An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss
Affiliations.
- 1 Division of Biomedical Sciences, Warwick Medical School, University of Warwick, Warwick, UK; Tommy's National Centre for Miscarriage Research, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK. Electronic address: [email protected].
- 2 Tommy's National Centre for Miscarriage Research, Institute of Metabolism and Systems Research, University of Birmingham, Birmingham, UK.
- 3 University of Illinois Recurrent Pregnancy Loss Program, Department of Obstetrics and Gynecology, University of Illinois at Chicago, Chicago, IL, USA.
- 4 Warwick Clinical Trials Unit, University of Warwick, Warwick, UK.
- 5 Division of Biomedical Sciences, Warwick Medical School, University of Warwick, Warwick, UK; Tommy's National Centre for Miscarriage Research, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK.
- 6 Tommy's Charity, Laurence Pountney Hill, London, UK.
- 7 CONICET, Universidad de Buenos Aires, Instituto de Química Biológica de la Facultad de Ciencias Exactas y Naturales IQUIBICEN, Buenos Aires, Argentina.
- 8 Department of Biology, Johns Hopkins University, Baltimore, MD, USA.
- 9 Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK.
- 10 Tommy's National Centre for Miscarriage Research, Imperial College London, London, UK.
- 11 Centre for Recurrent Pregnancy Loss of Western Denmark, Department of Obstetrics and Gynaecology, Aalborg University Hospital, Aalborg, Denmark.
- 12 Department of Obstetrics and Gynecology, Graduate School of Medical Sciences, Nagoya City University, Nagoya, Japan.
- PMID: 33915094
- DOI: 10.1016/S0140-6736(21)00682-6
Miscarriage is generally defined as the loss of a pregnancy before viability. An estimated 23 million miscarriages occur every year worldwide, translating to 44 pregnancy losses each minute. The pooled risk of miscarriage is 15·3% (95% CI 12·5-18·7%) of all recognised pregnancies. The population prevalence of women who have had one miscarriage is 10·8% (10·3-11·4%), two miscarriages is 1·9% (1·8-2·1%), and three or more miscarriages is 0·7% (0·5-0·8%). Risk factors for miscarriage include very young or older female age (younger than 20 years and older than 35 years), older male age (older than 40 years), very low or very high body-mass index, Black ethnicity, previous miscarriages, smoking, alcohol, stress, working night shifts, air pollution, and exposure to pesticides. The consequences of miscarriage are both physical, such as bleeding or infection, and psychological. Psychological consequences include increases in the risk of anxiety, depression, post-traumatic stress disorder, and suicide. Miscarriage, and especially recurrent miscarriage, is also a sentinel risk marker for obstetric complications, including preterm birth, fetal growth restriction, placental abruption, and stillbirth in future pregnancies, and a predictor of longer-term health problems, such as cardiovascular disease and venous thromboembolism. The costs of miscarriage affect individuals, health-care systems, and society. The short-term national economic cost of miscarriage is estimated to be £471 million per year in the UK. As recurrent miscarriage is a sentinel marker for various obstetric risks in future pregnancies, women should receive care in preconception and obstetric clinics specialising in patients at high risk. As psychological morbidity is common after pregnancy loss, effective screening instruments and treatment options for mental health consequences of miscarriage need to be available. We recommend that miscarriage data are gathered and reported to facilitate comparison of rates among countries, to accelerate research, and to improve patient care and policy development.
Copyright © 2021 Elsevier Ltd. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of interests We declare no competing interests.
- Miscarriage: worldwide reform of care is needed. The Lancet. The Lancet. Lancet. 2021 May 1;397(10285):1597. doi: 10.1016/S0140-6736(21)00954-5. Epub 2021 Apr 27. Lancet. 2021. PMID: 33915093 No abstract available.
- Making miscarriage matter. Chong K, Li W, Roberts I, Mol BW. Chong K, et al. Lancet. 2021 Aug 28;398(10302):743-744. doi: 10.1016/S0140-6736(21)01379-9. Lancet. 2021. PMID: 34454666 No abstract available.
- Making miscarriage matter. Lucas S, Knight M, Lucas N, Rodger A. Lucas S, et al. Lancet. 2021 Aug 28;398(10302):744-745. doi: 10.1016/S0140-6736(21)01381-7. Lancet. 2021. PMID: 34454667 No abstract available.
- Making miscarriage matter. Agampodi S, Hettiarachchi A, Agampodi T. Agampodi S, et al. Lancet. 2021 Aug 28;398(10302):745. doi: 10.1016/S0140-6736(21)01426-4. Lancet. 2021. PMID: 34454668 No abstract available.
Similar articles
- Subsequent pregnancy outcomes after second trimester miscarriage or termination for medical/fetal reason: A systematic review and meta-analysis of observational studies. Patel K, Pirie D, Heazell AEP, Morgan B, Woolner A. Patel K, et al. Acta Obstet Gynecol Scand. 2024 Mar;103(3):413-422. doi: 10.1111/aogs.14731. Epub 2023 Nov 30. Acta Obstet Gynecol Scand. 2024. PMID: 38037500 Free PMC article. Review.
- Risk of placental dysfunction disorders after prior miscarriages: a population-based study. Gunnarsdottir J, Stephansson O, Cnattingius S, Akerud H, Wikström AK. Gunnarsdottir J, et al. Am J Obstet Gynecol. 2014 Jul;211(1):34.e1-8. doi: 10.1016/j.ajog.2014.01.041. Epub 2014 Feb 1. Am J Obstet Gynecol. 2014. PMID: 24495667
- Spontaneous first trimester miscarriage rates per woman among parous women with 1 or more pregnancies of 24 weeks or more. Cohain JS, Buxbaum RE, Mankuta D. Cohain JS, et al. BMC Pregnancy Childbirth. 2017 Dec 22;17(1):437. doi: 10.1186/s12884-017-1620-1. BMC Pregnancy Childbirth. 2017. PMID: 29272996 Free PMC article.
- Do women with recurrent miscarriage constitute a high-risk obstetric population? Fawzy M, Saravelos S, Li TC, Metwally M. Fawzy M, et al. Hum Fertil (Camb). 2016 Apr;19(1):9-15. doi: 10.3109/14647273.2016.1142214. Epub 2016 Mar 22. Hum Fertil (Camb). 2016. PMID: 27002424
- Pregnancy complications and later life women's health. McNestry C, Killeen SL, Crowley RK, McAuliffe FM. McNestry C, et al. Acta Obstet Gynecol Scand. 2023 May;102(5):523-531. doi: 10.1111/aogs.14523. Epub 2023 Feb 17. Acta Obstet Gynecol Scand. 2023. PMID: 36799269 Free PMC article. Review.
- From bench to in silico and backwards: What have we done on genetics of recurrent pregnancy loss and implantation failure and where should we go next? Gomes FG, Boquett JA, Kowalski TW, Bremm JM, Michels MS, Pretto L, Rockenbach MK, Vianna FSL, Schuler-Faccini L, Sanseverino MTV, Fraga LR. Gomes FG, et al. Genet Mol Biol. 2024 Aug 26;46(3 Suppl 1):e20230127. doi: 10.1590/1678-4685-GMB-2023-0127. eCollection 2024. Genet Mol Biol. 2024. PMID: 39186710 Free PMC article.
- Effect of subchorionic hematoma on first-trimester maternal serum free β-hCG and PAPP-A levels. Akay A, Reis YA, Şahin B, Öncü AK, Obut M, İskender C, Çelen Ş. Akay A, et al. Rev Bras Ginecol Obstet. 2024 Jul 26;46:e-rbgo66. doi: 10.61622/rbgo/2024rbgo66. eCollection 2024. Rev Bras Ginecol Obstet. 2024. PMID: 39176201 Free PMC article.
- Clinical predictive value of pre-pregnancy tests for unexplained recurrent spontaneous abortion: a retrospective study. Wang J, Li D, Guo Z, Ren Y, Wang L, Liu Y, Kang K, Shi W, Huang J, Liao S, Hao Y. Wang J, et al. Front Med (Lausanne). 2024 Aug 7;11:1443056. doi: 10.3389/fmed.2024.1443056. eCollection 2024. Front Med (Lausanne). 2024. PMID: 39170044 Free PMC article.
- Depression after pregnancy loss: the role of the presence of living children, the type of loss, multiple losses, the relationship quality, and coping strategies. Balle SR, Nothelfer C, Mergl R, Quaatz SM, Hoffmann S, Hoffmann H, Allgaier AK, Eichhorn K. Balle SR, et al. Eur J Psychotraumatol. 2024;15(1):2386827. doi: 10.1080/20008066.2024.2386827. Epub 2024 Aug 14. Eur J Psychotraumatol. 2024. PMID: 39140607 Free PMC article.
- Trends, spatiotemporal variation and decomposition analysis of pregnancy termination among women of reproductive age in Ethiopia: Evidence from the Ethiopian demographic and health survey, from 2000 to 2016. Tebeje TM, Seifu BL, Seboka BT, Mare KU, Chekol YM, Tesfie TK, Gelaw NB, Abebe M. Tebeje TM, et al. Heliyon. 2024 Jul 14;10(14):e34633. doi: 10.1016/j.heliyon.2024.e34633. eCollection 2024 Jul 30. Heliyon. 2024. PMID: 39130402 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
Grants and funding
- 212233/Z/18/Z/WT_/Wellcome Trust/United Kingdom
LinkOut - more resources
Full text sources.
- Elsevier Science
Other Literature Sources
- The Lens - Patent Citations
- scite Smart Citations
- Genetic Alliance
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 7, Issue 3
- Experience of miscarriage: an interpretative phenomenological analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- S Meaney 1 , 2 ,
- P Corcoran 1 ,
- N Spillane 2 ,
- K O'Donoghue 2 , 3
- 1 National Perinatal Epidemiology Centre, University College Cork, Ireland
- 2 Pregnancy Loss Research Group, Dept. of Obstetrics and Gynaecology, University College Cork, Ireland
- 3 The Irish Centre for Fetal and Neonatal Translational Research (INFANT), University College Cork, Ireland
- Correspondence to Dr S Meaney; s.meaney{at}ucc.ie
Objective The objective of the study was to explore the experiences of those who have experienced miscarriage, focusing on men's and women's accounts of miscarriage.
Design This was a qualitative study using a phenomenological framework. Following in-depth semistructured interviews, analysis was undertaken in order to identify superordinate themes relating to their experience of miscarriage.
Setting A large tertiary-level maternity hospital in Ireland.
Participants A purposive sample of 16 participants, comprising 10 women and 6 men, was recruited.
Results 6 superordinate themes in relation to the participant's experience of miscarriage were identified: (1) acknowledgement of miscarriage as a valid loss; (2) misperceptions of miscarriage; (3) the hospital environment, management of miscarriage; (4) support and coping; (5) reproductive history; and (6) implications for future pregnancies.
Conclusions One of the key findings illustrates a need for increased awareness in relation to miscarriage. The study also indicates that the experience of miscarriage has a considerable impact on men and women. This study highlights that a thorough investigation of the underlying causes of miscarriage and continuity of care in subsequent pregnancies are priorities for those who experience miscarriage. Consideration should be given to the manner in which women who have not experienced recurrent miscarriage but have other potential risk factors for miscarriage could be followed up in clinical practice.
- QUALITATIVE RESEARCH
- pregnancy loss
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
https://doi.org/10.1136/bmjopen-2016-011382
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This study uses interpretative phenomenological analysis in order to interpret the experience of miscarriage.
Much of the research in relation to pregnancy loss is focused on women's experience. Purposive sampling was undertaken to ensure that both women's and men's experiences were included in this study.
Participants from this study were drawn from a large tertiary maternity hospital with a dedicated pregnancy loss clinic and it may be possible that their experiences may differ from those who attend a hospital where such a clinic is not available to them.
Miscarriage is the most common adverse outcome in pregnancy. This study highlights the need for the provision of appropriate clinical information as well as supportive information when counselling individuals who experienced miscarriage.
Introduction
Improvements in the quality of care provided during pregnancy have led to substantial reductions in perinatal and maternal mortality as well as a reduction in other adverse pregnancy outcomes. 1 However, these advances have had little effect on the high rate of miscarriage with between 20% and 30% of pregnancies ending in miscarriage. 1 , 2 Until now, much of the research has aimed to identify potential risk factors as the underlying aetiology of miscarriage is not well understood. 2
Studies indicate the need for familial and social support following miscarriage as it can be an extremely painful and upsetting experience, 3 , 4 with some women experiencing medical complications. 5 , 6 Quantitative studies indicate that the experience of miscarriage can negatively impact on the men's and women's psychological well-being. 4 , 7–14 These studies also report that the high levels of stress and anxiety experienced 7–9 can endure for 6–12 months following miscarriage. 8
In contrast, an interventional study in the USA examined the changes of women's feeling over the course of year following miscarriage. Swanson et al 15 found that women's responses recorded at 1 year were not significantly different from those recorded at 6 weeks. Considering the high incidence of miscarriage and the reported impact on the emotional well-being of people, there are comparatively few studies that have qualitatively examined the experience of miscarriage. Of these, most studies focused on the women's experience of miscarriage 3 , 16–18 whereby the male experience has been reported based on the women's perspective. 16 , 19 Our study builds on these findings as it aimed to explore the experiences of people who have experienced miscarriage. The purpose of this study was to focus on men's and women's accounts of miscarriage. Through a qualitative analysis, the objective of the study was to gain detailed insight into their expectations of pregnancy as well as their experience of miscarriage diagnosis and management.
An interpretative phenomenological analysis (IPA) was undertaken as this approach has its theoretical foundations in phenomenology. 20–22 Phenomenology examines perceptions and engages with the way individuals reflect on the experiences they deem significant in their lives. 21 Researchers who engage in IPA acknowledge how experience is subjective and is therefore only accessible through interpretation. 20 IPA has an ideographic approach which allows the researcher to rigorously explore how these experiences may affect a person. 20 IPA has increasingly been used in healthcare research as its ideographic approach facilitates researchers to rigorously explore how specific phenomena may affect a patient and consequently will impact on patient care. 20
The study took place in a large tertiary-level Irish maternity hospital. The sample was initially recruited from a list of women who had previously participated in a prospective cohort study regarding miscarriage 23 and agreed to be contacted for future research. It is important to note that there are geographical variations for the definition of miscarriage. For the purposes of this study, miscarriage was defined as any pregnancy loss which occurred before 24 weeks gestation in a fetus weighing <500 g. Participants were eligible for the study if they were aged 18 years and older and had experienced one or more miscarriages. Letters were sent to invite women and their partners to participate in the present study by the primary author. If an opt-out form was not returned, the primary author made contact to provide more detailed information about the study. Over the course of the study, six opt-out forms were returned. Three participants were recruited using snowballing techniques, through contact with the Miscarriage Association of Ireland and/or through the bereavement and loss hospital team. Information on the study was forwarded to them and they made contact with the primary author to become involved in the study. None of the participants were known to the researcher.
The primary author recruited until data saturation was met. The final sample consisted of 16 participants (10 female and 6 male), 4 of whom were couples ( table 1 ). All the participants signed an informed consent and were interviewed individually, by the primary author (an experienced female qualitative researcher), using a semistructured interview schedule ( table 2 ). All the interviews were conducted in a room onsite in the maternity hospital or a location convenient to the participant, with the exception of one interview that was undertaken by telephone under participant request. Each interview was digitally recorded and contemporaneous notes were taken immediately after each interview. The average interview was 43 min, ranging from 28 to 69 min in length.
- View inline
Overview of the sample
Overview of the semistructured interview schedule
The IPA involved: first listening and re-reading the interviews a number of times to ensure that a general sense of the participants' accounts were acquired. Second, emergent themes were initially identified which were then refined as similar themes were clustered together and subordinate and superordinate themes were identified. Patterns and connections across each individual transcript were examined. Finally, a master table of themes was created after each transcript was integrated into the final analysis. All analyses were carried out using Nvivo V.10 software (QSR International, Doncaster, Australia) by the primary author, a health sociologist. The analyses were then presented to the co-authors for review.
Analysis of the data indicated six superordinate themes in relation to the participant's experience of miscarriage: acknowledgement of miscarriage as a valid loss, misperceptions of miscarriage, the hospital environment, management of miscarriage, support and coping, reproductive history and implications for future pregnancies.
Acknowledgement of miscarriage as a valid loss
“But the miscarriage itself, I'd say it was until then…and the whole discussion became a very public thing…it was only at that stage that I started to move on from it and that would have been five years, five years later and it was always something that would of upset me…it is hard to know what you are grieving for in a way because it is fleeting, you know the whole experience of being pregnant and then not being pregnant and thinking if I didn't remember this baby then who would.” (P15, male, two miscarriages)
“At this stage I think we had attended a couple of the, of the October, the ahhh annual ahhhh [prompt from interviewer; the annual service of remembrance] yeah. And again they are huge out pouring of grief, and of joy for life, but of grief. The people there and the support, but the fact that there are children and parents and grandparents, it just gives a sense that look it doesn't matter what age you are, doesn't matter how wealthy you are, doesn't matter what colour you are, we have all experienced this in our own way and we are all here today to remember that. And, I think for me, that, that was [pause] I haven't missed one yet and I'll still be going for another while yet. You know, that's a lovely outreach and very important.” (P13 male, two miscarriages)
“What I think happens, from my own experience, is I don't think it is recognised enough. Like cancer is recognised, god help us we have all had it and all those things. But a loss, it's a different loss when it's a child. They're still a child, they may not be grown but they're still a child” (P1, female, two miscarriages)
The acknowledgement of the loss through miscarriage, both by people and through ritual, was of importance. Participants discussed marking or remembering their loss in a variety of ways such as keeping a diary, writing of poems and songs or through the organisation of a funeral or similar ceremony. Some participants spoke of the importance of rituals particularly around the anniversary of the miscarriage in order to continue to acknowledge their loss. A number of participants remarked about the significance of attending the annual service of remembrance, which is organised by the hospital.
Misperceptions of miscarriage
“I got spotting and I thought surely it's not going to happen again, cause they [people] always say one spontaneous [miscarriage] but you never (pause) but I think with miscarriage people just don't talk about it and they just don't think that it happens to everybody and they don't think it is as common as it is until you talk to other people about it. So I think the perception I would have had was if you had one you're not really likely to have another, that's what I thought.” (P3, female, four miscarriages)
“A friend of mine in work is pregnant and it's her first pregnancy and she's not kind of as worried as I am for her. She is oblivious and naïve and while I'm thinking ‘oh god’ she is saying ‘it's fine’.” (P7, female, two miscarriages)
“Well when I did have the miscarriage and I said it to people, everyone says ‘oh you know I had one’ and it all comes out from the woodwork and em everyone knows someone who has had a miscarriage. It's so common how could you not but people generally don't talk about it…you don't have the knowledge…people need to know that this can happen.” (P11, female, three miscarriages)
The hospital environment and management of miscarriage
When the participants spoke about how they were treated in the hospital, they remarked about how divergent an experience it was. The participants stated that any negative experiences in the hospital were related to the administration and/or physical design of the hospital specifically relating to the emergency department and the general clinics. When the women were miscarrying, they first attended the emergency department and found it difficult to be sitting in the waiting area surrounded by women attending with varying symptoms. This was considered one of the hardest aspects of the miscarriage experience as they felt they could not express any emotion (eg, anger or upset) relating to their loss, as they did not wish to distress the other pregnant women.
“We came straight up here [the maternity hospital] and we went into the emergency place downstairs and we were seen straight away. But there were other patients and staff behind curtains, we were behind ours waiting on the doctor to come round. And there were nurses in there chatting and they were laughing and chatting and jokes and stuff, which they are entitled to have…but I was there with [husband] and we were worried sick that we were losing our baby and the doctor came in and she went through all the things and said ‘No, I can't find a fetal heartbeat, it's gone’. Well, I started roaring crying, I was so upset but all the life was happening all around us, carrying on you know happily in behind the curtains…it was absolutely horrendous. But they organised for me to come back to the early pregnancy clinic, you know I didn't have to speak to anybody we just left the hospital [pause] that was hard.” (P8, female, seven miscarriages)
“That was hugely traumatic, cause em, I didn't miscarry the same as the last time it just went on and on and on. I was in and out of here [maternity hospital] every second day for blood tests. The first day they went up a bit and then they went down a bit and then it was kind of, like, and it was just two weeks really of turmoil.” (P4, female, three miscarriages)
“I woke up an hour later and I just completely haemorrhaged and I passed out a couple of times. Then I got in the bath and em, I was saying god people should warn people or prepare people if they are going to have miscarriages, cause I didn't know what was happening to me. And em what I excreted was unbelievable cause I was 12 weeks. And I started vomiting and I passed out again and then he rang the hospital. I tried talking to the hospital but I couldn't get the words out I was so weak at this point, you know, and they told me to come straight in. So I did and they killed me [slang: were annoyed with me] when I got in cause they said I should've called the ambulance.” (P3, female, three miscarriages)
“The first and the last were spontaneous and the last two I had to take medication but it would of happened inevitably but I, I just wanted to speed up [the miscarriage]…” (P5, female, four miscarriages)
Participants experienced anxiety about attending the hospital to get tests over a number of days to confirm the loss of their baby. This was relatively impractical for some with work commitments, but was also difficult as they did not want to reattend the hospital to face the inevitable diagnosis. Many of the women expressed how they had suspected that something was wrong but had no knowledge of what to expect or what is considered normal while miscarrying. Those who miscarried at a later gestation discussed how they were wholly unprepared for the extent of the bleeding when they miscarried ( box 3 ). When women had a choice, most chose to have some form of medical intervention. A number of factors influenced the decision to choose to intervene with women citing other commitments such as having to take care of other children in the family.
Support and coping
Keeping busy helped participants cope with their loss; this was particularly evident in the participants who already had children. Participants were hesitant to receive formal support by way of counselling and most opted for support from family, friends and/or support groups instead. Men felt that their primary role was to support their partners through the loss and, at times reluctantly, while planning subsequent pregnancies. During subsequent pregnancies, the participants disclosed that high levels of anxiety were experienced. They spoke of how they navigated through the pregnancy focusing on specific gestational weeks as goals, including exceeding the gestation they had experienced their miscarriage(s) at, as well as those coinciding with clinic appointments at the maternity hospital. Many of the participants detailed how these actions meant they could not fully enjoy the experience of being pregnant.
“I was upset for a good while after but I had the other three [children] to keep me going [slang: busy] with school and everything…I had the D&C the same week as my daughter's communion, so I had to just go ahead and get on with things you know, I had to be happy for her.” (P10, female, two miscarriages)
“I'd say we were slightly different in that if we had called it a day at the end of number seven, we both would have been extremely disappointed but you know I think, em, it's more about protection I suppose, I didn't want to have to go through it again. The decision was extremely difficult, now I mean [wife] was very much in favour of going forward and trying again, em, I would have been a bit more reticent I suppose, em a bit more, you know, a bit more nervous about it. Obviously she had major concerns but you I think, I think it was a case of a tough decision but we just went for it.” (P9, male, seven miscarriages)
“I love babies and if someone was to say on Friday that you are pregnant and you are going to have to have the baby tomorrow, I would say yeah that's great but I just can't do the, the nine months of worrying.” (P7, female, two miscarriages)
“I went up to the [early pregnancy clinic] and they said ‘the next time you get pregnant call us here and come in and we will do a scan, we will do an early scan, we will give you that reassurance’. That made a huge difference, it made a huge difference because it felt like ok someone is not saying ‘yeah, yeah, yeah move it along, move it along, next person’ someone is actually saying ‘we care about you, we know this is hard and the next time you get pregnant we know it's going to be distressful for the first few weeks so come in and we will give you scans’. And they were so good about it and when I did get pregnant it was one of the first calls I did make.” (P12, female, two miscarriages)
Reproductive history and implications for future pregnancies
“We already had a loss, I know they were two, two different losses but I was thinking not again, what is going on, is there something wrong with me, am I ever going to have children.” (P1, female, two miscarriages)
“One of the things that I asked for was an appointment with [the specialist in pregnancy loss]to have tests done to see why I was having the miscarriages but I was told I would have to have 3 miscarriages before they would see me and I was kind of thinking, do they not take age into account? You know, you have to have three and I think two is an adequate level at my age. If I was in my twenties maybe you'd manage the three but not at my age.” (P4, female, three miscarriages)
Medical investigations, such as karyotyping, are not offered to women unless they have experienced recurrent miscarriage (three consecutive miscarriages). 24 Participants expressed frustration that these tests were not offered to them following a second miscarriage. This dissatisfaction was heightened in women who felt that other risk factors, such as advancing maternal age, should be considered ( box 5 ).
The findings of this qualitative study indicate that the experience of miscarriage has a considerable impact on men and women. Findings from this study support what has been reported by others, that there is a need for increased awareness in relation to the frequent occurrence of miscarriage. Miscarriage is a common occurrence, yet as revealed by these participants it is not until a miscarriage was experienced that the participants were made aware of these high rates. A study from the USA also indicated that people believe that miscarriage is a rare complication of pregnancy. 25 The participants from this study believed that improvement of information provision would be beneficial in allowing individuals to better prepare for the possibility that their pregnancy could end in miscarriage and, if it does occur, that support is available.
Second, given that a cause cannot be determined in as many as 50% of miscarriages, it was felt that having this information in advance may alleviate some of the guilt experienced. Participants emphasised that such information provision should also focus on the physical aspects of miscarrying. These findings mirror those of Moohan et al , 26 whereby women felt unprepared when miscarrying spontaneously and were questioning of whether what they had experienced was normal. Wong et al 27 support this finding by detailing how miscarriage may be a physically traumatic event as women may experience considerable and sudden pain, loss of blood and may need to be hospitalised. Similar to the longitudinal study by Côté-Arsenault, 28 the participants in this study indicated how pregnancy following miscarriage was stressful. There is a need for improved communication between healthcare professionals and patients to better counsel patients through the miscarriage and provide reassurance in subsequent pregnancies.
One coping strategy adopted by men and women was focusing on commitments, particularly taking care of other children in the family. In a review of the literature on grief following miscarriage, Brier states that having living children has also been used as an indicator for the importance attached to the pregnancy. This belief is based on the assumption that the absence of living children is associated with a relatively greater desire for children. 29 Wong et al 27 also highlight how, given this belief, it is also assumed that women with children will be less emotionally distressed and are less likely to receive emotional support from nursing staff. In contrast, the findings from this study illustrated that these participants were affected emotionally and did go through a grieving process irrespective of gestation of the pregnancy loss or whether they had living children or not. The findings also indicated the importance that healthcare professionals acknowledge miscarriage and how appreciative participants were of the support given to them.
It has been documented that men and women grieve differently following miscarriage in the literature, 30 , 31 and these findings are also reflected in the accounts of the participants in this study. Similar to Johnson and Puddifoot, 31 the men in this study indicated that they were less likely to openly discuss the miscarriage unless prompted by another person with a similar experience. This was also the case with discussing the impact of the miscarriage on them with their partners with the men identifying their primary role as that of a support to their partner. However, as outlined by Brier, 29 this could suggest differences in the general expression of emotion and grief rather than affective reactions to miscarriage. Although the men in this study did not actively seek out support, they did reiterate that certain experiences and rituals were helpful for their grieving process as they allowed them to mark and remember their loss.
Participants in this study were reasonably satisfied with the care provided to them by the hospital. However, a number of shortcomings with the system were identified. When miscarrying, the first contact with the maternity hospital was with the emergency room. It was felt that waiting for extended periods of time in an area with other pregnant women was particularly difficult and a situation which hospital management should be more sensitive to. Wong et al 27 outlined that in previous studies women believed that medical staff do not consider miscarriage as either important or an emergency and considered medical staff insensitive and unsympathetic about accommodation. Our findings build on these results whereby participants identified this insensitivity to be as a result of the hospital setting rather than medical staff. Participants were appreciative of staff, especially those whom they considered to be knowledgeable and those who displayed understanding and compassion. The dedicated early pregnancy clinic was an environment they believed could be further developed to enhance the care currently provided to women when they are miscarrying.
Consistent with a number of other studies, 1 , 4 , 27 all the participants expressed a desire to determine the cause of the miscarriage. Participants expressed dissatisfaction that they were ineligible to have tests to fully investigate the cause of their miscarriage as they had not experienced the requisite three consecutive miscarriages. In our study, this perceived inadequacy in service provision was amplified in women of advancing maternal age. As Brier 29 outlines, maternal age can potentially influence an individual's goals with regard to childbearing. Advancing maternal age in combination with a number of losses experienced by a woman may impact on the duration and intensity of grief experienced. The women in this study expressed dissatisfaction with their ineligibility for investigations, maintaining that staff should appreciate that although they had not experienced recurrent miscarriage, there were other risk factors, such as their age, to be considered.
As part of the analysis, it is important to consider any factors which may influence the results. The participants in the study all made reference to the dedicated early pregnancy loss clinic. This clinic is staffed by a dedicated pregnancy loss team. Such a dedicated clinic is not available in all hospitals. Thus, the presence of such a team in the hospital may have raised awareness about miscarriage among other medical staff and influenced how they cared for the participants sampled here. It is important to note, that although a qualitative methodology was deemed appropriate for this study, the findings of such studies are context-specific. The experiences of the women and men in this study may or may not reflect the experiences of those who attend other units with differing resources and practices. Notwithstanding these limitations, given the level of agreement with other studies, we feel that these results add additional insight into the experiences of miscarriage.
Conclusions
This study highlights that a thorough investigation of the underlying causes of miscarriage and continuity of care in subsequent pregnancies are priorities for those who experience miscarriage. The provision of appropriate clinical information as well as supportive information when counselling individuals who are experiencing a miscarriage is important. Consideration should be given to the manner in which women who have not experienced recurrent miscarriage but have other potential risk factors for miscarriage could be followed up in clinical practice.
Acknowledgments
The authors are grateful to the participants for participating in the study and giving of their time freely.
- Simmons RK ,
- Maconochie N , et al
- Maconochie N ,
- Prior S , et al
- Adolfsson A
- Peloggia A ,
- Grimes D , et al
- Saraiya M ,
- Shulman H , et al
- Neugebauer R
- Nikcevic AV ,
- Tunkel SA ,
- Kuczmierczyk AR , et al
- Geller PA ,
- Maruyama T ,
- Koizumi T , et al
- Hiley A , et al
- Serrano F ,
- Swanson KM ,
- Jolley SN , et al
- Gerber-Epstein P ,
- Leichtentritt RD ,
- Benyamini Y
- Glasser JK ,
- Sundaram ME
- Wojnar DM ,
- Adolfsson AS
- Karmali ZA ,
- Powell SH , et al
- Biggerstaff D ,
- Thompson AR
- Flowers P ,
- Lutomski JE ,
- Corcoran P , et al
- ↵ RCOG Green-top Guideline No. 17 . The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage . Royal College of Obstetricians and Gynaecologists , April 2011 .
- Friedenthal J , et al
- Crawford TJ ,
- Gask L , et al
- Côté-Arsenault D
- Willner H ,
- Deckardt R , et al
- Johnson MP ,
- Puddifoot JE
Twitter Follow Sarah Meaney @sarahmeaney5
Contributors SM and KOD contributed to and were responsible for the conception and design of the study. SM and NS were responsible for data collection. SM was responsible for transcription, data analysis and the initial drafting of the article. SM, PC, NS and KOD contributed to revising the manuscript critically for important intellectual content; final approval of the version to be published and the decision to submit the article for publication.
Funding This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Ethics approval Ethical approval for the study was provided by the Clinical Research Ethics Committee of the Cork Teaching Hospitals (CREC; Reference: ECM 4 (iii) 10/01/12).
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional data are available.
Read the full text or download the PDF:
- Research article
- Open access
- Published: 19 November 2018
University students’ awareness of causes and risk factors of miscarriage: a cross-sectional study
- Indra San Lazaro Campillo ORCID: orcid.org/0000-0001-7281-8424 1 , 2 ,
- Sarah Meaney 1 , 2 ,
- Jacqueline Sheehan 1 ,
- Rachel Rice 1 &
- Keelin O’Donoghue 1
BMC Women's Health volume 18 , Article number: 188 ( 2018 ) Cite this article
7687 Accesses
9 Citations
15 Altmetric
Metrics details
Spontaneous miscarriage is the most common complication of pregnancy, occurring in up to 20% of pregnancies. Despite the prevalence of miscarriage, little is known regarding peoples’ awareness and understanding of causes of pregnancy loss. The aim of this study was to explore university students’ understanding of rates, causes and risk factors of miscarriage.
A cross-sectional study including university students. An online questionnaire was circulated to all students at the University College Cork using their university email accounts in April and May 2016. Main outcomes included identification of prevalence, weeks of gestation at which miscarriage occurs and causative risk factors for miscarriage.
A sample of 746 students were included in the analysis. Only 20% ( n = 149) of students correctly identified the prevalence of miscarriage, and almost 30% ( n = 207) incorrectly believed that miscarriage occurs in less than 10% of pregnancies. Female were more likely to correctly identify the rate of miscarriage than men (21.8% versus 14.5%). However, men tended to underestimate the rate and females overestimate it. Students who did not know someone who had a miscarriage underestimated the rate of miscarriage, and those who were aware of some celebrities who had a miscarriage overestimated the rate. Almost 43% ( n = 316) of students correctly identified fetal chromosomal abnormalities as the main cause of miscarriage. Females, older students, those from Medical and Health disciplines and those who were aware of a celebrity who had a miscarriage were more likely to identify chromosomal abnormalities as a main cause. However, more than 90% of the students believed that having a fall, consuming drugs or the medical condition of the mother was a causative risk factor for miscarriage. Finally, stress was identified as a risk factor more frequently than advanced maternal age or smoking.
Although almost half of the participants identified chromosomal abnormalities as the main cause of miscarriage, there is still a lack of understanding about the prevalence and most important risk factors among university students. University represents an ideal opportunity for health promotion strategies to increase awareness of potential adverse outcomes in pregnancy.
Peer Review reports
Miscarriage is one of the most common complications in pregnancy [ 1 ]. It is estimated that one out of four clinically recognised pregnancies will end in miscarriage during the first-trimester, and approximately 1% of pregnant women will experience a second-trimester miscarriage [ 2 ]. Despite the prevalence of miscarriage, 50% are attributed to chromosomal abnormalities [ 3 ], and a considerable percentage are classified as unexplained [ 4 ]. Therefore, identifying risk factors and effective interventions to prevent miscarriage has become a priority in the medical and scientific community [ 5 ]. Well-known risk factors include advanced maternal and paternal age, heavy smoking, alcohol consumption, infertility and previous miscarriage [ 6 , 7 , 8 , 9 , 10 ].
Preconception health care aims to identify and increase awareness to reduce risk factors before pregnancy that might affect the future maternal, child and family health [ 11 , 12 , 13 ]. An effort has been made to develop effective intervention plans and to include preconception risk factors in prenatal prevention programs internationally [ 14 , 15 , 16 , 17 , 18 ]. One of the main recommendations is to promote effective preconception health care interventions to develop curricula of preconception risk factors at undergraduate and postgraduate level [ 15 ]. Insight into students’ awareness of miscarriage might help to assess the effectiveness of preconception care education at a university level, but also to highlight the gaps of knowledge among this targeted population. Therefore, a cross-sectional study was conducted to explore university students’ understanding of prevalence, causes and risk factors of miscarriage.
Study design and data source
A cross sectional study was carried at University College Cork (UCC). Cork is one of the three cities in the Republic of Ireland with the highest full-time enrolments in the academic year 2016/2017 [ 19 ]. UCC currently has 20,000 full-time students of whom 14,000 are undergraduate [ 19 ]. It has over 3000 international students from 100 countries around the world. There are over 120 degree and professional programmes in Medicine, Dentistry, Pharmacy, Nursing and the Clinical Therapies, along with the Humanities, Business, Law, Architecture, Science, Food and Nutritional Sciences, available at UCC. Students were asked to select their area of study at UCC from a list of six options. For the purpose of this study, this list was grouped into four categories in accordance with the organisation of the Colleges within the University (i.e. The College of Medicine and Health, The College of Arts and Social Science, The College of Engineering & Food Science and The College of Business and Commerce & Law) [ 20 ]. For example, the College of Medicine and Health includes the Schools of Medicine, Dental School, Clinical Therapies, Nursing and & Midwifery, Pharmacy and Public Health.
An online questionnaire was circulated to all students at UCC using their university email accounts, in April and May 2016. The questionnaire was compiled using SurveyMonkey®, which is a user-friendly site to develop and administer online surveys. The questionnaire was anonymous and voluntary. An informed consent form explaining the objectives of the survey had to be completed before accessing the questionnaire. The main questionnaire consisted of twenty-six questions utilised to assess students’ understanding of the topic of miscarriage. Topics included general demographic and educational characteristics (i.e. sex, age, marital status, discipline and level of study), general knowledge and risk factors for miscarriage (i.e. agree, disagree and unsure of both well-known and spurious risk factors), identification of previous experience of miscarriage among themselves or their partners, and awareness of family member, friends or a celebrity who had a miscarriage. Students were asked to select the most common causes of miscarriage from a list of six options including lifestyle of mother (i.e. smoking and alcohol), medical condition or medical problem with the mother; genetic problem with the baby; psychological problems during pregnancy (i.e. stress, depression) and incident during pregnancy (i.e. fall, injury, accident). In addition, students were asked to provide rates of miscarriage in Ireland (i.e. “ In your opinion, what percentage of pregnancies in Ireland ends in a miscarriage? Please insert a number anywhere from 0 to 100 %”) and weeks of gestation at which miscarriage occurs (“ when can a miscarriage occur? Between week “x” to week “x” of a pregnancy ”).
Definitions of miscarriage vary significantly between countries and jurisdictions [ 21 ]. For the purposes of this study, miscarriage is defined as the spontaneous demise of a pregnancy from the time of conception up to 24 completed weeks of gestation [ 22 , 23 , 24 ]. This study also reported the number of students who were only aware of first trimester miscarriage, which is defined as the loss of a pregnancy up to 12 weeks of gestation [ 22 , 23 , 24 ]. It is estimated that approximately one fifth of clinical pregnancies will end in a miscarriage in Ireland [ 24 ]. Therefore, a rate of 20% of miscarriage was selected as the cut-off rate in this study.
Statistical analysis
Descriptive analysis was carried out using mean and standard deviation (SD) for continuous variables and percentages for categorical variables. Age was categorised using tertiles (i.e. 33.3% of the students were 21 years old or younger and 66.7% were 23 years old or younger). Three categories were created to calculate the number of students who underestimated (i.e. below the correct answer), correctly estimated or overestimated (i.e. above the correct answer) the rate of miscarriage. Information regarding the university students’ knowledge about contributory risk factors of miscarriage was assessed using a 5-point Likert scale ranging from strongly agree to strongly disagree. In the context of this study, answers were categorised as agree, unsure and disagree.
Chi-square tests were performed to assess the relationship between general demographic and educational characteristics, and knowing someone who had a miscarriage and identifying the correct rate of miscarriage. Chi-square tests were also calculated to investigate the relationship between independent variables and awareness of the most common causes of miscarriage. Binary logistic regression was calculated to estimate the probability of selecting risk factors for miscarriage (i.e. agree versus disagree) and general demographic and educational characteristics, knowing or not someone who had a miscarriage (i.e. themselves, partners, family, friends or celebrities) and whether the rate of miscarriage was correct, underestimated or overestimated. A high number of university students were unsure of their answers, and therefore, we also explored the relationship between agree versus unsure in the identification of risk factors for miscarriage; however, only those results which showed statistically significant differences and which added extra information to the comparison were reported.
A total number of 25 possible causes of miscarriage were alphabetically ordered in the questionnaire. For the purpose of this study we only analysed the Odds Ratios for those risk factors with a strong association with miscarriage (i.e. age, chromosomal abnormalities, smoking, alcohol and medical condition of mother) and for some spurious risk factors for miscarriage (i.e. flu vaccine, flying, hair dye, verbal arguments and vitamin C). Unadjusted and adjusted odds ratios (OR and aOR respectively) were calculated for all independent variables with their corresponding 95% confidence intervals (CI). All the analyses were performed using SPSS 21.0 (IBM).
Overall, 872 students responded to the online survey. Of those, 126 were excluded from the analysis because they did not complete more than half of the survey or they had highly extreme answers in demographic characteristic such as age. Therefore, a total sample of 746 university students were included in our analysis. The mean age was 24.3 years (SD = 6.58), and most of students were between 21 and 22 years old ( n = 284; 38.1%) or were 23 years old or older ( n = 289; n = 38.7%) ranging between 18 and 60 years old. More than half of the respondents were females ( n = 577; 77.3%), and approximately 80% were single ( n = 617). The discipline with the lower response rate was Business and Commerce and Law ( n = 104; 13.9%) and with the highest response rate was Medicine and Health ( n = 280; 31.9%).
Male students were more likely to report that they did not know anyone who had a miscarriage compared to female students (23.9% versus 9.6%; p < 0.001). Students aged 23 years old or older were more likely to report they knew someone who had a miscarriage; however, students of 20 years of age or younger were more likely to report they were aware of a celebrity who had had a miscarriage ( p < 0.05). Single students were also more likely not to know anyone who had a miscarriage compared to those who had a partner, were married, were cohabiting or divorced (14.1% versus 5.8%; p < 0.05). Females were more likely to be aware of a celebrity who had a miscarriage than male students (16.9% versus 7.0%, Table 1 ). Students from Engineering and Food Science ( n = 34; 18.3%) or Business and Commerce and Law ( n = 14; 14.9%) disciplines were more likely to report that they did not know anyone with a miscarriage. Medicine and Health ( n = 159; 74%), and Arts and Social Science ( n = 130; 72.6%) were more likely to know someone who had a miscarriage (Table 1 ).
Only 20% ( n = 149) of students identified a mean rate of 20% for miscarriage. The remaining students underestimated or overestimated the rate of miscarriage (Table 2 ). Female students, older students and those who knew someone who had a miscarriage were more likely to identify the 20% rate of miscarriage. Students from Arts and Social Science ( n = 45, 22.5%) and Medicine and Health ( n = 52, 21.9) were more likely to estimate the correct rate of miscarriage (Table 2 ). A total of 96 (12.9%) students correctly responded that miscarriage happens up to 12 weeks of gestation (early miscarriage) or up to 24 weeks of gestation (late miscarriage). Overall, only 54 (6.2%) students were aware that miscarriage can happen from conception until 24 weeks of gestation. A quarter of all students ( n = 179; 24%) thought miscarriage could happen at any stage of pregnancy.
The most common cause of miscarriage identified by the university students was chromosomal abnormalities in the baby, ( n = 316; 42.4%), followed by medical conditions ( n = 177; 23.7%) and lifestyles ( n = 109; 14.6%). Chromosomal abnormalities of the baby were identified as the most common cause of miscarriage in a higher percentage of female students, older students (i.e. 23 years old or older), students who reported being married, divorced or cohabiting, students from Medicine and Health and for those students who knew a celebrity who had a miscarriage. Male students, younger and single students, students from Engineering and Food Science and Business and Commerce and Law, and students who reported that they did not know anyone who had a miscarriage were more likely to report lifestyles and the medical condition of the mother as the most common cause of miscarriage (Table 3 ).
Students who correctly estimated the rate of miscarriage were more likely to select chromosomal abnormalities as the main cause of miscarriage ( n = 72; 48.3% for correct rate of miscarriage, n = 136; 45.9% for overestimated rate and n = 107; 36.3% for underestimated rate; Table 3 ). Conversely, students who correctly identified the rate of miscarriage were less likely to select psychological problems as the main cause of miscarriage. Students who overestimated the rate of miscarriage were less likely to identify medical conditions of the mother as a cause of miscarriage, whereas those who underestimated were more likely to select it. Approximately 15% (underestimated rate n = 42; correct rate n = 22 and overestimated rate n = 44) of students selected lifestyle behaviour as the main cause of miscarriage independently of the selected rate of miscarriage (Table 3 ).
The most reported risk factors for miscarriage were accident or fall, drugs, medical condition of the mother, alcohol, stress, age smoking and being underweight. Most students disagreed that sexual intercourse, hair dye, vitamin C and exercise were risk factors for miscarriage (Fig. 1 ).
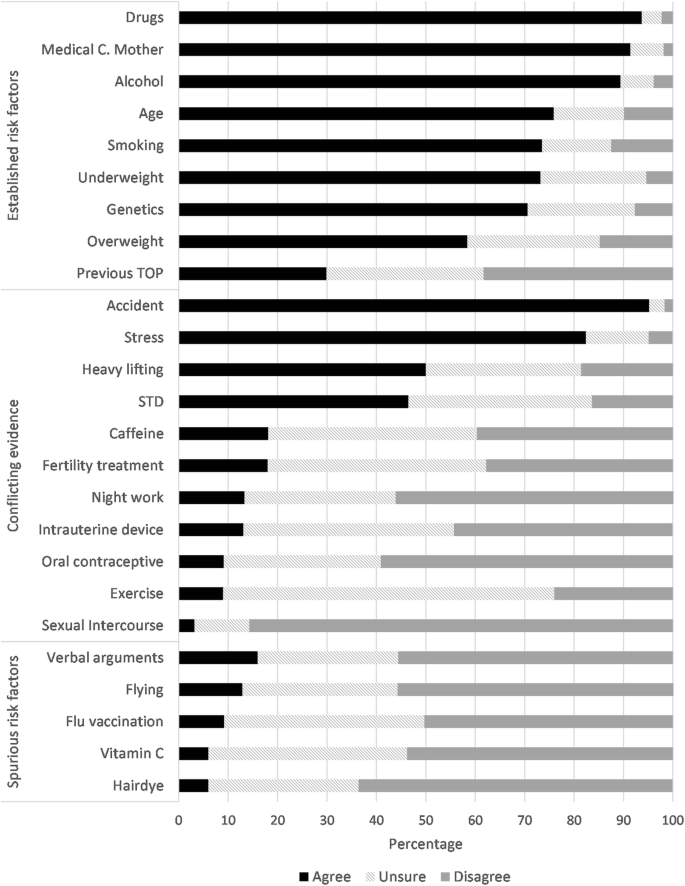
Percentage of most selected risk factors for miscarriage
Overall, the majority of college students correctly selected age ( n = 566; 88%) and medical conditions of the mother ( n = 682; 98%) as contributory risk factors for miscarriage. No statistically significant differences between agree or disagree responses for age or for medical conditions of mother were found between groups (Additional file 1 : Table S1). However, students from Arts and Social Science were more likely to be unsure about age as a risk factor (aOR 2.78; 95% CI 1.52–5.09). Students of 21 years of age or older were more likely to identify chromosomal abnormalities as a causative factor for miscarriage than those aged 20 years old or younger (students aged 21–22: aOR 0.27; 95% CI 0.12–0.61 and students aged 23 years old or older: aOR 0.48; 95% CI 0.24–0.96; Additional file 1 : Table S1). Students from Arts and Social Science or Business and Commerce and Law more frequently did not identify chromosomal abnormalities as a potential causative factor compared to college students from Medical and Health (aOR 2.40; 95% CI 1.01–5.73 and aOR 3.0; 95% CI 1.16–7.73 respectively; Additional file 1 : Table S1).
Male students were more likely to agree that smoking was a risk factor for miscarriage compared to female students (aOR 0.47; 95% CI 0.24–0.94). Older students (i.e. 23 years old or older) disagreed more frequently that smoking was a risk factor for miscarriage compared to students who were 20 years old or younger (aOR 2.09; 95% CI 1.08–4.07). Compared to students from Medicine and Health, the remaining disciplines disagreed more frequently that smoking was a risk factor. For alcohol, older students and those from Business and Commerce and Law were more likely to disagree that it was a risk factor for miscarriage (Additional file 1 : Table S1).
Students from Arts and Social Science were more likely to identify flu vaccination as a risk factor for miscarriage ( n = 25; 26.9%; Additional file 1 : Table S2). Students from Engineering and Food Science and Business and Commerce and Law were more likely to identify verbal arguments as a risk factor for miscarriage (aOR 0.56; 95% CI 0.31–0.99 and aOR 0.42; 95% CI 0.21–0.82). Students between 21 and 22 years old were more likely to be unsure that vitamin C was a risk factor for miscarriage compared to younger students (aOR 2.85; 95% CI 1.21–6.72; Additional file 1 : Table S2). Only students who were 23 years old or older were more likely to identify vitamin C as a spurious risk factor compared to students who were 20 years old or younger (aOR 2.34; 95% CI 1.03–5.34; Additional file 1 : Table S2).
Among the remaining potential causative risk factors for miscarriage, male students were less likely to identify working night shifts and previous termination of pregnancy (TOP) as risk factors (aOR 0.45; 95% CI 0.25–0.80and aOR 0.44; 95% CI 0.26–0.72). Older students (i.e. 23 years old or older) were less likely to identify caffeine as a risk factor (aOR 2.61; 95%CI 1.45–4.70). Compared to students from the college of Medicine and Health, those from Business and Commerce and Law were less likely to identify sexually transmitted disease, previous TOP and being underweight as contributory risk factors for miscarriage (aOR 3.39; 95% CI 1.77–6.51 and aOR 2.20; 95% CI 1.13–4.25 and aOR 2.79; 95% CI 1.10–7.03). Students from Engineering and Food Science were less likely to identify night work as a risk factor, but were more likely to consider stress as a contributory risk factor for miscarriage compared to Medicine and Health students (aOR 2.06; 95%CI 1.08–3.93 and aOR 0.36; 95% CI 0.13–0.98). The odds of not identifying oral contraceptive as a cause of miscarriage were lower for students who overestimated the rate of miscarriage compared to those who correctly identified the rate (OR: 0.30; 95% CI 0.12–0.75). Finally, only students from Arts and Social Science were more likely to identify heavy lifting as a risk factor.
Main findings
This cross-sectional study provides insight into university students’ awareness of prevalence and risk factors of miscarriage. The findings of this study illustrate that common misunderstandings still prevail regarding the aetiology of miscarriage, suggesting a deficiency in formal information and access to information related to reproductive health. For example, only 20% of the students correctly identified the prevalence of miscarriage at 20%, and almost 30% incorrectly believed the prevalence of miscarriage is less common than 10%. Female students were more likely to identify the correct rate, but also to overestimate it, and male students tended to underestimate it. Almost one-quarter of the students believed miscarriage can happen from conception until birth, and 87% of the students erroneously selected the weeks of gestation at which miscarriage occurs. Females students, older students, those from Medicine and Health, those who were aware of a celebrity who had a miscarriage, and those who identified the correct rate of miscarriage were more likely to identify chromosomal abnormalities as the most common cause of miscarriage. However, this was only identified by 43% of the total sample.
Strengths and limitations
The nature of the study design implies that data were collected at one point in time. Previous studies have found an association between ethnicity and religion and the perception of risk factors for miscarriage [ 25 ], however we did not include this information in our survey and no comparison can be made. One of the main limitations is that a higher percentage of female students responded to the survey compared to male students. Although similar gender distributions were reported at UCC in the academic year 2006/2007 (36% male and 64% females) [ 26 ], recent overall data shows a more equal gender distribution for third-level graduates in the Republic of Ireland in 2016, with 52.2% of the students being female [ 27 ]. This percentage is similar to the European Union (EU-28) in 2015 [ 28 ]. Nevertheless, our sample seems to be representative of the overall distribution of male and females by discipline. In 2016, women represented more than three out of four (76.4%) graduates in Health, and more than four out of five (82.4%) graduates in Engineering were male [ 27 ] in the Republic of Ireland.
No standardised instrument of relevance was found in the literature for the purpose of this study; and therefore our survey was not validated. A multidisciplinary team specialised in pregnancy loss developed and reviewed all questions. In addition, a patient advocate for women who experience pregnancy loss also reviewed the questionnaire to ensure clarity. To our knowledge, this is one of the largest studies exploring the knowledge of rates and risk factors for miscarriage among college students from multiple disciplines, representing the main strength of this study.
Comparison with other studies
Our study is in keeping with the results of two previous studies [ 25 , 29 ]. In a cross-sectional study including 1084 adults located in 49 states within the United States, Bardos et al. found that half of the participants believed that miscarriage was uncommon, occurring in 5% or less of all pregnancies. Similar to our results, it also found that approximately one fifth of the respondents incorrectly believed that lifestyle behaviours such as consumption of drugs, alcohol or tobacco were the only cause of miscarriage. In addition, men were more likely to identify lifestyle behaviours as a contributing risk factor for miscarriage. Also, participants with a higher educational degree identified chromosomal abnormalities more frequently as a cause of miscarriage compare to less educated respondents [ 25 ]. It is important to note that approximately 80% of these participants attended some college or medical school. Interestingly, in our study, male students were also more likely to identify smoking as a contributing risk factor. In another study, Delgado et at assessed awareness among undergraduate students related to preconception health and pregnancy. Results showed a low to moderate level of awareness, with women having a slightly higher awareness than men [ 29 ].
Assessing the reasons behind overestimating or underestimating the risk of miscarriage is difficult to understand [ 30 ]. It could be possible that students who overestimate the risk of miscarriage were under unnecessary stress or anxiety at the time of this study. Some studies have shown a link between psychological distress and anticipatory representations of possible future threats or overestimating the risk of a disease [ 31 , 32 ]. No studies have evaluated college students’ psychological and lifestyles factors and perception of risk of pregnancy loss; therefore, more research needs to be done to assess which are the underlying factors that might impact on population’s perception of risk of pregnancy loss.
Implications
Despite the high occurrence of miscarriage, some studies highlight the potential barriers that might influence the lack of awareness of this topic among the general public. For example, the existence of guilt, shame or feeling responsible for the pregnancy loss might have reinforced the reclusion of the topic exclusively to the close family or friends, or in some cases, only among the couple who experience miscarriage [ 33 , 34 ]. This has led to miscarriage being a “taboo” or “unspoken” topic in some cultures, increasing the chance of the causes of miscarriage being surrounded by myths and folklore [ 25 , 35 ]. The potential benefits of promoting healthy behaviours, lifestyle, mental and social factors during women and men’s reproductive years has been increasingly accepted in the medical and scientific community [ 13 , 36 ].In this context, preconception health care is a unique opportunity to increase personal responsibility and awareness of risk factors and adverse pregnancy outcomes during the reproductive years of this targeted population [ 16 ].
Universities are underused settings for improving preconception health among the community. They provide an opportunity to reach a population with a diverse socioeconomic and gender background. In a scoping review of 29 preconception health care interventions evaluations, six of them were delivered at a School, college or university settings [ 17 ]. All of them reported an improvement in preconception health knowledge [ 29 , 37 , 38 , 39 , 40 ]; however, most of the interventions were provided to women who were identified as being at-risk of developing adverse maternal outcomes, and men were not generally included in the interventions [ 37 ]. Although the Republic of Ireland has one of the highest birth rates in Europe [ 41 ], to our knowledge, there are no preconception healthcare intervention programmes or clinical practice guidelines focused on improved preconception healthcare in higher education settings.
According to our results and the little evidence available, misunderstanding of causes and risk factors for miscarriage is a public health issue. The findings of this study highlight an opportunity for public health interventions to improve reproductive health education. Universally preconception healthcare programmes successfully provide health promotion strategies to increase awareness of potential adverse outcomes in pregnancy. In particular, University settings are an ideal opportunity to reach a targeted population.
Abbreviations
Adjusted odds ratios
Confidence intervals
European Union of 28 member states
Unadjusted odds ratios
Standard deviation
Termination of pregnancy
University College Cork
Jurkovic D, Overton C, Bender-Atik R. Diagnosis and management of first trimester miscarriage. BMJ. 2013;346:f3676.
Article Google Scholar
Zinaman MJ, Clegg ED, Brown CC, O’Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996;65(3):503–9.
Article CAS Google Scholar
Larsen EC, Christiansen OB, Kolte AM, Macklon N. New insights into mechanisms behind miscarriage. BMC Med. 2013;11.
Regan L, Rai R. Epidemiology and the medical causes of miscarriage. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14(5):839–54.
Prior M, Bagness C, Brewin J, Coomarasamy A, Easthope L, Hepworth-Jones B, Hinshaw K, O’Toole E, Orford J, Regan L, et al. Priorities for research in miscarriage: a priority setting partnership between people affected by miscarriage and professionals following the James Lind Alliance methodology. BMJ Open. 2017;7(8):e016571.
De La Rochebrochard E, Thonneau P. Paternal age and maternal age are risk factors for miscarriage; results of a multicentre European study. Hum Reprod. 2002;17(6):1649–56.
Weintraub AY, Sergienko R, Harlev A, Holcberg G, Mazor M, Wiznitzer A, Sheiner E. An initial miscarriage is associated with adverse pregnancy outcomes in the following pregnancy. Am J Obstet Gynecol. 2011;205(3):286.e1-5.
Hyland A, Piazza KM, Hovey KM, Ockene JK, Andrews CA, Rivard C, Wactawski-Wende J. Associations of lifetime active and passive smoking with spontaneous abortion, stillbirth and tubal ectopic pregnancy: a cross-sectional analysis of historical data from the Women’s health initiative. Tob Control. 2015;24(4):328–35.
Armstrong DS. Impact of prior perinatal loss on subsequent pregnancies. J Obstet Gynecol Neonatal Nurs. 2004;33(6):765–73.
Venners SA, Wang X, Chen C, Wang L, Chen D, Guang W, Huang A, Ryan L, O’Connor J, Lasley B, et al. Paternal smoking and pregnancy loss: a prospective study using a biomarker of pregnancy. Am J Epidemiol. 2004;159(10):993–1001.
Seshadri S, Oakeshott P, Nelson-Piercy C, Chappell LC. Prepregnancy care. BMJ. 2012;344:e3467.
Jack BW, Culpepper L. Preconception care. Risk reduction and health promotion in preparation for pregnancy. JAMA. 1990;264(9):1147–9.
Preconception Health and Health Care [ https://www.cdc.gov/preconception/index.html ]. Accessed 23 May 2018.
Atrash HK, Johnson K, Adams M, Cordero JF, Howse J. Preconception care for improving perinatal outcomes: the time to act. Matern Child Health J. 2006;10(5 Suppl):S3–11.
Johnson K, Posner SF, Biermann J, Cordero J, Atrash HK, Parker CS, Boulet SL, Curtis MG. Recommendations to improve preconception health and health care - United States. A report of the CDC/ATSDR preconception care work group and the select panel on preconception care. JSTOR. 2006;55:1–23.
Google Scholar
Shawe J, Delbaere I, Ekstrand M, Hegaard HK, Larsson M, Mastroiacovo P, Stern J, Steegers E, Stephenson J, Tyden T. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur J Contracept Reprod Health Care. 2015;20(2):77–87.
Hemsing N, Greaves L, Poole N. Preconception health care interventions: a scoping review. Sex Reprod Healthc. 2017;14:24–32.
Boulet SL, Parker C, Atrash H. Preconception care in international settings. Matern Child Hlth J. 2006;10(5 Suppl):S29–35.
Higher Education Authority: Key Facts and Figures ( 2016/2017 ) . In Dublin: Higher Education Authority; 2018.
University College Cork. University College Cork. National University of Ireland, Cork. Principal statute. In: Universities Act 1997. Ireland: University College Cork; 2009.
Wright PM. Barriers to a comprehensive understanding of pregnancy loss. J Loss Trauma. 2011;16(1):1–12.
Royal College of Physicians of Ireland: Ultrasound Diagnosis of Early Pregnancy Miscarriage. In: National Clinical Guidelines in Obstetrics and Gynaecology. Republic of Ireland: Royal College of Physicians of Ireland, RCPI; 2010.
Royal College of Obstetricians and Gynaecologists: The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. In.: Royal College of Obstetricians and Gynaecologists; 2011.
Royal College of Physicians of Ireland. The management of second trimester miscarriage. In: National Clinical Guidelines in Obstetrics and Gynaecology. Republic of Ireland: Royal College of Pysicians of Ireland, RCPI; 2017.
Bardos J, Hercz D, Friedenthal J, Missmer SA, Williams Z. A national survey on public perceptions of miscarriage. Obstet Gynecol. 2015;125(6):1313–20.
Irish Universities Association. Irish Universities Study. Gender at a glance: Evidence from the Irish Universities Study. Ireland: Irish Universities Association; 2009.
Central Statistics Office. Women and Men in Ireland 2016 [ https://www.cso.ie/en/releasesandpublications/ep/p-wamii/womenandmeninireland2016/education/#d.en.140093 ] Accessed 3 Aug. 2018.
European Commission. Eurostat. Tertiary education statistics [ http://ec.europa.eu/eurostat/statistics-explained/index.php/Tertiary_education_statistics#Gender_distribution_of_participation ] Accessed 3 Aug. 2018.
Delgado CE. Undergraduate student awareness of issues related to preconception health and pregnancy. Matern Child Health J. 2008;12(6):774–82.
Sjoberg L. Factors in risk perception. Risk Anal. 2000;20(1):1–11.
Audrain J, Schwartz MD, Lerman C, Hughes C, Peshkin BN, Biesecker B. Psychological distress in women seeking genetic counseling for breast-ovarian cancer risk: the contributions of personality and appraisal. Ann Behav Med. 1997;19(4):370–7.
Grupe DW, Nitschke JB. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat Rev Neurosci. 2013;14(7):488–501.
Broen AN, Moum T, Bodtker AS, Ekeberg O. The course of mental health after miscarriage and induced abortion: a longitudinal, five-year follow-up study. BMC Med. 2005;3:18.
Barr P. Guilt- and shame-proneness and the grief of perinatal bereavement. Psychol Psychother. 2004;77(Pt 4):493–510.
Schaffir J. Do patients associate adverse pregnancy outcomes with folkloric beliefs? Arch Womens Ment Health. 2007;10(6):301–4.
Hussein N, Kai J, Qureshi N. The effects of preconception interventions on improving reproductive health and pregnancy outcomes in primary care: a systematic review. Eur J Gen Pract. 2016;22(1):42–52.
Dejoy SB. Pilot test of a preconception and midwifery care promotion program for college women. J Midwifery Women Health. 2014;59(5):523–7.
Gardiner P, Hempstead MB, Ring L, Bickmore T, Yinusa-Nyahkoon L, Tran H, Paasche-Orlow M, Damus K, Jack B. Reaching Women Through Health Information Technology: The Gabby Preconception Care System. Am J Health Promot. 2013;27(3):Es11–20.
Richards J, Mousseau A. Community-based participatory research to improve preconception health among Northern Plains American Indian adolescent women. Am Indian Alaska Nat. 2012;19(1):154–85.
Schiavo R, Conzalez-Flores M, Ramesh R, Estrada-Portales I. taking the pulse of progress toward preconception health: preliminary assessment of a national OMH program for infant mortality prevention. J Commun Healthc. 2013;4(2):106–17.
Department of Health. Creating a better future together: National Maternity Strategy 2016-2026. Ireland: Department of Health Dublin. p. 2016.
Download references
Acknowledgements
Not applicable.
Ethical approval and consent to participate
This study received ethical approval from the Clinical Research Ethics Committee of the Cork Teaching Hospital on ECM 6 (rrrr) 120,416. Consent to participate was implied through completed surveys.
This study was supported by departmental funding. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Pregnancy Loss Research Group, The Irish Centre for Fetal and Neonatal Translational Research, University College Cork, Cork, Ireland
Indra San Lazaro Campillo, Sarah Meaney, Jacqueline Sheehan, Rachel Rice & Keelin O’Donoghue
National Perinatal Epidemiology Centre, Department of Obstetrics and Gynaecology, University College Cork, 5th floor, Cork University Maternity Hospital, Wilton, Cork, T12 YE02, Ireland
Indra San Lazaro Campillo & Sarah Meaney
You can also search for this author in PubMed Google Scholar
Contributions
JS, RR, SM and KOD conception and designed of the survey. JS obtained the data and ISLC analysed them. ISLC and SM interpreted the data. The questionnaire was anonymous and data were only accessed by the authors involved in the study. We confirm that all authors included in this study participated in the drafting and have approved the manuscript for submission. This manuscript has not been published and is not under consideration for publication elsewhere. We have no conflicts of interest to disclose.
Corresponding author
Correspondence to Indra San Lazaro Campillo .
Ethics declarations
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Table S1. Odds Ratios of agreement with strong risk factors for miscarriage. Table S2. Odds Ratios of disagreement with spurious risk factors for miscarriage. (DOCX 33 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
San Lazaro Campillo, I., Meaney, S., Sheehan, J. et al. University students’ awareness of causes and risk factors of miscarriage: a cross-sectional study. BMC Women's Health 18 , 188 (2018). https://doi.org/10.1186/s12905-018-0682-1
Download citation
Received : 29 June 2018
Accepted : 07 November 2018
Published : 19 November 2018
DOI : https://doi.org/10.1186/s12905-018-0682-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Miscarriage
- University students
- Risk factors
BMC Women's Health
ISSN: 1472-6874
- General enquiries: [email protected]
- Open access
- Published: 31 March 2023
Factors that shape recurrent miscarriage care experiences: findings from a national survey
- Caragh Flannery 1 , 2 ,
- Marita Hennessy 1 , 2 ,
- Rebecca Dennehy 1 , 2 ,
- Karen Matvienko-Sikar 3 ,
- Con Lucey 4 ,
- Jennifer Ui Dhubhgain 4 &
- Keelin O’Donoghue 1 , 2
BMC Health Services Research volume 23 , Article number: 317 ( 2023 ) Cite this article
1875 Accesses
4 Citations
14 Altmetric
Metrics details
Learning what matters to women/couples with recurrent miscarriage (RM) is essential to inform service improvement efforts and future RM care practices. Previous national and international surveys have examined inpatient stays, maternity care, and care experiences around pregnancy loss, but there is little focus on RM care. We aimed to explore the experiences of women and men who have received RM care and identify patient-centred care items linked to overall RM care experience.
Between September and November 2021, we invited people who had experienced two or more consecutive first trimester miscarriages and received care for RM in Ireland in the ten-year period prior to participate in a cross-sectional web-based national survey. The survey was purposefully designed and administered via Qualtrics. It included questions on sociodemographics, pregnancy and pregnancy loss history, investigation and treatment for RM, overall RM care experience, and patient-centred care items at various stages of the RM care pathway such as respect for patients' preferences, information and support, the environment, and involvement of partners/family. We analysed data using Stata.
We included 139 participants (97% women, n = 135) in our analysis. Of the 135 women, 79% were aged 35–44 years ( n = 106), 24% rated their overall RM care experience as poor ( n = 32), 36% said the care they received was much worse than expected ( n = 48), and 60% stated health care professionals in different places did not work well together ( n = 81). Women were more likely to rate a good care experience if they had a healthcare professional to talk to about their worries/fears for RM investigations (RRR 6.11 [95% CI: 1.41–26.41]), received a treatment plan ( n = 70) (RRR 3.71 [95% CI: 1.28–10.71]), and received answers they could understand in a subsequent pregnancy ( n = 97) (RRR 8 [95% CI: 0.95–67.13]).
Conclusions
While overall experience of RM care was poor, we identified areas that could potentially improve people’s RM care experiences – which have international relevance – such as information provision, supportive care, communication between healthcare professionals and people with RM, and care coordination between healthcare professionals across care settings.
Peer Review reports
Recurrent miscarriage (RM) affects 1–3% of the reproductive-aged population [ 1 ]. However, international guidelines vary in how it is defined [ 2 ]. The Royal College of Obstetricians and Gynaecologists [ 3 ] define RM as three or more first-trimester miscarriages (which do not have to be consecutive or with the same partner). The Practice Committee of the American Society for Reproductive Medicine [ 4 ] describes it as the loss of two or more consecutive pregnancies. Similarly, the European Society of Human Reproduction and Embryology now also define RM as the loss of two or more pregnancies, with the sequence of the miscarriages not necessarily consecutive [ 5 ].
Guidelines recommend that care for women with RM should be offered within a dedicated RM clinic [ 6 , 7 ]. Healthcare professionals with the necessary skills and expertise [ 5 , 8 , 9 ], and those with a sub-specialisation in RM, provide a better standard of care when assessed against current guidelines [ 10 ]. RM clinics are consultant-led, non-acute and offer specialist investigations, support, and treatment to women/couples [ 6 , 7 ]. In addition, they provide care plans to reduce the risk of further losses through treatments and addressing modifiable risk factors, where appropriate [ 6 , 7 ]. Ideally, couples are seen together and given accurate information to facilitate decision-making about future pregnancies [ 5 ]. While there is limited evidence that this approach improves pregnancy outcomes, couples report valuing such care plans, and guidelines advocate for this approach [ 1 , 11 ].
Quality in healthcare is shaped by the experiences and engagement of patients, families, caregivers, and professionals [ 12 , 13 , 14 , 15 , 16 , 17 ]. While ensuring that patients' perspectives and contributions to their healthcare decisions are considered and responded to accordingly, in general, it is not perceived to occur between women and maternity services following RM [ 18 , 19 ]. While clinical practice guidelines for RM describe investigations and treatments, some do not provide mechanisms to ensure patient-centred care is guided by the values and needs of women/couples [ 20 , 21 ]. As patient experience is multifaceted [ 22 ], learning what matters to women/couples during RM is essential to inform service improvement efforts and future RM care practices.
Previous national and international surveys have examined inpatient stays, maternity care, and care experiences around pregnancy loss, but there is little focus on RM care [ 23 , 24 , 25 , 26 , 27 ]. This study aimed to explore the experiences of women and men who have received RM care in Ireland and identify patient-centred care items linked to overall RM care experience.
The Strengthening the Reporting of Observational Studies in Epidemiology checklist [ 28 ] was used to inform reporting of the findings. Ethical approval was granted by the Clinical Research Ethics Committee of the Cork Teaching Hospitals, University College Cork (ECM 4 (jj) 09/03/2021 & ECM 3 (jj) 19/10/2021).
Study design
A cross-sectional study using an anonymous web-based survey was conducted to examine the experience of people who have interacted with the health services following RM.
Sample selection and survey distribution
Women and men over 18 who experienced two or more consecutive first-trimester miscarriages in the preceding ten years (2010–2021), and who received care for RM in Ireland were invited to participate. Two or more consecutive first-trimester miscarriages were selected based on growing consensus and updated guidelines [ 5 , 29 ], and the period of ten years was chosen to reflect the research and investment in miscarriage services in Ireland following the Miscarriage Misdiagnosis Review in 2010 [ 30 , 31 , 32 ]. The terms women and men are used throughout the paper, but participants were asked to identify themselves as ‘Mother/I carried the pregnancy’ or ‘Father/partner’ in the survey.
We used self-selection or voluntary response sampling, a type of non-probability sampling, where individuals volunteer themselves, i.e. responded to an open call for participants. This is a common approach for samples that need to meet specific criteria. We did this to develop an understanding of a smaller, under researched population in Ireland. We distributed the survey through existing professional, collegial and support networks, and the Clinical Midwife Specialists in Bereavement and Loss in each of the 19 maternity units/hospitals across Ireland from September to November 2021. The link to the survey was shared through email distribution lists, websites, newsletters, and social media, including those of the research team and the INFANT Research Centre, the Pregnancy Loss Research Group, and miscarriage/ pregnancy loss organisations. Recruitment materials, including posters/flyers and business cards, were tailored to women and men by including photos and quotes from those with lived experience of RM, which were also distributed nationally throughout pregnancy loss clinics and early pregnancy assessment units. Women and men with recurrent miscarriage in line with the eligibility criteria were invited to take part in the study through this open call for participants. Information about the study was presented to potential participants when they clicked the survey link and they then provided informed consent prior to completing the survey.

Survey design
In a questionnaire consisting of 10 sections, 165 questions were purposefully designed using relevant literature [ 1 , 19 , 33 , 34 ] and existing care experience surveys [ 5 , 12 , 27 , 35 ] related to maternity care and/or pregnancy loss. Research findings from the RE:CURRENT Project [ 2 , 36 ] informed the questionnaire, specifically qualitative research with healthcare professionals and women and men who had experienced RM [ 37 ] to tailor care experience questions to this cohort and ensure that relevant questions were being asked. The final questionnaire (see Additional File 1 ) was developed by the Research Team in consultation with key stakeholders, including parent advocates from the RE:CURRENT Research Advisory Group.
The structured questionnaire consisted of questions across several areas, including sociodemographic information, pregnancy and pregnancy loss history, investigations, receiving results and treatment for RM, follow-up care for subsequent pregnancies, the impact of RM, information, and support provision. The RE:CURRENT Project research team, and members of the RE:CURRENT Research Advisory Group, and Pregnancy Loss Research Group at Cork University Maternity Hospital, piloted the survey. After this pilot, changes were made to the wording, layout, and the selection of required responses within the online survey platform. The survey was formatted and managed using Qualtrics [ 38 ] with the advice and support of the RE:CURRENT Research Advisory Group.
Survey measures
Stages of the rm care pathway.
Tailored questions for women and men were used, with women asked more specific questions relating to the care they received to explore their experiences at various stages of the RM pathway.
For investigations, women were asked if they had investigations for RM ( yes vs no ); if investigations were offered ( vs requested ); the wait time for investigations ( less than one month, 1–2 months , 3–4 months, 5–12 months, I don't know/I can't remember ); types of medical tests ( yes vs no ) for medical history, blood test, ultrasound, MRI, hysteroscopy, genetic testing of pregnancy tissue, genetic tests or other. Finally, women were asked if they felt that their healthcare professionals did everything to investigate the cause of their RM ( no, yes definitely, yes to some extent ).
Women were asked if they received their results ( yes vs no ); the wait time for results ( less than one month, 1–2 months , 3–4 months, 5–12 months, I don't know/I can't remember ); who provided their results ( yes vs no ) general practitioner, midwife or nurse in the hospital, a sonographer, consultant in a public hospital, doctor in a public hospital, private consultant, healthcare professional at a fertility clinic, admin staff or other; if results were received by ( phone, email, face-to-face, virtual contact, other ) and if the results provided answers for the cause of their RM ( no, yes, I don't know ). Women were also asked if a treatment plan was put in place ( yes vs no ); if their healthcare professional did everything they could treat their RM ( no, yes definitely, yes to some extent ); if they had a subsequent pregnancy ( yes vs no ); if they were offered early reassurance scans ( yes vs no ) and if their healthcare professionals did everything to support them during their subsequent pregnancy ( no, yes definitely, yes to some extent ).
Patient-centred care items
The survey contained additional patient-centred care items [ 33 ], including questions relating to respect for patients' preferences, information and support, the environment and involvement of family at various stages of the RM care pathway (Table 1 ).
Outcome measure
Women and men were asked to rate their overall RM care experience, on a scale from 1–10, with one being 'a very poor experience' and ten 'a very good experience'. Due to small numbers in some categories, participant ratings were recoded as poor (rating 1–3), satisfactory (rating 4–6) and good (rating 7–10) for this analysis.
Participant characteristics
Women and men were asked to provide details of their: age ( 18–24 years, 24–34 years, 35–44 years, 55–64 years, 65 + years ); nationality ( Irish vs. non-Irish ); relationship status ( married, living with a partner, separated or divorced, single, prefer not to say ); education ( primary school or less, some secondary school, completed secondary school, post-secondary school technical training, university degree, postgraduate certificate or diploma, postgraduate degree (Masters or PhD) ); employment ( employed full-time, employed part-time, self-employed, employed casually, full-time student, part-time student, not employed, prefer not to say, other ); medical cover ( medical card or GP visit cardholder, private health insurance, none of the above ); number of consecutive losses ( two consecutive, three consecutive, more than three consecutive ); the year initial RM care received ( between 2011—2021 ); ever diagnosed with infertility ( yes vs no ).
The data were checked by CF to ensure all participants met the inclusion criteria. Analysis was carried out using Stata V.13 [ 39 ]. Descriptive analyses were carried out for all variables through the RM care pathway. Associations between sample characteristics and care experience were explored using χ2 test. Unadjusted multinomial logistic regression was conducted to examine the association between patient-centred care items throughout the RM care pathway and overall RM care experience rating. Adjusted multinomial logistic regression analysis was not performed due to varying sample sizes through the RM pathway.
Sample characteristics
A total of 213 participants completed the survey. However, 74 participants were not eligible for this analysis as they did not experience a consecutive miscarriage ( n = 63) or did not receive care between 2011 and 2021 ( n = 11). Of the eligible participants ( n = 139), 97% were women ( n = 135). Due to the small number of men ( n = 4) (see Additional File 2 ), this section only presents results for women who participated. Of the women participants, 79% were aged 35–44 years ( n = 106), 85% were married ( n = 114), 39% had postgraduate degrees ( n = 53) with 80% having private health insurance ( n = 108). Furthermore, 57% had experienced two consecutive miscarriages ( n = 77), 75% had received care in the last five years (2016–2021), and 24% had been diagnosed with infertility ( n = 32) (Table 2 ).
Participant's rating of overall RM care experience
Rating of overall RM care experience was characterised as follows: poor (44%, n = 60), satisfactory (39%, n = 52) and good (17%, n = 23). Based on χ2 test, overall RM care experience rating was not associated with participant characteristics (Table S3.1, Additional File 3 ).
Participant's experiences of the various stages of the RM care pathway
Participants' experiences of the various stages of the RM care pathway are depicted in Fig. 1 (Also, see supporting data, Tables S3.2-S3.7, Additional File 3 ). Of the participants ( n = 135), 66% had discussed RM with a healthcare professional, 53% had investigations for RM ( n = 71), 62% requested these investigations ( n = 44), 35% waited between 3–4 months for investigations ( n = 25) to take place, and 49% felt their healthcare professional did not do everything to investigate their RM ( n = 35).
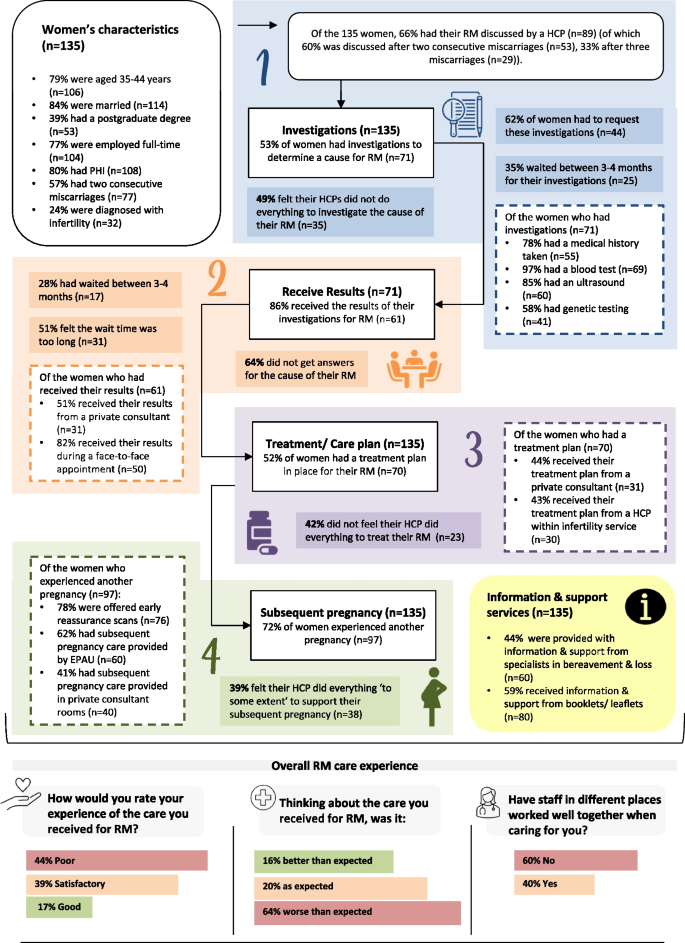
Overview of women’s experiences of the various stages of the RM care pathway HCP, healthcare professional; RM, recurrent miscarriage; EPAU, early pregnancy assessment unit; PHI, private health insurance
Of the participants who had investigations ( n = 71), 86% received their results ( n = 61), 28% waited 3–4 months for results ( n = 17), 51% felt the wait time was too long, 51% received results from a private consultant ( n = 31), and 64% did not get answers about causes of their RM ( n = 39). Furthermore, 52% had a treatment plan in place ( n = 70), of which 44% received their treatment plan from a private consultant ( n = 31), and 42% did not feel their healthcare professional did everything to treat their RM ( n = 23).
Finally, 72% experienced another pregnancy ( n = 97), of which 78% were offered early reassurance scans ( n = 76), and 39% felt their healthcare professional 'to some extent' did everything to support their subsequent pregnancy ( n = 38). When thinking about their RM care, 64% said it was worse than expected ( n = 87), with 60% stating that healthcare professionals did not work well together during their care ( n = 84).
Patient-centred care items throughout the RM care pathway and overall RM care experience
In the unadjusted multinomial logistic regression, some patient-centred care items for investigations, receiving results, treatment plans and subsequent pregnancy were linked to either satisfactory or good RM care experience (see Additional File 4 ).
For participants who had RM investigations ( n = 71), those who requested these were less likely to report a good RM care experience relative to those who were offered investigations (RRR 0.19 [95% CI:0.48–0.71]). Participants who received verbal information (RRR 13.10 [95% CI: 2.48–60.30]), written information (RRR 5.37 [95% CI: 1.06–27.00]) and answers they could understand regarding investigations (RRR 8.89 [95% CI: 1.03–76.68]) were more likely to report a good overall RM care experience. Also, participants who had a healthcare professional to talk to about their worries/fears (RRR 6.11 [95% CI: 1.41–26.41]) and whose partner could ask questions about investigations (RRR 3.83 [95% CI: 1.01–14.48]) were more likely to report a good overall RM care experience.
For participants who received their RM investigation results (n = 61), those who received information about their results (RRR 10.21 [95% CI: 1.15–90.53]) had a healthcare professional to talk to about their worries/fears (RRR 18.70 [95% CI: 2.09–167.27]) and whose partner could ask questions about their investigation results (RRR 5.88 [95% CI: 1.30–26.51]) were more likely to report a good overall RM care experience.
Participants who received a treatment plan ( n = 70) were more likely to rate a good care experience (RRR 3.71 [95% CI: 1.28–10.71]). Also, participants that had a healthcare professional to talk to about their worries and fears surrounding their treatment (RRR 12 [95% CI: 2.25–63.98]) and who reported that they felt their healthcare professional did everything to treat their RM (RRR 36 [95% CI: 4.05–320.12]) were more likely to rate a good care experience.
For participants who had a subsequent pregnancy ( n = 97), those who were offered reassurance scans were more likely to rate a satisfactory care experience (RRR 3.27 [95% CI: 1.10–9.67]) or a good care experience (vs poor) (RRR 8.96 [95% CI: 1.07–74.91]) compared to those who did not get reassurance scans. Participants who received answers they could understand (RRR 8 [95% CI: 0.95–67.13]), had someone they could contact with questions (RRR 12.00 [95% CI: 2.40–60.05]) and had a healthcare professional they could talk to about their worries/fears (RRR 6.43 [95% CI: 1.29–32.0]) concerning their subsequent pregnancy were more likely to rate a good care experience.
This study aimed to explore the experiences of women and men who have received RM care in the Republic of Ireland, exploring their experiences at various stages of the RM care pathway and identifying patient-centred care items linked to their overall care experience. Despite an open call to recruit women and men, only four men participated in this survey, highlighting the already recognised challenge of recruiting men for reproductive health and pregnancy loss research [ 40 , 41 ]. Previous research indicated that men may 'feel in the way' during the miscarriage process; therefore, more inclusivity is needed, and a couple-focused approach to care and support implemented [ 42 , 43 ].
Of the women who participated ( n = 135), 44% rated a poor overall RM care experience ( n = 60), with 64% stating the care was worse than expected ( n = 87) and 60% reporting that healthcare professionals did not work well together ( n = 84) then providing their RM care. However, across the RM care pathway, a range of patient-centred care items such as having a healthcare professional to talk to about worries and fears, partners involvement, receiving enough information and having time to discuss and be involved in decisions regarding investigations and subsequent pregnancies were linked to a satisfactory or good rating of RM care experience.
A clear gap exists between the care women want and the care they receive [ 19 , 37 , 44 ]. Like previous international research, women reported a poor RM care experience, with RM care worse than expected, citing a lack of information, communication, and follow-up care [ 45 , 46 , 47 , 48 ]. In Ireland, miscarriage is not officially recorded and is most likely underreported, as not all women attend hospital for miscarriage care [ 16 , 17 , 18 , 19 ]. Despite increased allocation of resources following the Miscarriage Misdiagnosis Review in 2010 in Ireland, pregnancy loss/miscarriage services are still seen as a low priority [ 30 , 31 ]. Miscarriage data is required to compare miscarriage/RM rates among countries, accelerate research, improve patient care, and support advocacy efforts and policy development [ 1 ].
In this study, women felt that healthcare professionals across different care settings did not work well together, indicating a lack of communication, undermining RM care and support consistency. Multidisciplinary teams are required for RM to enhance and encourage knowledge-sharing between healthcare professionals, allowing for effective communication between primary and secondary care and other services (emergency department/fertility/perinatal mental health). Moreover, in line with previous international research, results indicated a better care experience if women were given time to discuss and actively contribute to their RM care [ 44 , 49 ]. Women want more effective doctor-patient communication, which requires interventions to change long-established behaviours and perceptions of both staff and patients [ 47 ]. Providing care through dedicated RM clinics would facilitate a multi-disciplinary approach, open communication channels, and encourage teamwork between healthcare professionals.
Research indicates that providing physical, emotional and psychological support, and information and education for family and friends about pregnancy loss is key to improving care experience [ 24 ]. Women were more likely to rate a satisfactory or good RM care experience if they had received enough information regarding their miscarriage, particularly concerning investigations and results. The consequences of RM can be profound and life-changing for women/partners/families and, as such, the provision of supportive care should be central to the management of women/couples [ 45 ]. In tandem with emotional and informational support from healthcare professionals, as varying consistency/trustworthiness of information exists, women and men should be supported to mobilise evidence-based information and support for themselves [ 46 ]. Geller and colleagues [ 46 ] provided a table of well-established websites that can be distributed to women and valuable educational resources for healthcare professionals. Women are more likely to rate a satisfactory or good RM care experience if they had a healthcare professional to talk to about their worries and fear at each stage of the RM care pathway. In a study where women who attended follow-up appointments with healthcare professionals to discuss their miscarriages, women were less likely to experience psychological distress [ 48 ].
Overall, these findings align with the work of others internationally that has highlighted the need to invest in a better model of care that supports women/couples with RM while including women/couples in improvement efforts [ 12 , 50 , 51 ]. Dedicated RM clinics, where skilled and experienced healthcare professionals, provide women/couples with treatment plans, education, and continuous support into the next pregnancy within a dedicated service have been implemented nationally and internationally [ 7 ] as a potential solution. In the UK, a graded model of care has been put forward to address the balance between evidence-based management and supportive care and healthcare resources, with care pathways based on the first and subsequent miscarriages [ 11 ]. To ensure patient-centred care items are achieved, these approaches offer concrete solutions to help individualise care according to women’s and their partner's needs and preferences [ 6 , 7 ]. Future research in needed to check the scalability and sustainability of such models of care to maximise the impact on health outcomes and to respond to budgetary constraints in the health system [ 52 , 53 ].
Strengths and limitations
Our findings add to the extant knowledge base on the care experiences of people who experience pregnancy loss, addressing an important gap in the literature specifically regarding RM. While our study was conducted in Ireland, our findings regarding overall care experiences are similar to those observed in other international studies. This study employed a strict inclusion criterion that included women/men who had experienced two or more first-trimester miscarriages, and as the guidelines and definitions for RM vary, some women/men were excluded from this analysis. As ten years were chosen to reflect the research and investment in miscarriage services in Ireland since 2010 following the Miscarriage Misdiagnosis Review [ 30 ], recall bias may be present. Although less is known about paternal recall, previous studies on reproductive events have demonstrated that maternal recall has acceptably high reliability and is little affected by time from the event [ 54 ]. Many participants who took part in this study were of White Irish ethnicity. A more diverse sample in terms of ethnicity and socioeconomic background may have provided broader insight into the experience of RM care. As noted earlier, further work is also needed to engage men in this type of research and to elicit their views and experiences. As the survey was self-selecting, findings cannot be generalised to the Irish population. Most participants were older, of a higher socioeconomic status and well-educated, with private health insurance. Data on miscarriage is not routinely recorded in Ireland; however, cohort studies show that women with recurrent miscarriage tend to be older (aged ≥ 35 years) [ 55 , 56 ]; age is a key demographic risk factor for miscarriage [ 1 ]. Our use of voluntary response sampling introduces some biases in the sample as some people are inherently more likely to volunteer than others, and our sample is not representative of the population under study. For example, negative bias can influence motivation to complete a task, women with negative experiences may be over-represented [ 57 , 58 ]. Several variables were re-categorised for the analysis, easy interpretation, and presentation of results [ 59 ]. Each stage of the RM pathway had different sample sizes resulting in wide confidence intervals indicating the data does not provide a precise representation. While using statistical inference is not recommended in non-probability sampling, in this instance the confidence interval/ p -value confronts the sample with a certain probability model, which enabled this analysis to highlight patient centred care items that predict/ influence overall care experience as data is limited in Ireland for RM. Therefore, results should be interpreted with caution.
Nonetheless, the care experience survey was a valuable tool for assessing RM care delivery processes and including women's experiences in quality improvement research [ 33 ]. Addressing an identified research gap, our results highlight patient centred care items that influence overall care experience ratings, and provide a starting point for future work. Building on previous surveys and input from the RE:CURRENT Research Advisory Group in the development, distribution and analysis added substantial strength to this study and has resulted in a tool that could be used/adapted in future research.
This study provides an overview of women's experiences through the RM care pathway and identifies patient-centred care items that shape the overall rating of RM care experience. While overall experience of RM care was poor, areas that could potentially improve the care experience, included information provision, supportive care and communication between healthcare professionals and patients which reiterates the work of others [ 12 , 45 , 50 , 51 ]. To ensure patient-centred care items are achieved, approaches such as RM clinics and graded approaches to providing RM care could be implemented globally to provide collaborative teamwork and a unified, holistic approach to RM care [ 11 ]. Overall, the results provide a better understanding of the drivers shaping care experiences to help inform and improve RM care.
Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information.
Abbreviations
- Recurrent miscarriage
Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, Fisher J, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397(10285):1658–67.
Article CAS PubMed Google Scholar
Hennessy M, Dennehy R, Meaney S, Linehan L, Devane D, Rice R, et al. Clinical practice guidelines for recurrent miscarriage in high-income countries: A systematic review. Reprod Biomed Online. 2021;42(6):1146–71.
Article PubMed Google Scholar
Royal College of Obstetricians and Gynaecologists. New draft guideline outlines best practice for treating recurrent miscarriage and endorses ground breaking model of care for women who have one or more miscarriages; 2021. Available from: https://www.rcog.org.uk/en/news/new-draft-guideline-outlines-best-practice-for-treating-recurrent-miscarriage-and-endorses-ground-breaking-model-of-care-for-women-who-have-one-or-more-miscarriages/ . Accessed 19 Oct 2021.
Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2020;113(3):533–5.
ESHRE Early Pregnancy Guideline Development Group. Guideline on the Management of Recurrent Pregnancy Loss. Version 2. Grimbergen: European Society of Human Reproduction and Embryology; 2017.
Habayeb OM, Konje JC. The one-stop recurrent miscarriage clinic: an evaluation of its effectiveness and outcome. Hum Reprod. 2004;19(12):2952–8.
Van den Berg M, Vissenberg R, Goddijn M. Recurrent miscarriage clinics. Obstet Gynecol Clin North Am. 2014;41(1):145–55.
Royal College of Obstetricians and Gynaecologists. Green-top Guideline Number 17. The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. London: RCOG; 2011.
Roman E. Fetal loss rates and their relation to pregnancy order. J Epidemiol Community Health. 1984;38(1):29–35.
Article CAS PubMed PubMed Central Google Scholar
Van den Berg M, Dancet E, Erlikh T, van der Veen F, Goddijn M, Hajenius P. Patient-centered early pregnancy care: a systematic review of quantitative and qualitative studies on the perspectives of women and their partners. Hum Reprod Update. 2018;24(1):106–18.
Coomarasamy A, Dhillon-Smith RK, Papadopoulou A, Al-Memar M, Brewin J, Abrahams VM, et al. Recurrent miscarriage: evidence to accelerate action. Lancet. 2021;397(10285):1675–82.
Watson J, Simmonds A, La Fontaine M, Fockler ME. Pregnancy and infant loss: a survey of families’ experiences in Ontario Canada. BMC Pregnancy Childbirth. 2019;19(1):129.
Article PubMed PubMed Central Google Scholar
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759–69.
Article Google Scholar
Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. 2013;69(1):4–15.
Frampton SB. Healthcare and the patient experience: harmonizing care and environment. Los Angeles, CA: SAGE Publications; 2012. p. 3–6.
Google Scholar
Berwick DM. What ‘patient-centered’should mean: confessions of an extremist: A seasoned clinician and expert fears the loss of his humanity if he should become a patient. Health Aff. 2009;28(Suppl1):w555–65.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. New Eng J Med. 2013;368(3):201–3.
Land V, Parry R, Seymour J. Communication practices that encourage and constrain shared decision making in health-care encounters: Systematic review of conversation analytic research. Health Expect. 2017;20(6):1228–47.
Meaney S, Corcoran P, Spillane N, O’Donoghue K. Experience of miscarriage: an interpretative phenomenological analysis. BMJ Open. 2017;7(3):e011382.
Jauniaux E, Farquharson RG, Christiansen OB, Exalto N. Evidence-based guidelines for the investigation and medical treatment of recurrent miscarriage. Hum Reprod. 2006;21(9):2216–22.
Webster K, Eadon H, Fishburn S, Kumar G. Ectopic pregnancy and miscarriage: diagnosis and initial management: summary of updated NICE guidance. BMJ. 2019;367.
Grocott A, McSherry W, editors. The patient experience: informing practice through identification of meaningful communication from the patient’s perspective. Healthcare (Basel). 2018;6(1):26.
deMontigny F, Verdon C, Meunier S, Dubeau D. Women’s persistent depressive and perinatal grief symptoms following a miscarriage: the role of childlessness and satisfaction with healthcare services. Arch Women’s Ment Health. 2017;20(5):655–62.
Emond T, de Montigny F, Guillaumie L. Exploring the needs of parents who experience miscarriage in the emergency department: A qualitative study with parents and nurses. J Clin Nurs. 2019;28(9–10):1952–65.
Silverio SA, Easter A, Storey C, Jurković D, Sandall J, on behalf of the PGC. Preliminary findings on the experiences of care for parents who suffered perinatal bereavement during the COVID-19 pandemic. BMC Pregnancy Childbirth. 2021;21(1):840.
Horey D, Boyle FM, Cassidy J, Cassidy PR, Erwich JJHM, Gold KJ, et al. Parents’ experiences of care offered after stillbirth: An international online survey of high and middle-income countries. Birth. 2021;48(3):366–74.
National Care Experience Programme. Findings of the National Maternity Experience Survey 2020. Dublin: National Care Experience Programme; 2020.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
RCOG. New draft guideline outlines best practice for treating recurrent miscarriage. 2021.
Health Service Executive. National Miscarriage Misdiagnosis Review. Dublin: Health Service Executive; 2011.
Health Service Executive. National Women and Infants Health Programme Annual Report 2020 Dublin: Health Service Executive; 2021. Available from: https://www.hse.ie/eng/about/who/acute-hospitals-division/woman-infants/national-reports-on-womens-health/national-women-and-infants-health-programme-annual-report-2020.pdf . Accessed 19 Dec 2022.
Department of Health. Women's Health Taskforce 2019. Available from: https://www.gov.ie/en/campaigns/-womens-health/ . Accessed 19 Dec 2022.
Anhang Price R, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–54.
Gerteis M. Through the patient's eyes: understanding and promoting patient-centered care. San Francisco: Jossey-Bass; 1993.
Loughnan SA, Gautam R, Silverio SA, Boyle FM, Cassidy J, Ellwood D, et al. Multicountry study protocol of COCOON: COntinuing Care in COVID-19 Outbreak global survey of New, expectant, and bereaved parent experiences. BMJ Open. 2022;12(9):e061550.
Hennessy M, Linehan L, Dennehy R, Devane D, Rice R, Meaney S, et al. Developing guideline-based key performance indicators for recurrent miscarriage care: lessons from a multi-stage consensus process with a diverse stakeholder group. Res Involv Engagem. 2022;8(1):18.
Dennehy R, Hennessy M, Meaney S, Matvienko-Sikar K, O’Sullivan-Lago R, UíDhubhgain J, et al. How we define recurrent miscarriage matters: A qualitative exploration of the views of people with professional or lived experience. Health Expect. 2022;25(6):2992–3004.
Qualtrics. Qualtrics Survey Platform 2021. Available from: Accessed 01 Aug 2021.
StataCorp. Stata Statistical Software: Release 13. College Station: StataCorp LP; 2013.
Harlow AF, Zheng A, Nordberg J, Hatch EE, Ransbotham S, Wise LA. A qualitative study of factors influencing male participation in fertility research. Reprod Health. 2020;17(1):1–14.
Law C. Men on the margins? Reflections on recruiting and engaging men in reproduction research. Method Innov. 2019;12(1):2059799119829425.
Koert E, Malling GMH, Sylvest R, Krog M, Kolte A, Schmidt L, et al. Recurrent pregnancy loss: couples’ perspectives on their need for treatment, support and follow up. Hum Reprod. 2019;34(2):291–6.
Harty T, Trench M, Keegan O, O’Donoghue K, Nuzum D. The experiences of men following recurrent miscarriage in an Irish tertiary hospital: A qualitative analysis. Health Expect. 2022;25(3):1048–57.
Due C, Obst K, Riggs DW, Collins C. Australian heterosexual women’s experiences of healthcare provision following a pregnancy loss. Women Birth. 2018;31(4):331–8.
Bailey SL, Boivin J, Cheong YC, Kitson-Reynolds E, Bailey C, Macklon N. Hope for the best …but expect the worst: a qualitative study to explore how women with recurrent miscarriage experience the early waiting period of a new pregnancy. BMJ Open. 2019;9(5):e029354.
Geller PA, Psaros C, Kerns D. Web-based resources for health care providers and women following pregnancy loss. J Obstet Gynecol Neonatal Nurs. 2006;35(4):523–32.
Joseph-Williams N, Edwards A, Elwyn G. Power imbalance prevents shared decision making. BMJ. 2014;348.
Rowlands IJ, Lee C. ‘The silence was deafening’: social and health service support after miscarriage. J Reprod Infant Psychol. 2010;28(3):274–86.
McLean A, Flynn C. ‘It’s not just a pap-smear’: Women speak of their experiences of hospital treatment after miscarriage. Qual Soc Work. 2012;12(6):782–98.
Fockler ME, Ladhani NNN, Watson J, Barrett JF. Pregnancy subsequent to stillbirth: medical and psychosocial aspects of care. Semin Fetal Neonatal Med. 2017;22(3):186–19.
Sejourne N, Callahan S, Chabrol H. Support following miscarriage: what women want. J Reprod Infant Psychol. 2010;28(4):403–11.
Milat AJ, Bauman A, Redman S. Narrative review of models and success factors for scaling up public health interventions. Implement Sci. 2015;10(1):1–11.
WHO. Guide to fostering change to scale up effective health services. World Health Organization; 2013.
Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL. Medical record validation of maternally reported birth characteristics and pregnancy-related events: a report from the Children’s Cancer Group Am. J Epidemiol. 1997;145(1):58–67.
Article CAS Google Scholar
Linehan LA, San Lazaro Campillo I, Hennessy M, Flannery C, O’Donoghue K. Reproductive outcomes following recurrent first-trimester miscarriage: a retrospective cohort study. Hum Reprod Open. 2022;2022(4):hoac045.
Green DM, O’Donoghue K. A review of reproductive outcomes of women with two consecutive miscarriages and no living child. J Obstet Gynaecol. 2019;39(6):816–21.
Vaish A, Grossmann T, Woodward A. Not all emotions are created equal: the negativity bias in social-emotional development. Psychol Bull. 2008;134(3):383.
Cacioppo JT, Cacioppo S, Gollan JK. The negativity bias: Conceptualization, quantification, and individual differences. Behav Brain Sci. 2014;37(3):309–10.
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080.
Download references
Acknowledgements
We thank all those who helped distribute the survey online, including Cork University Maternity Hospital Remembers, INFANT Research Centre, the Pregnancy Loss Research Group, the Miscarriage Association of Ireland, and Féileacáin (Stillbirth and Neonatal Death Association of Ireland). Thank you to all the women and men who took part and shared their experiences with us.
We would like to thank the RE:CURRENT Project Research Advisory Group for their strategic direction, advice, and guidance concerning this research programme. In particular, we thank Orla O’Connell, Con Lucey, and Jennifer Ui Dhubhgain, who piloted, reviewed, reviewed and distributed recruitment materials and the survey.
This work was funded by the Health Research Board (HRB) Ireland (ILP-HSR-2019–011). In addition, author KMS is supported by a HRB Applying Policy into Practice Research Fellowship (HRB-ARPP-A-2018–011). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and affiliations.
Pregnancy Loss Research Group, Department of Obstetrics & Gynaecology, University College Cork, Cork, Ireland
Caragh Flannery, Marita Hennessy, Rebecca Dennehy & Keelin O’Donoghue
INFANT Research Centre, University College Cork, Cork, Ireland
School of Public Health, University College Cork, Cork, Ireland
Karen Matvienko-Sikar
RE:CURRENT Research Advisory Group, Pregnancy Loss Research Group, Department of Obstetrics & Gynaecology, University College Cork, Cork, Ireland
Con Lucey & Jennifer Ui Dhubhgain
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation & methodology: CF, MH, RD, KOD formulated the overarching aims and methods of the study. Investigation: CF, MH controlled the data collection and management. Formal analysis: CF conducted the analysis. Original draft: CF prepared the initial draft. Writing – review & editing: CF, MH, RD, KMS, JUD, CL, KOD with all authors approving the final version of the manuscript.
Corresponding author
Correspondence to Marita Hennessy .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by the Clinical Research Ethics Committee of the Cork Teaching Hospitals, University College Cork (ECM 4 (jj) 09/03/2021 & ECM 3 (jj) 19/10/2021). Participants provided informed consent (electronically) prior to study participation. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
RE:CURRENT Care Experience Survey.
Additional file 2: Table S2.1.
Men’s characteristics. Figure S2.1. Location where the majority of RM investigations were carried out (Men) . Figure S2.2. Attendance at RM care appointments (Men). Table S2.2. Patient-centred care items for investigation, receiving results, treatment/plan of care, and subsequent pregnancy (Men). Figure S2.3. RM care experience (Men) .
Additional file 3: Table S3.1.
Women’s characteristics by overall RM care experience rating. Table S3.2. Care received by women during investigations for RM. Table S3.3. Care received by women when receiving the results of their investigations for RM. Table S3.4. Care received by women when getting their treatment plan for RM . Table S3.5 . Care received by women for a subsequent pregnancy following RM . Table S3.6. Information and support services used by women for RM. Table S3.7. Women’s overall RM care experience rating.
Additional file 4:
Table S4.1. Unadjusted associations for patient-centred care items during investigations by overall care experience rating. Table S4.2. Unadjusted associations for patient-centred care items when receiving results by overall care experience rating. Table S4.3. Unadjusted associations for patient-centred care items for treatment/plan of care by overall care experience rating. Table S4.4. Unadjusted associations for patient-centred care items during subsequent pregnancy care by overall care experience rating.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Flannery, C., Hennessy, M., Dennehy, R. et al. Factors that shape recurrent miscarriage care experiences: findings from a national survey. BMC Health Serv Res 23 , 317 (2023). https://doi.org/10.1186/s12913-023-09347-1
Download citation
Received : 19 December 2022
Accepted : 27 March 2023
Published : 31 March 2023
DOI : https://doi.org/10.1186/s12913-023-09347-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pregnancy loss
- Patient-centred care
- Patient experience
- Care quality
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

This page has been archived and is no longer being updated regularly.
Miscarriage and loss
Losing a pregnancy can affect a woman — and her family — for years, research finds.
By Elizabeth Leis-Newman
June 2012, Vol 43, No. 6
Print version: page 56

The tragedy of miscarriage has traditionally been private, an event grieved largely by the mother, on her own. Health-care professionals advised these women that the sadness would grow less pronounced over time, especially following a successful pregnancy.
But new research suggests that some women may mourn for much longer than expected, even after the birth of a healthy child, although the range and severity of the symptoms may vary. That's also true for men, as new studies have found that men grieve over a miscarriage more than once thought.
"Because it is medically common, the impact of miscarriage is often underestimated," says Janet Jaffe, PhD, a clinical psychologist at the Center for Reproductive Psychology in San Diego and co-author of the 2010 book "Reproductive Trauma: Psychotherapy with Infertility and Pregnancy Loss Clients." "But miscarriage is a traumatic loss, not only of the pregnancy, but of a woman's sense of self and her hopes and dreams of the future. She has lost her ‘reproductive story,' and it needs to be grieved."
A woman who has a miscarriage is at risk for depression and anxiety symptoms in subsequent years, says University of Rochester Medical Center psychiatry professor Emma Robertson Blackmore, PhD. In addition, even after having a healthy child, women who miscarry have a higher risk of postpartum depression, Robertson Blackmore has found. In a paper published in 2011 in the British Journal of Psychiatry , she followed more than 13,000 women for three years post-birth. Of the 2,823 who had miscarriages, about 15 percent experienced clinically significant depression and/or anxiety during and after pregnancies for up to three years.
Mothers may also struggle to manage the needs of a healthy child after a loss. For example, research by Sherryl S. Heller and Charles H. Zeanah looked at mothers who had delivered a child within 19 months after a perinatal loss. When the child was a year old, the researchers assessed the mother-child attachment relationships and found that 45 percent of the infants had disorganized attachments to their mothers ( Infant Mental Health Journal ). A 2001 study also found evidence of disorganized attachment behavior in infants born subsequent to stillbirth ( Journal of Child Psychology and Psychiatry ).
Robertson Blackmore says such findings may mean miscarriages have psychological implications for future children. "This raises the important issue of how and whether previous perinatal loss and associated mood symptoms may alter a child's outcome," she says.
Another common misunderstanding about miscarriage is that a woman will experience less grief if she loses the baby early in her pregnancy. But most researchers have not been able to find an association between the length of gestation and intensity of grief, anxiety or depression ( Research in Nursing & Health ). A woman who has lost her child at 11 weeks may be as distraught as a woman who has lost her child at 20 weeks, says Jaffe's co-author, Martha Diamond, PhD.
"While the medical experience might vary, it depends on the meaning of the pregnancy to that person," Diamond says. "By labeling it a traumatic loss, we validate the experience."
While reproductive technology is a blessing for many expectant parents, it might also increase grief when the pregnancy fails, says Kristen M. Swanson, RN, PhD, dean of the School of Nursing at the University of North Carolina, who has extensively studied miscarriage and early pregnancy loss. She says historically, a woman may have miscarried and never even known she was pregnant. That is much less likely today.
"Take ultrasound — that window into the womb is more common," Swanson says. "We are paying more and more attention to the early phase of pregnancy. [These days,] you can know within hours of conception if you are pregnant. We are much more attentive."
Still, for women who miscarry early, their grief is less socially acceptable than the anguish of someone who miscarries later in their pregnancy, says Jaffe. "With later losses, people can have a funeral or memorial service. When it's an early miscarriage or even a failed IVF cycle, it is often unacknowledged by others, [yet] these are invisible losses that feel disenfranchised and not validated."
For some women, Diamond says, anxiety after a miscarriage can stem from experiencing a seemingly inexplicable trauma. Women will engage in what she calls "retroactive bargaining" in an effort to feel less out of control.
"They will spend enormous amounts of emotional energy trying to explain why it happened," Diamond says. "They often blame themselves, even when it is inaccurate, to help make sense of it. Women may torment themselves with guilt and blame, rewriting the story, so to speak: ‘If I hadn't gone to the grocery store' or ‘If I didn't stay up so late.' It's a way of coping with the loss. I've come to see this as part of the grief process."
Such feelings can be particularly difficult for women who were ambivalent about the pregnancy to begin with. That can create feelings of guilt, Diamond says.
"It's very, very important that clients know that their ambivalence did not cause the loss," she advises. Diamond remembers working with a 16-year-old who miscarried at 12 weeks. "Everyone around her was thrilled and relieved. It took three sessions for her to acknowledge that she was grief-stricken," she says. "Part of her was relieved, but she was already used to the idea. Nobody around her could validate her sadness."
Men and miscarriage
Another myth surrounding miscarriage is that it does not affect men, says Mark Kiselica, PhD, vice provost and interim dean of the School of Education at the College of New Jersey.
In "Helping Men with the Trauma of Miscarriage," published in Psychotherapy: Theory, Research, Practice, Training in 2010, Kiselica and Martha Rinehart, PhD, looked at case studies of men whose partners had lost a baby. They found that the fathers' sadness and grief were largely dismissed by others. Rinehart, who is completing her master's degree in counseling with a focus on marriage and family counseling at the College of New Jersey, became interested in men's reactions to miscarriage when she miscarried nearly 20 years ago. "My father-in-law had a reaction that was really wounding to my husband. It was all the clichés, like, ‘You'll have other children,'" she remembers.
Her father-in-law statement's reflected how miscarriage was seen by an earlier generation as having nothing to do with men, Rinehart says. She and Kiselica found that men may mask their grief over a miscarriage as anger. They recommend that health-care professionals learn how to determine whether a man is suffering from masked depression after a miscarriage, by doing a male-oriented mental status examination or obtaining a Perinatal Grief Scale score for those whose grief seems extreme.
Men also grapple with the physical loss of their wives after a miscarriage, Kiselica and Swanson say. "What I know from my own data, and working with support groups in counseling, is that miscarriage does a number on your sex life," says Swanson, who has conducted support groups for couples who have miscarried. "For men it was, ‘When can I go back to her? I miss her.' For women, it was, ‘If I never have sex again, I'll die a happy woman.'"
Not surprisingly, pregnancy loss among lesbian relationships can be just as devastating, Swanson says. One of her former doctoral students, Danuta M. Wojnar, RN, PhD, an assistant professor and chair at Seattle University, is researching lesbian couples' responses to miscarriage. Wojnar has found that the non-pregnant partner has a similar response to a man following the miscarriage. "The response tends to be, ‘I lost her and I don't know how to get her back,'" Swanson says. Lesbian couples may also face other stressors, she says. For example, they may face a lack of support from those who disapproved of their becoming parents in the first place.
Swanson advises couples consciously separate "sex for fun and sex for function." The first is to enjoy being intimate; the second is with the plan of becoming pregnant.
In addition, couples should be reminded that pregnancy hormones can continue to cause emotional turbulence, Swanson says. "Prior to the menstruation post-miscarriage, there is a physical component to the sadness where it almost feels like the sadness owns you," Swanson says. "After the hormones get resettled, there is a shift and it will start to feel like you own the sadness."
Support systems
Psychologists can help women access support services for miscarriage by encouraging obstetricians and other physicians to refer women to counseling and by acting as advocates to make discussing miscarriage less of a societal taboo. One resource for guiding health professionals was developed by Pamela Geller, PhD, a Drexel University psychology professor and director of the student counseling center, and her colleagues, Christof Daetwyler, MD, and Mark Woodland, MD, in the Drexel University College of Medicine. Their website is called "Psychological and Medical Aspects of Pregnancy Loss" (see "Further resources").
Another way to help women is to guide them to Web-based resources, Geller says. In a 2006 paper in the Journal of Obstetric, Gynecologic, & Neonatal Nursing titled "Web-based Resources for Health Care Providers and Women Following Pregnancy Loss," Geller highlights eight organizations with websites that offer everything from chat rooms to advice on creating memorials for lost children.
In addition to letting a woman choose what she is ready for, the forums can provide anonymity. "Not everyone gravitates to individual psychotherapy," Geller says. "When women go to good websites they can get information when they want it, even if that's at two in the morning."
But whether a woman engages in one-on-one therapy, group sessions or web-based forums, a key component of all communications to couples who miscarry is that they are not alone, says Robertson Blackmore.
"We've had some very touching emails from older women, even women who are now grandmothers," she says. "It's still very relevant and very sad for many women decades after a loss."
Elizabeth Leis-Newman is a writer and editor in Chicago.
Further resources
With funding from the APGO/WHEO (Association of Professors of Gynecology & Obstetrics/Women's Healthcare Education Office) Interdisciplinary Women's Health Competency Award, Pamela Geller, along with two physicians, created a comprehensive website called "Psychological and Medical Aspects of Pregnancy Loss ," available online . Sections include "What You Can Do" and "How To Break Bad News."
Letters to the Editor
- Send us a letter
Women Who Miscarry Have Long-lasting Mental Health Problems

The depression and anxiety experienced by many women after a miscarriage can continue for years, even after the birth of a healthy child, according to a study led by University of Rochester Medical Center researchers and published online today by the British Journal of Psychiatry .
“Our study clearly shows that the birth of a healthy baby does not resolve the mental health problems that many women experience after a miscarriage or stillbirth,” said Emma Robertson Blackmore, Ph.D. , assistant professor of Psychiatry at the Medical Center and the lead researcher. “This finding is important because, when assessing if a women is at risk of antenatal or postnatal depression, previous pregnancy loss is usually not taken into account in the same way as other risk factors such as a family history of depression, stressful life events or a lack of social support.”
“We know that maternal depression can have adverse impacts on children and families,” Robertson Blackmore said. “If we offer targeted support during pregnancy to women who have previously lost a baby, we may be able to improve health outcomes for both the women and their children.”
Pregnancy loss by miscarriage or stillbirth affects more than an estimated one million women in the United States annually. Between 50 and 80 percent of women who experience pregnancy loss become pregnant again.
The researchers studied 13,133 pregnant women in the United Kingdom who were taking part in a long-term study known as the Avon Longitudinal Study of Parents and Children . The women were asked to report the number of previous miscarriages and stillbirths they had experienced. They were assessed for symptoms of depression and anxiety twice during their pregnancy and four times after giving birth, at 8 weeks, 8 months, 21 months and 33 months. The majority of women reported no miscarriages. But 2,823 women, or 21 percent, reported having one or more previous miscarriages, while 108 reported having one previous stillbirth and three women had two previous stillbirths.
“We found no evidence that affective symptoms associated with previous prenatal loss resolve with the birth of a healthy child. Rather, previous prenatal loss showed a persisting prediction of depressive and anxiety symptoms well after what would conventionally be defined as the postnatal period,” the researchers concluded.
Of the women who had one miscarriage or stillbirth before giving birth to a healthy child, for example, almost 13 percent still had symptoms of depression 33 months after the birth. Of those with two previous losses, almost 19 percent had symptoms of depression 33 months after the birth of a healthy child.
Prenatal loss is not routinely considered a risk factor for antenatal or postpartum depression in the same way as, for instance, personal or family history of depression, exposure to stressful life events or lack of social support, according to the study. Routinely assessing loss history would be valuable as a predictor of current and postpartum risk and as a possible marker for intervention, the researcher.
“Given the adverse outcomes of persistent maternal depression on both child and family outcomes, early recognition of symptoms can lead to preventive interventions to reduce the burden of illness, provide coping strategies to reduce anxiety and depression and promote healthy adjustment of the mother, family and child,” the researchers stated.
In addition to Robertson Blackmore, the authors of the study include: Denise Côté-Arsenault , Ph.D. , associate professor at the University of Rochester School of Nursing; Wan Tang, Ph.D ., research assistant professor of Biostatistics, and Thomas G. O’Connor, Ph.D. , professor of Psychiatry, both of the Medical Center; Vivette Glover, Ph.D., professor of Perinatal Psychobiology at the Imperial College School of Medicine, London, United Kingdom; and Jonathan Evans, Ph.D., consultant senior lecturer in Psychiatry, and Jean Golding, Ph.D., emeritus professor of Pediatrics and Perinatal Epidemiology, both of University of Bristol, United Kingdom.
Funds from the National Institute of Mental Health and the Wellcome Trust supported the research.
- mental health

Samantha Putterman, PolitiFact Samantha Putterman, PolitiFact
Leave your feedback
- Copy URL https://www.pbs.org/newshour/politics/fact-checking-warnings-from-democrats-about-project-2025-and-donald-trump
Fact-checking warnings from Democrats about Project 2025 and Donald Trump
This fact check originally appeared on PolitiFact .
Project 2025 has a starring role in this week’s Democratic National Convention.
And it was front and center on Night 1.
WATCH: Hauling large copy of Project 2025, Michigan state Sen. McMorrow speaks at 2024 DNC
“This is Project 2025,” Michigan state Sen. Mallory McMorrow, D-Royal Oak, said as she laid a hardbound copy of the 900-page document on the lectern. “Over the next four nights, you are going to hear a lot about what is in this 900-page document. Why? Because this is the Republican blueprint for a second Trump term.”
Vice President Kamala Harris, the Democratic presidential nominee, has warned Americans about “Trump’s Project 2025” agenda — even though former President Donald Trump doesn’t claim the conservative presidential transition document.
“Donald Trump wants to take our country backward,” Harris said July 23 in Milwaukee. “He and his extreme Project 2025 agenda will weaken the middle class. Like, we know we got to take this seriously, and can you believe they put that thing in writing?”
Minnesota Gov. Tim Walz, Harris’ running mate, has joined in on the talking point.
“Don’t believe (Trump) when he’s playing dumb about this Project 2025. He knows exactly what it’ll do,” Walz said Aug. 9 in Glendale, Arizona.
Trump’s campaign has worked to build distance from the project, which the Heritage Foundation, a conservative think tank, led with contributions from dozens of conservative groups.
Much of the plan calls for extensive executive-branch overhauls and draws on both long-standing conservative principles, such as tax cuts, and more recent culture war issues. It lays out recommendations for disbanding the Commerce and Education departments, eliminating certain climate protections and consolidating more power to the president.
Project 2025 offers a sweeping vision for a Republican-led executive branch, and some of its policies mirror Trump’s 2024 agenda, But Harris and her presidential campaign have at times gone too far in describing what the project calls for and how closely the plans overlap with Trump’s campaign.
PolitiFact researched Harris’ warnings about how the plan would affect reproductive rights, federal entitlement programs and education, just as we did for President Joe Biden’s Project 2025 rhetoric. Here’s what the project does and doesn’t call for, and how it squares with Trump’s positions.
Are Trump and Project 2025 connected?
To distance himself from Project 2025 amid the Democratic attacks, Trump wrote on Truth Social that he “knows nothing” about it and has “no idea” who is in charge of it. (CNN identified at least 140 former advisers from the Trump administration who have been involved.)
The Heritage Foundation sought contributions from more than 100 conservative organizations for its policy vision for the next Republican presidency, which was published in 2023.
Project 2025 is now winding down some of its policy operations, and director Paul Dans, a former Trump administration official, is stepping down, The Washington Post reported July 30. Trump campaign managers Susie Wiles and Chris LaCivita denounced the document.
WATCH: A look at the Project 2025 plan to reshape government and Trump’s links to its authors
However, Project 2025 contributors include a number of high-ranking officials from Trump’s first administration, including former White House adviser Peter Navarro and former Housing and Urban Development Secretary Ben Carson.
A recently released recording of Russell Vought, a Project 2025 author and the former director of Trump’s Office of Management and Budget, showed Vought saying Trump’s “very supportive of what we do.” He said Trump was only distancing himself because Democrats were making a bogeyman out of the document.
Project 2025 wouldn’t ban abortion outright, but would curtail access
The Harris campaign shared a graphic on X that claimed “Trump’s Project 2025 plan for workers” would “go after birth control and ban abortion nationwide.”
The plan doesn’t call to ban abortion nationwide, though its recommendations could curtail some contraceptives and limit abortion access.
What’s known about Trump’s abortion agenda neither lines up with Harris’ description nor Project 2025’s wish list.
Project 2025 says the Department of Health and Human Services Department should “return to being known as the Department of Life by explicitly rejecting the notion that abortion is health care.”
It recommends that the Food and Drug Administration reverse its 2000 approval of mifepristone, the first pill taken in a two-drug regimen for a medication abortion. Medication is the most common form of abortion in the U.S. — accounting for around 63 percent in 2023.
If mifepristone were to remain approved, Project 2025 recommends new rules, such as cutting its use from 10 weeks into pregnancy to seven. It would have to be provided to patients in person — part of the group’s efforts to limit access to the drug by mail. In June, the U.S. Supreme Court rejected a legal challenge to mifepristone’s FDA approval over procedural grounds.
WATCH: Trump’s plans for health care and reproductive rights if he returns to White House The manual also calls for the Justice Department to enforce the 1873 Comstock Act on mifepristone, which bans the mailing of “obscene” materials. Abortion access supporters fear that a strict interpretation of the law could go further to ban mailing the materials used in procedural abortions, such as surgical instruments and equipment.
The plan proposes withholding federal money from states that don’t report to the Centers for Disease Control and Prevention how many abortions take place within their borders. The plan also would prohibit abortion providers, such as Planned Parenthood, from receiving Medicaid funds. It also calls for the Department of Health and Human Services to ensure that the training of medical professionals, including doctors and nurses, omits abortion training.
The document says some forms of emergency contraception — particularly Ella, a pill that can be taken within five days of unprotected sex to prevent pregnancy — should be excluded from no-cost coverage. The Affordable Care Act requires most private health insurers to cover recommended preventive services, which involves a range of birth control methods, including emergency contraception.
Trump has recently said states should decide abortion regulations and that he wouldn’t block access to contraceptives. Trump said during his June 27 debate with Biden that he wouldn’t ban mifepristone after the Supreme Court “approved” it. But the court rejected the lawsuit based on standing, not the case’s merits. He has not weighed in on the Comstock Act or said whether he supports it being used to block abortion medication, or other kinds of abortions.
Project 2025 doesn’t call for cutting Social Security, but proposes some changes to Medicare
“When you read (Project 2025),” Harris told a crowd July 23 in Wisconsin, “you will see, Donald Trump intends to cut Social Security and Medicare.”
The Project 2025 document does not call for Social Security cuts. None of its 10 references to Social Security addresses plans for cutting the program.
Harris also misleads about Trump’s Social Security views.
In his earlier campaigns and before he was a politician, Trump said about a half-dozen times that he’s open to major overhauls of Social Security, including cuts and privatization. More recently, in a March 2024 CNBC interview, Trump said of entitlement programs such as Social Security, “There’s a lot you can do in terms of entitlements, in terms of cutting.” However, he quickly walked that statement back, and his CNBC comment stands at odds with essentially everything else Trump has said during the 2024 presidential campaign.
Trump’s campaign website says that not “a single penny” should be cut from Social Security. We rated Harris’ claim that Trump intends to cut Social Security Mostly False.
Project 2025 does propose changes to Medicare, including making Medicare Advantage, the private insurance offering in Medicare, the “default” enrollment option. Unlike Original Medicare, Medicare Advantage plans have provider networks and can also require prior authorization, meaning that the plan can approve or deny certain services. Original Medicare plans don’t have prior authorization requirements.
The manual also calls for repealing health policies enacted under Biden, such as the Inflation Reduction Act. The law enabled Medicare to negotiate with drugmakers for the first time in history, and recently resulted in an agreement with drug companies to lower the prices of 10 expensive prescriptions for Medicare enrollees.
Trump, however, has said repeatedly during the 2024 presidential campaign that he will not cut Medicare.
Project 2025 would eliminate the Education Department, which Trump supports
The Harris campaign said Project 2025 would “eliminate the U.S. Department of Education” — and that’s accurate. Project 2025 says federal education policy “should be limited and, ultimately, the federal Department of Education should be eliminated.” The plan scales back the federal government’s role in education policy and devolves the functions that remain to other agencies.
Aside from eliminating the department, the project also proposes scrapping the Biden administration’s Title IX revision, which prohibits discrimination based on sexual orientation and gender identity. It also would let states opt out of federal education programs and calls for passing a federal parents’ bill of rights similar to ones passed in some Republican-led state legislatures.
Republicans, including Trump, have pledged to close the department, which gained its status in 1979 within Democratic President Jimmy Carter’s presidential Cabinet.
In one of his Agenda 47 policy videos, Trump promised to close the department and “to send all education work and needs back to the states.” Eliminating the department would have to go through Congress.
What Project 2025, Trump would do on overtime pay
In the graphic, the Harris campaign says Project 2025 allows “employers to stop paying workers for overtime work.”
The plan doesn’t call for banning overtime wages. It recommends changes to some Occupational Safety and Health Administration, or OSHA, regulations and to overtime rules. Some changes, if enacted, could result in some people losing overtime protections, experts told us.
The document proposes that the Labor Department maintain an overtime threshold “that does not punish businesses in lower-cost regions (e.g., the southeast United States).” This threshold is the amount of money executive, administrative or professional employees need to make for an employer to exempt them from overtime pay under the Fair Labor Standards Act.
In 2019, the Trump’s administration finalized a rule that expanded overtime pay eligibility to most salaried workers earning less than about $35,568, which it said made about 1.3 million more workers eligible for overtime pay. The Trump-era threshold is high enough to cover most line workers in lower-cost regions, Project 2025 said.
The Biden administration raised that threshold to $43,888 beginning July 1, and that will rise to $58,656 on Jan. 1, 2025. That would grant overtime eligibility to about 4 million workers, the Labor Department said.
It’s unclear how many workers Project 2025’s proposal to return to the Trump-era overtime threshold in some parts of the country would affect, but experts said some would presumably lose the right to overtime wages.
Other overtime proposals in Project 2025’s plan include allowing some workers to choose to accumulate paid time off instead of overtime pay, or to work more hours in one week and fewer in the next, rather than receive overtime.
Trump’s past with overtime pay is complicated. In 2016, the Obama administration said it would raise the overtime to salaried workers earning less than $47,476 a year, about double the exemption level set in 2004 of $23,660 a year.
But when a judge blocked the Obama rule, the Trump administration didn’t challenge the court ruling. Instead it set its own overtime threshold, which raised the amount, but by less than Obama.
Support Provided By: Learn more
Educate your inbox
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.

Advertisement
Republicans Gain Edge as Voters Worry About Economy, Times/Siena Poll Finds
With elections next month, independents, especially women, are swinging to the G.O.P. despite Democrats’ focus on abortion rights. Disapproval of President Biden seems to be hurting his party.
- Share full article

By Shane Goldmacher
- Oct. 17, 2022
Republicans enter the final weeks of the contest for control of Congress with a narrow but distinct advantage as the economy and inflation have surged as the dominant concerns, giving the party momentum to take back power from Democrats in next month’s midterm elections, a New York Times/Siena College poll has found.
The poll shows that 49 percent of likely voters said they planned to vote for a Republican to represent them in Congress on Nov. 8, compared with 45 percent who planned to vote for a Democrat. The result represents an improvement for Republicans since September, when Democrats held a one-point edge among likely voters in the last Times/Siena poll. (The October poll’s unrounded margin is closer to three points, not the four points that the rounded figures imply.)
With inflation unrelenting and the stock market steadily on the decline, the share of likely voters who said economic concerns were the most important issues facing America has leaped since July , to 44 percent from 36 percent — far higher than any other issue. And voters most concerned with the economy favored Republicans overwhelmingly, by more than a two-to-one margin.
Which party’s candidate are you more likely to vote for in this year’s election for Congress?

Likely voters
65 and older
BY RACE/ETHNICITY
BY EDUCATION
Bachelor’s
degree or higher
No bachelor’s
Don’t know/refused to answer

Democratic candidate
Republican candidate
18 to 29 years old
Bachelor’s degree
No bachelor’s degree
Both Democrats and Republicans have largely coalesced behind their own party’s congressional candidates. But the poll showed that Republicans opened up a 10-percentage point lead among crucial independent voters, compared with a three-point edge for Democrats in September, as undecided voters moved toward Republicans.
The biggest shift came from women who identified as independent voters. In September, they favored Democrats by 14 points. Now, independent women backed Republicans by 18 points — a striking swing given the polarization of the American electorate and how intensely Democrats have focused on that group and on the threat Republicans pose to abortion rights.
4 Takeaways From the Campaign Trail

With elections less than a month away, our reporters are across the country following candidates. Scandal roiled the Los Angeles City Council, Mitch McConnell affirmed his support for Herschel Walker, and Senate and governor candidates in Nevada sought endorsements.
Here’s a look at the week in political news →
Los Angeles was rocked by news that three City Council members took part in a secretly recorded conversation involving racist comments . Faced with swirling public condemnation, including from President Biden, the Council president, Nury Martinez, resigned, while the other two officials have so far stayed put.
In the critical swing state of Nevada, the Democratic Senate incumbent, Catherine Cortez Masto, received an endorsement from 14 family members of her Republican opponent, Adam Laxalt. In the governor’s race, the state’s largest teachers’ union announced that it wouldn’t endorse either candidate.
Polling in Georgia found less support among female, Black and independent voters for Herschel Walker, the Republican Senate candidate. He trails Senator Raphael Warnock, but by just three points, within the margin of error. Senator Mitch McConnell said he’d “stick with Walker,” an anti-abortion candidate who has been accused of paying for an abortion.
Two Democratic groups said they would pour millions of dollars into local races in a half dozen states before the midterms in hopes of winning back legislatures. The groups, the States Project and the National Democratic Redistricting Committee, are particularly focused on protecting voting and abortion rights .
Catch up on more political news.

We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rom J Morphol Embryol
- v.61(1); Jan-Mar 2020

A research on abortion: ethics, legislation and socio-medical outcomes. Case study: Romania
Andreea mihaela niţă.
1 Faculty of Social Sciences, University of Craiova, Romania
Cristina Ilie Goga
This article presents a research study on abortion from a theoretical and empirical point of view. The theoretical part is based on the method of social documents analysis, and presents a complex perspective on abortion, highlighting items of medical, ethical, moral, religious, social, economic and legal elements. The empirical part presents the results of a sociological survey, based on the opinion survey method through the application of the enquiry technique, conducted in Romania, on a sample of 1260 women. The purpose of the survey is to identify Romanians perception on the decision to voluntary interrupt pregnancy, and to determine the core reasons in carrying out an abortion.
The analysis of abortion by means of medical and social documents
Abortion means a pregnancy interruption “before the fetus is viable” [ 1 ] or “before the fetus is able to live independently in the extrauterine environment, usually before the 20 th week of pregnancy” [ 2 ]. “Clinical miscarriage is both a common and distressing complication of early pregnancy with many etiological factors like genetic factors, immune factors, infection factors but also psychological factors” [ 3 ]. Induced abortion is a practice found in all countries, but the decision to interrupt the pregnancy involves a multitude of aspects of medical, ethical, moral, religious, social, economic, and legal order.
In a more simplistic manner, Winston Nagan has classified opinions which have as central element “abortion”, in two major categories: the opinion that the priority element is represented by fetus and his entitlement to life and the second opinion, which focuses around women’s rights [ 4 ].
From the medical point of view, since ancient times there have been four moments, generally accepted, which determine the embryo’s life: ( i ) conception; ( ii ) period of formation; ( iii ) detection moment of fetal movement; ( iv ) time of birth [ 5 ]. Contemporary medicine found the following moments in the evolution of intrauterine fetal: “ 1 . At 18 days of pregnancy, the fetal heartbeat can be perceived and it starts running the circulatory system; 2 . At 5 weeks, they become more clear: the nose, cheeks and fingers of the fetus; 3 . At 6 weeks, they start to function: the nervous system, stomach, kidneys and liver of the fetus, and its skeleton is clearly distinguished; 4 . At 7 weeks (50 days), brain waves are felt. The fetus has all the internal and external organs definitively outlined. 5 . At 10 weeks (70 days), the unborn child has all the features clearly defined as a child after birth (9 months); 6 . At 12 weeks (92 days, 3 months), the fetus has all organs definitely shaped, managing to move, lacking only the breath” [ 6 ]. Even if most of the laws that allow abortion consider the period up to 12 weeks acceptable for such an intervention, according to the above-mentioned steps, there can be defined different moments, which can represent the beginning of life. Nowadays, “abortion is one of the most common gynecological experiences and perhaps the majority of women will undergo an abortion in their lifetimes” [ 7 ]. “Safe abortions carry few health risks, but « every year, close to 20 million women risk their lives and health by undergoing unsafe abortions » and 25% will face a complication with permanent consequences” [ 8 , 9 ].
From the ethical point of view, most of the times, the interruption of pregnancy is on the border between woman’s right over her own body and the child’s (fetus) entitlement to life. Judith Jarvis Thomson supported the supremacy of woman’s right over her own body as a premise of freedom, arguing that we cannot force a person to bear in her womb and give birth to an unwanted child, if for different circumstances, she does not want to do this [ 10 ]. To support his position, the author uses an imaginary experiment, that of a violinist to which we are connected for nine months, in order to save his life. However, Thomson debates the problem of the differentiation between the fetus and the human being, by carrying out a debate on the timing which makes this difference (period of conception, 10 weeks of pregnancy, etc.) and highlighting that for people who support abortion, the fetus is not an alive human being [ 10 ].
Carol Gilligan noted that women undergo a true “moral dilemma”, a “moral conflict” with regards to voluntary interruption of pregnancy, such a decision often takes into account the human relationships, the possibility of not hurting the others, the responsibility towards others [ 11 ]. Gilligan applied qualitative interviews to a number of 29 women from different social classes, which were put in a position to decide whether or not to commit abortion. The interview focused on the woman’s choice, on alternative options, on individuals and existing conflicts. The conclusion was that the central moral issue was the conflict between the self (the pregnant woman) and others who may be hurt as a result of the potential pregnancy [ 12 ].
From the religious point of view, abortion is unacceptable for all religions and a small number of abortions can be seen in deeply religious societies and families. Christianity considers the beginning of human life from conception, and abortion is considered to be a form of homicide [ 13 ]. For Christians, “at the same time, abortion is giving up their faith”, riot and murder, which means that by an abortion we attack Jesus Christ himself and God [ 14 ]. Islam does not approve abortion, relying on the sacral life belief as specified in Chapter 6, Verse 151 of the Koran: “Do not kill a soul which Allah has made sacred (inviolable)” [ 15 ]. Buddhism considers abortion as a negative act, but nevertheless supports for medical reasons [ 16 ]. Judaism disapproves abortion, Tanah considering it to be a mortal sin. Hinduism considers abortion as a crime and also the greatest sin [ 17 ].
From the socio-economic point of view, the decision to carry out an abortion is many times determined by the relations within the social, family or financial frame. Moreover, studies have been conducted, which have linked the legalization of abortions and the decrease of the crime rate: “legalized abortion may lead to reduced crime either through reductions in cohort sizes or through lower per capita offending rates for affected cohorts” [ 18 ].
Legal regulation on abortion establishes conditions of the abortion in every state. In Europe and America, only in the XVIIth century abortion was incriminated and was considered an insignificant misdemeanor or a felony, depending on when was happening. Due to the large number of illegal abortions and deaths, two centuries later, many states have changed legislation within the meaning of legalizing voluntary interruption of pregnancy [ 6 ]. In contemporary society, international organizations like the United Nations or the European Union consider sexual and reproductive rights as fundamental rights [ 19 , 20 ], and promotes the acceptance of abortion as part of those rights. However, not all states have developed permissive legislation in the field of voluntary interruption of pregnancy.
Currently, at national level were established four categories of legislation on pregnancy interruption area:
( i ) Prohibitive legislations , ones that do not allow abortion, most often outlining exceptions in abortion in cases where the pregnant woman’s life is endangered. In some countries, there is a prohibition of abortion in all circumstances, however, resorting to an abortion in the case of an imminent threat to the mother’s life. Same regulation is also found in some countries where abortion is allowed in cases like rape, incest, fetal problems, etc. In this category are 66 states, with 25.5% of world population [ 21 ].
( ii ) Restrictive legislation that allow abortion in cases of health preservation . Loosely, the term “health” should be interpreted according to the World Health Organization (WHO) definition as: “health is a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity” [ 22 ]. This type of legislation is adopted in 59 states populated by 13.8% of the world population [ 21 ].
( iii ) Legislation allowing abortion on a socio-economic motivation . This category includes items such as the woman’s age or ability to care for a child, fetal problems, cases of rape or incest, etc. In this category are 13 countries, where we have 21.3% of the world population [ 21 ].
( iv ) Legislation which do not impose restrictions on abortion . In the case of this legislation, abortion is permitted for any reason up to 12 weeks of pregnancy, with some exceptions (Romania – 14 weeks, Slovenia – 10 weeks, Sweden – 18 weeks), the interruption of pregnancy after this period has some restrictions. This type of legislation is adopted in 61 countries with 39.5% of the world population [21].
The Centre for Reproductive Rights has carried out from 1998 a map of the world’s states, based on the legislation typology of each country (Figure (Figure1 1 ).

The analysis of states according to the legislation regarding abortion. Source: Centre for Reproductive Rights. The World’s Abortion Laws, 2018 [ 23 ]
An unplanned pregnancy, socio-economic context or various medical problems [ 24 ], lead many times to the decision of interrupting pregnancy, regardless the legislative restrictions. In the study “Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008” issued in 2011 by the WHO , it was determined that within the states with restrictive legislation on abortion, we may also encounter a large number of illegal abortions. The illegal abortions may also be resulting in an increased risk of woman’s health and life considering that most of the times inappropriate techniques are being used, the hygienic conditions are precarious and the medical treatments are incorrectly administered [ 25 ]. Although abortions done according to medical guidelines carry very low risk of complications, 1–3 unsafe abortions contribute substantially to maternal morbidity and death worldwide [ 26 ].
WHO has estimated for the year 2008, the fact that worldwide women between the ages of 15 and 44 years carried out 21.6 million “unsafe” abortions, which involved a high degree of risk and were distributed as follows: 0.4 million in the developed regions and a number of 21.2 million in the states in course of development [ 25 ].
Case study: Romania
Legal perspective on abortion
In Romania, abortion was brought under regulation by the first Criminal Code of the United Principalities, from 1864.
The Criminal Code from 1864, provided the abortion infringement in Article 246, on which was regulated as follows: “Any person, who, using means such as food, drinks, pills or any other means, which will consciously help a pregnant woman to commit abortion, will be punished to a minimum reclusion (three years).
The woman who by herself shall use the means of abortion, or would accept to use means of abortion which were shown or given to her for this purpose, will be punished with imprisonment from six months to two years, if the result would be an abortion. In a situation where abortion was carried out on an illegitimate baby by his mother, the punishment will be imprisonment from six months to one year.
Doctors, surgeons, health officers, pharmacists (apothecary) and midwives who will indicate, will give or will facilitate these means, shall be punished with reclusion of at least four years, if the abortion took place. If abortion will cause the death of the mother, the punishment will be much austere of four years” (Art. 246) [ 27 ].
The Criminal Code from 1864, reissued in 1912, amended in part the Article 246 for the purposes of eliminating the abortion of an illegitimate baby case. Furthermore, it was no longer specified the minimum of four years of reclusion, in case of abortion carried out with the help of the medical staff, leaving the punishment to the discretion of the Court (Art. 246) [ 28 ].
The Criminal Code from 1936 regulated abortion in the Articles 482–485. Abortion was defined as an interruption of the normal course of pregnancy, being punished as follows:
“ 1 . When the crime is committed without the consent of the pregnant woman, the punishment was reformatory imprisonment from 2 to 5 years. If it caused the pregnant woman any health injury or a serious infirmity, the punishment was reformatory imprisonment from 3 to 6 years, and if it has caused her death, reformatory imprisonment from 7 to 10 years;
2 . When the crime was committed by the unmarried pregnant woman by herself, or when she agreed that someone else should provoke the abortion, the punishment is reformatory imprisonment from 3 to 6 months, and if the woman is married, the punishment is reformatory imprisonment from 6 months to one year. Same penalty applies also to the person who commits the crime with the woman’s consent. If abortion was committed for the purpose of obtaining a benefit, the punishment increases with another 2 years of reformatory imprisonment.
If it caused the pregnant woman any health injuries or a severe disablement, the punishment will be reformatory imprisonment from one to 3 years, and if it has caused her death, the punishment is reformatory imprisonment from 3 to 5 years” (Art. 482) [ 29 ].
The criminal legislation from 1936 specifies that it is not considered as an abortion the interruption from the normal course of pregnancy, if it was carried out by a doctor “when woman’s life was in imminent danger or when the pregnancy aggravates a woman’s disease, putting her life in danger, which could not be removed by other means and it is obvious that the intervention wasn’t performed with another purpose than that of saving the woman’s life” and “when one of the parents has reached a permanent alienation and it is certain that the child will bear serious mental flaws” (Art. 484, Par. 1 and Par. 2) [ 29 ].
In the event of an imminent danger, the doctor was obliged to notify prosecutor’s office in writing, within 48 hours after the intervention, on the performance of the abortion. “In the other cases, the doctor was able to intervene only with the authorization of the prosecutor’s office, given on the basis of a medical certificate from hospital or a notice given as a result of a consultation between the doctor who will intervene and at least a professor doctor in the disease which caused the intervention. General’s Office Prosecutor, in all cases provided by this Article, shall be obliged to maintain the confidentiality of all communications or authorizations, up to the intercession of any possible complaints” (Art. 484) [ 29 ].
The legislation of 1936 provided a reformatory injunction from one to three years for the abortions committed by doctors, sanitary agents, pharmacists, apothecary or midwives (Art. 485) [ 29 ].
Abortion on demand has been legalized for the first time in Romania in the year 1957 by the Decree No. 463, under the condition that it had to be carried out in a hospital and to be carried out in the first quarter of the pregnancy [ 30 ]. In the year 1966, demographic policy of Romania has dramatically changed by introducing the Decree No. 770 from September 29 th , which prohibited abortion. Thus, the voluntary interruption of pregnancy became a crime, with certain exceptions, namely: endangering the mother’s life, physical or mental serious disability; serious or heritable illness, mother’s age over 45 years, if the pregnancy was a result of rape or incest or if the woman gave birth to at least four children who were still in her care (Art. 2) [ 31 ].
In the Criminal Code from 1968, the abortion crime was governed by Articles 185–188.
The Article 185, “the illegal induced abortion”, stipulated that “the interruption of pregnancy by any means, outside the conditions permitted by law, with the consent of the pregnant woman will be punished with imprisonment from one to 3 years”. The act referred to above, without the prior consent from the pregnant woman, was punished with prison from two to five years. If the abortion carried out with the consent of the pregnant woman caused any serious body injury, the punishment was imprisonment from two to five years, and when it caused the death of the woman, the prison sentence was from five to 10 years. When abortion was carried out without the prior consent of the woman, if it caused her a serious physical injury, the punishment was imprisonment from three to six years, and if it caused the woman’s death, the punishment was imprisonment from seven to 12 years (Art. 185) [ 32 ].
“When abortion was carried out in order to obtain a material benefit, the maximum punishment was increased by two years, and if the abortion was made by a doctor, in addition to the prison punishment could also be applied the prohibition to no longer practice the profession of doctor”.
Article 186, “abortion caused by the woman”, stipulated that “the interruption of the pregnancy course, committed by the pregnant woman, was punished with imprisonment from 6 months to 2 years”, quoting the fact that by the same punishment was also sanctioned “the pregnant woman’s act to consent in interrupting the pregnancy course made out by another person” (Art. 186) [ 26 ].
The Regulations of the Criminal Code in 1968, also provided the crime of “ownership of tools or materials that can cause abortion”, the conditions of this holding being met when these types of instruments were held outside the hospital’s specialized institutions, the infringement shall be punished with imprisonment from three months to one year (Art. 187) [ 32 ].
Furthermore, the doctors who performed an abortion in the event of extreme urgency, without prior legal authorization and if they did not announce the competent authority within the legal deadline, they were punished by imprisonment from one month to three months (Art. 188) [ 32 ].
In the year 1985, it has been issued the Decree No. 411 of December 26 th , by which the conditions imposed by the Decree No. 770 of 1966 have been hardened, meaning that it has increased the number of children, that a woman could have in order to request an abortion, from four to five children [ 33 ].
The Articles 185–188 of the Criminal Code and the Decree No. 770/1966 on the interruption of the pregnancy course have been abrogated by Decree-Law No. 1 from December 26 th , 1989, which was published in the Official Gazette No. 4 of December 27 th , 1989 (Par. 8 and Par. 12) [ 34 ].
The Criminal Code from 1968, reissued in 1997, maintained Article 185 about “the illegal induced abortion”, but drastically modified. Thus, in this case of the Criminal Code, we identify abortion as “the interruption of pregnancy course, by any means, committed in any of the following circumstances: ( a ) outside medical institutions or authorized medical practices for this purpose; ( b ) by a person who does not have the capacity of specialized doctor; ( c ) if age pregnancy has exceeded 14 weeks”, the punishment laid down was the imprisonment from 6 months to 3 years” (Art. 185, Par. 1) [ 35 ]. For the abortion committed without the prior consent of the pregnant woman, the punishment consisted in strict prison conditions from two to seven years and with the prohibition of certain rights (Art. 185, Par. 2) [ 35 ].
For the situation of causing serious physical injury to the pregnant woman, the punishment was strict prison from three to 10 years and the removal of certain rights, and if it had as a result the death of the pregnant woman, the punishment was strict prison from five to 15 years and the prohibition of certain rights (Art. 185, Par. 3) [ 35 ].
The attempt was punished for the crimes specified in the various cases of abortion.
Consideration should also be given in the Criminal Code reissued in 1997 for not punishing the interruption of the pregnancy course carried out by the doctor, if this interruption “was necessary to save the life, health or the physical integrity of the pregnant woman from a grave and imminent danger and that it could not be removed otherwise; in the case of a over fourteen weeks pregnancy, when the interruption of the pregnancy course should take place from therapeutic reasons” and even in a situation of a woman’s lack of consent, when it has not been given the opportunity to express her will, and abortion “was imposed by therapeutic reasons” (Art. 185, Par. 4) [ 35 ].
Criminal Code from 2004 covers abortion in Article 190, defined in the same way as in the prior Criminal Code, with the difference that it affects the limits of the punishment. So, in the event of pregnancy interruption, in accordance with the conditions specified in Paragraph 1, “the penalty provided was prison time from 6 months to one year or days-fine” (Art. 190, Par. 1) [ 36 ].
Nowadays, in Romania, abortion is governed by the criminal law of 2009, which entered into force in 2014, by the section called “aggression against an unborn child”. It should be specified that current criminal law does not punish the woman responsible for carrying out abortion, but only the person who is involved in carrying out the abortion. There is no punishment for the pregnant woman who injures her fetus during pregnancy.
In Article 201, we can find the details on the pregnancy interruption infringement. Thus, the pregnancy interruption can be performed in one of the following circumstances: “outside of medical institutions or medical practices authorized for this purpose; by a person who does not have the capacity of specialist doctor in Obstetrics and Gynecology and the right of free medical practice in this specialty; if gestational age has exceeded 14 weeks”, the punishment is the imprisonment for six months to three years, or fine and the prohibition to exercise certain rights (Art. 201, Par. 1) [ 37 ].
Article 201, Paragraph 2 specifies that “the interruption of the pregnancy committed under any circumstances, without the prior consent of the pregnant woman, can be punished with imprisonment from 2 to 7 years and with the prohibition to exercise some rights” (Art. 201, Par. 1) [ 37 ].
If by facts referred to above (Art. 201, Par. 1 and Par. 2) [ 37 ] “it has caused the pregnant woman’s physical injury, the punishment is the imprisonment from 3 to 10 years and the prohibition to exercise some rights, and if it has had as a result the pregnant woman’s death, the punishment is the imprisonment from 6 to 12 years and the prohibition to exercise some rights” (Art. 201, Par. 3) [ 37 ]. When the facts have been committed by a doctor, “in addition to the imprisonment punishment, it will also be applied the prohibition to exercise the profession of doctor (Art. 201, Par. 4) [ 37 ].
Criminal legislation specifies that “the interruption of pregnancy does not constitute an infringement with the purpose of a treatment carried out by a specialist doctor in Obstetrics and Gynecology, until the pregnancy age of twenty-four weeks is reached, or the subsequent pregnancy interruption, for the purpose of treatment, is in the interests of the mother or the fetus” (Art. 201, Par. 6) [ 37 ]. However, it can all be found in the phrases “therapeutic purposes” and “the interest of the mother and of the unborn child”, which predisposes the text of law to an interpretation, finally the doctors are the only ones in the position to decide what should be done in such cases, assuming direct responsibility [ 38 ].
Article 202 of the Criminal Code defines the crime of harming an unborn child, pointing out the punishments for the various types of injuries that can occur during pregnancy or in the childbirth period and which can be caused by the mother or by the persons who assist the birth, with the specification that the mother who harms her fetus during pregnancy is not punished and does not constitute an infringement if the injury has been committed during pregnancy or during childbirth period if the facts have been “committed by a doctor or by an authorized person to assist the birth or to follow the pregnancy, if they have been committed in the course of the medical act, complying with the specific provisions of his profession and have been made in the interest of the pregnant woman or fetus, as a result of the exercise of an inherent risk in the medical act” (Art. 202, Par. 6) [ 37 ].
The fact situation in Romania
During the period 1948–1955, called “the small baby boom” [ 39 ], Romania registered an average fertility rate of 3.23 children for a woman. Between 1955 and 1962, the fertility rate has been less than three children for a woman, and in 1962, fertility has reached an average of two children for a woman. This phenomenon occurred because of the Decree No. 463/1957 on liberalization of abortion. After the liberalization from 1957, the abortion rate has increased from 220 abortions per 100 born-alive children in the year 1960, to 400 abortions per 100 born-alive children, in the year 1965 [ 40 ].
The application of provisions of Decrees No. 770 of 1966 and No. 411 of 1985 has led to an increase of the birth rate in the first three years (an average of 3.7 children in 1967, and 3.6 children in 1968), followed by a regression until 1989, when it was recorded an average of 2.2 children, but also a maternal death rate caused by illegal abortions, raising up to 85 deaths of 100 000 births in the year of 1965, and 170 deaths in 1983. It was estimated that more than 80% of maternal deaths between 1980–1989 was caused by legal constraints [ 30 ].
After the Romanian Revolution in December 1989 and after the communism fall, with the abrogation of Articles 185–188 of the Criminal Code and of the Decree No. 770/1966, by the Decree of Law No. 1 of December 26 th , 1989, abortion has become legal in Romania and so, in the following years, it has reached the highest rate of abortion in Europe. Subsequently, the number of abortion has dropped gradually, with increasing use of birth control [ 41 ].
Statistical data issued by the Ministry of Health and by the National Institute of Statistics (INS) in Romania show corresponding figures to a legally carried out abortion. The abortion number is much higher, if it would take into account the number of illegal abortion, especially those carried out before 1989, and those carried out in private clinics, after the year 1990. Summing the declared abortions in the period 1958–2014, it is to be noted the number of them, 22 037 747 exceeds the current Romanian population. A detailed statistical research of abortion rate, in terms of years we have exposed in Table Table1 1 .
The number of abortions declared in Romania in the period 1958–2016
|
|
|
|
|
|
|
|
|
|
|
| 1958 | 112 100 | 1970 | 292 410 | 1982 | 468 041 | 1994 | 530 191 | 2006 | 150 246 |
| 1959 | 578 000 | 1971 | 330 000 | 1983 | – | 1995 | 502 840 | 2007 | 137 226 |
| 1960 | 774 000 | 1972 | 381 000 | 1984 | 303 123 | 1996 | 456 221 | 2008 | 137 226 |
| 1961 | 865 000 | 1973 | 376 000 | 1985 | 302 838 | 1997 | 347 126 | 2009 | 115 457 |
| 1962 | 967 000 | 1974 | 335 000 | 1986 | 183 959 | 1998 | 271 496 | 2010 | 101 915 |
| 1963 | 1 037 000 | 1975 | 359 417 | 1987 | 182 442 | 1999 | 259 888 | 2011 | 101 915 |
| 1964 | 1 100 000 | 1976 | 383 000 | 1988 | 185 416 | 2000 | 257 865 | 2012 | 88 135 |
| 1965 | 1 115 000 | 1977 | 379 000 | 1989 | 193 084 | 2001 | 254 855 | 2013 | 86 432 |
| 1966 | 973 000 | 1978 | 394 000 | 1990 | 992 265 | 2002 | 247 608 | 2014 | 78 371 |
| 1967 | 206 000 | 1979 | 404 000 | 1991 | 866 934 | 2003 | 224 807 | 2015 | 70 447 |
| 1968 | 220 000 | 1980 | 413 093 | 1992 | 691 863 | 2004 | 191 038 | 2016 | 63 085 |
| 1969 | 258 000 | 1981 | – | 1993 | 585 761 | 2005 | 163 459 |
|
|
Source: Pro Vita Association (Bucharest, Romania), National Institute of Statistics (INS – Romania), EUROSTAT [ 42 , 43 , 44 ]
Data issued by the United Nations International Children’s Emergency Fund (UNICEF) in June 2016, for the period 1989–2014, in matters of reproductive behavior, indicates a fertility rate for Romania with a continuous decrease, in proportion to the decrease of the number of births, but also a lower number of abortion rate reported to 100 deliveries (Table (Table2 2 ).
Reproductive behavior in Romania in 1989–2014
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Total fertility rate (births per woman) | 2.2 | 1.8 | 1.6 | 1.5 | 1.4 | 1.4 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.2 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.4 | 1.3 | 1.0 | 1.36 | 1.40 | 1.44 |
| Live births (1000s) | 369.5 | 314.7 | 275.3 | 260.4 | 250.0 | 246.7 | 236.6 | 231.3 | 236.9 | 237.3 | 234.6 | 234.5 | 220.4 | 210.5 | 212.5 | 216.3 | 221.0 | 219.5 | 214.7 | 221.9 | 222.4 | 212.2 | 196.2 | 201.1 | 182.3 | 183.7 |
| Abortion rate (legally induced abortions per 100 live births) | – | 315.3 | 314.9 | 265.7 | 234.3 | 214.9 | 212.5 | 197.2 | 146.5 | 114.4 | 110.8 | 110.0 | 115.6 | 117.6 | 105.8 | 88.3 | 73.9 | 68.5 | 63.9 | 57.6 | 52.2 | 48.0 | 52.7 | 43.7 | 47.2 | 42.7 |
Source: United Nations International Children’s Emergency Fund (UNICEF), Transformative Monitoring for Enhanced Equity (TransMonEE) Data. Country profiles: Romania, 1989–2015 [ 45 ].
By analyzing data issued for the period 1990–2015 by the International Organization of Health , UNICEF , United Nations Fund for Population Activity (UNFPA), The World Bank and the United Nations Population Division, it is noticed that maternal mortality rate has currently dropped as compared with 1990 (Table (Table3 3 ).
Maternal mortality estimation in Romania in 1990–2015
|
|
|
|
|
|
| 2015 | 31 [22–44] | 56 | 179 | 1.1 |
| 2010 | 30 [26–35] | 61 | 202 | 1.2 |
| 2005 | 33 [28–38] | 71 | 217 | 1.1 |
| 2000 | 51 [44–58] | 110 | 222 | 1.5 |
| 1995 | 77 [66–88] | 180 | 241 | 2.1 |
| 1990 | 124 [108–141] | 390 | 318 | 5.2 |
Source: World Health Organization (WHO), Global Health Observatory Data. Maternal mortality country profiles: Romania, 2015 [ 46 ].
Opinion survey: women’s opinion on abortion
Argument for choosing the research theme
Although the problematic on abortion in Romania has been extensively investigated and debated, it has not been carried out in an ample sociological study, covering Romanian women’s perception on abortion. We have assumed making a study at national level, in order to identify the opinion on abortion, on the motivation to carry out an abortion, and to identify the correlation between religious convictions and the attitude toward abortion.
Examining the literature field of study
In the conceptual register of the research, we have highlighted items, such as the specialized literature, legislation, statistical documents.
Formulation of hypotheses and objectives
The first hypothesis was that Romanian women accept abortion, having an open attitude towards this act. Thus, the first objective of the research was to identify Romanian women’s attitude towards abortion.
The second hypothesis, from which we started, was that high religious beliefs generate a lower tolerance towards abortion. Thus, the second objective of our research has been to identify the correlation between the religious beliefs and the attitude towards abortion.
The third hypothesis of the survey was that, the main motivation in carrying out an abortion is the fact that a woman does not want a baby, and the main motivation for keeping the pregnancy is that the person wants a baby. In this context, the third objective of the research was to identify main motivation in carrying out an abortion and in maintaining a pregnancy.
Another hypothesis was that modern Romanian legislation on the abortion is considered fair. Based on this hypothesis, we have assumed the fourth objective, which is to identify the degree of satisfaction towards the current regulatory provisions governing the abortion.
Research methodology
The research method is that of a sociological survey by the application of the questionnaire technique. We used the sampling by age and residence looking at representative numbers of population from more developed as well as underdeveloped areas.
Determination of the sample to be studied
Because abortion is a typical women’s experience, we have chosen to make the quantitative research only among women. We have constructed the sample by selecting a number of 1260 women between the ages of 15 and 44 years (the most frequently encountered age among women who give birth to a child). We also used the quota sampling techniques, taking into account the following variables: age group and the residence (urban/rural), so that the persons included in the sample could retain characteristic of the general population.
By the sample of 1260 women, we have made a percentage of investigation of 0.03% of the total population.
The Questionnaires number applied was distributed as follows (Table (Table4 4 ).
The sampling rates based on the age, and the region of residence
|
|
|
|
|
|
|
|
| |
| Women in North-West | Urban | 37 898 | 58 839 | 50 527 | 54 944 | 53 962 | 60 321 | 316 491 |
| Rural | 36 033 | 37 667 | 36 515 | 41 837 | 43 597 | 42 877 | 238 526 | |
| Sample in North-West | Urban | 11 | 18 | 15 | 17 | 16 | 18 | 95 |
| Rural | 11 | 11 | 11 | 13 | 13 | 13 | 72 | |
| Women in the Center | Urban | 32 661 | 46 697 | 46 713 | 54 031 | 52 590 | 59 084 | 291 776 |
| Rural | 29 052 | 31 767 | 29 562 | 34 402 | 35 334 | 35 502 | 195 619 | |
| Sample in the Center | Urban | 10 | 14 | 14 | 16 | 16 | 18 | 88 |
| Rural | 9 | 9 | 9 | 10 | 11 | 11 | 59 | |
| Women in North-East | Urban | 38 243 | 50 228 | 45 924 | 51 818 | 49 959 | 63 157 | 299 329 |
| Rural | 63 466 | 51 814 | 47 524 | 60 495 | 67 009 | 65 717 | 356 025 | |
| Sample in North-East | Urban | 11 | 15 | 14 | 16 | 15 | 19 | 90 |
| Rural | 19 | 16 | 14 | 18 | 20 | 20 | 107 | |
| Women in South-East | Urban | 31 556 | 40 879 | 43 317 | 53 461 | 53 756 | 67 135 | 290 104 |
| Rural | 34 494 | 32 446 | 29 987 | 37 828 | 41 068 | 42 836 | 218 659 | |
| Sample in South-East | Urban | 10 | 12 | 13 | 16 | 16 | 20 | 87 |
| Rural | 10 | 10 | 9 | 11 | 12 | 13 | 65 | |
| Women in South Muntenia | Urban | 30 480 | 38 066 | 40 049 | 47 820 | 49 272 | 64 739 | 270 426 |
| Rural | 52 771 | 55 286 | 49 106 | 60 496 | 67 660 | 74 401 | 359 720 | |
| Sample in South Muntenia | Urban | 9 | 11 | 12 | 14 | 15 | 19 | 80 |
| Rural | 16 | 17 | 15 | 18 | 20 | 22 | 108 | |
| Women in Bucharest–Ilfov | Urban | 41 314 | 83 927 | 90 607 | 102 972 | 86 833 | 98 630 | 504 283 |
| Rural | 5385 | 7448 | 7952 | 9997 | 9400 | 10 096 | 50 278 | |
| Sample in Bucharest–Ilfov | Urban | 12 | 25 | 27 | 31 | 26 | 30 | 151 |
| Rural | 2 | 2 | 2 | 3 | 3 | 3 | 15 | |
| Women in South-West Oltenia | Urban | 26 342 | 31 155 | 33 493 | 39 064 | 39 615 | 50 516 | 220 185 |
| Rural | 31 223 | 29 355 | 26 191 | 32 946 | 36 832 | 40 351 | 196 898 | |
| Sample in South-West Oltenia | Urban | 8 | 9 | 10 | 12 | 12 | 15 | 66 |
| Rural | 9 | 9 | 8 | 10 | 11 | 12 | 59 | |
| Women in West | Urban | 30 258 | 45 687 | 39 583 | 44 808 | 44 834 | 54 155 | 259 325 |
| Rural | 19 205 | 20 761 | 19 351 | 22 788 | 24 333 | 26 792 | 133 230 | |
| Sample in West | Urban | 9 | 14 | 12 | 13 | 14 | 16 | 78 |
| Rural | 6 | 6 | 6 | 7 | 7 | 8 | 40 | |
| Total women | 540 381 | 662 022 | 636 401 | 749 707 | 756 054 | 856 309 | 4 200 874 | |
| Total sample | 162 | 198 | 191 | 225 | 227 | 257 | 1260 | |
Source: Sample built, based on the population data issued by the National Institute of Statistics (INS – Romania) based on population census conducted in 2011 [ 47 ].
Data collection
Data collection was carried out by questionnaires administered by 32 field operators between May 1 st –May 31 st , 2018.
The analysis of the research results
In the next section, we will present the main results of the quantitative research carried out at national level.
Almost three-quarters of women included in the sample agree with carrying out an abortion in certain circumstances (70%) and only 24% have chosen to support the answer “ No, never ”. In modern contemporary society, abortion is the first solution of women for which a pregnancy is not desired. Even if advanced medical techniques are a lot safer, an abortion still carries a health risk. However, 6% of respondents agree with carrying out abortion regardless of circumstances (Table (Table5 5 ).
Opinion on the possibility of carrying out an abortion
|
| |
|
|
|
| Yes, under certain circumstances | 70% |
| No, never | 24% |
| Yes, regardless the situation | 6% |
| Total | 100% |
Although abortions carried out after 14 weeks are illegal, except for medical reasons, more than half of the surveyed women stated they would agree with abortion in certain circumstances. At the opposite pole, 31% have mentioned they would never agree on abortions after 14 weeks. Five percent were totally accepting the idea of abortion made to a pregnancy that has exceeded 14 weeks (Table (Table6 6 ).
Opinion on the possibility of carrying out an abortion after the period of 14 weeks of pregnancy
|
| |
|
|
|
| Yes, under certain circumstances | 64% |
| No, never | 31% |
| Yes, regardless the situation | 5% |
| Total | 100% |
For 53% of respondents, abortion is considered a crime as well as the right of a women. On the other hand, 28% of the women considered abortion as a crime and 16% associate abortion with a woman’s right (Table (Table7 7 ).
Opinion on abortion: at the border between crime and a woman’s right
|
| |
|
|
|
| A crime and a woman’s right | 53% |
| A crime | 28% |
| A woman’s right | 16% |
| I don’t know | 2% |
| I don’t answer | 1% |
| Total | 100% |
Opinions on what women abort at the time of the voluntary pregnancy interruption are split in two: 59% consider that it depends on the time of the abortion, and more specifically on the pregnancy development stage, 24% consider that regardless of the period in which it is carried out, women abort a child, and 14% have opted a fetus (Table (Table8 8 ).
Abortion of a child vs. abortion of a fetus
|
| |
|
|
|
| Both, depending on the moment when the abortion takes place | 59% |
| A child | 24% |
| A fetus | 14% |
| I don’t answer | 3% |
| Total | 100% |
Among respondents who consider that women abort a child or a fetus related to the time of abortion, 37.5% have considered that the difference between a baby and a fetus appears after 14 weeks of pregnancy (the period legally accepted for abortion). Thirty-three percent of them have mentioned that the distinction should be performed at the first few heartbeats; 18.1% think it is about when the child has all the features definitively outlined and can move by himself; 2.8% consider that the difference appears when the first encephalopathy traces are being felt and the child has formed all internal and external organs. A percentage of 1.7% of respondents consider that this difference occurs at the beginning of the central nervous system, and 1.4% when the unborn child has all the features that we can clearly see to a newborn child (Table (Table9 9 ).
The opinion on the moment that makes the difference between a fetus and a child
|
| |
|
|
|
| Over 14 weeks (the period legally accepted for abortion) | 37.5% |
| From the very first heart beat (18 days) | 33.3% |
| When the child has all organs contoured and can move by himself (12 weeks) | 18.1% |
| When the first encephalon traces are being felt and the child has formed all internal and external organs (seven weeks) | 2.8% |
| At the beginning of the central nervous system, liver, kidneys, stomach (six weeks) | 1.7% |
| When the unborn child has all the characteristics that we can clearly observe to a child after birth | 1.4% |
| When you can clearly distinguish his features (nose, cheeks, eyes) (five weeks) | 1.2% |
| Other | 1% |
| I don’t know | 3% |
| Total | 100% |
We noticed that highly religious people make a clear association between abortion and crime. They also consider that at the time of pregnancy interruption it is aborted a child and not a fetus. However, unexpectedly, we noticed that 27% of the women, who declare themselves to be very religious, have also stated that they see abortion as a crime but also as a woman’s right. Thirty-one percent of the women, who also claimed profound religious beliefs, consider that abortion may be associated with the abortion of a child but also of a fetus, this depending on the time of abortion (Tables (Tables10 10 and and11 11 ).
The correlation between the level of religious beliefs and the perspective on abortion seen as a crime or a right
|
| |||||||
|
|
|
| |||||
| A woman’s right | A crime | Both depending on the moment when it took place | Not know | No | |||
| Are you a religious person? | A very religious and practicant person | 1% | 11% | 12% | – | – | 24% |
| A very religious but non practicant person | 4% | 7% | 15% | – | 1% | 27% | |
| A relatively religious and practicant person | 5% | 6% | 13% | – | – | 24% | |
| Relatively religious but non practicant person | 6% | 4% | 13% | 2% | – | 25% | |
| Total | 16% | 28% | 53% | 2% | 1% | 100% | |
The correlation between the level of religious beliefs and the perspective on abortion procedure conducted on a fetus or a child
|
| ||||||
|
|
|
| ||||
| A fetus | A child | Both depending on the time of abortion | Not know | |||
| Are you a religious person? | A very religious and practicant person | 2% | 8% | 14% | – | 24% |
| A very religious but non practicant person | 3% | 7% | 17% | – | 27% | |
| A relatively religious and practicant person | 4% | 5% | 16% | 3% | 28% | |
| Relatively religious but non practicant person | 5% | 4% | 12% | 3% | 24% | |
| Total | 14% | 24% | 59% | 6% | 100% | |
More than half of the respondents have opted for the main reason for abortion the appearance of medical problems to the child. Baby’s health represents the main concern of future mothers, and of each parent, and the birth of a child with serious health issues, is a factor which frightens any future parent, being many times, at least theoretically, one good reason for opting for abortion. At the opposite side, 12% of respondents would not choose abortion under any circumstances. Other reasons for which women would opt for an abortion are: if the woman would have a medical problem (22%) or would not want the child (10%) (Table (Table12 12 ).
Potential reasons for carrying out an abortion
|
| |
|
|
|
| If the child would have a medical problem (genetic or developmental abnormalities of fetus) | 55% |
| If I would have a medical problem | 22% |
| In any of these situations, I would abort | 12% |
| If the child would not be desired | 10% |
| I don’t know | 1% |
| Total | 100% |
Most of the women want to give birth to a child, 56% of the respondents, representing also the reason that would determine them to keep the child. Morality (26%), faith (10%) or legal restrictions (4%), are the three other reasons for which women would not interrupt a pregnancy. Only 2% of the respondents have mentioned other reasons such as health or age.
A percentage of 23% of the surveyed people said that they have done an abortion so far, and 77% did not opted for a surgical intervention either because there was no need, or because they have kept the pregnancy (Table (Table13 13 ).
Rate of abortion among women in the sample
|
| |
|
|
|
| No | 77% |
| Yes | 23% |
| Total | 100% |
Most respondents, 87% specified that they have carried out an abortion during the first 14 weeks – legally accepted limit for abortion: 43.6% have made abortion in the first four weeks, 39.1% between weeks 4–8, and 4.3% between weeks 8–14. It should be noted that 8.7% could not appreciate the pregnancy period in which they carried out abortion, by opting to answer with the option “ I don’t know ”, and a percentage of 4.3% refused to answer to this question.
Performing an abortion is based on many reasons, but the fact that the women have not wanted a child is the main reason mentioned by 47.8% of people surveyed, who have done minimum an abortion so far. Among the reasons for the interruption of pregnancy, it is also included: women with medical problems (13.3%), not the right time to be a mother (10.7%), age motivation (8.7%), due to medical problems of the child (4.3%), the lack of money (4.3%), family pressure (4.3%), partner/spouse did not wanted. A percentage of 3.3% of women had different reasons for abortion, as follows: age difference too large between children, career, marital status, etc. Asked later whether they regretted the abortion, a rate of 69.6% of women who said they had at least one abortion regret it (34.8% opted for “ Yes ”, and 34.8% said “ Yes, partially ”). 26.1% of surveyed women do not regret the choice to interrupted the pregnancy, and 4.3% chose to not answer this question. We noted that, for women who have already experienced abortion, the causes were more diverse than the grounds on which the previous question was asked: “What are the reasons that determined you to have an abortion?” (Table (Table14 14 ).
The reasons that led the women in the sample to have an abortion
|
| |
|
|
|
| I did not desired the child | 47.8% |
| Because of my medical problems | 13.3% |
| It was not the right time | 10.7% |
| I was too young | 8.7% |
| Because the child had health problems (genetic or developmental abnormalities of fetus) | 4.3% |
| Because I did not have financial resources (I couldn’t afford raising a child) | 4.3% |
| Because of the pressure of my family | 4.3% |
| The partner/husband did not wanted | 4.3% |
| Other reasons | 3.3% |
| Total | 100% |
The majority of the respondents (37.5%) considered that “nervous depression” is the main consequence of abortion, followed by “insomnia and nightmares” (24.6%), “disorders in alimentation” and “affective disorders” (each for 7.7% of respondents), “deterioration of interpersonal relationships” and “the feeling of guilt”(for 6.3% of the respondents), “sexual disorders” and “panic attacks” (for 6.3% of the respondents) (Table (Table15 15 ).
Opinion on the consequences of abortion
|
| |
|
|
|
| Nervous depression | 37.5% |
| Insomnia and nightmares | 24.6% |
| Disorders in alimentation | 7.7% |
| Affective disorders | 7.7% |
| Deterioration of interpersonal relationships | 6.3% |
| The feeling of guilt | 6.3% |
| Sexual disorders | 3.3% |
| Panic attacks | 3.3% |
| Other reasons | 3.3% |
| Total | 100% |
Over half of the respondents believe that abortion should be legal in certain circumstances, as currently provided by law, 39% say it should be always legal, and only 6% opted for the illegal option (Table (Table16 16 ).
Opinion on the legal regulation of abortion
|
| |
|
|
|
| Legal in certain terms | 53% |
| Always legal | 39% |
| Illegal | 6% |
| I don’t know | 2% |
| Total | 100% |
Although the current legislation does not punish pregnant women who interrupt pregnancy or intentionally injured their fetus, survey results indicate that 61% of women surveyed believe that the national law should punish the woman and only 28% agree with the current legislation (Table (Table17 17 ).
Opinion on the possibility of punishing the woman who interrupts the course of pregnancy or injures the fetus
|
| |
|
|
|
| Yes | 61% |
| No | 28% |
| I don’t know | 7% |
| I don’t answer | 4% |
| Total | 100% |
For the majority of the respondents (40.6%), the penalty provided by the current legislation, the imprisonment between six months and three years or a fine and deprivation of certain rights for the illegal abortion is considered fair, for a percentage of 39.6% the punishment is too small for 9.5% of the respondents is too high. Imprisonment between two and seven years and deprivation of certain rights for an abortion performed without the consent of the pregnant woman is considered too small for 65% of interviewees. Fourteen percent of them think it is fair and only 19% of respondents consider that Romanian legislation is too severe with people who commit such an act considering the punishment as too much. The imprisonment from three to 10 years and deprivation of certain rights for the facts described above, if an injury was caused to the woman, is considered to be too small for more than half of those included in the survey, 64% and almost 22% for nearly a quarter of them. Only 9% of the respondents mentioned that this legislative measure is too severe for such actions (Table (Table18 18 ).
Opinion on the regulation of abortion of the Romanian Criminal Code (Art. 201)
|
|
|
|
|
|
|
|
| |
| Reasonable | 40.6% | 14% | 22% |
| Too small | 39.6% | 65% | 64% |
| Too big | 9.5% | 19% | 9% |
| I don’t know | 6.6% | 2% | 3% |
| I don’t answer | 3.7% | – | 2% |
| Total | 100% | 100% | 100% |
Conclusions
After analyzing the results of the sociological research regarding abortion undertaken at national level, we see that 76% of the Romanian women accept abortion, indicating that the majority accepts only certain circumstances (a certain period after conception, for medical reasons, etc.). A percentage of 64% of the respondents indicated that they accept the idea of abortion after 14 weeks of pregnancy (for solid reasons or regardless the reason). This study shows that over 50% of Romanian women see abortion as a right of women but also a woman’s crime and believe that in the moment of interruption of a pregnancy, a fetus is aborted. Mostly, the association of abortion with crime and with the idea that a child is aborted is frequently found within very religious people. The main motivation for Romanian women in taking the decision not to perform an abortion is that they would want the child, and the main reason to perform an abortion is the child’s medical problems. However, it is noted that, in real situations, in which women have already done at least one abortion, most women resort to abortion because they did not want the child towards the hypothetical situation in which women felt that the main reason of abortion is a medical problem. Regarding the satisfaction with the current national legislation of the abortion, the situation is rather surprising. A significant percentage (61%) of respondents felt as necessary to punish the woman who performs an illegal abortion, although the legislation does not provide a punishment. On the other hand, satisfaction level to the penalties provided by law for various violations of the legal conditions for conducting abortion is low, on average only 25.5% of respondents are being satisfied with these, the majority (average 56.2%) considering the penalties as unsatisfactory. Understood as a social phenomenon, intensified by human vulnerabilities, of which the most obvious is accepting the comfort [ 48 ], abortion today is no longer, in Romanian society, from a legal or religious perspective, a problem. Perceptions on the legislative sanction, moral and religious will perpetual vary depending on beliefs, environment, education, etc. The only and the biggest social problem of Romania is truly represented by the steadily falling birth rate.
Conflict of interests
The authors declare that they have no conflict of interests.

COMMENTS
This paper is the first of three in this Series on miscarriage in which we present the current knowledge, recommendations, need for further research, and a call to action on priorities. We discuss the epidemiology of sporadic and recurrent miscarriage, and present a literature review of the risk factors and consequences of miscarriage on future ...
Miscarriage is generally defined as the loss of a pregnancy before viability. An estimated 23 million miscarriages occur every year worldwide, translating to 44 pregnancy losses each minute. The pooled risk of miscarriage is 15·3% (95% CI 12·5-18·7%) of all recognised pregnancies. The population pre …
A new Series of 3 papers published in The Lancet reviews this evidence on miscarriage and challenges many misconceptions. The authors, Siobhan Quenby, Arri Coomarasamy, and colleagues, call for a complete rethink of the narrative around miscarriage and a comprehensive overhaul of medical care and advice offered to women who have miscarriages.
The odds of miscarriage are 10.28 times in mothers with the age of 40 years or older as compared to younger mothers (AOR=10.28; p-value=0.001) after adjusting all other independent variables. Secondly, women who are overweight or obese are more likely to have a miscarriage than mothers with normal BMI (AOR=3.01; p-value=0.001).
Introduction and background. Spontaneous miscarriage is the loss of a pregnancy prior to 20 weeks of gestation, which is the most common complication of pregnancy [ 1 ]. Spontaneous miscarriages occur in about 20% of pregnancies in the United States [ 2 ]. Women experiencing miscarriage may be treated in a multitude of places: prenatal clinics ...
Therefore we propose the need for high quality research into an association between the experience of stress in a variety of contexts and miscarriage risk. In the present meta-analysis, on sub analysis, six studies with higher quality showed a significantly increased miscarriage risk in women suffering from psychological stress, but this was ...
Abstract. Abstract: The ESHRE defined recurrent miscarriage (RM) as ≥3 consecutive pregnancy losses before 22 weeks` gestation. Five to fifteen percent of RM women have significantly elevated ...
Strengths and limitations of this study. This study uses interpretative phenomenological analysis in order to interpret the experience of miscarriage. Much of the research in relation to pregnancy loss is focused on women's experience. Purposive sampling was undertaken to ensure that both women's and men's experiences were included in this study.
Background Spontaneous miscarriage is the most common complication of pregnancy, occurring in up to 20% of pregnancies. Despite the prevalence of miscarriage, little is known regarding peoples' awareness and understanding of causes of pregnancy loss. The aim of this study was to explore university students' understanding of rates, causes and risk factors of miscarriage. Methods A cross ...
The risk of miscarriage is much higher in women with previous losses. The risk of miscarriage after two consecutive losses is between 17-25%, and the risk of miscarriage after three consecutive losses is between 25-46% [2,5]. Figure1: The outcome of conception; 60% preclinical miscarriage, 10% clinical miscarriage,
miscarriage is the primary focus of this paper. Symptoms that a woman may experience that indicate an inevitable, or unavoidable, miscarriage are bleeding, cramping, absence of the usual signs of pregnancy, absence of fetal heartbeat, and absence of fetal tissue on sonogram (Limbo, Glasser, & Sundaram, 2014).
Epidemiology of sporadic and recurrent miscarriage. Human reproduction is characterized by its inefficiency. Prospective cohort studies using sensitive and specific daily urinary hCG assays in women trying to conceive have demonstrated that only around one-third of conceptions progress to a live birth [34-36].An estimated 30% of human conceptions are lost prior to implantation and a further 30 ...
This paper is the first of three in this Series on miscarriage in which we present the current knowledge, recommendations, need for further research, and a call to action on priorities. We discuss the epidemiology of sporadic and recurrent miscarriage, and present a literature review of the risk factors and consequences of miscarriage on future ...
The terms women and men are used throughout the paper, but participants were asked to identify themselves as 'Mother/I carried the pregnancy' or 'Father/partner' in the survey. ... As ten years were chosen to reflect the research and investment in miscarriage services in Ireland since 2010 following the Miscarriage Misdiagnosis Review ...
The women described their experience of miscarriage and perceptions of what helped or hindered their emotional recovery, particularly physicians' actions. A grief reaction that can be divided into ...
A new Series of 3 papers published in The Lancet reviews this evidence on miscarriage and challenges many misconceptions. The authors, Siobhan Quenby, Arri Coomarasamy, and colleagues, call for a complete rethink of the narrative around miscarriage and a comprehensive overhaul of medical care and advice offered to women who have miscarriages.
The tragedy of miscarriage has traditionally been private, an event grieved largely by the mother, on her own. Health-care professionals advised these women that the sadness would grow less pronounced over time, especially following a successful pregnancy. But new research suggests that some women may mourn for much longer than expected, even ...
A miscarriage is the spontaneous demise of a pregnancy in utero before the fetus reaches viability. ... Consideration should also be given to both the financial and research implications of including large numbers of low-risk couples with an overall good prognosis for future pregnancies, in a group subjected to investigations and treatments for ...
We estimated an average annual miscarriage rate of 11.3%. In our final sample ( n = 79,978 women), the fully-adjusted model indicated that use of infertility drugs was associated with a 4 percentage point higher risk of miscarriage (95% CI 0.02, 0.06) and a past suicide attempt with a 3 percentage point higher risk (95% CI -0.002, 0.07).
This paper is a research-based description of what it is like to miscarry. The investigator suggests an empirically tested theory of caring for women who have miscarried. Conclusions are derived from a 15-year program of interpretive, descriptive, and experimental research. A clinical case study of one woman who miscarried illustrates both the ...
The depression and anxiety experienced by many women after a miscarriage can continue for years, even after the birth of a healthy child, according to a study led by University of Rochester Medical Center researchers and published online today by the British Journal of Psychiatry. "Our study clearly shows that the birth of a healthy baby does not resolve the mental health problems that many ...
Project 2025 wouldn't ban abortion outright, but would curtail access The Harris campaign shared a graphic on X that claimed "Trump's Project 2025 plan for workers" would "go after birth ...
Furthermore, the emotional impact of miscarriage is frequently underestimated, and it can be difficult for women and partners to find acknowledgment from friends, family, or health care providers (HCPs). 6 Importantly, research has shown that women frequently experience significant psychological distress, trauma, and grief as a result of ...
With elections next month, independents, especially women, are swinging to the G.O.P. despite Democrats' focus on abortion rights. Disapproval of President Biden seems to be hurting his party.
Abstract. This article presents a research study on abortion from a theoretical and empirical point of view. The theoretical part is based on the method of social documents analysis, and presents a complex perspective on abortion, highlighting items of medical, ethical, moral, religious, social, economic and legal elements.