11 per 100 person-years in individuals with eGFR above 60 ml/min/1.73 m 2 but was 11.29 per 100 person-years in individuals with eGFR between 30 and 44 ml/min/1.73 m 2 . This contributes to comorbidity and the burden of disease for many individuals with CKD, leading to an increase in both the number of medications and hospital visits. In a Scottish primary care study [ 6 ], it was demonstrated that 98.2% of adults with CKD had at least one comorbidity, versus 51.8% in controls. Hypertension, heart failure, diabetes, and coronary heart disease were found to be the most frequent concordant conditions. Furthermore, despite substantial improvement in both our understanding of the pathophysiology but also the treatment of cardiovascular risk and disease throughout the past decades, genuine advances in patients with advanced CKD including end-stage renal disease have remained elusive [ 7 ]. Plausibly, patients with advanced CKD have been systematically excluded from participation in large prospective clinical trials, leading to a lack of documentation of the benefit of treatment due to a paucity of evidence with implications direct for patient care [ 6 , 8 , 9 ].
Adding to the impact, the cost of renal replacement therapy (RRT), both dialysis and transplantation constitutes some of the most significant expenses in hospital-based health care. Based on annualized estimates of cost ascertained from national health care registers in Sweden, kidney disease is associated with a substantial economic burden, with costs elevated 4-fold, >10-fold, and >30-fold in patients with CKD, transplanted patients and patients on chronic dialysis, respectively [ 10 ]. The economic burden is predominantly driven by expenses related to excess hospitalization and dialysis treatment, each contributing >20% and >50% of total healthcare spending, respectively; with overall cost accounting for 1-2% of total healthcare spending in the UK [ 10 , 11 ]. The mean prevalence of end-stage renal disease treatment is currently 750 per million population globally, with the cost of treatment—and annual attributable cost of treatment—closely associated with the national income level per capita [ 12 ]. Notably, the prevalence of treated end-stage renal disease has increased globally in spite of stagnant incidence rates in developed countries; plausibly due to increasing incidences in developing countries, overall improvement in survival rates, demographic population shift, and growth in prevalence of risk factors for end-stage renal disease including diabetes [ 13 ].
Survival in end-stage kidney disease is poor, annual mortality is estimated to be >10%, with five-year survival at approximately 50%. Cardiovascular disease continues to be the largest sole contributor to excess mortality in patients with end-stage kidney disease, with the attributable risk of cardiovascular death estimated to be >20-fold greater compared with general populations. Arrhythmias and sudden cardiac death continue to account for >30% of mortality in end-stage kidney disease, with an incidence estimated to be >25-fold greater compared with general populations. Due to the general exclusion of patients with advanced CKD from cardiovascular trials, evidence supporting current therapies remains uncertain. The implications are clear, and although a steady increase in treatment probability amongst patients with severe renal insufficiency has been noted, adherence to standard therapies in patients with CKD and cardiovascular disease including reperfusion therapy in myocardial infarction remains less implemented [ 14 – 17 ].
As expected, and well-known to many clinicians, this chronic and often silent condition affects the quality of life, not only among patients but also among their caretakers. In a large French survey [ 18 ], health-related quality of life in 2,693 patients with CKD stage 3–5 was compared with responses from 20,574 responders representing the general population. Health status was perceived as fair or poor by 27% of patients with CKD3, 44% of those with CKD4-5, and 43% of those receiving dialysis. Corresponding results were 12% of transplant recipients and 3% in the general population. Importantly, in a systematic review by Gilbertson et al. [ 19 ] comprising an international collection of studies, it was demonstrated that caregivers and partners of individuals on dialysis experience significant disease burden and reduced quality of life, further adding to the impact of the condition.
2. Diagnosis
The initial diagnosis of CKD is simple as it is based on biochemical parameters, i.e., an estimated glomerular filtration rate using a measure of plasma creatinine, with the help of an equation such as the CKD-EPI [ 20 ], which takes age, gender, and race into consideration. Recently, an update to the equation has been published [ 21 ], looking into more detail on the race-dependent differences, with a suggestion to include cystatin c in future measurements. There is however at present no international consensus on the wide endorsement of the latest version of the equation. Specific definitions of CKD can vary but seems to have only minor effects on global prevalence. An investigation of six different laboratory-based classifications of CKD used in a register study found differences in CKD incidence and prevalence between the different classifications used, but it did not impact mortality and ESKD rates [ 22 ].
CKD can be caused by many different diseases. Some are defined by distinct kidney diseases with renal pathology features (eg. glomerulopathies) while in other cases may be more of a result or a secondary complication to other acute or chronic conditions (eg. diabetes or hypertension). To help distinguish between different causes of CKD, urine analysis is important. Measurement of albuminuria/proteinuria provides essential information on the type of CKD, on prognosis, and can also be used as a target for treatment. Additional diagnostic tools are kidney ultrasound, specific blood samples, and in selected or severe cases a kidney biopsy to provide the true pathology for CKD.
For CKD in diabetes, there is some variation as to the diagnosis used. Diabetic kidney disease (DKD) is defined by elevated albuminuria, with a urinary albumin excretion rate (UACR) >300 mg/g in at least two out of three consecutive samples. The presence of retinopathy and the absence of other known kidney diseases supports the diagnosis. In addition, there is also a growing focus on persons with diabetes with nonalbuminuric impaired kidney function, perhaps with a more mixed etiology, and with less risk of progression. This is usually termed kidney disease in diabetes [ 23 ].
3. Treatment
Treatment for CKD can be divided into specific and general approaches ( Table 1 ). Specific targeted treatments are available for only a fraction of patients with CKD depending on the accurate diagnosis. This is relevant e.g. for patients with glomerulonephritis where specific treatments with glucocorticoids or antibody therapies are recommended.
Recommended pharmacological treatments for CKD.
| Treatment | General population | Type 2 diabetes | Type 1 diabetes | Heart failure | Potential side effects |
|---|---|---|---|---|---|
| ACEi/ARB | X | X | X | X | Hyperkalemia, hypotension, and cough (ACEi) |
| SGLT2i | X | X | X | Polyuria, genital infections (diabetes), and ketoacidosis (diabetes) | |
| ns-MRA | X | Hyperkalemia |
ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker; SGLT2i: sodium–glucose cotransporter 2 inhibitors; ns-MRA: nonsteroidal mineralocorticoid receptor antagonist.
For the majority of patients with CKD, pharmacological treatment entails a more general approach nondependent on the pathology of CKD. The general form of treatment is rarely curative, but instead aims at slowing the progression of the disease and delaying kidney failure. Although many attempts have been made to develop new therapies for CKD, standard therapy supported by the best evidence remains blood pressure control and employment of blockers of the renin-angiotensin system (RAS), i.e., angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB). In addition to their blood pressure-lowering effects, these drugs are thought to have specific anti-inflammatory and antifibrotic effects of benefit in CKD. In various degrees of nephropathy in both types of diabetes, the collaborative group study [ 24 ] and the IRMA2 [ 25 ], IDNT [ 26 ], and the RENAAL study [ 27 ] demonstrated clear benefits with regards to delaying the progression of kidney outcome. In nondiabetic CKD the REIN [ 28 ] and the benazepril studies [ 29 ] demonstrated comparable results, backed up overall by findings in the more wide-ranging HOPE study [ 30 ].
Importantly, many of these studies also demonstrated cardiovascular protection in these high-risk populations, further securing RAS-blockade as standard therapy in guidelines.
In recent years, the emergence of sodium-glucose cotransporter 2 inhibitors (SGLT2i) has added results from a number of trials, with the majority being in type 2 diabetes, showing added benefit on top of standard care. The first dedicated kidney study was the CREDENCE study [ 31 ], testing canagliflozin 100 mg once daily in persons with diabetic nephropathy. The study was stopped prematurely after an interim analysis and showed a 30% relative reduction in the primary composite outcome of end-stage kidney disease (dialysis, transplantation, or a sustained eGFR of <15 ml/min/1.73 m 2 ), a doubling of the serum creatinine, or death from renal or cardiovascular causes. In 2020, the DAPA-CKD study followed [ 32 ], with a mixed study population consisting of participants with diabetes and CKD as well as CKD without diabetes. The primary outcome was a composite of a sustained decline in the eGFR of at least 50%, end-stage kidney disease, or death from renal or cardiovascular causes. The study demonstrated a 39% relative reduction in the primary outcome, which was present in participants with diabetes, prediabetes, and nondiabetes [ 33 ] as well as in participants with diabetic nephropathy and nondiabetic CKD [ 34 ]. In fact, results in subgroup analyses of chronic glomerulonephritides (i.e. IgA nephropathy) were significant and offer novel therapeutic options in these conditions [ 34 , 35 ].
SGLT2 inhibition is therefore included in recent guideline updates [ 36 ] as standard therapy in individuals with CKD with eGFR 25–75 ml/min/1.73 m 2 and albuminuria, and dapagliflozin has expanded its label to include CKD. There are already indications from real-world data in type 2 diabetes that the use of SGLT2 inhibitors is associated with reduced eGFR decline and a lower number of kidney-related outcomes. The findings of the CVD-REAL 3 study [ 37 ], a multinational observational cohort with more than 65000 patients, suggested that results from the randomized controlled trials are transferable to a more general population. In a propensity-matched analysis, patients that initiated SGLT2i demonstrated a lower rate of eGFR decline and lower risk of major adverse kidney outcomes, as compared to people on other glucose-lowering drugs. Pending more widespread implementation of SGLT2i as kidney preventive treatment, these results should bode well also for the global CKD population.
Recently, the nonsteroidal mineralocorticoid receptor antagonist finerenone was added to guideline-recommended [ 38 ] therapy in persons with type 2 diabetes and CKD. This was done following two randomized controlled trials demonstrating benefits in relation to both cardiovascular and kidney outcomes [ 39 , 40 ]. Ongoing trials on heart failure and nondiabetic CKD will perhaps broaden the use in the future.
It can be difficult to monitor the effect of initiated preventive treatment in CKD. To monitor eGFR requires serial measurements in stable conditions during 1-2 years for reliable assess the individual slope of kidney function decline. In proteinuric CKD however, a change in urinary albumin excretion (albuminuria) following initiation of treatment can be used as a prognostic indicator, as demonstrated in two metanalyses of observational and randomized controlled trials, respectively [ 41 , 42 ]. A treatment-induced reduction of albuminuria of >30% is favorable in relation to both cardiovascular and kidney events and such associations have been demonstrated with blockers of the renin-angiotensin system [ 43 – 45 ], SGLT2 inhibitors [ 46 ] and GLP-1 receptor agonists [ 47 ] among others. This target of albuminuria reduction is now included in the updated ADA guidelines for the treatment of diabetes. That said, there is however a lack of clinical studies using albuminuria as a treatment target, with consecutive addition of treatments with the aim of maximal albuminuria reduction, similar to what is done with blood pressure.
4. Implementation
Even though albuminuria testing is a noninvasive, noncomplicated test that adds important knowledge for both risk prediction and for monitoring of treatment effect, there is considerable room for improvement of albuminuria monitoring in CKD. Several global reports indicate a low percentage of albuminuria measurements in populations with type 2 diabetes. A recent survey across 24 primary care organizations in the United States found that a median of 52.9% of the individuals with type diabetes had the recommended annual samples collected. In Denmark, there are signs of improved albuminuria measurements in primary care, as an analysis of repeated cross-sectional studies shows an increase in annual samples from 57.8% in 2012 to 82.7% in 2020 [ 48 ]. In nondiabetic CKD however, it seems as if albuminuria testing is much less frequent. In the large CURE-CKD registry in California, comprising more than 2 million individuals with and without diabetes, albuminuria or proteinuria results in individuals with CKD were available in 8.7% and 4.1%, respectively [ 49 ]. This calls for an increased focus on albuminuria testing in overall CKD, to improve diagnosis, risk prediction, and treatment selection. In the same publication [ 49 ], it was also reported that a renin-angiotensin inhibitor was prescribed to 20.6%, which is far from optimal.
Even with recent updates in guidelines and significant improvements in CVD and CKD protection seen in randomized controlled trials, implementation and uptake of new therapies is slow. One example is the recent CVD protective focus on type 2 diabetes, where SGLT2i and GLP-1RA are recommended when type 2 diabetes and manifest CVD coexists. In a Danish register-based study [ 50 ], the uptake of these drugs in this high-risk group was as low as 18%, pointing to a need for the education of healthcare professionals and patients. Similar findings in type 2 diabetes have been demonstrated in the UK general practice database [ 51 ], and in global settings [ 52 ]. From a kidney protection perspective, it will be interesting to learn whether the current change of guidelines can be implemented quickly across a number of medical specialties and between primary and secondary health care.
5. Discussion
Is this disease mongering? Disease mongering is an expression attributed to the medical journalist Lynn Payer describing a broadening of the definition of a treatable disease in order to increase demand for medicinal products and services.
One could argue that health professionals pointing to a large undetected group of people with a silent but chronic condition and at the same time advocating for medical treatment, could just be trying to expand the use and indication for existing drugs. This is not our intention with this paper. Particularly earlier identification of patients with chronic illness could lead to erosion of treatment benefits due to the implementation of treatment in patients with limited risk overall. Raising awareness of the possibility of treatment leading to prevention of ensuing illness is however an important element of public health education and an invaluable means of enhancing professional and public understanding of specific diseases and promoting appropriate uptake of novel therapies. As such, an appropriate balance is indicated.
In that sense, it is important to remember that the CKD classification is not age-adjusted, and widespread screening may lead to the potential overdiagnosing of elderly people with a benign prognosis [ 53 ]. This calls for updated guidelines for referral and treatment of elder subjects with impaired kidney function.
We argue that end-stage kidney disease, although developing slowly and with few symptoms, is a grave condition with a severe impact on quality of life, on survival, and is associated with extensive comorbidity and health care costs. Therefore, the implementation of effective medical treatment for people at risk of developing ESKD must be considered, especially if it causes little or no harm. Whether this implementation of treatment should be accompanied by population-wide screening programs, might seem logical and tempting, but it is not clear from the literature that screening efforts lead unequivocally to a better outcome, and clearly more research is needed in this area. Few studies have examined the value of early widespread screening for proteinuria. Boulware et al. analyzed the cost-benefit of annual screening for proteinuria at age 50 years using a Markov model. They concluded that early detection of urine protein followed by treatment with an ACEi or ARB to slow the progression of CKD and decrease mortality is not cost-effective unless selectively directed toward high-risk groups (older persons and persons with hypertension) [ 54 ]. As a long-term effect of the current standard treatment of diabetes and CKD, i.e. blocking of the renin-angiotensin system, remains unaddressed, an interesting study has tried to model the possible impact of “early” and “late” intervention [ 55 ]. Using data from available randomized clinical trials, it was found that “early” intervention with angiotensin II receptor blockade in a typical subject of 60 years of age, would delay the onset of ESKD by 4.2 years as opposed to 1.4 years, if treatment was initiated at a late stage. This was even more pronounced if patients were younger.
The cost of CKD, and especially ESKD, is high. A large study from Spain [ 56 ] documented that in contrast to what many may think, medication costs averaged only 6.6% of the total healthcare cost, with cardiovascular hospitalizations conversely accounting for 77% of total healthcare expenditure in this group. In addition, people on dialysis are associated with higher healthcare costs than people with a kidney transplant. The health care cost of a typical dialysis patient in Denmark is approximately €90,000 annually, provided by the general health care system.
It is clear that CKD is quickly becoming one of the major chronic diseases globally, with a very silent growth that needs attention. Although it can be debated whether screening would be of benefit, it will in any case be necessary for clinicians both in primary and secondary care to try to optimize the selection of CKD patients in whom further work-up and treatment to delay the progression of kidney function decline is appropriate. Particularly, current guidance for treatment selection from the initial workup with biochemistry, urine analysis, and perhaps imaging remains limited in all but a few patients with specific symptoms and findings (i.e., polycystic kidney disease, IgA-nephropathy, and systemic diseases with kidney involvements).
Research is however ongoing with regard to identifying more specific markers for earlier diagnosis of CKD or perhaps even just the risk of developing CKD. New techniques known as “omics” or sometimes referred to as systems medicine are being explored to better understand complex metabolic pathways, often with multiple biomarkers analyzed with proteomics, metabolomics, lipidomics, or genomics [ 57 ]. As the biological samples analyzed with these techniques yield a high number of data points, specialized computer software and interpretation are needed, making it unsuitable for everyday clinical practice, but so far mostly for discovering new pathways of disease. One recent example of early diagnosis of diabetic kidney disease is the use of urinary proteomics. A urine sample from an individual with type 2 diabetes with no signs of kidney damage can be analyzed for several thousand peptides and collagen fragments, showing a distinct and previously defined risk pattern for later development of microalbuminuria and CKD [ 58 ]. The presence of this “risk pattern” has been demonstrated years before the onset of microalbuminuria. The concept has also been tested prospectively in the PRIORITY study [ 59 ], where the urinary proteomic risk pattern could select people at risk for the later development of microalbuminuria. Similar approaches are being tested with other techniques as plasma proteomics [ 60 ]and lipidomics [ 61 ]. There is still, however, considerable work needed to be done before these techniques become validated and widely available for all types of kidney disease.
Earlier and perhaps more specific diagnoses could contribute to a more differentiated treatment approach. As there is variation in progression rate, there is also a need to select some for more aggressive treatment while others can be monitored solely. This distinction is currently difficult and would probably benefit from well-validated precision techniques as discussed above. Not only is there a need for guidance on which individuals to select for treatment but there is also the topic of what treatment to select. The current approach describes a few general pharmacological classes of drugs with evidence of kidney protection but is used in a very generalized way and often in the late stage of CKD. Much like antihypertensive treatment, it would be great to start therapy early to be able to prevent progression, but also to be able to select therapy in a more modern way, guided by biomarkers or a detailed understanding of the underlying pathology. In late-stage CKD the kidney biopsy is the ultimate diagnostic tool, which sometimes leads to a more targeted therapy, but widespread use is limited by safety concerns. The hope is that the kidney biopsy in the future can be replaced by a “liquid” biopsy, by use of validated use of “omics” or similar techniques and provide early and widespread guidance on CKD pathology leading to more targeted treatment choices. Randomized trials using this approach are however still lacking in CKD.
In addition, the patient with little or no symptoms and therefore undetected or perhaps newly detected CKD is also challenged by the organization of health care. As an example, an individual with type 2 diabetes and diabetic kidney disease may well be involved with different principal caretakers over the many years this condition is present. Being sent back and forth between primary care, specialist diabetes care, and perhaps also the nephrologist will sometimes be complicated and confusing for the patient. A special effort to ensure alignment of patient education and sharing of medical records must be made. Indeed, joint diabetes and nephrology outpatient clinics may prove to benefit the patient, and perhaps even broaden the perspectives of the involved specialists. Joint guidelines are also helping to ensure the best care for the complicated patient with CKD and comorbidity. In the future, primary care physicians can learn from discussing shared cases with specialists, evolving their understanding of CKD, and nephrologists can perhaps develop from being “end-stage” specialists to also contribute to the prevention of CKD and related comorbidity as CVD. Notwithstanding there is much work to do to secure a future with high-quality treatment and prevention of CKD.
6. Conclusion
CKD prevalence is increasing but preventive treatment has a great potential. Greater awareness and appropriate screening are necessary first steps to try to avoid a future increase in CKD morbidity and healthcare costs. A large part of this will take place in primary care settings.
Acknowledgments
Publication costs for this manuscript were paid by Astra Zeneca.
Data Availability
Conflicts of interest.
The authors declare that they have no conflicts of interest.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 08 March 2023
Researchers tackle chronic kidney disease
You can also search for this author in PubMed Google Scholar
Every 30 minutes, the kidneys filter all the blood in the body. This round-the-clock removal of toxins is hard work, and over a lifetime of purification, these vital organs can falter. The result is a progressive condition that affects roughly 10% of the world’s population — an astonishing 800 million people. In fact, chronic kidney disease (CKD) has become one of the leading causes of death worldwide. The stakes are high, and research is advancing on multiple fronts .
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 615 , S1 (2023)
doi: https://doi.org/10.1038/d41586-023-00647-4
This article is part of Nature Outlook: Chronic kidney disease , an editorially independent supplement produced with the financial support of third parties. About this content .
Related Articles

Sponsor feature: CKD is a hidden threat, but the treatment landscape is evolving
- Medical research
- Therapeutics
- Health care

DNA-sensing inflammasomes cause recurrent atherosclerotic stroke
Article 07 AUG 24

Molecular mimicry in multisystem inflammatory syndrome in children

Sophisticated natural products as antibiotics
Review Article 31 JUL 24

Engineered brain parasite ferries useful proteins into neurons
Research Highlight 07 AUG 24

Blood tests could soon predict your risk of Alzheimer’s
News Feature 07 AUG 24
Breast-cancer cells enlist nerves to spread throughout the body
News 07 AUG 24
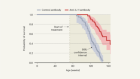
Blocking an inflammatory protein slows the pace of ageing
News & Views 29 JUL 24

A Trojan horse for thirsty tumours
Outlook 11 JUL 24

Faecal transplants can treat some cancers — but probably won’t ever be widely used
Outlook 04 JUL 24
Faculty position – Department of Bone Marrow Transplantation & Cellular Therapy
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Faculty Position, Department of Diagnostic Imaging - AI Imaging Research
Neuroscience faculty position.
Neuroscience Faculty Position-Center for Pediatric Neurological Disease Research, St. Jude Pediatric Translational Neuroscience Initiative
RNA Mass Spectrometry Platform Manager (Level B)
The RNA mass spectrometry (MS) Platform Manager will be responsible for developing RNA MS workflows and managing the platform operation.
Monash University, Monash (AU)
Monash University
Postdoctoral Associate
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The kidney in acute respiratory distress syndrome: victim or partner in crime?
- Published: 29 July 2024
- Volume 50 , pages 1313–1316, ( 2024 )
Cite this article

- Faeq Husain-Syed ORCID: orcid.org/0000-0001-6742-5052 1 ,
- Daniele Poole ORCID: orcid.org/0000-0001-5279-9844 2 &
- Michael Joannidis ORCID: orcid.org/0000-0002-6996-0881 3
946 Accesses
1 Altmetric
Explore all metrics
Avoid common mistakes on your manuscript.
Acute kidney injury (AKI) is a frequent complication in critically ill patients and significantly contributes to both morbidity and mortality [ 1 ]. AKI is also common in patients with acute respiratory distress syndrome (ARDS). The co-occurrence of AKI and ARDS is associated with a marked decrease in patient survival—from approximately 60% to around 40%—as reported in the LUNG SAFE study [ 2 ]. Although AKI in patients with ARDS may reflect the overall severity of the disease, there could also be a direct causal link both with organ cross-talk and critical care interventions (e.g., mechanical ventilation, extracorporeal membrane oxygenation) further contributing to AKI [ 3 ].
In this issue of Intensive Care Medicine, Antonucci et al. [ 4 ] make an attempt to evaluate the attributable mortality of AKI complicating ARDS by individual patient data analysis of 5148 patients from 10 multicenter randomized controlled trials (RCTs) conducted in the United States of America by the ARDS Network and the Prevention and Early Treatment of Acute Lung Injury Network. These trials prospectively investigated various interventions for ARDS between 1996 and 2018. AKI occurrence was investigated within the first 7 days after randomization by the Kidney Disease: Improving Global Outcomes (KDIGO) serum creatinine criterion without considering urinary output. The authors found an average unadjusted incidence of AKI of 43.7%, with the trial-specific rates ranging from 30.5% to 63.1%. About half of the patients developed AKI stage 3, 37.1% of the AKI patients showed characteristics of rapidly improving AKI (defined as a return to stage zero AKI within 48 h from AKI onset), which was more common in patients with milder stages of AKI. Meanwhile, 46.2% met the criteria for acute kidney disease (AKD) [ 5 ], which was more common in patients with severe AKI.
Overall, excess mortality attributed to AKI was 14.1% at 28 days and 15.4% at 90 days, which is higher than reported for a general intensive care unit (ICU) population (i.e., 8.6%) [ 6 ]. Predictably, rapidly improving AKI had a low attributable 90-day mortality rate of 4.7%, whereas AKD showed a higher attributable mortality of 28.4%, even surpassing that of severe AKI (20.3%). These findings seem conclusive, as persistent AKI and AKI–AKD transition can worsen fluid accumulation, electrolyte and acid base disturbances, and systemic inflammation, all of which increase cardiovascular risk, favor secondary infections and negatively impact survival [ 5 , 7 , 8 ].
Several aspects of the Antonucci et al. study stand out [ 4 ]. First, the AKI incidence in patients enrolled in ARDS trials has remained relatively stable over the last 20 years. Notably, the only intervention resulting in reduced mortality (low vs. high tidal volume ventilation in the ARMA trial) did not affect the incidence of AKI. In contrast, differences in AKI incidence between the control and intervention groups were observed only in the FACTT trial and its secondary analyses, which compared conservative and liberal fluid management [ 9 ]. However, these differences did not translate into differences in mortality. Given that the trials investigated various interventions on mortality in ARDS, data on covariates beyond ventilatory parameters are limited, and it is unclear whether any interventions outside the protocol-specified treatments were performed to mitigate AKI progression. Interestingly, the severity of ARDS and the presence of non-renal organ failure, rather than ventilatory parameters at baseline, were significantly associated with mortality following AKI. This indicates that AKI may indeed be a consequence of the overall severity of the disease and that the impact of the current standard-of-care mechanical ventilation on AKI might be limited. Unfortunately, changes in ventilator parameters were not taken into account.
Where do we go from here? While it is likely that Antonucci et al. [ 4 ] underestimated the true incidence of AKI using a dataset that was not specifically designed to examine kidney outcomes (supplementary Table S1), their study still provides valuable insights into the epidemiology of AKI and renal recovery over the last 20 years. Importantly, it highlights that, although AKI might not be entirely preventable, our efforts should focus on better subphenotyping AKI and understanding AKI trajectories to identify patients at risk for persistent AKI and AKI–AKD transition [ 8 , 10 ]. This observation is important because AKI–AKD transition appears as a significant and, in the landscape of RCTs, neglected factor contributing to morbidity and mortality [ 5 ]. Identifying risk factors associated with the progression of AKI, classifying AKI based on these risks, and investigating strategies that can improve post-AKI outcomes are important areas of future research. Furthermore, given the lower attributable mortality of AKI in cases that showed rapid improvement, it would be important to investigate the procedures, which may fasten recovery aside from the well-known KDIGO bundle [ 11 ].
Another aspect to consider is the methodological approach of this study, which raises some concerns. Seeking causal relationships between exposures and outcomes based on data from observational studies has always been a challenge for researchers in the medical field. In RCTs, there is a balance between measured and unmeasured factors so that the study arm allocation is the only difference between exposed and non-exposed patients. In observational studies, ideally, we should control for all the factors that are causally related both with the exposure and the outcome [ 12 ].
Antonucci and coworkers used a propensity score to calculate each patient’s probability of developing AKI and inverse probability treatment weighting (IPTW) to generate two pseudo-populations, that is, one where all patients developed AKI and the other one where no patients did. The differences in outcomes between the two pseudo-populations are expected to provide an estimate of the impact of AKI on mortality because the prognostic factors included in the propensity score are balanced in the two study arms.
As mentioned earlier, the propensity score should ideally consider all covariates causally linked to both exposure and outcome, in order to meet the no unmeasured confounders’ assumption [ 13 , 14 ]. For example, if the development of AKI were strongly influenced by the occurrence of septic shock, right heart failure or hypoxemia during the stay, not controlling for these variables would result in a biased model. The lack of these and other potentially relevant variables in this study did not match the need of completeness required by explanatory models. Although, it is quite plausible that AKI worsens prognosis in ARDS patients, the quantification of mortality attributable to AKI provided by the study has a high probability of not being trustworthy.
Another important limitation of this investigations is the unresolved problem of evaluating two heterogeneous syndromes, namely ARDS and AKI, each of which consists of several subphenotypes with varying underlying pathophysiology and impact on outcome (Fig. 1 ) [ 10 , 15 ]. This variation in subphenotype composition between the investigated trials may explain the significant differences observed in both AKI incidence and its effect on outcomes.

Schematic representation of ARDS subphenotypes and their link with AKI subphenotypes and associated outcomes. The schematic representation highlights the heterogeneity among ARDS patients and those with AKI complicating ARDS, illustrating the need for tailored therapeutic approaches based on specific subphenotypes, their associated risk factors, and disease modifiers. As depicted in the gray circles, AKI subphenotypes can be characterized by severity (subclinical AKI vs. stage 1–3 AKI), duration (rapidly improving AKI vs. persistent AKI), and injury trajectory (recurrent AKI vs. AKI–AKD transition), each with distinct clinical characteristics and outcomes. AKI Subphenotype Z might occur whereas the first 7 days are marked by slowly worsening kidney function that does not technically meet the criteria for AKI but shows positivity for tubular stress/damage biomarkers, indicating subclinical AKI, but still progresses to AKD. Notably, it is likely that additional AKI patterns will be discovered in the coming years. Identifying AKI subphenotypes and their link to ARDS phenotypes could enhance the design of future clinical trials by providing a biologically and clinically consistent framework, thus enriching critical ill populations that were historically treated uniformly in previous ARDS randomized controlled trials. It is also important to note that a single patient may simultaneously belong to multiple subphenotypes, which can change over the course of the illness. Prospective trials will be required before applying these subphenotypes for clinical decision-making. AKD acute kidney disease; AKI acute kidney injury; ARDS acute respiratory distress syndrome; CKD chronic kidney disease; ECMO extracorporeal membrane oxygenation
To conclude, while observational studies can provide strong evidence in situations where causal inference is sought and are not inherently weak, they often provide low-quality evidence when the pool of variables available is inadequate. Thus, the implications of the Antonucci et al. study [ 4 ] in terms of the role of lung–kidney interactions in the development of AKI versus AKI as a marker of overall severity of the disease in patients with ARDS should be treated with caution. Despite these shortcomings, the results of the study offer valuable insights into the epidemiology of AKI and AKD in ARDS. In future, prospectively collected data from carefully planned observational studies, designed with the same rigor as RCTs, will be necessary to provide trustworthy evidence for causal relationships.
Hoste EAJ, Kellum JA, Selby NM, Zarbock A, Palevsky PM, Bagshaw SM, Goldstein SL, Cerda J, Chawla LS (2018) Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 14:607–625
Article CAS PubMed Google Scholar
McNicholas BA, Rezoagli E, Pham T, Madotto F, Guiard E, Fanelli V, Bellani G, Griffin MD, Ranieri M, Laffey JG, ESICM Trial Group and the Large observational study to UNderstand the Global impact of Severe Acute respiratory FailurE (LUNG SAFE) Investigators (2019) Impact of early acute kidney injury on management and outcome in patients with acute respiratory distress syndrome: a secondary analysis of a multicenter observational study. Crit Care Med 47:1216–1225
Joannidis M, Forni LG, Klein SJ, Honore PM, Kashani K, Ostermann M, Prowle J, Bagshaw SM, Cantaluppi V, Darmon M, Ding X, Fuhrmann V, Hoste E, Husain-Syed F, Lubnow M, Maggiorini M, Meersch M, Murray PT, Ricci Z, Singbartl K, Staudinger T, Welte T, Ronco C, Kellum JA (2020) Lung-kidney interactions in critically ill patients: consensus report of the Acute Disease Quality Initiative (ADQI) 21 Workgroup. Intensive Care Med 46:654–672
Article PubMed Google Scholar
Antonucci E, Garcia B, Chen D, Matthay MA, Liu KD, Legrand M (2024) Incidence of acute kidney injury and attributive mortality in acute respiratory distress syndrome randomized trials. Intensive Care Med. https://doi.org/10.1007/s00134-024-07485-6
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL, Forni L, Kane-Gill SL, Hoste E, Koyner J, Liu KD, Macedo E, Mehta R, Murray P, Nadim M, Ostermann M, Palevsky PM, Pannu N, Rosner M, Wald R, Zarbock A, Ronco C, Kellum JA, Acute Disease Quality Initiative W (2017) Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 13:241–257
Vaara ST, Pettilä V, Kaukonen KM, Bendel S, Korhonen AM, Bellomo R, Reinikainen M (2014) The attributable mortality of acute kidney injury: a sequentially matched analysis*. Crit Care Med 42:878–885
Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, Himmelfarb J (2011) Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med 37:241–248
Hoste E, Bihorac A, Al-Khafaji A, Ortega LM, Ostermann M, Haase M, Zacharowski K, Wunderink R, Heung M, Lissauer M, Self WH, Koyner JL, Honore PM, Prowle JR, Joannidis M, Forni LG, Kampf JP, McPherson P, Kellum JA, Chawla LS, Investigators R (2020) Identification and validation of biomarkers of persistent acute kidney injury: the RUBY study. Intensive Care Med 46:943–953
Article CAS PubMed PubMed Central Google Scholar
Liu KD, Thompson BT, Ancukiewicz M, Steingrub JS, Douglas IS, Matthay MA, Wright P, Peterson MW, Rock P, Hyzy RC, Anzueto A, Truwit JD, Institutes of Health National Heart L, Blood Institute Acute Respiratory Distress Syndrome N (2011) Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med 39:2665–2671
Article PubMed PubMed Central Google Scholar
Vaara ST, Forni LG, Joannidis M (2022) Subphenotypes of acute kidney injury in adults. Curr Opin Crit Care 28:599–604
von Groote TC, Ostermann M, Forni LG, Meersch-Dini M, Zarbock A, Prev AKII (2022) The AKI care bundle: all bundle components are created equal-are they? Intensive Care Med 48:242–245
Article Google Scholar
Poole D, Mayo PH, Moller MH (2020) The wicked path of causal inference in observational studies. Intensive Care Med 46:799–801
Robins JM, Hernan MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11:550–560
Lunceford JK, Davidian M (2004) Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med 23:2937–2960
Grasselli G, Calfee CS, Camporota L, Poole D, Amato MBP, Antonelli M, Arabi YM, Baroncelli F, Beitler JR, Bellani G, Bellingan G, Blackwood B, Bos LDJ, Brochard L, Brodie D, Burns KEA, Combes A, D’Arrigo S, De Backer D, Demoule A, Einav S, Fan E, Ferguson ND, Frat JP, Gattinoni L, Guerin C, Herridge MS, Hodgson C, Hough CL, Jaber S, Juffermans NP, Karagiannidis C, Kesecioglu J, Kwizera A, Laffey JG, Mancebo J, Matthay MA, McAuley DF, Mercat A, Meyer NJ, Moss M, Munshi L, Myatra SN, Ng Gong M, Papazian L, Patel BK, Pellegrini M, Perner A, Pesenti A, Piquilloud L, Qiu H, Ranieri MV, Riviello E, Slutsky AS, Stapleton RD, Summers C, Thompson TB, Valente Barbas CS, Villar J, Ware LB, Weiss B, Zampieri FG, Azoulay E, Cecconi M, European Society of Intensive Care Medicine Taskforce on A (2023) ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med 49:727–759
Download references
Author information
Authors and affiliations.
Division of Nephrology, Department of Internal Medicine II, University Hospital Giessen and Marburg, Justus-Liebig-University Giessen, Klinikstrasse 33, 35392, Giessen, Germany
Faeq Husain-Syed
Operative Unit of Anesthesia and Intensive Care, S. Martino Hospital, Viale Europa, 22, 32100, Belluno, Italy
Daniele Poole
Division of Intensive Care and Emergency Medicine, Department of Internal Medicine, Medical University Innsbruck, Anichstrasse 35, 6020, Innsbruck, Austria
Michael Joannidis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michael Joannidis .
Ethics declarations
Conflicts of interest.
FH-S reports no COI. DP reports support for ESICM methodology group meetings outside the submitted work. MJ has received honoraria or research support from Baxter Healthcare Corp, AM-Pharma, CLS Behring, Fresenius, Takeda and Novartis outside the submitted work.
Ethical approval
Not applicable.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 21 KB)
Rights and permissions.
Reprints and permissions
About this article
Husain-Syed, F., Poole, D. & Joannidis, M. The kidney in acute respiratory distress syndrome: victim or partner in crime?. Intensive Care Med 50 , 1313–1316 (2024). https://doi.org/10.1007/s00134-024-07558-6
Download citation
Received : 10 June 2024
Accepted : 09 July 2024
Published : 29 July 2024
Issue Date : August 2024
DOI : https://doi.org/10.1007/s00134-024-07558-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Chronic kidney disease (CKD) is the 16th leading cause of years of life lost worldwide. Appropriate screening, diagnosis, and management by primary care clinicians are necessary to prevent adverse CKD-associated outcomes, including cardiovascular disease, ...
Despite notable progress in basic, clinical and translational nephrology research in the past 50 years, many challenges remain. In this Review, the authors provide an overview of the current ...
Chronic kidney disease (CKD) is a complex disease which affects approximately 13% of the world's population. Over time, CKD can cause renal dysfunction and progression to end-stage kidney disease and cardiovascular disease. Complications associated ...
Chronic kidney disease is defined by the presence of kidney damage or decreased kidney function for at least three months, irrespective of the cause. 2 Kidney damage generally refers to pathologic anomalies in the native or transplanted kidney, established via imaging, biopsy, or deduced from clinical markers like increased albuminuria— that is, albumin‐to‐creatinine ratio (ACR) >30 mg/g ...
Chronic kidney disease (CKD) is defined as a progressive loss of renal function that lasts for more than 3 months, and is classified according to the degree of kidney damage - measured by the ...
First published in 1981, the American Journal of Kidney Diseases (AJKD) is the official journal of the National Kidney Foundation Opens in new window , AJKD is recognized worldwide as a leading source of information devoted to clinical nephrology research and practice. Learn more.
Sleep disorders in chronic kidney disease. In this Review, Owen Lyons discusses the diagnosis, epidemiology and pathophysiology of three sleep disorders that commonly affect patients with chronic ...
Patients with type 2 diabetes and chronic kidney disease are at high risk for kidney failure, cardiovascular events, and death. Whether treatment with semaglutide would mitigate these risks is unkn...
Chronic kidney disease (CKD) represents a global public health crisis, but awareness by patients and providers is poor. Defined as persistent abnormalities in kidney structure or function for more than three months, manifested as either low glomerular filtration rate or presence of a marker of kidney damage such as albuminuria, CKD can be identified through readily available blood and urine ...
Chronic kidney disease is a progressive disease with no cure and high morbidity and mortality that occurs commonly in the general adult population, especially in people with diabetes and hypertension. Preservation of kidney function can improve outcomes and can be achieved through non-pharmacological strategies (eg, dietary and lifestyle adjustments) and chronic kidney disease-targeted and ...
Read the latest articles of Advances in Chronic Kidney Disease at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature
2023 was a big year for the nephrology (kidney) research field. From developments in organ transplant options to a new understanding of kidney disease risk, it can be challenging to keep up with it all. Fortunately, the American Kidney Fund (AKF) has been keeping tabs on these headlines for you.
Chronic kidney disease is a progressive condition that affects >10% of the general population worldwide, amounting to >800 million individuals. Chronic kidney disease is more prevalent in older individuals, women, racial minorities, and in people experiencing diabetes mellitus and hypertension. Chronic kidney disease represents an especially large burden in low- and middle-income countries ...
Abstract. Chronic kidney disease is a progressive condition that affects >10% of the general population worldwide, amounting to >800 million individuals. Chronic kidney disease is more prevalent in older individuals, women, racial minorities, and in people experiencing diabetes mellitus and hypertension. Chronic kidney disease represents an ...
FindingsIn this cohort study of the Center for Kidney Research, Education, and Hope (CURE-CKD) registry, more than 2.6 million adults and children had chronic kidney disease or were at risk. Albuminuria or proteinuria was tested in approximately one-eighth of adults with chronic kidney disease, renin-angiotensin system inhibitors were prescribed to one-fifth, and nonsteroidal anti-inflammatory ...
This editorial describes the science behind detecting and treating autoimmunity in kidney disease.
The identification of a specific immune-cell subpopulation underlying disease progression should allow the development of treatments that preserve kidney health and function.
People with diabetes and chronic kidney disease (CKD) are at high risk for kidney failure, atherosclerotic cardiovascular disease, heart failure, and premature mortality. Recent clinical trials support new approaches to treat diabetes and CKD. The 2022 American Diabetes Association (ADA) Standards of Medical Care in Diabetes and the Kidney Disease: Improving Global Outcomes (KDIGO) 2022 ...
NIH-funded effort provides interactive resource for global research community. In a major breakthrough toward understanding and treating kidney disease, a nationwide research team funded by the National Institutes of Health has created the most comprehensive atlas of the human kidney. Data from the Kidney Tissue Atlas will allow the comparison of healthy kidney cells to those injured by kidney ...
Additionally, ongoing research in genomics and personalized medicine may lead to more effective strategies for the prevention and treatment of kidney diseases with a genetic component.To describe the genetic landscape of cystic kidney diseases and the recent advances in the identification of genetic disorders of the kidney.
Delaying disease progression and reducing the risk of mortality are key goals in the treatment of chronic kidney disease (CKD). New drug classes to augment renin-angiotensin-aldosterone system (RAAS) inhibitors as the standard of care ...
Methods: Search of literature for randomised controlled trials, quasi-experimental studies and pre-experimental studies on chronic kidney disease-related educational interventions for nurses was conducted across 10 databases. Two reviewers independently screened articles, appraised studies and extracted data.
Background This study aimed to investigate the association between central sensitivity to thyroid hormones and all-cause mortality in euthyroid patients with chronic kidney disease (CKD). Methods Data on thyroid function indicators and all-cause mortality for CKD patients were extracted from the NHANES database (2007-2012). Central sensitivities to thyroid hormones were mainly evaluated by ...
Kidney diseases are hereditary and nonhereditary disorders that affect the kidney. Diabetes mellitus and high blood pressure are important risk factors for kidney disease. A new study demonstrates ...
Statin use and the progression of coronary artery calcification in chronic kidney disease: Findings from the KNOW-CKD study ... a potential explanation for the lack of mortality benefit observed with statin use in patients with end-stage kidney disease (ESKD). Therefore, future research should explore the differential effects on mortality ...
This cohort study aimed to explore the relationship between hydration status and the risk of diabetic kidney disease (DKD) as well as all-cause death in DKD patients.Weighted univariable and multiv...
Chronic kidney disease (CKD) is becoming one of the world's most prevalent noncommunicable chronic diseases. The World Health Organization projects CKD to become the 5th most common chronic disease in 2040. Causes of CKD are multifactorial and diverse, but early-stage symptoms are often few and silent. Progression rates are highly variable, but ...
Researchers tackle chronic kidney disease. Innovative technology and a class of drugs called SGLT2 inhibitors could help more people with this common condition. Every 30 minutes, the kidneys ...
Acute kidney injury (AKI) is a frequent complication in critically ill patients and significantly contributes to both morbidity and mortality [].AKI is also common in patients with acute respiratory distress syndrome (ARDS).
Background Autosomal dominant polycystic kidney disease (ADPKD) is caused by mutations in the PKD1 and PKD2 genes, and often progresses to end stage renal disease (ESRD). ADPKD progression is not uniform among patients, suggesting that factors secondary to the PKD1/2 gene mutation could regulate the rate of disease progression. Here we tested the effect of circadian clock disruption on ADPKD ...