Information
- Author Services

Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Current advances in the management of diabetes mellitus.

1. Introduction
3. risk factors of diabetes, 4. management of diabetes, 4.1. internet intervention for lifestyle modification in diabetes, 4.2. nanotechnology and diabetes, 4.3. medical nutrition therapy in diabetes, 4.4. gene therapy and diabetes mellitus, 4.5. stem cell therapy in diabetes, 4.6. latest inventions in diabetes management, 4.6.1. drugs recently introduced, 4.6.2. drugs in the pipeline, 5. discussion of major findings, 6. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Giovannini, P.; Howes, M.J.R.; Edwards, S.E. Medicinal plants used in the traditional management of diabetes and its sequelae in Central America: A review. J. Ethnopharmacol. 2016 , 184 , 58–71. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- International Diabetes Federation. Data from: IFD Diabetes Altas Globally. IDF Diabetes Atlas, 8th ed, 2017. Available online: https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf (accessed on 11 May 2022).
- WHO. Global Report on Diabetes ; WHO: Geneva, Switzerland, 2016; Available online: http://www.who.int/diabetes/global-report/en/ (accessed on 11 May 2022).
- Wu, Y.; Ding, Y.; Tanaka, Y.; Zhang, W. Risk Factors Contributing to Type 2 Diabetes and Recent Advances in the Treatment and Prevention. Int. J. Med. Sci. 2014 , 11 , 1185–1200. [ Google Scholar ] [ CrossRef ]
- Group, T.D.P. Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999. Diabet. Med. 2006 , 23 , 857–866. [ Google Scholar ] [ CrossRef ]
- Rask-Madsen, C.; King, G.L. Vascular complications of diabetes: Mechanisms of injury and protective factors. Cell Metab. 2013 , 17 , 20–33. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The effect of Intensive Treatment of diabetes on the development and progression of ling-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993 , 329 , 977–986. [ Google Scholar ] [ PubMed ]
- Callejas, D.; Mann, C.J.; Ayuso, E.; Lage, R.; Grifoll, I.; Roca, C.; Andaluz, A.; Ruiz-de Gopegui, R.; Montané, J.; Muñoz, S.; et al. Treatment of diabetes and long-term survival after insulin and glucokinase gene therapy. Diabetes 2013 , 62 , 1718–1729. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Palmer, S.C.; Mavridis, D.; Nicolucci, A.; Johnson, D.W.; Tonelli, M.; Craig, J.C.; Maggo, J.; Gray, V.; De Berardis, G.; Ruospo, M.; et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes a meta-analysis. J. Am. Med. Assoc. 2016 , 316 , 313–324. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Defronzo, R.; Fleming, G.A.; Chen, K.; Bicsak, T.A. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metab. Clin. Exp. 2016 , 65 , 20–29. [ Google Scholar ] [ CrossRef ]
- Banting, F.G.; Best, C.H. Pancreatic extracts. J. Lab. Clin. Med. 1990 , 115 , 254–272. [ Google Scholar ] [ PubMed ]
- Control, T.D.; Trial, C. Hypoglycemia in the diabetes control and complications trial. Diabetes 1997 , 46 , 271–286. [ Google Scholar ] [ CrossRef ]
- Group, T.D.R. Weight gain associated with intensive therapy in the diabetes control and complications trial. Diabetes Care 1988 , 11 , 567–573. [ Google Scholar ] [ CrossRef ]
- Meek, T.H.; Morton, G.J. The role of leptin in diabetes: Metabolic effects. Diabetologia 2016 , 59 , 928–932. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Noh, J.-W.; Jung, J.H.; Park, J.E.; Lee, J.H.; Sim, K.H.; Park, J.; Kim, M.H.; Yoo, K.-B. The relationship between age of onset and risk factors including family history and life style in Korean population with type 2 diabetes mellitus. J. Phys. Ther. Sci. 2018 , 30 , 201–206. [ Google Scholar ] [ CrossRef ]
- Asiimwe, D.; Mauti, G.O.; Kiconco, R. Prevalence and Risk Factors Associated with Type 2 Diabetes in Elderly Patients Aged 45–80 Years at Kanungu District. J. Diabetes Res. 2020 , 2020 , 5152146. [ Google Scholar ] [ CrossRef ]
- Mordarska, K.; Godziejewska-Zawada, M. Diabetes in the elderly. Prz. Menopauzalny 2017 , 16 , 38–43. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ye, J. Mechanisms of insulin resistance in obesity. Front. Med. China 2013 , 7 , 14–24. [ Google Scholar ] [ CrossRef ]
- FDA. Cigarette Smoking: A Risk Factor for Type 2 Diabetes. 2020. Available online: https://www.fda.gov/tobacco-products/health-effects-tobacco-use/cigarette-smoking-risk-factor-type-2-diabetes (accessed on 20 July 2022).
- Herman, W.H.; Ye, W.; Griffin, S.J.; Simmons, R.K.; Davies, M.J.; Khunti, K.; Rutten, G.E.H.M.; Sandbaek, A.; Lauritzen, T.; Borch-Johnsen, K.; et al. Early detection and treatment of type 2 diabetes reduce cardiovascular morbidity and mortality: A simulation of the results of the Anglo-Danish-Dutch study of intensive treatment in people with screen-detected diabetes in primary care (ADDITION-Europe). Diabetes Care 2015 , 38 , 1449–1455. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Franz, M.J. Lifestyle modifications for diabetes management. Endocrinol. Metab. Clin. North Am. 1997 , 26 , 499–510. [ Google Scholar ] [ CrossRef ]
- Chong, S.; Ding, D.; Byun, R.; Comino, E.; Bauman, A.; Jalaludin, B. Lifestyle changes after a diagnosis of type 2 diabetes. Diabetes Spectr. 2017 , 30 , 43–50. [ Google Scholar ] [ CrossRef ]
- Cotter, A.P.; Durant, N.; Agne, A.A.; Cherrington, A.L. Internet interventions to support lifestyle modification for diabetes management: A systematic review of the evidence. J. Diabetes Its Complicat. 2014 , 28 , 243–251. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Veiseh, O.; Tang, B.C.; Whitehead, K.A.; Anderson, D.G.; Langer, R. Managing diabetes with nanomedicine: Challenges and opportunities. Nat. Rev. Drug Discov. 2014 , 14 , 45–57. [ Google Scholar ] [ CrossRef ]
- Disanto, R.M.; Subramanian, V.; Gu, Z. Recent advances in nanotechnology for diabetes treatment. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015 , 7 , 548–564. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lemmerman, L.R.; Das, D.; Higuita-Castro, N.; Mirmira, R.G.; Gallego-Perez, D. Nanomedicine-Based Strategies for Diabetes: Diagnostics, Monitoring, and Treatment. Trends Endocrinol. Metab. 2020 , 31 , 448–458. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Weir, G.C.; Bonner-Weir, S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes 2004 , 53 (Suppl. 3). [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tamborlane, W.; Beck, R.; Bode, B.; Buckingham, B.; Chase, H.; Clemons, R.; Fiallo-Scharer, R.; Fox, L.; Gilliam, L.; Hirsch, I.; et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N. Engl. J. Med. 2008 , 359 , 1464–1476. [ Google Scholar ] [ CrossRef ]
- Edelman, S.V.; Argento, N.B.; Pettus, J.; Hirsch, I.B. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care 2018 , 41 , 2265–2274. [ Google Scholar ] [ CrossRef ]
- Hovorka, R.; Nodale, M.; Haidar, A.; Wilinska, M.E. Assessing performance of closed-loop insulin delivery systems by continuous glucose monitoring: Drawbacks and way forward. Diabetes Technol. Ther. 2013 , 15 , 4–12. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Scognamiglio, V. Nanotechnology in glucose monitoring: Advances and challenges in the last 10 years. Biosens. Bioelectron. 2013 , 47 , 12–25. [ Google Scholar ] [ CrossRef ]
- Grunberger, G. The need for better insulin therapy. Diabetes Obes. Metab. 2013 , 15 (Suppl. 1), 1–5. [ Google Scholar ] [ CrossRef ]
- Lagopati, N.; Pavlatou, E. Nanotechnology in Diabetes Management. Interv. Obes. Diabetes 2021 , 5 , 419–424. [ Google Scholar ] [ CrossRef ]
- Garber, A.J.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bloomgarden, Z.T.; Bush, M.A.; Dagogo-Jack, S.; DeFronzo, R.A.; Einhorn, D.; Fonseca, V.A.; et al. Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive type 2 diabetes management algorithm—2018 executive summary. Endocr. Pract. 2018 , 24 , 91–120. [ Google Scholar ] [ CrossRef ]
- Viswanathan, V.; Krishnan, D.; Kalra, S.; Chawla, R.; Tiwaskar, M.; Saboo, B.; Baruah, M.; Chowdhury, S.; Makkar, B.M.; Jaggi, S. Insights on Medical Nutrition Therapy for Type 2 Diabetes Mellitus: An Indian Perspective. Adv. Ther. 2019 , 36 , 520–547. [ Google Scholar ] [ CrossRef ]
- Institute of Medicine. Dietary Reference Intakes: Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) ; National Academy Press: Washington, DC, USA, 2005. [ Google Scholar ]
- Moreno-Castilla, C.; Mauricio, D.; Hernandez, M. Role of Medical Nutrition Therapy in the Management of Gestational Diabetes Mellitus. Curr. Diabetes Rep. 2016 , 16 , 22. [ Google Scholar ] [ CrossRef ]
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014 , 383 , 1999–2007. [ Google Scholar ] [ CrossRef ]
- Dunbar, C.E.; High, K.A.; Joung, J.K.; Kohn, D.B.; Ozawa, K.; Sadelain, M. Gene therapy comes of age. Science 2018 , 175. [ Google Scholar ] [ CrossRef ]
- Xu, R.; Li, H.; Lai-yin, T.; Hsiang-fu, K.; Lu, H.; Lam, K. Diabetes Gene Therapy: Potential and Challenges. Curr. Gene Ther. 2003 , 3 , 65–82. [ Google Scholar ] [ CrossRef ]
- Wong, M.S.; Hawthorne, W.J.; Manolios, N. Gene therapy in diabetes. Self/Nonself 2010 , 1 , 165–175. [ Google Scholar ] [ CrossRef ]
- Mali, S. Delivery systems for gene therapy. Indian J. Hum. Genet. 2013 , 19 , 3–8. [ Google Scholar ] [ CrossRef ]
- Kaufmann, K.B.; Büning, H.; Galy, A.; Schambach, A.; Grez, M. Gene therapy on the move. EMBO Mol. Med. 2013 , 5 , 1642–1661. [ Google Scholar ] [ CrossRef ]
- Tsokos, G.C.; Nepom, G.T. Gene therapy in the treatment of autoimmune diseases. J. Clin. Investig. 2000 , 106 , 181–183. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Liu, X.; Zhang, S.; Li, X.; Zheng, P.; Hu, F.; Zhou, Z. Vaccination with a co-expression DNA plasmid containing GAD65 fragment gene and IL-10 gene induces regulatory CD4+ T cells that prevent experimental autoimmune diabetes. Diabetes/Metab. Res. Rev. 2016 , 32 , 522–533. [ Google Scholar ] [ CrossRef ]
- Chellappan, D.K.; Yap, W.S.; Bt Ahmad Suhaimi, N.A.; Gupta, G.; Dua, K. Current therapies and targets for type 2 diabetes mellitus. Panminerva Med. 2018 , 60 , 117–131. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bakay, M.; Pandey, R.; Hakonarson, H. Genes involved in type 1 diabetes: An update. Genes 2013 , 4 , 499–521. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kwak, S.H.; Park, K.S. Recent progress in genetic and epigenetic research on type 2 diabetes. Exp. Mol. Med. 2016 , 48 , e220–e228. [ Google Scholar ] [ CrossRef ]
- Florez, J.C. Pharmacogenetics in type 2 diabetes: Precision medicine or discovery tool? Diabetologia 2017 , 60 , 800–807. [ Google Scholar ] [ CrossRef ]
- Abderrazak, A.; El Hadri, K.; Bosc, E.; Blondeau, B.; Slimane, M.N.; Büchele, B.; Simmet, T.; Couchie, D.; Rouis, M. Inhibition of the inflammasome NLRP3 by arglabin attenuates inflammation, protects pancreatic β-cells from apoptosis, and prevents type 2 diabetes mellitus development in ApoE2Ki mice on a chronic high-fat diet. J. Pharmacol. Exp. Ther. 2016 , 357 , 487–494. [ Google Scholar ] [ CrossRef ]
- Yue, Z.; Zhang, L.; Li, C.; Chen, Y.; Tai, Y.; Shen, Y.; Sun, Z. Advances and potential of gene therapy for type 2 diabetes mellitus. Biotechnol. Biotechnol. Equip. 2019 , 33 , 1150–1157. [ Google Scholar ] [ CrossRef ]
- Mccall, M.D.; Toso, C.; Baetge, E.E.; Shapiro, A.M.J. Are stem cells a cure for diabetes? Clin. Sci. 2009 , 118 , 87–97. [ Google Scholar ] [ CrossRef ]
- Abdulazeez, S.S. Diabetes treatment: A rapid review of the current and future scope of stem cell research. Saudi Pharm. J. 2015 , 23 , 333–340. [ Google Scholar ] [ CrossRef ]
- Bonner-Weir, S.; Baxter, L.A.; Schuppin, G.T.; Smith, F.E. A second pathway for regeneration of adult exocrine and endocrine pancreas: A possible recapitulation of embryonic development. Diabetes 1993 , 42 , 1715–1720. [ Google Scholar ] [ CrossRef ]
- Bonner-Weir, S.; Taneja, M.; Weir, G.C.; Tatarkiewicz, K.; Song, K.H.; Sharma, A.; O’Neil, J.J. In vitro cultivation of human islets from expanded ductal tissue. Proc. Natl. Acad. Sci. USA 2000 , 97 , 7999–8004. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gao, R.; Ustinov, J.; Pulkkinen, M.A.; Lundin, K.; Korsgren, O.; Otonkoski, T. Characterization of endocrine progenitor cells and critical factors for their differentiation in human adult pancreatic cell culture. Diabetes 2003 , 52 , 2007–2015. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brazelton, T.R.; Rossi, F.M.; Keshet, G.I.; Blau, H.M. From Marrow to Brain: Expression of Neuronal Phenotypes in Adult Mice Timothy. Science 2000 , 290 , 1775–1779. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Krause, D.S.; Theise, N.D.; Collector, M.I.; Henegariu, O.; Hwang, S.; Gardner, R.; Neutzel, S.; Sharkis, S.J. Multi-organ, multi-lineage engraftment by a single bone marrow-derived stem cell. Cell 2001 , 105 , 369–377. [ Google Scholar ] [ CrossRef ]
- Jiang, Y.; Jahagirdar, B.N.; Reinhardt, R.L.; Schwartz, R.E.; Keene, C.D.; Ortiz-Gonzalez, X.R.; Reyes, M.; Lenvik, T.; Lund, T.; Blackstad, M.; et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 2002 , 418 , 41–49. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ianus, A.; Holz, G.G.; Theise, N.D.; Hussain, M.A. In vivo derivation of glucose-competent pancreatic endocrine cells from bone marrow without evidence of cell fusion. J. Clin. Investig. 2003 , 111 , 843–850. [ Google Scholar ] [ CrossRef ]
- Hess, D.; Li, L.; Martin, M.; Sakano, S.; Hill, D.; Strutt, B.; Thyssen, S.; Gray, D.A.; Bhatia, M. Bone marrow-derived stem cells initiate pancreatic regeneration. Nat. Biotechnol. 2003 , 21 , 763–770. [ Google Scholar ] [ CrossRef ]
- Couri, C.E.B.; Oliveira, M.C.B.; Stracieri, A.B.P.L.; Moraes, D.A.; Madeira, M.I.A.; Malmegrim, K.C.R.; Simo, B.P.; Foss, M.C.; Burt, R.K. C-Peptide Levels and Insulin Independence Following Autologous Nonmyeloablative Hematopoietic Stem Cell Transplantation in Newly Diagnosed Type 1 Diabetes Mellitus. JAMA 2009 , 301 , 1573–1579. [ Google Scholar ] [ CrossRef ]
- Estrada, E.J.; Valacchi, F.; Nicora, E.; Brieva, S.; Esteve, C.; Echevarria, L.; Froud, T.; Bernetti, K.; Cayetano, S.M.; Velazquez, O.; et al. Combined treatment of intrapancreatic autologous bone marrow stem cells and hyperbaric oxygen in type 2 diabetes mellitus. Cell Transplant. 2008 , 17 , 1295–1304. [ Google Scholar ] [ CrossRef ]
- FDA. FDA Approves Novel, Dual-Targeted Treatment for Type 2 Diabetes. 2022. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-novel-dual-targeted-treatment-type-2-diabetes (accessed on 16 September 2022).
- Bertsch, T. An Introduction to Tirzepatide. Clin. Diabetes 2022 , 40 , 371–372. [ Google Scholar ] [ CrossRef ]
- Kawai, T.; Sun, B.; Yoshino, H.; Feng, D.; Suzuki, Y.; Fukazawa, M.; Nagao, S.; Wainscott, D.B.; Showalter, A.D.; Droz, B.A.; et al. Structural basis for GLP-1 receptor activation by LY3502970, an orally active nonpeptide agonist. Proc. Natl. Acad. Sci. USA 2020 , 117 , 29959–29967. [ Google Scholar ] [ CrossRef ]
- SCOHIA. SCO-094 GLP-1R/GIPR Dual Agonist. 2022. Available online: https://www.scohia.com/eng/sys/pipeline/sco-094/ (accessed on 16 September 2022).
- Piemonti, L.; Keymeulen, B.; Gillard, P.; Linn, T.; Bosi, E.; Rose, L.; Pozzilli, P.; Giorgino, F.; Cossu, E.; Daffonchio, L.; et al. Ladarixin, an inhibitor of the interleukin-8 receptors CXCR1 and CXCR2, in new-onset type 1 diabetes: A multicentre, randomized, double-blind, placebo-controlled trial. Diabetes Obes. Metab. 2022 , 24 , 1840–1849. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zimmet, P.; Alberti, K.; Shaw, J. Global and societal implications of the diabetes epidemic. Nature 2001 , 414 , 782–787. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- American Diabetes Association Task Force for Writing Nutrition Principles and Recommendations for the Management of Diabetes and Related Complications. American Diabetes Association position statement: Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. J. Am. Diet. Assoc. 2002 , 102 , 109–118. [ Google Scholar ] [ CrossRef ]
- Casares, S.; Hurtado, A.; McEvoy, R.C.; Sarukhan, A.; von Boehmer, H.; Brumeanu, T. Down-regulation of diabetogenic CD4+ T cells by a soluble dimeric peptide-MHC class II chimera. Nature Inmmunol. 2002 , 3 , 383–391. [ Google Scholar ] [ CrossRef ]
- Dong, H.; Altomonte, J.; Morral, N.; Meseck, M.; Thung, S.N.; Woo, S.L.C. Basal insulin gene expression significantly improves conventional insulin therapy in type 1 diabetic rats. Diabetes 2002 , 51 , 130–138. [ Google Scholar ] [ CrossRef ]
- Sharma, N.R.; Rao, G.H.R. Diabetes Management: Expectations and Limitations. J. Diabetes Metab. 2016 , 7 , 4. [ Google Scholar ] [ CrossRef ]
- Touchefeu, Y.; Harrington, K.J.; Galmiche, J.P.; Vassaux, G. Review article: Gene therapy, recent developments and future prospects in gastrointestinal oncology. Aliment. Pharmacol. Ther. 2010 , 32 , 953–968. [ Google Scholar ] [ CrossRef ]
- Varga, C.M.; Hong, K.; Lauffenburger, D.A. Quantitative analysis of synthetic gene delivery vector design properties. Mol. Ther. 2001 , 4 , 438–446. [ Google Scholar ] [ CrossRef ]
- Samulski, R.J.; Sally, M.; Muzyczka, N. Adenoassociated viral vectors. In Development of Human Gene Therapy ; Cold Spring Habour Laboratory Press: Cold Spring Harbor, NY, USA, 1999; pp. 131–172. [ Google Scholar ]
- León-Quinto, T.; Jones, J.; Skoudy, A.; Burcin, M.; Soria, B. In vitro directed differentation of mouse embryonic stem cells into insulin-producing cells. Diabetologia 2004 , 47 , 1442–1451. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Holm, S. Time to reconsider stem cell ethics—The importance of induced pluripotent cells. J. Med. Ethics 2008 , 34 , 63–64. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
| Class | Genes | Main Function |
|---|---|---|
| Genes modulating homeostasis of glucose | GLUTs | Involved in the re-absorption of filtered glucose from the kidney into the bloodstream |
| SGLTs | Partake profoundly in muscle and hepatic glucose fluxes | |
| FGFs | Functions significantly in the homeostasis of glucose | |
| SIRT6 | Connected with an expression of GLUTs and increased glycolysis | |
| Genes enhancing the secretion of insulin and/or sensitivity | GLP-1 and its analogs/agonists | Boost the survival of beta-cell, provoke the expression of the insulin gene, and synthesis |
| GPGRs and their agonists | Enhances the secretion of insulin and GLP-1 | |
| CTB-APSL | Enhances secretion of insulin and insulin resistance | |
| IKK E, TBK1 | Linked with diminution in weight, insulin resistance, fatty liver as well as inflammation | |
| Genes attenuating diabetic induced complications | IL-1b | Linked with inflammation and b-cell failure |
| ADPN | Attenuates diabetic nephropathy | |
| TGF-a | Has a function in DKD linked with nephron reduction | |
| NLRP3 | Attenuates diabetic cardiomyopathy | |
| CDKN2A/2B | connected with modulation of T-cell phenotype and chronic inflammation | |
| HSP70 | Connected with bioenergetics of mitochondrion and diabetic sensory neuropathy | |
| MicroRNAs | Implicated in the modulation of diabetic microvasculature |
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Aloke, C.; Egwu, C.O.; Aja, P.M.; Obasi, N.A.; Chukwu, J.; Akumadu, B.O.; Ogbu, P.N.; Achilonu, I. Current Advances in the Management of Diabetes Mellitus. Biomedicines 2022 , 10 , 2436. https://doi.org/10.3390/biomedicines10102436
Aloke C, Egwu CO, Aja PM, Obasi NA, Chukwu J, Akumadu BO, Ogbu PN, Achilonu I. Current Advances in the Management of Diabetes Mellitus. Biomedicines . 2022; 10(10):2436. https://doi.org/10.3390/biomedicines10102436
Aloke, Chinyere, Chinedu Ogbonnia Egwu, Patrick Maduabuchi Aja, Nwogo Ajuka Obasi, Jennifer Chukwu, Blessing Oluebube Akumadu, Patience Nkemjika Ogbu, and Ikechukwu Achilonu. 2022. "Current Advances in the Management of Diabetes Mellitus" Biomedicines 10, no. 10: 2436. https://doi.org/10.3390/biomedicines10102436
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Type 2 diabetes articles from across Nature Portfolio
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency of the pancreatic β-cell hormone insulin.
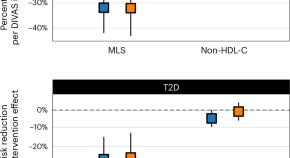
Blood lipid profiling indicates that dietary fat quality is associated with cardiometabolic risk
Dietary guidelines advise substituting saturated fats with unsaturated fats. We used detailed blood fat composition profiling in diet trials and population studies to confirm that a moderate high-fat diet from plant oils is better for metabolism and heart health than a diet with similar fat levels from animal sources.
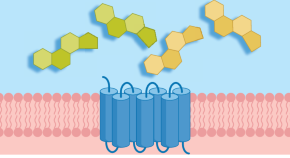
New insights into the regulation of GIPR signalling
Two recent studies have unravelled novel modes of glucose-dependent insulinotropic polypeptide receptor (GIPR) signalling regulation. Kizilkaya et al. characterized the effect of changes in β-arrestin 2 coupling with naturally occurring GIPR coding variants, whereas Regmi et al. investigated GIPR expression profiles and functional regulation in adipocytes.
- Yusman Manchanda
- Alejandra Tomas

Years lived with and years lost to multiple long-term condition combinations that include diabetes
We introduced time-based metrics to analyze multiple long-term condition (MLTC) combinations of two or more conditions that include diabetes, among adults in England. We calculated the median age of MLTC onset and years of life lived with and lost to the MLTC, and examined MLTC burdens from both individual perspectives and community perspectives.
Latest Research and Reviews
Tirzepatide outcompetes long-acting insulin in managing type 2 diabetes: a meta-analysis of three phase 3 randomized controlled trials
- Razieh Mohammad Jafari
- Mohammad Poursalehian
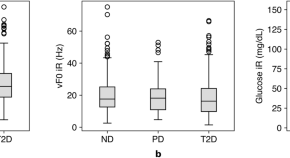
Linear effects of glucose levels on voice fundamental frequency in type 2 diabetes and individuals with normoglycemia
- Jaycee Kaufman
- Jouhyun Jeon
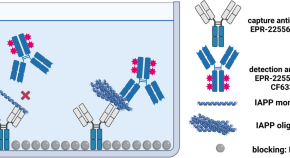
IAPP - oligomerisation levels in plasma of people with type 2 diabetes
- Fabian Rehn
- Victoria Kraemer-Schulien
- Dieter Willbold
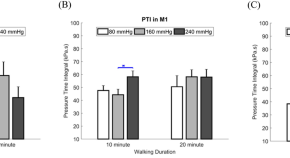
Effect of different inner pressures of air insoles and walking durations on plantar pressure time integral
- Gilang Titah Ramadhan
- Fahni Haris
- Chi-Wen Lung
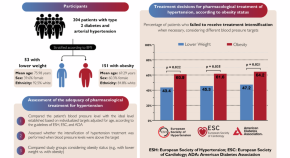
Hidden barriers: obesity bias in hypertension treatment
- Guilherme Heiden Telo
- Lucas Strassburger Matzenbacher
- Gabriela Heiden Telo

A roadmap to the molecular human linking multiomics with population traits and diabetes subtypes
Multiomic phenotyping provides molecular insights into complex physiological processes and pathologies. The study uses 18 omics platforms to analyze biofluids from 391 participants. It constructs a comprehensive molecular network based on omics integration, revealing insights into diabetes and other traits.
- Anna Halama
- Shaza Zaghlool
- Karsten Suhre
News and Comment
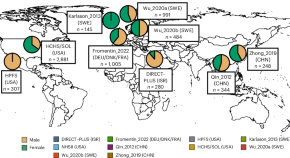
Linking gut microbial strains and functions to diabetes in an international population
Although gut microorganisms have been associated with type 2 diabetes, the mechanisms involving specific microbial strains remain unidentified. Now, a comprehensive study has analyzed 8,117 shotgun metagenomes from the USA, Europe, Israel and China, providing cross-population microbial signatures in a strain-resolved manner and new mechanistic insights into type 2 diabetes.

How medical schools can prepare students for new technologies
Patient educators and nurses can demonstrate the real-life use of health technologies.
- Chantal Mathieu
Bile acid receptor protects against diabetic cardiomyopathy
Activation of the bile acid receptor TGR5 inhibits CD36-mediated fatty acid uptake in cardiomyocytes and protects against cardiac lipotoxicity and the development of diabetic cardiomyopathy in mice, according to a new study.
- Irene Fernández-Ruiz
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
HYPOTHESIS AND THEORY article
Type 2 diabetes mellitus: a pathophysiologic perspective.

- Department of Medicine, Duke University, Durham, NC, United States
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5–10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years, and their effectiveness may simply be due to lowering the dietary contribution to glucose and insulin levels, which then leads to improvements in hyperglycemia and hyperinsulinemia. Treatments for T2DM that lead to improvements in glycemic control and reductions in blood insulin levels are sensible based on this pathophysiologic perspective. In this article, a pathophysiological argument for using carbohydrate restriction to treat T2DM will be made.
Introduction
Type 2 Diabetes Mellitus (T2DM) is characterized by a persistently elevated blood glucose, or an elevation of blood glucose after a meal containing carbohydrate ( 1 ) ( Table 1 ). Unlike Type 1 Diabetes which is characterized by a deficiency of insulin, most individuals affected by T2DM have elevated insulin levels (fasting and/or post glucose ingestion), unless there has been beta cell failure ( 2 , 3 ). The term “insulin resistance” (IR) has been used to explain why the glucose levels remain elevated even though there is no deficiency of insulin ( 3 , 4 ). Attempts to determine the etiology of IR have involved detailed examinations of molecular and intracellular pathways, with attribution of cause to fatty acid flux, but the root cause has been elusive to experts ( 5 – 7 ).
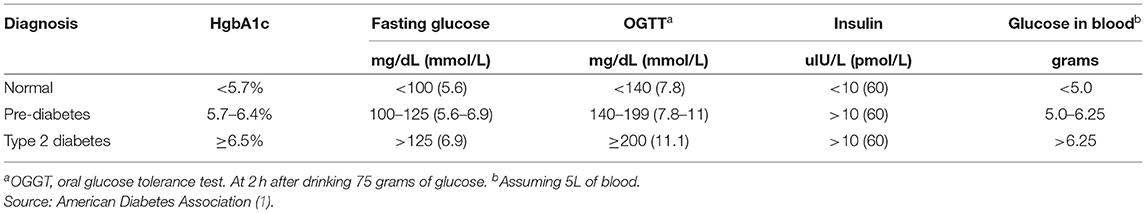
Table 1 . Definition of type 2 diabetes mellitus.
How Much Glucose Is in the Blood?
Keeping in mind that T2DM involves an elevation of blood glucose, it is important to understand how much glucose is in the blood stream to begin with, and then the factors that influence the blood glucose—both exogenous and endogenous factors. The amount of glucose in the bloodstream is carefully controlled—approximately 5–10 grams in the bloodstream at any given moment, depending upon the size of the person. To calculate this, multiply 100 milligrams/deciliter × 1 gram/1,000 milligrams × 10 deciliters/1 liter × 5 liters of blood. The “zeros cancel” and you are left with 5 grams of glucose if the individual has 5 liters of blood. Since red blood cells represent about 40% of the blood volume, and the glucose is in equilibrium, there may be an extra 40% glucose because of the red blood cell reserve ( 8 ). Adding the glucose from the serum and red blood cells totals about 5–10 grams of glucose in the entire bloodstream.
Major Exogenous Factors That Raise the Blood Glucose
Dietary carbohydrate is the major exogenous factor that raises the blood glucose. When one considers that it is common for an American in 2021 to consume 200–300 grams of carbohydrate daily, and most of this carbohydrate is digested and absorbed as glucose, the body absorbs and delivers this glucose via the bloodstream to the cells while attempting to maintain a normal blood glucose level. Thinking of it in this way, if 200–300 grams of carbohydrates is consumed in a day, the bloodstream that holds 5–10 grams of glucose and has a concentration of 100 milligrams/deciliter, is the conduit through which 200,000–300,000 milligrams (200 grams = 200,000 milligrams) passes over the course of a day.
Major Endogenous Factors That Raise the Blood Glucose
There are many endogenous contributors that raise the blood glucose. There are at least 3 different hormones that increase glucose levels: glucagon, epinephrine, and cortisol. These hormones increase glucose levels by increasing glycogenolysis and gluconeogenesis ( 9 ). Without any dietary carbohydrate, the normal human body can generate sufficient glucose though the mechanism of glucagon secretion, gluconeogenesis, glycogen storage and glycogenolysis ( 10 ).
Major Exogenous Factors That Lower the Blood Glucose
A reduction in dietary carbohydrate intake can lower the blood glucose. An increase in activity or exercise usually lowers the blood glucose ( 11 ). There are many different medications, employing many mechanisms to lower the blood glucose. Medications can delay sucrose and starch absorption (alpha-glucosidase inhibitors), slow gastric emptying (GLP-1 agonists, DPP-4 inhibitors) enhance insulin secretion (sulfonylureas, meglitinides, GLP-1 agonists, DPP-4 inhibitors), reduce gluconeogenesis (biguanides), reduce insulin resistance (biguanides, thiazolidinediones), and increase urinary glucose excretion (SGLT-2 inhibitors). The use of medications will also have possible side effects.
Major Endogenous Factors That Lower the Blood Glucose
The major endogenous mechanism to lower the blood glucose is to deliver glucose into the cells (all cells can use glucose). If the blood glucose exceeds about 180 milligrams/deciliter, then loss of glucose into the urine can occur. The blood glucose is reduced by cellular uptake using glut transporters ( 12 ). Some cells have transporters that are responsive to the presence of insulin to activate (glut4), others have transporters that do not require insulin for activation. Insulin-responsive glucose transporters in muscle cells and adipose cells lead to a reduction in glucose levels—especially after carbohydrate-containing meals ( 13 ). Exercise can increase the glucose utilization in muscle, which then increases glucose cellular uptake and reduce the blood glucose levels. During exercise, when the metabolic demands of skeletal muscle can increase more than 100-fold, and during the absorptive period (after a meal), the insulin-responsive glut4 transporters facilitate the rapid entry of glucose into muscle and adipose tissue, thereby preventing large fluctuations in blood glucose levels ( 13 ).
Which Cells Use Glucose?
Glucose can used by all cells. A limited number of cells can only use glucose, and are “glucose-dependent.” It is generally accepted that the glucose-dependent cells include red blood cells, white blood cells, and cells of the renal papilla. Red blood cells have no mitochondria for beta-oxidation, so they are dependent upon glucose and glycolysis. White blood cells require glucose for the respiratory burst when fighting infections. The cells of the inner renal medulla (papilla) are under very low oxygen tension, so therefore must predominantly use glucose and glycolysis. The low oxygen tension is a result of the countercurrent mechanism of urinary concentration ( 14 ). These glucose-dependent cells have glut transporters that do not require insulin for activation—i.e., they do not need insulin to get glucose into the cells. Some cells can use glucose and ketones, but not fatty acids. The central nervous system is believed to be able to use glucose and ketones for fuel ( 15 ). Other cells can use glucose, ketones, and fatty acids for fuel. Muscle, even cardiac muscle, functions well on fatty acids and ketones ( 16 ). Muscle cells have both non-insulin-responsive and insulin-responsive (glut4) transporters ( 12 ).
Possible Dual Role of an Insulin-Dependent Glucose-Transporter (glut4)
A common metaphor is to think of the insulin/glut transporter system as a key/lock mechanism. Common wisdom states that the purpose of insulin-responsive glut4 transporters is to facilitate glucose uptake when blood insulin levels are elevated. But, a lock serves two purposes: to let someone in and/or to keep someone out . So, one of the consequences of the insulin-responsive glut4 transporter is to keep glucose out of the muscle and adipose cells, too, when insulin levels are low. The cells that require glucose (“glucose-dependent”) do not need insulin to facilitate glucose entry into the cell (non-insulin-responsive transporters). In a teleological way, it would “make no sense” for cells that require glucose to have insulin-responsive glut4 transporters. Cells that require glucose have glut1, glut2, glut3, glut5 transporters—none of which are insulin-responsive (Back to the key/lock metaphor, it makes no sense to have a lock on a door that you want people to go through). At basal (low insulin) conditions, most glucose is used by the brain and transported by non-insulin-responsive glut1 and glut3. So, perhaps one of the functions of the insulin-responsive glucose uptake in muscle and adipose to keep glucose OUT of the these cells at basal (low insulin) conditions, so that the glucose supply can be reserved for the tissue that is glucose-dependent (blood cells, renal medulla).
What Causes IR and T2DM?
The current commonly espoused view is that “Type 2 diabetes develops when beta-cells fail to secrete sufficient insulin to keep up with demand, usually in the context of increased insulin resistance.” ( 17 ). Somehow, the beta cells have failed in the face of insulin resistance. But what causes insulin resistance? When including the possibility that the environment may be part of the problem, is it possible that IR is an adaptive (protective) response to excess glucose availability? From the perspective that carbohydrate is not an essential nutrient and the change in foods in recent years has increased the consumption of refined sugar and flour, maybe hyperinsulinemia is the cause of IR and T2DM, as cells protect themselves from excessive glucose and insulin levels.
Insulin Is Already Elevated in IR and T2DM
Clinical experience of most physicians using insulin to treat T2DM over time informs us that an escalation of insulin dose is commonly needed to achieve glycemic control (when carbohydrate is consumed). When more insulin is given to someone with IR, the IR seems to get worse and higher levels of insulin are needed. I have the clinical experience of treating many individuals affected by T2DM and de-prescribing insulin as it is no longer needed after consuming a diet without carbohydrate ( 18 ).
Diets Without Carbohydrate Reverse IR and T2DM
When dietary manipulation was the only therapy for T2DM, before medications were available, a carbohydrate-restricted diet was used to treat T2DM ( 19 – 21 ). Clinical experience of obesity medicine physicians and a growing number of recent studies have demonstrated that carbohydrate-restricted diets reverse IR and T2DM ( 18 , 22 , 23 ). Other methods to achieve caloric restriction also have these effects, like calorie-restricted diets and bariatric surgery ( 24 , 25 ). There may be many mechanisms by which these approaches may work: a reduction in glucose, a reduction in insulin, nutritional ketosis, a reduction in metabolic syndrome, or a reduction in inflammation ( 26 ). Though there may be many possible mechanisms, let's focus on an obvious one: a reduction in blood glucose. Let's assume for a moment that the excessive glucose and insulin leads to hyperinsulinemia and this is the cause of IR. On a carbohydrate-restricted diet, the reduction in blood glucose leads to a reduction in insulin. The reduction in insulin leads to a reduction in insulin resistance. The reduction in insulin leads to lipolysis. The resulting lowering of blood glucose, insulin and body weight reverses IR, T2DM, AND obesity. These clinical observations strongly suggest that hyperinsulinemia is a cause of IR and T2DM—not the other way around.
What Causes Atherosclerosis?
For many years, the metabolic syndrome has been described as a possible cause of atherosclerosis, but there are no RCTs directly targeting metabolic syndrome, and the current drug treatment focuses on LDL reduction, so its importance remains controversial. A recent paper compared the relative importance of many risk factors in the prediction of the first cardiac event in women, and the most powerful predictors were diabetes, metabolic syndrome, smoking, hypertension and BMI ( 27 ). The connection between dietary carbohydrate and fatty liver is well-described ( 28 ). The connection between fatty liver and atherosclerosis is well-described ( 29 ). It is very possible that the transport of excess glucose to the adipose tissue via lipoproteins creates the particles that cause the atherosclerotic damage (small LDL) ( Figure 1 ) ( 30 – 32 ). This entire process of dietary carbohydrate leading to fatty liver, leading to small LDL, is reversed by a diet without carbohydrate ( 26 , 33 , 34 ).
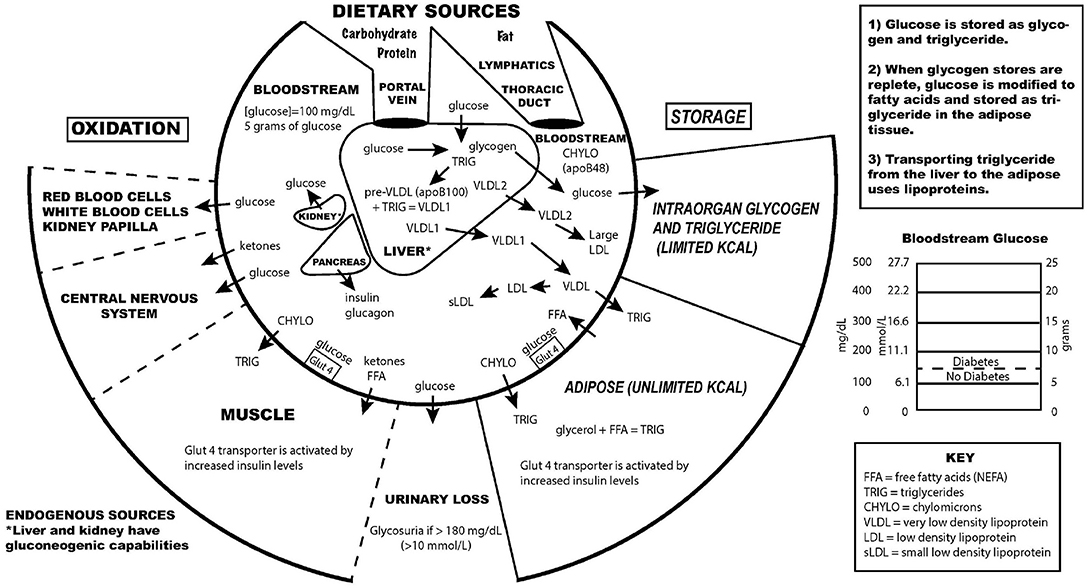
Figure 1 . Key aspects of the interconnection between glucose and lipoprotein metabolism.
Reducing dietary carbohydrate in the context of a low carbohydrate, ketogenic diet reduces hyperglycemia and hyperinsulinemia, IR and T2DM. In the evaluation of an individual for a glucose abnormality, measure the blood glucose and insulin levels. If the insulin level (fasting or after a glucose-containing meal) is high, do not give MORE insulin—instead, use an intervention to lower the insulin levels. Effective ways to reduce insulin resistance include lifestyle, medication, and surgical therapies ( 23 , 35 ).
The search for a single cause of a complex problem is fraught with difficulty and controversy. I am not hypothesizing that excessive dietary carbohydrate is the only cause of IR and T2DM, but that it is a cause, and quite possibly the major cause. How did such a simple explanation get overlooked? I believe it is very possible that the reductionistic search for intracellular molecular mechanisms of IR and T2DM, the emphasis on finding pharmaceutical (rather than lifestyle) treatments, the emphasis on the treatment of high total and LDL cholesterol, and the fear of eating saturated fat may have misguided a generation of researchers and clinicians from the simple answer that dietary carbohydrate, when consumed chronically in amounts that exceeds an individual's ability to metabolize them, is the most common cause of IR, T2DM and perhaps even atherosclerosis.
While there has historically been a concern about the role of saturated fat in the diet as a cause of heart disease, most nutritional experts now cite the lack of evidence implicating dietary saturated fat as the reason for lack of concern of it in the diet ( 36 ).
The concept of comparing medications that treat IR by insulin-sensitizers or by providing insulin itself was tested in the Bari-2D study ( 37 ). Presumably in the context of consuming a standard American diet, this study found no significant difference in death rates or major cardiovascular events between strategies of insulin sensitization or insulin provision.
While lifestyle modification may be ideal to prevent or cure IR and T2DM, for many people these changes are difficult to learn and/or maintain. Future research should be directed toward improving adherence to all effective lifestyle or medication treatments. Future research is also needed to assess the effect of carbohydrate restriction on primary or secondary prevention of outcomes of cardiovascular disease.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
EW receives royalties from popular diet books and is founder of a company based on low-carbohydrate diet principles (Adapt Your Life, Inc.).
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care . (2016) 39 (Suppl. 1):S13–22. doi: 10.2337/dc16-S005
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Bogardus C, Lillioja S, Howard BV, Reaven G, Mott D. Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest. (1984) 74:1238–46. doi: 10.1172/JCI111533
3. Reaven GM. Compensatory hyperinsulinemia and the development of an atherogenic lipoprotein profile: the price paid to maintain glucose homeostasis in insulin-resistant individuals. Endocrinol Metab Clin North Am. (2005) 34:49–62. doi: 10.1016/j.ecl.2004.12.001
4. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. (1991) 14:173–94. doi: 10.2337/diacare.14.3.173
5. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. (2005) 365:1415–28. doi: 10.1016/S0140-6736(05)66378-7
6. Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. (2019) 234:8152–61. doi: 10.1002/jcp.27603
7. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. (2000) 106:171–6. doi: 10.1172/JCI10583
8. Guizouarn H, Allegrini B. Erythroid glucose transport in health and disease. Pflugers Arch. (2020) 472:1371–83. doi: 10.1007/s00424-020-02406-0
9. Petersen MC, Vatner DF, Shulman GI. Regulation of hepatic glucose metabolism in health and disease. Nat Rev Endocrinol. (2017) 13:572–87. doi: 10.1038/nrendo.2017.80
10. Tondt J, Yancy WS, Westman EC. Application of nutrient essentiality criteria to dietary carbohydrates. Nutr Res Rev. (2020) 33:260–70. doi: 10.1017/S0954422420000050
11. Colberg SR, Hernandez MJ, Shahzad F. Blood glucose responses to type, intensity, duration, and timing of exercise. Diabetes Care. (2013) 36:e177. doi: 10.2337/dc13-0965
12. Mueckler M, Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol Aspects Med. (2013) 34:121–38. doi: 10.1016/j.mam.2012.07.001
13. Bryant NJ, Govers R, James DE. Regulated transport of the glucose transporter GLUT4. Nat Rev Mol Cell Biol. (2002) 3:267–77. doi: 10.1038/nrm782
14. Epstein FH. Oxygen and renal metabolism. Kidney Int. (1997) 51:381–5. doi: 10.1038/ki.1997.50
15. Cahill GF. Fuel metabolism in starvation. Annu Rev Nutr. (2006) 26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258
16. Murashige D, Jang C, Neinast M, Edwards JJ, Cowan A, Hyman MC, et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science. (2020) 370:364–8. doi: 10.1126/science.abc8861
17. Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. (2017) 66:241–55. doi: 10.2337/db16-0806
18. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. (2008) 5:36. doi: 10.1186/1743-7075-5-36
CrossRef Full Text | Google Scholar
19. Allen F. The treatment of diabetes. Boston Med Surg J. (1915) 172:241–7. doi: 10.1056/NEJM191502181720702
20. Osler W, McCrae T. The Principles and Practice of Medicine . 9th ed. New York and London: Appleton & Company (1923).
21. Lennerz BS, Koutnik AP, Azova S, Wolfsdorf JI, Ludwig DS. Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest. (2021) 131:e142246. doi: 10.1172/JCI142246
22. Steelman GM, Westman EC. Obesity: Evaluation and Treatment Essentials . 2nd ed. Boca Raton: CRC Press, Taylor & Francis Group (2016). 340 p.
23. Athinarayanan SJ, Adams RN, Hallberg SJ, McKenzie AL, Bhanpuri NH, Campbell WW, et al. Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol. (2019) 10:348. doi: 10.3389/fendo.2019.00348
24. Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. (2011) 54:2506–14. doi: 10.1007/s00125-011-2204-7
25. Isbell JM, Tamboli RA, Hansen EN, Saliba J, Dunn JP, Phillips SE, et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care. (2010) 33:1438–42. doi: 10.2337/dc09-2107
26. Bhanpuri NH, Hallberg SJ, Williams PT, McKenzie AL, Ballard KD, Campbell WW, et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol. (2018) 17:56. doi: 10.1186/s12933-018-0698-8
27. Dugani SB, Moorthy MV, Li C, Demler OV, Alsheikh-Ali AA, Ridker PM, et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident coronary heart disease in women. JAMA Cardiol. (2021) 6:437–47. doi: 10.1001/jamacardio.2020.7073
28. Duwaerts CC, Maher JJ. Macronutrients and the adipose-liver axis in obesity and fatty liver. Cell Mol Gastroenterol Hepatol. (2019) 7:749–61. doi: 10.1016/j.jcmgh.2019.02.001
29. Zhang L, She Z-G, Li H, Zhang X-J. Non-alcoholic fatty liver disease: a metabolic burden promoting atherosclerosis. Clin Sci Lond Engl. (1979) 134:1775–99. doi: 10.1042/CS20200446
30. Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am J Clin Nutr. (1995) 62:19–29. doi: 10.1093/ajcn/62.1.19
31. Packard C, Caslake M, Shepherd J. The role of small, dense low density lipoprotein (LDL): a new look. Int J Cardiol. (2000) 74 (Suppl. 1):S17–22. doi: 10.1016/S0167-5273(99)00107-2
32. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. (2020) 41:2313–30. doi: 10.1093/eurheartj/ehz962
33. Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. (2004) 140:769. doi: 10.7326/0003-4819-140-10-200405180-00006
34. Tendler D, Lin S, Yancy WS, Mavropoulos J, Sylvestre P, Rockey DC, et al. The effect of a low-carbohydrate, ketogenic diet on nonalcoholic fatty liver disease: a pilot study. Dig Dis Sci. (2007) 52:589–93. doi: 10.1007/s10620-006-9433-5
35. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. (1995) 222:339–50. doi: 10.1097/00000658-199509000-00011
36. Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 76:844–57. doi: 10.1016/j.jacc.2020.05.077
37. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med . (2009) 360:2503–15. doi: 10.1056/NEJMoa0805796
Keywords: type 2 diabetes, insulin resistance, pre-diabetes, carbohydrate-restricted diets, hyperinsulinemia, hyperglycemia
Citation: Westman EC (2021) Type 2 Diabetes Mellitus: A Pathophysiologic Perspective. Front. Nutr. 8:707371. doi: 10.3389/fnut.2021.707371
Received: 09 May 2021; Accepted: 20 July 2021; Published: 10 August 2021.
Reviewed by:
Copyright © 2021 Westman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eric C. Westman, ewestman@duke.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Diabetes mellitus: an overview of the types, symptoms, complications and management
Affiliation.
- 1 School of Nursing, Avondale University, Wahroonga, Sydney NSW, Australia.
- PMID: 34708622
- DOI: 10.7748/ns.2021.e11709
The incidence of diabetes mellitus is rapidly increasing, and this condition often results in significant metabolic disease and severe complications. Nurses have a crucial role in monitoring, educating and supporting people with diabetes, as well as their families and significant others. This article provides an overview of the main types and common symptoms of diabetes, its acute and long-term complications and its management. It also outlines the nurse's role in diabetes care, which frequently includes assessing and empowering patients.
Keywords: blood glucose; clinical; diabetes; diabetic foot ulcers; diabetic ketoacidosis; glycaemic control; hyperglycaemia; hypoglycaemia; insulin; type 1 diabetes; type 2 diabetes.
© 2021 RCN Publishing Company Ltd. All rights reserved. Not to be copied, transmitted or recorded in any way, in whole or part, without prior permission of the publishers.
PubMed Disclaimer
Conflict of interest statement
None declared
Similar articles
- Perioperative care of the adult diabetic patient. Lloyd H. Lloyd H. J Perioper Pract. 2020 Dec;30(12):372-377. doi: 10.1177/1750458920915660. Epub 2020 Apr 17. J Perioper Pract. 2020. PMID: 32301384
- [Diabetes mellitus in children]. Körner A. Körner A. Orv Hetil. 2005 Jun 19;146(25):1335-43. Orv Hetil. 2005. PMID: 16106756 Review. Hungarian.
- Children and young people with diabetes: recognition and management. Hamilton H, Knudsen G, Vaina CL, Smith M, Paul SP. Hamilton H, et al. Br J Nurs. 2017 Mar 23;26(6):340-347. doi: 10.12968/bjon.2017.26.6.340. Br J Nurs. 2017. PMID: 28345986
- Understanding the principles of insulin use in type 1 and type 2 diabetes management. Smyth T. Smyth T. Nurs Stand. 2021 Jan 13;36(1):61-66. doi: 10.7748/ns.2020.e11677. Epub 2020 Dec 30. Nurs Stand. 2021. PMID: 33377355
- Repaglinide : a pharmacoeconomic review of its use in type 2 diabetes mellitus. Plosker GL, Figgitt DP. Plosker GL, et al. Pharmacoeconomics. 2004;22(6):389-411. doi: 10.2165/00019053-200422060-00005. Pharmacoeconomics. 2004. PMID: 15099124 Review.
- In vivo and computational investigation of butin against alloxan-induced diabetes via biochemical, histopathological, and molecular interactions. Bukhari HA, Afzal M, Al-Abbasi FA, Sheikh RA, Alqurashi MM, Bawadood AS, Alzarea SI, Alamri A, Sayyed N, Kazmi I. Bukhari HA, et al. Sci Rep. 2024 Sep 4;14(1):20633. doi: 10.1038/s41598-024-71577-y. Sci Rep. 2024. PMID: 39232184 Free PMC article.
- Diabetes and Osteoarthritis: Exploring the Interactions and Therapeutic Implications of Insulin, Metformin, and GLP-1-Based Interventions. Halabitska I, Babinets L, Oksenych V, Kamyshnyi O. Halabitska I, et al. Biomedicines. 2024 Jul 23;12(8):1630. doi: 10.3390/biomedicines12081630. Biomedicines. 2024. PMID: 39200096 Free PMC article. Review.
- Bergenin mitigates neuroinflammatory damage induced by high glucose: insights from Zebrafish, murine microbial cell line, and rat models. Yu W, Luo R, He C, Li Z, Yang M, Zhou J, He J, Chen Q, Song Z, Cheng S. Yu W, et al. Front Pharmacol. 2024 Aug 1;15:1339178. doi: 10.3389/fphar.2024.1339178. eCollection 2024. Front Pharmacol. 2024. PMID: 39148536 Free PMC article.
- Anethole Prevents the Alterations Produced by Diabetes Mellitus in the Sciatic Nerve of Rats. Barbosa-Ferreira BS, Silva FERD, Gomes-Vasconcelos YA, Joca HC, Coelho-de-Souza AN, Ferreira-da-Silva FW, Leal-Cardoso JH, Silva-Alves KSD. Barbosa-Ferreira BS, et al. Int J Mol Sci. 2024 Jul 25;25(15):8133. doi: 10.3390/ijms25158133. Int J Mol Sci. 2024. PMID: 39125701 Free PMC article.
- Association between weight-adjusted waist index and risk of diabetes mellitus type 2 in United States adults and the predictive value of obesity indicators. Li X, Zhao D, Wang H. Li X, et al. BMC Public Health. 2024 Jul 29;24(1):2025. doi: 10.1186/s12889-024-19576-6. BMC Public Health. 2024. PMID: 39075353 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Perception and coping mechanisms of patients with diabetes mellitus during the COVID-19 pandemic in Ibadan, Nigeria
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing
Affiliation Department of Sociology, University of Wroclaw, Wroclaw, Poland
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Demography and Population Studies, University of Witwatersrand, Johannesburg, South Africa, Department of Public Health, School of Business and Health Studies, York St John University, London, United Kingdom
Roles Writing – original draft, Writing – review & editing
Affiliation Department of Family and Community Health, Fred N. Binka School of Public Health, University of Health and Allied Sciences, Hohoe, Ghana
Affiliation Department of Internal Medicine, College of Medicine, University of Ibadan & University College Hospital, Ibadan, Nigeria
- Olajumoke Ololade Tunji-Adepoju,
- Obasanjo Afolabi Bolarinwa,
- Richard Gyan Aboagye,
- Williams O. Balogun

- Published: August 27, 2024
- https://doi.org/10.1371/journal.pone.0309451
- Peer Review
- Reader Comments
The 2019 coronavirus disease (COVID-19) ushered in a period of fear and uncertainty, resulting in structural instability across the globe. Vulnerable individuals, such as patients with diabetes mellitus, are predispose to have adverse effects and complications of COVID-19 when infected. We explored the perception of diabetes mellitus patients during the COVID-19 pandemic and their coping mechanisms at the University College Hospital, Ibadan.
We employed an exploratory qualitative study design to explore diabetes mellitus patients’ perceptions and coping mechanisms during the COVID-19 pandemic. A purposive sampling technique was used to recruit 32 participants (2 health professionals and 30 diabetes mellitus patients). In-depth interviews were used to collect the data from the participants. All the recorded audio data were transcribed verbatim and exported to NVivo software for thematic data analyses.
Most diabetes mellitus patients were not fearful of the pandemic but were optimistic that it would not affect their health. Mechanisms such as the usage of herbal medicines and adherence to COVID-19 precautionary measures were noticed among patients. The study also revealed that the hospital’s coping mechanism during the COVID-19 pandemic include prolonged appointments, limiting the number of patients attended per clinic day, and the provision of telehealth service. Patients in our study utilised negative coping mechanisms such as reduced drug dosages, subscriptions to cheaper drug brands, and reliance on religious institutions rather than a clinic for health instructions.
Conclusions
The study has shown that diabetes mellitus patients were not fearful of the COVID-19 pandemic. The utilisation of telehealth, encouragement of daily monitoring of sugar levels, provision of avenues for a medication review, and adherence to the safety protocols were coping mechanisms employed by the health system and diabetes mellitus patients. We recommend that the government and other healthcare stakeholders reinforce the resilience of diabetes mellitus patients by alleviating their health burdens during the pandemic. This could be done by subsidizing the prices of drugs, tests, and consultation fees for patients with diabetes mellitus. Also, more efforts should be made to elevate the health system through the reduction in waiting and appointment times in the diabetes clinic and employing more health personnel in the clinic.
Citation: Tunji-Adepoju OO, Afolabi Bolarinwa O, Aboagye RG, Balogun WO (2024) Perception and coping mechanisms of patients with diabetes mellitus during the COVID-19 pandemic in Ibadan, Nigeria. PLoS ONE 19(8): e0309451. https://doi.org/10.1371/journal.pone.0309451
Editor: Sylla Thiam, Sunu Sante Consulting, SENEGAL
Received: June 26, 2023; Accepted: August 12, 2024; Published: August 27, 2024
Copyright: © 2024 Tunji-Adepoju et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data utilised in this research contain potentially identifying or sensitive patient information; data are owned by the Institute for Advanced Medical Research and Training (IAMRAT). Please get in touch with IAMRAT via [email protected] or the first author for data request and access.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: COVID-19, Coronavirus Disease 2019; IDI, In-depth Interview; KII, Key Informant Interview; NCD, Non-Communicable Diseases; NCDC, Nigeria Centre for Disease Control and Prevention; WHO, World Health Organization
Diabetes Mellitus has been an important global health concern even prior to the outbreak of the 2019 coronavirus disease (COVID-19). Diabetes mellitus is a chronic health condition characterized by high blood glucose due to either the inability of the pancreas to produce adequate insulin or the body’s resistance to available insulin [ 1 ]. Poorly managed diabetes mellitus can result in long-term complications such as amputation, cardiovascular disease, vision impairment, and renal disease [ 1 ]. The prevalence of diabetes mellitus is increasing across the globe. Between 1980 and 2014, the number of patients with diabetes mellitus increased from 108 million to 422 million [ 2 ] and over 500 million in 2020 [ 3 , 4 ]. Diabetes mellitus is projected to be the seventh leading cause of death worldwide by 2030 [ 2 ]. The burden of diabetes is greatly increasing in sub-Saharan Africa, and Nigeria has the largest share of this burden [ 5 , 6 ]. Evidence suggests that an estimated 11 million Nigerians have diabetes [ 7 ]. This implies that more than five percent of the Nigerian population is living with the disease, and it is a major cause of death among many Nigerians below 70 years old [ 8 ].
Research has shown that the presence of excess blood glucose, also known as hyperglycemia in diabetes patients, makes them susceptible to COVID-19 [ 9 , 10 ]. In the same vein, a study reported that patients with diabetes are two times more likely to develop severe conditions or die from COVID-19, while people living with uncontrolled diabetes are about 13 times more likely to die from the virus [ 9 ]. This has instilled fear in many patients with diabetes in Nigeria [ 10 ]. Hence, the fact that patients with diabetes need extra health care and attention during the pandemic remains undisputable [ 11 ]. Measures to prevent and control Non-Communicable Diseases (NCDs), such as diabetes, in developing countries, including Nigeria, have not been effectively implemented. The COVID-19 pandemic worsened the accumulated effects of Nigeria’s failure to improve the healthcare structure and system, particularly the care of people with NCDs. The outbreak of COVID-19 in Nigeria on the 27th of February 2020 [ 12 ] also caused dysfunctionality and complications in the Nigerian social structures, requiring sporadic responses.
Predictably, the response to COVID-19 in Nigeria infringed on treating other diseases, including diabetes mellitus [ 13 ]. For instance, many public hospitals were converted to COVID-19 treatment centers resulting in restricted access of other patients to medical care [ 5 , 14 ]. Also, the World Health Organization (WHO) stipulated in its report that the COVID-19 pandemic negatively impacted the equity regarding essential health service delivery in its member states [ 4 , 17 ]. The report further revealed that more than 50% of its member states experienced disruption in delivering health care services on NCDs, cancer, and mental health disorders. Some of the reasons given for this disruption include shortage of staff due to their transfer to COVID-19 care centers, lack of public transport, and cancellation of planned appointments, while the reasons recorded in 20% of the member states were: the shortage of medicines, diagnostics, and other technologies [ 4 ]. Due to the various forms of hardship or discomfort caused by the pandemic, vulnerable individuals, such as people with diabetes mellitus, are likely to perceive the period differently than healthy people. Patients with diabetes are likely to have a negative perception of the COVID-19 condition, which could influence the adoption of harmful coping mechanisms that could further hamper their health outcomes. Although several perception studies have been done on COVID-19 generally in Nigeria, such as that of Osahon and Memudu [ 15 ] on the perception and healthy attitudes of Nigerians to COVID-19, very little data is available about the perception of diabetes patients of the COVID-19 pandemic. This study explored the perceptions of patients with diabetes mellitus during the pandemic and their coping mechanisms during the period. This is important to illuminate the experiences of patients with diabetes mellitus during the pandemic, and the findings could be beneficial to the government and healthcare stakeholders in formulating policies to help improve the health outcomes of patients with diabetes during the pandemic.
Study design
We adopted an explorative qualitative research approach [ 16 ]. This approach is suitable for understanding the perception of diabetes mellitus patients at University College Hospital and the coping mechanisms during the COVID-19 pandemic. This qualitative research approach also guide the collection of in-depth data from the participants in their natural form [ 16 ].
Study setting
The study was conducted in the University College Hospital, Ibadan. University College Hospital is a tertiary health center that serves Oyo state and neighbouring states where patients with diabetes, including those with suspected COVID-19 cases, are seen. According to statistics from the Nigeria Centre for Disease Control and Prevention (NCDC) [ 17 ], Oyo State is among the COVID-19 most infected states in Nigeria, and Ibadan is its capital city. The University College Hospital was founded in November 1952, located at Oritamefa in the Ibadan North Local Government Area. It is the first teaching hospital in Nigeria to provide in-patient and outpatient health care services. It receives referrals from southwestern and other parts of Nigeria and outside the country. The Diabetes clinic runs every Monday, and an average of 50–70 patients visit the clinic daily.
Participant sampling and sample size
Participants in this study were registered diabetes patients who had been visiting the outpatient diabetes clinic at University College Hospital before the pandemic and are still attending the clinic during the pandemic. We used a purposive sampling technique to recruit 30 participants for the study, which was determined using the data saturation method. These participants constituted those who experienced the phenomena under study. Patients who were living with diabetes mellitus disease prior to the pandemic (at least more than a year) and aged 18 years and above were included. However, those accessible during the data collection period were included. The rationale was that this category of patients with diabetes mellitus could tell the difference between their experiences in the clinic before and during the pandemic. Being coherent, healthy, gave informed consent were other inclusion criteria for the study. Patients who did not consent to the study or were no longer interested in participating even while in the middle of it were excluded from the study. Patients diagnosed with diabetes after the outbreak of COVID-19 and/or who did not attend the diabetes clinic during the study period were not included. Also, patients with acute or chronic debilitating comorbidities were not included in the study.
Data collection procedure
Four (4) trained research assistants were used for the data collection. The research assistants were trained anthropologists, who the authors also trained in areas consisting of the consenting process, interviews, asking probing questions, and recording. The authors developed an interview guide as the data collection tool. Data on the participants’ sociodemographic characteristics and the study objectives were collected after obtaining consent. The probe questions were structured to capture responses to the participants’ perceptions of the COVID-19 pandemic. It also covered responses to the coping mechanisms adopted by diabetes mellitus patients during the pandemic. Prior to the data collection, we informed the participants about any possible discomfort, benefits, and compensation associated with the study. Interviews were conducted once the participants agreed to a date, time, and place of convenience to participants. The participants were approached for recruitment at the end of the medical appointments, and those who consented were interviewed at the premises of the hospital. The data collection lasted for an average of 60 minutes per participant. The participants were compensated with an equivalent gift of three US dollars ($3) at the end of the interview.
About 15 interviews were conducted each week for two weeks by one of the authors with four trained anthropologists who had qualitative fieldwork experiences. The anthropologist helped in administering the interview guide. Interviews were conducted with strict adherence to the COVID-19 precautionary measures. The data collection/interviews were done between the 15 th to 22 nd of March 2021 using a pretested interviewer guide. The participants were recruited using a purposive sampling technique. All the interviews were tape-recorded, and field notes were taken and utilised during the transcription and analysis. Data transcription was carried out after every fieldwork, and this helped in identifying questions that may have been left unanswered during the interview or those needing further probing, as well as identifying the point of saturation where no further interviews were conducted. The research assistants helped with field notes, tape recording and data analysis.
Data analysis
All the audio data was transcribed verbatim on the same day the data was collected. After the transcription by the research assistants, After the transcription of the data, the transcripts were vetted and proofread by OOTA, OAB and WOB. Later, the transcripts were made accessible to OAB, who performed the initial independent thematic analysis [ 18 ]. Using the ‘nodes’ function in NVivo-12 software, where codes were assigned to the text data from the transcripts [ 19 ]. During the analysis, all similar recurring codes were categorised to generate themes and, subsequently, sub-themes [ 18 ]. The extracts and quotes from the themes and sub-themes generated were used to support the results of the study. All the authors approved the extracts and quotes. A pretest of the interview guide was done with two (2) potential respondents (male and female) among those who came for medical appointments prior to the actual commencement of the main data collection. The interview guide pretest results show accurate consistency, but the results were not included in the main study.
Rigour and trustworthiness
In every qualitative study, credibility and trustworthiness measures are critical. In achieving this, we allowed two research assistants with experience in qualitative analysis to transcribe and analyze tape-recorded interviews separately. The two research assistants’ themes and sub-themes, as well as the authors, were compared to ascertain their consistency. To strengthen the credibility of the results, direct quotations and precise summaries of participant remarks were used. A week after the transcription and preliminary data analysis, we conducted member-checking with three of the participants to demonstrate trustworthiness. This allowed the participants to attest that the transcripts accurately captured the content of the interviews. Nobody offered changes or voiced complaints about the interviews’ calibre or content in terms of clearly expressing their viewpoints. The participants’ nonverbal cues, their concerns, and the interviewers’ observations were all documented in the field notes that were taken following each interview and consulted throughout the research. The authors who carried out the interviews are qualified healthcare researchers with expertise in conducting IDIs.
Ethical issues
Ethical clearance was sought from the Ibadan/University College Hospital Ethics Committee (UI/UCH EC) with approval number UI/EC/21/0064. In this study, we complied with all the ethical guidelines pertaining to using human participants and peculiar to qualitative studies. We anonymized all the transcripts and audio files by giving them pseudonyms to remove any personal information that may be used to identify the study participants. The participants in the study were given an information sheet that included information on the objectives, methods, potential risks and advantages, compensations, who to contact, and an affirmation of confidentiality, privacy, and autonomy. The participants gave written consent by signing the consent form for participating, and for recording the interviews. Later, the participants’ signed informed consent was requested. This demonstrated that they had read and understood the terms of reference before deciding to participate freely in our study. We also encrypted a passcode and locked the audio files and transcripts to prevent unauthorised individuals from accessing the material.
In-depth interviews were held with thirty patients with diabetes mellitus in the outpatient ward of the endocrinology clinic. Each interview lasted for about an hour.
Demographic characteristics of participants
A total of thirty participants were recruited for the study, consisting of approximately two-thirds females and one-third males. Most participants were elderly, with the oldest being an 84-year-old female and the youngest a 21-year-old male. More than half were Christians, with the remainder being Muslims. All males, except the youngest, were married. Among the females, most were married, with two widows, one single and one separated.
Over half of the participants had tertiary education, a few had secondary education, and a small number had primary education. Only a few females had no formal education, whereas all males had some level of formal education.
Most males were retired, with three employed and one unemployed (the youngest male). Among females, more than two-thirds were employed, three were unemployed, and two were retired. Participants’ socio-economic status ranged from average to low.
Concerning diabetes type awareness, seven out of ten female participants did not know their type, while all but one male participant was aware. Most participants had type 2 diabetes, except for one male and one female in their twenties who had type 1 diabetes.
Emerging themes from the study
Table 1 presents the major themes and sub-themes that emerged from the study. While analyzing data, two key themes emerged: The perception of Diabetes Patients during the COVID-19 Pandemic and the coping mechanisms employed by diabetes mellitus patients during the pandemic.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0309451.t001
Perception of diabetes mellitus patients during the COVID-19 pandemic
This theme contains three sub-themes (clinic appointments, effects of the COVID-19 pandemic on diabetes patients, and adherence to COVID-19 protocols).
Clinic appointments.
Data from the key informant interviews revealed that the pandemic was perceived as a period that has negatively affected appointments, clinic attendance, and the management of diabetes in the clinic. A participant stated that
Yes, like I just told you, it has affected it a lot because I have been coming for months now, and I have not been able to see the doctor (IDI, Participant 10, Female, 45 years). The pandemic has affected my clinic attendance because, presently, I only come to the clinic when the doctor gives me appointments. Prior to the pandemic, asides from my appointment dates, I come to the clinic every first Monday of the month because we diabetes patients usually hold meetings in the diabetes association office; however, since the emergence of the pandemic, we have stopped holding the meeting (IDI, Participant 9, Male, 21 years)
Effects of the COVID-19 pandemic on patients with diabetes mellitus.
This sub-theme has ten codes, which include the vulnerable groups during the pandemic. The participants revealed a clear understanding of the fact that diabetes patients are vulnerable during the pandemic. A number of the patients demonstrated a clear knowledge of the category of people who are vulnerable to COVID-19 infection. They perceived this category of people as the aged, those who defy preventive measures, and people with comorbidities. However, some of the participants were unaware of who could be susceptible to the virus.
Some of the diabetic patients who were not observing the COVID-19 precautionary measures are vulnerable to the virus, as encapsulated in the excerpt below:
Anybody can contract it, especially those who fail to wash their hands and follow the preventive measures (IDI, Participant 2, Male , 75 years). Those who fail to adhere to the necessary precautions , those who talk with their whole mouth open without using their nose masks and those who stay too close to other people (IDI , Participant 9 , Male , 21 years) . The elderly / people with underlying diseases Yes, people that are already sick before and the elderly ones (IDI, Participant 10, female, 45 years). It cannot have any negative impact on diabetes patients if they take their medications regularly and follow necessary precautions (IDI , Participant 9 , Male 21 years) .
Some participants, however, did not know who could get infected with the virus, as evidenced in the below excerpt:
I can’t say (IDI, Participant 1, female , 74 years). Only God knows (IDI , Participant 4 , female , 84years)
They posited that the COVID-19 virus could have severe impacts on them. The opinion of one participant in this regard is captured in the excerpt below:
The diabetes patient could get infected and the person might not get cured of it. It could even kill such a person (IDI, Participant 8 , Female, 52years).
A few others were of the opinion that COVID-19 cannot have any deadly implications on patients with diabetes since one can be treated if infected.
The impact it can have is for one to get infected, and even if one gets infected, since it can be treated. I don’t think it can bring about any deadly impact except for someone whose time is up on this planet earth already (IDI, Participant 12 , Female 28 years).
Patients with diabetes are not vulnerable in as much as they follow their diabetes regimen:
I don ’ t think there should be any effects if they use their drugs regularly, exercise as well and take away the fear of contracting the disease (IDI , Participant 2 , Male 75 years) .
The in-depth interview further revealed that most of the participants were not afraid of the COVID-19 virus. The submission of a participant is clear on this, as evident in the statement below:
Ehn … It did not make me scared because I firstly did not believe it was real but as time went on and I started hearing that people were really contracting it, it was then I believed that COVID-19 is real. However, till now, I have not seen anyone who has contracted it in my vicinity. As such, that is one of the reasons I did not really get scared about it (IDI, Participant 12, Female 28years).
Patients with diabetes mellitus noted that they were not fearful of the pandemic because they trusted in the Supreme Being, their object of worship (God). The results further showed that a couple of patients with diabetes mellitus were not afraid during the pandemic due to their trust in their medications, the quality of health care provided in the University College Hospital diabetes clinic and their proper adherence to the COVID-19 precautionary measures. The excerpts below capture this:
I’m unruffled. I know we have problems all over the world but I’m a Christian and I’m unruffled (IDI, Participant 2 , Male 75 years). I was not afraid , I don’t believe in it . I have Jesus (IDI , Participant 21 , Male 65 years) .
On the contrary, a few participants perceived that the COVID-19 pandemic was a fearful one, and they perceived it to be the end of their life. This is evident in the excerpts below:
A fearful period
I was thinking I was going to die (IDI, Participant 14 , Female 30years). I was very scared , but God’s grace is sufficient (IDI , Participant 1 , Male 74 years) .
Adherence to COVID-19 protocols.
This sub-theme encompassed the physical presentation of patients only when necessary and allowance of physical presentation of patients with strict adherence to COVID-19 protocols.
Findings from the interviews revealed that the clinic avoided unnecessary physical presentation of diabetes mellitus patients during the pandemic by prolonging appointments. Patients were advised to call doctors on the clinic lines except when there is a pressing health concern that requires a physical presentation of the patient in the clinic. Also, the opinion of a participant revealed that patients are informed to adhere to the COVID-19 precautionary measures whenever they need to be physically present in the clinic. These opinions are encapsulated in the opinions below:
Adherence to the COVID-19 safety protocols through prolonged appointments
They did well before the pandemic, and they answered us on our appointed dates, but since the pandemic started, I’m just coming to see the doctor, it’s over a year already. I’ve been coming in the previous weeks but I was sent back home saying that only when the doctor calls me is when I can come. All these were not there before the pandemic; they kept to their appointments then ((IDI, Participant 18 , Female 80 years). Yes , I am faithful but here , they are not faithful . The staff , attendants and the records officials are not faithful . Sometimes , when I come on my appointment dates , on getting here , they would tell me they have rescheduled my appointment because of COVID-19 (IDI , Participant 10 , Female 45 years) . I didn’t visit the hospital when the pandemic began , but when the hospital was open , I came , and we were told to use our drugs , and I haven’t been able to see the doctor again . It’s been a year I saw a doctor; I just saw the doctor on the first of March this year since all these while . Whenever I have appointments , I use to come , but University College Hospital is not helping matters cause most times I will come , they will say they’ve re-scheduled my appointment many times (IDI , Participant 22 , Female , 72 years) .
One of the diabetes mellitus patients indicated that the COVID-19 precautionary measures were mandatory for all patients in the clinic.
They make sure we use our nose mask, they do temperature checks before you come in, even at the gate, they tell you to put your mask on (IDI, Participants 20 , Male 75 years).
Coping mechanisms adopted by patients with diabetes mellitus
Coping mechanisms emerged as the second theme. The sub-themes were mechanisms adopted by the clinic, coping mechanisms adopted by the patients with diabetes mellitus, reasons for low subscription to telehealth, and dangerous coping mechanisms used by the patients with diabetes mellitus.
Mechanisms adopted by the clinic.
Under this sub-theme, the patients with diabetes mellitus mentioned that the coping mechanisms put in place at the diabetes clinic include the adoption of an online database, provision of avenues to review prescriptions, encouragement of daily monitoring of blood sugar, telehealth, and awareness creation. The following narrative quotes to support this sub-theme;
Now that they’re using technology, things are improving, so little by little, I hope they will do better (IDI, Participants 11 , Female 65 years). They treat me well each time I come. I am always instructed to get an exercise book to write my blood sugar level when I check it every morning and night every day. Once I come to the clinic, I do show the doctor the book. If it is normal, the doctor will not increase my medications, but if it is high, my medications will be increased. That is the way I am attended to (IDI, Participant 12, Female 28 years)
Telehealth.
Participants shared their experiences with the communication services provided by the clinic:
They have call center, they introduced a call center that patients can call and speak to the doctors and nurses, errm I think it’s not 24 hours, but its during working hours (IDI, Participants 17, Male 77 years). I am only aware of the fact that I got a message from the clinic during the early period of the pandemic that I should call some numbers in case an emergency issue arises concerning my health (IDI, Participant 8, Female 52 years).
Coping mechanisms adopted by patients with diabetes mellitus.
The patients utilized positive coping mechanisms such as adherence to preventive measures and reliance on the media for COVID-19 updates. This is captured in the responses below by a number of the participants:
Adherence to the COVID-19 precautionary measures was one of the coping mechanisms the patients with diabetes mellitus adopted in preventing themselves from COVID-19 infection.
They make sure we use our nose mask, they do temperature check before you come in, even at the gate they tell you to put your mask on (IDI, Participants 20 , Male 75 years). I simply follow the laid preventive measures and I keep myself clean in the house’ (IDI , Participant 4 , Female 84 years) . I was just doing what I was supposed to do and didn’t do what i wasn’t supposed to . For example , I have been avoiding crowded places . I have not attended Jumat service since the pandemic began rather , my family and I observe our prayers together at home (IDI , Participant 3 , Male 63 years) .
A couple of the patients with diabetes mellitus relied on the frequent updates on COVID-19 from the mass media as a coping mechanism against the pandemic.
I listened to health programs on the radio and I adhered to their health advices and I also took precautions. It was the precautionary messages and COVID-19 jingles delivered by newscasters on the radio I listened and adhered to (IDI, Participants 8, Female , 52 years).
A few of the participants averred that though they were aware of the telehealth service provided by the clinic, they did not utilize it as a coping mechanism. This is vivid in the opinion of some participants.
During the COVID I received text messages inviting me to come for my check up. But I didn’t come ooo!. But they’re trying (IDI Participants 11, Female 65 years). I didn’t because there was no reason for me to call them ( IDI , Participants 3 , Male 63 years) .
One of the patients opined that they were not aware of the telehealth service provided by the clinic. The provision of the telehealth service was helpful as it came as a timely intervention for some patients who utilized it. This is evident in the response of one of the participants, who opined thus:
Yes during the pandemic when we wanted to see the doctor, we were told to call him on the phone, when I called the doctor I was told the drugs to buy (IDI, Participants 30 , Female 44 years).
Reasons for low subscription to telehealth.
The findings of the study revealed that despite the provision of telehealth service as a coping mechanism, there are however some limitations to its use among patients with diabetes mellitus in University College Hospital.
One of the diabetes mellitus patients opined that he did not use it because a need to utilize the service did not arise. The excerpt below encapsulates this.
I didn’t because there was no reason for me to call them (IDI, Participants 3, Male 63 years)
Also, a level of full awareness regarding telehealth has not been reached among diabetes mellitus patients in the clinic; as such, a few patients did not utilize the service because they were unaware of it.
No, I did not. I wasn’t aware of that service (IDI, Participants 4, Female 84 years). No, I am not aware of it (IDI, Participants 12, Female 28 years).
Dangerous mechanisms employed by patients with diabetes mellitus in the clinic.
The study revealed the employment of negative mechanisms by diabetes mellitus patients in the clinic. This is evident in the excerpts below:
The use of herbal medicines
I used some traditional herbs to also compliment my medications. I drank the juice from boiled mango leaves and ginger. I also took my injections. I stayed indoors and maintain social distancing the few times I go out. Most times even if I feel like going out, my parents will not allow me go out because they know that I am more vulnerable to COVID-19 ( IDI, Participants 12, female, 28 years). I do a lot of steaming , herbal steaming , I cook dongoyaro leaves and the bark , we boil it , and we drink on the first day and subsequent days we just steam . Everybody in my house steams , we use menthol , we add menthol to it and we take a lot of supplements , vitamin C and D , that’s all we’ve done so far ( IDI , Participants 17 , Male 77 years) .
Usage of old prescriptions
I continued buying the drug that was prescribed to me since the last time I came to the clinic. By the time my health deteriorated recently and I have been coming to the clinic, the prescription was changed, but I was already used to my old prescription (IDI, Participant 12, Female, 28 years).
Inconsistency in clinic attendance
Many at times, most of us do not come to the clinic because we do not have money (IDI, Participant 9, Male 21 years).
Suggested coping mechanisms for the management of the University college hospital clinic and the government.
The patients with diabetes mellitus gave some recommendations on how the management of the University College Hospital Diabetes Clinic and the government can assist in easing the stressful conditions of diabetes mellitus patients during the COVID-19 pandemic. They are captured in the excerpts below:
Some participants want their medications to be subsidized and be easy to get.
What I think can be done is….You see, there is a saying that someone who has diabetes and does not want to die early needs money because it is not easy if I would be honest with you. I think what they can do is if they can help us subsidize our drugs. If we are given free drugs once in a while even if it is one drug, it would go a long way. What can be done is if they can help us that way once in a while then if they can help us find means through which our medications will not be scarce to get and they should help us such that it would not be too expensive than what we can bear. See… if it is not too expensive, there is nobody that does not want to use their medications and be healthy but the inability to afford the drugs makes one not to be faithful with the medications. Those are the ways I think they can help us ( IDI, Participant 12, Female 28 years). They can make the drugs cheaper, some can’t afford it and it led to their death(IDI, Participant 18, Female 52years) They should provide free drugs for us . Many at times , most of us do not come to the clinic because we do not have money ( IDI , Participant 9 , Male 21 years) .
Some patients with diabetes mellitus mentioned that the consultation fees should be reduced and this is captured in the narratives below.
One thing they can do is to reduce the consultation fees. Sometimes after paying the money, there won’t be anything left anymore. And sometimes, if we pay and the doctor is not around, the hospital won’t refund the money; that one is gone ( IDI, Participants 30, Female 44 years). We are not equal and not all buoyant . The consultation fee can be reduced and some things can be given for free , even if it is a few drugs ( IDI , Participants 13 , Female 49 years) .
Reduction of waiting time was one of the recommendations suggested by patients with diabetes for the management of University College Hospital. This is supported by the quote below;
Ah the major thing is that they should answer us in time. I understand that they will first do ward round but immediately they come back they should answer us ( IDI, Participants 11, Female 65 years).
One of the participants opined that there should be continuous or regular meetings which can be held in an open space within the clinic in other for them to be updated on their next line of action such as receiving medications, medication review, and adherence to COVID-19 protocols. The except below summarises this assertion.
We have an association but University College Hospital is not allowing us to hold meetings now, and its affecting a lot, through the association, we have had numerous lectures from physiotherapist and dieticians, to teach us more about our condition but our venue is small and due to COVID-19 regulations, those meetings can’t hold but we have pleaded with the management to allow us to do it outside in the open. Because the absence of those meetings is affecting some of us who have no clue as to go about something regarding our ailment ( IDI, Participants 26, Female 68 years).
Other suggested coping mechanisms include: opening more call lines to ensure efficient telehealth services, ensuring patients are treated politely in the clinic, and provision of hygienic toilet facilities.
This study explored the perception and coping mechanisms employed by patients with diabetes mellitus during the COVID-19 pandemic. We found that most participants were not fearful due to the pandemic; rather, they were optimistic while they played their part in ensuring they were safe. This is consistent with the findings of a study conducted in India [ 20 ], which revealed that most of the participants in their study were not so anxious about the pandemic but were rather optimistic. Also, the participants in this study demonstrated a clear understanding of those vulnerable to COVID-19, as some posited that anybody who defies the COVID-19 precautionary measures, people with underlying diseases such as diabetes, are susceptible to the virus. This attests to the supposition that COVID-19 sensitization and training were done in communities and health facilities. Also, surveillance mechanisms were improved in communities in Nigeria [ 20 ].
Literature has revealed that some health facilities had to shut down the entire clinic, including diabetes outpatients, to protect the health care providers and patients from contracting the virus [ 21 ]. Similarly, our findings show that the vulnerable nature of the patients informed why all appointments in the University College Hospital diabetes clinic were cancelled during the early period of the pandemic, after which they were rescheduled till January 2021. Furthermore, our study confirms compliance with WHO’s [ 4 ] recommendation on the use of telemedicine in other to bridge the health access gap caused by the pandemic. Hence, the physical presentation of patients during the pandemic was only encouraged when necessary. However, the study also revealed that patients who attend the diabetes clinic have been adhering to the COVID-19 precautionary protocols such as wearing masks and social distancing most especially when they attend the clinic since it reopened.
Contrary to the assertion made by Ahmed [ 5 ] that most of the public hospitals have been converted to COVID-19 treatment centers, which made lots of patients with comorbidities stranded when they needed medical attention, this study found that the University College Hospital diabetes clinic was only closed during the early period of the pandemic in order to ensure the safety of its staff and patients. In addition, the study revealed that the patients were not left stranded by the clinic as telehealth was provided as an alternative was provided. Patients also had access to healthcare personnel on an appointment basis after the clinic reopened in January 2021. Interestingly, the study revealed that patients were encouraged by the clinic to monitor their blood glucose daily by keeping records of it in a book. Another measure instituted was reducing the crowd in the outpatient clinic by extending patients’ appointment dates. This had the negative effect of limiting access to healthcare personnel during the pandemic. As a result, many patients with diabetes have had their routine screening deferred [ 11 ].
The findings of this study revealed that COVID-19 precautionary measures were strictly adhered to in the clinic, and patients have been compliant. This is, therefore, consistent with the recommendations of the WHO that preventive measures such as social distancing, the use of masks, and hand sanitisers should be adhered to [ 4 ]. Awareness of the availability of the telehealth service was high among the participants. However, awareness goes beyond knowing that a service exists. It is concerned with understanding and utilizing that knowledge [ 22 ].
Contrary to the findings of Hartmann-Boyce [ 23 ], which showed that many patients could not utilize the telehealth service because of their inability to afford the equipment needed for the process, findings from the in-depth interviews revealed that most patients did not utilize telehealth because they did not have reasons to use it. However, very few participants who claimed to utilize the service in this study reported that it was helpful.
The religious nature of Nigerian society is evident in the findings of this study, as most of the participants found succor from the worries and fears of the pandemic in the “Supreme Being”. This is consistent with the supposition that most patients with diabetes eased their fear during the pandemic by trusting the divine being and seeking supernatural protection from the same [ 24 ]. Reliance on the media for sensitization and updates on the pandemic was noted in the study. This affirms the views of Effiong et al. [ 25 ] in Nigeria, where the media was utilized to disseminate messages to the masses on how the virus can be spread and how it can be prevented. Some patients coped by being regular on their medications. This finding is consistent with similar studies [ 26 , 27 ], as it also revealed that some patients with diabetes in University College Hospital were able to cope when the clinic was closed during the early period of the pandemic by using their last prescriptions before the pandemic to procure more drugs.
Furthermore, the use of traditional herbs alongside medications was shown in the study. This is consistent with the findings from the key informant interviews. This confirms that most non-COVID-19 patients relied more on local medications and homemade remedies to cater for their health during the pandemic [ 28 ]. Evidence shows that the burden of diabetes management is more on patients with diabetes mellitus in Nigeria, as about 74.5% of the health care expenditure is self-financed by patients while the government provides only 25.5% [ 29 ]. This study found that interventions such as subsidisation, availability of drugs, and reduction of consultation fees would help patients cope better during the pandemic. In addition, approval of the resumption of the University College Hospital diabetes association meeting, shortening waiting time in clinics, creation of more call lines, polite treatment of patients, increased sensitization, and the provision of hygienic toilet facilities would help alleviate the stress of the pandemic on diabetes patients in University College Hospital.
Strengths and limitations
The study’s main strength is that it examined the perception and coping mechanisms of patients with diabetes mellitus in a tertiary health center during the COVID-19 pandemic. The qualitative nature of the study only permitted a small number of participants in the hospital to be interviewed; therefore, it is important to evaluate our findings carefully before extrapolating them to the entire country.
Implications for public health research
Based on the study’s findings, it is imperative for health professionals to routinely conduct psychological assessments for diabetes mellitus patients. Also, the health service managers can design a guidance and assistance programme for patients with diabetes mellitus intended to improve their ability to adopt coping mechanisms.
The study has shown that patients with diabetes mellitus were not fearful of the COVID-19 pandemic despite their status as diabetes mellitus patients. Diabetes mellitus patients were found to be adherent to the COVID-19 precautionary protocols. The health systems’ coping mechanisms to avert the pandemic’s negative implications were telehealth, encouragement of daily monitoring of sugar levels, and the provision of avenues for a medication review. Additionally, the patients relied on mass media advice and adherence to safety protocols to cope with COVID-19. Based on the study’s outcomes, the government and other healthcare stakeholders must reinforce the resilience of diabetes mellitus patients by alleviating their health burdens during the pandemic. This could be done by subsidizing the prices of drugs, tests, and consultation fees, improving the waiting and appointment system in the clinic, creating an online presence for the University College Hospital Diabetes Association Office, and employing more health personnel in the clinic.
Supporting information
S1 checklist. strengthening the reporting of observational studies in epidemiology statement checklist..
https://doi.org/10.1371/journal.pone.0309451.s001
S1 File. Study questionnaire.
https://doi.org/10.1371/journal.pone.0309451.s002
Acknowledgments
The authors express their appreciation to the University College Hospital, Ibadan, for the privilege of conducting the study within its diabetes clinic. We also thank everyone for their various contributions and assistance during the study.
- 1. Organization WH. Global report on diabetes: World Health Organization; 2016.
- 2. Organization WH. Diabetes 2022 [3rd November, 2022]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/ .
- 3. Programme UND. The Impact of the COVID-19 Pandemic in Nigeria: A Socio-Economic Analysis 2020 [4th November, 2022].
- 4. Organization WH. Rapid assessment of continuity of essential health services (EHS) during the COVID-19 pandemic 2020 [3rd November, 2022].
- View Article
- Google Scholar
- PubMed/NCBI
- 17. (NCDC). NCfDCaP. NCDC COVID-19 report dashboard 2020 [cited 2020 July 1, 2020]. Available from: https://covid19.ncdc.gov.ng/ .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Med Princ Pract
- v.30(2); 2021 Apr

Management of Type 2 Diabetes: Current Strategies, Unfocussed Aspects, Challenges, and Alternatives
Swapnil p. borse.
a AYUSH-Center of Excellence, Center for Complementary and Integrative Health (CCIH), Interdisciplinary School of Health Sciences, Savitribai Phule Pune University (SPPU), Pune, India
b Department of Pharmacology and Toxicology, B. V. Patel Pharmaceutical Education and Research Development (PERD) Centre, Thaltej, India
Abu Sufiyan Chhipa
c Institute of Pharmacy, Nirma University, Ahmedabad, India
Vipin Sharma
d Translational Health Science and Technology Institute, Faridabad, India
Devendra Pratap Singh
e Sun Pharmaceutical Industries Ltd., Vadodara, India
Manish Nivsarkar
Type 2 diabetes mellitus (T2DM) accounts for >90% of the cases of diabetes in adults. Resistance to insulin action is the major cause that leads to chronic hyperglycemia in diabetic patients. T2DM is the consequence of activation of multiple pathways and factors involved in insulin resistance and β-cell dysfunction. Also, the etiology of T2DM involves the complex interplay between genetics and environmental factors. This interplay can be governed efficiently by lifestyle modifications to achieve better management of diabetes. The present review aims at discussing the major factors involved in the development of T2DM that remain unfocussed during the anti-diabetic therapy. The review also focuses on lifestyle modifications that are warranted for the successful management of T2DM. In addition, it attempts to explain flaws in current strategies to combat diabetes. The employability of phytoconstituents as multitargeting molecules and their potential use as effective therapeutic adjuvants to first line hypoglycemic agents to prevent side effects caused by the synthetic drugs are also discussed.
- Type 2 diabetes is a multifactorial disorder that leads to a disturbed glucose homeostasis.
- Lifestyle management along with pharmacological approaches is crucial to achieve a successful management of diabetes.
- Complex interplays between genetics and environmental factors play important roles in the development of diabetes.
- Combinational therapies employed after failure of monotherapy result in comorbidities.
- Phytoconstituents are better alternatives owing to their multitargeting capability.
Introduction
Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [ 1 ]. Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects. However, T2DM is classically viewed as a disorder of insulin deficiency and resistance, and further insights into the pathophysiology of T2DM suggest the role of other key players in insulin deficiency and its functional inability. Pancreatic islets are composed of insulin-releasing β-cells (48–59%), glucagon-releasing α-cells (33–46%), somatostatin (SsT)-releasing δ-cells, and F cells that release polypeptides (PPs) in similar proportion [ 2 ]. Moreover, paracrine interactions occur in the sequence from β-cell to α-cells followed by δ-cells and PP-cells/F-cells [ 3 ]. While the β-cell interactions are emphasized at present, the interaction of other cells in pancreas is of crucial importance that needs to be explored further to understand their roles in glucose homeostasis [ 2 ]. Also, the development of glucose resistance in T2DM is largely influenced by fat cells (accelerated lipolysis), gastrointestinal tract (incretin deficiency/resistance), α-cells (hyperglucagonemia), kidneys (increased glucose reabsorption) and brain (insulin resistance), and complex interactions that occur between these factors and T2DM associated genes [ 4 ]. Changes in the lifestyle of T2DM patients are crucial along with pharmacological interventions to improve the overall health status of the patient. The present review discusses our current understanding of the pathogenesis of T2DM and attempts to emphasize on generally unfocused aspects of T2DM pathogenesis and treatment that may contribute significantly to treatment approaches and patient-related outcomes.
Understanding the Diabetes Machinery: The Unfocused Aspects
Amylin proteins and pancreatic β-cell function.
β-Cells are the most extensively studied pancreatic cells for their roles in glucose homeostasis in T2DM. Islet amyloid PP (amylin) is a β-cell peptide hormone that is secreted along with insulin in the ratio of approximately 100:1. Its secretion is also altered in diabetic patients. Amylin functions as an inhibitor of glucagon secretion and delays gastric emptying thus acting as a satiety agent [ 5 ]. Amylin action is executed through an area postrema (glucose-sensitive part of the brain stem) that collectively aims to reduce the demand of total insulin [ 6 ]. Besides these functions, amylin also plays roles in the destruction of β-cell via the formation of amyloid aggregates and fibers [ 7 ]. Findings from histopathology have shown the accumulation of extracellular amyloid proteins, hyperphosphorylated tau, ubiquitin, apolipoprotein E, apolipoprotein (a), c-Jun N-terminal kinases (JNK1), and islet-brain 1/JNK1 interacting protein-1 (IB1/JIP-1) as the characteristic feature of pancreatic islets in T2DM individuals, suggesting that amylin in association with endocrine system plays important roles in physiology, pathology, and progression of T2DM [ 8 ].
α-Cells
α-cells are known to play crucial roles in the pathophysiology of T2DM. The secretion of glucagon from α-cell is regulated by glucose, hormones, and other substrates that work in unison. Any abnormality in α-cells is reflected in altered glucose homeostasis [ 9 ]. In T2DM, a relative elevated secretion of glucagon takes place in fasting and postprandial states during normal and increased glucose levels along with altered hypoglycemic response [ 10 ]. According to the bi-hormonal hypothesis, T2DM is the consequence of insulin resistance/deficiency with a relative excess glucagon secretion, leading to a rate of hepatic glucose production that is much higher than the rates of glucose utilization. This consequently results in hyperglycemia. The hypothesis is supported by a plethora of clinical and experimental investigations [ 11 , 12 ]. Reduced suppression of glucagon release under hyperglycemic conditions is a contributing factor to postprandial hyperglycemia [ 13 ]. Interestingly, α-cells do not show this behavior in the presence of adequate insulin levels, suggesting that impairment in insulin machinery also cause the abnormalities in glucagon release in T2DM [ 14 ]. In addition to this, hypoglycemia is remarkably influenced by glucagon secretion in T2DM patients treated with insulin. In such patients, the secretory response of α-cells to low-glucose concentrations is compromised, which further aggravates the risks of severe hypoglycemia [ 15 ]. The deficiency of glucagon action in response to hypoglycemia is linked with multiple failures in α-cell regulation [ 16 ]. Even in the situation of islet allotransplantation that helps diabetes patients to remain independent to insulin for a long time, the retarded response of α-cell response to hypoglycemia usually remains unaffected, indicating that the procedure does not completely restore the physiological functions of α-cells [ 17 ]. Collectively, defects in α-cell regulation and glucagon secretion lead to defective glucose sensing, loss of β-cell function, and insulin resistance.
δ-Cells, SsT, and Pancreatic PP Cells (F-Cells)
The δ-cells are located in the stomach, intestine, neuroendocrine cells, and pancreas. They secrete SsT in a pulsatile manner in response to fluctuations in glucose levels [ 18 ]. SsT regulates the endocrine functions and also plays an important role in the gut-brain axis. The receptors of SsT are present on α- and β-cells where they act as inhibitory receptors for the secretion of insulin and glucagon. SsT exerts a tonic inhibitory effect on the secretion of insulin and glucagon and facilitates the islet response to cholinergic activation. In addition, SsT is also involved in the suppression of nutrient-induced glucagon secretion [ 19 ]. Further, SsT significantly alters the normal glucose homeostasis and feedback loops [ 20 ].
F-cells of the pancreas release pancreatic PP after the food intake. It exerts inhibitory postprandial effects on gastric emptying, intestinal motility, exocrine pancreatic secretion, hepatic glucose production, and gallbladder contraction. Functional abilities of PP significantly affect food intake and energy metabolism [ 21 ]. When administered through intracerebroventricular route, PP exerts an orexigenic (appetite stimulating) effect in the brain. On contrary, intraperitoneal administration of PP reduces the food intake and lowers body weight by enhancing energy expenditure [ 22 , 23 ]. Increased plasma levels of PP are implicated in obesity and diabetes.
Adipose Tissue and Resistin
Adipose tissue consists of adipocytes, connective tissue matrix, nerve tissue, stromovascular cells, and immune cells. The role of adipose tissue as an endocrine organ is well established [ 24 ]. It releases leptin, cytokines, adiponectin, complement components, plasminogen activator inhibitor-1, proteins of the renin-angiotensin system, and resistin. Apart from secreting factors/hormones, adipose tissue also functions in coordination with other hormone systems and the central nervous system. Typically, adipose tissues serve as a store house for fat under normal conditions, while they also release free fatty acids (FFAs) in metabolic disorders. Consistent decline in the function of β-cell in normal individuals has been shown to be associated with progressive secretion of FFAs and insulin resistance in adipose tissue [ 25 ]. Resistin or adipose tissue-specific secretory factor released from adipose tissue is largely implicated in the progression and development of T2DM [ 24 ]. It acts as an inhibitory hormone that causes resistance to insulin [ 26 ]. Levels of circulating resistin increase in T2DM, resulting in oxidative stress, insulin resistance, and platelet activation [ 27 ]. Expression of the resistin gene is also observed in the pancreatic islets, pituitary, and hypothalamus [ 28 ]. Although resistin is primarily secreted by macrophages in humans [ 29 ] where it is involved in the recruitment of immune cells and pro-inflammatory factors, the involvement of resistin is also seen in hyperglycemia and insulin resistance [ 30 , 31 ]. Resistin-induced hyperglycemia and obesity are induced through the activation of AMP-protein kinase and decreased expression of gluconeogenic enzymes in the liver. Induction of insulin resistance is also evident in rodents after the administration of recombinant resistin that reverses with the immune neutralization [ 32 ].
T2DM is notorious for being “the geneticist's nightmare.” Occurring due to the combined contribution of genetic and environmental factors, leading to multiple gene alterations [ 33 ]. Multiple mechanisms act either directly or in association with other factors to influence the development and progression of T2DM. These include defects in pancreatic angiogenesis, innervation, and modification of parental imprinting [ 34 ]. The pathogenesis of T2DM depends on the intensity of both maternal and paternal insulin resistivity and/or insulin sensitivity [ 35 ]. According to one study, the first-degree relatives of T2DM patients live at a higher risk of developing T2DM and have a strong genetic predisposition to β-cell failure [ 36 ]. Moreover, β-cell dysfunction, autosomal dominance, and heterozygous mutations in β-cell transcription factors are some of the major causes leading to early onset of T2DM. The identified genes responsible for the early-onset T2DM include insulin promoter factor-1, hepatocyte nuclear factor (HNF)-4α, NeuroD1/BETA2, HNF-1α, and HNF-1β [ 37 ]. A hyperglycemic intrauterine environment has also been implicated in T2DM or pre-diabetes in the offspring of women suffering from gestational diabetes [ 38 ]. Also, during gestational diabetes, the expression of insulin receptor-β, PI3K (phosphatidylinositol 3-kinase) with its subunit p85α and GLUT-4 decreases with a compensatory elevation in the expression of GLUT-1 mRNA in placental tissues [ 39 ]. Polymorphism in resistin gene 299 (G>A) and increase in serum resistin is also known to be a contributing factor to increased insulin resistance with a subsequent higher risk of T2DM in offspring. Moreover, offspring carrying AA and combined GA + AA genotypes tend to be at higher risk [ 40 ]. On the other hand, diabetes also has the capacity to make genetic alterations leading to associated comorbidities. For instance, alterations in genes involved in vitamin synthesis leads to lowering of levels of riboflavin and glycemia, microalbumineria, and altered levels of uric acid in T2DM individuals and development of insulin resistance due to vitamin D deficiency [ 41 , 42 , 43 , 44 , 45 , 46 ]. Importantly, the genes of vitamin D receptor and its binding protein along with CYP1α show polymorphisms in diabetics [ 42 , 43 , 44 ].
The gut serves as a prominent link between the brain and the enteric nervous system [ 47 ]. The secretion of gastrointestinal hormones (incretin, glucagon-like peptide-1 [GLP-1], and glucose-dependent insulinotropic polypeptide [GIP]) increases after food intake. These hormones assist insulin and glucagon in maintaining glucose homeostasis and improve α-cell glucose sensing. GLP-1 promotes assimilation of ingested nutrients through glucose-stimulated insulin secretion and evidently improves β-cell sensitivity to glucose [ 48 ]. Moreover, GLP-1 also suppresses glucose-dependent glucagon secretion, retards gastric emptying, and promotes satiety [ 49 ]. In the pancreas, β-cell proliferation and inhibition of apoptosis are promoted by GIP and GLP-1 that ultimately expand pancreatic β-cell mass. In addition, fat deposition is also facilitated by GIP. In the brain, GIP and GLP-1 are involved in appetite control. GIP also decreases gastric acid secretion, while GLP-1 decreases the duration of gastric emptying. Moreover, the insulinotropic effects of GIP and GLP-1 differ in T2DM patients such that GLP-1 secretion is impaired, while the secretion of GIP remains unaffected [ 50 ]. Alterations in incretin functioning and the associated pathways result in increased gastrointestinal permeability in T2DM and form one of the basic underlying mechanisms responsible for diabetic comorbidities in the latter phase [ 48 , 49 , 51 ].
The gut also releases other hormones which are involved in multiple signaling cascades. These include (but not limited to) ghrelin, galanin, cholecystokinin (CCK or pancreozymin) and leptin [ 52 ]. The enteroendocrine cells (I cells of the duodenum and jejunum) and neurons synthesize and release CCK in response to meals and induce pancreatic acinar cells to secrete pancreatic digestive enzymes. CCK also reduces gastric emptying and enhances the digestion process [ 53 ]. Vagus stimulation causes trypsin release from pancreas that hydrolyzes CCK to maintain homeostasis through the feedback mechanism. CCK is positively associated with leptin and insulin levels resulting in disrupted glucose homeostasis and diabetic complications in T2DM [ 53 , 54 ].
Gut Microbiota
Diabetes is considered as a disease of the intestine where gut microbiota plays a crucial role [ 55 , 56 ]. The concentration of microflora distally increases along the length of the gastrointestinal tract [ 57 ]. The flora of the upper intestine generally accounts for <10 5 cfu/mL of the total microflora content. The concentration of microflora increases in the mid-ileum to 10 7 cfu/mL and ultimately populates the colon heavily [ 57 , 58 ]. Commonly populating bacteria in humans are (a) Firmicutes (60–80%): Ruminiococcus , Clostridium , and Lactobacillus ; (b) Bacteroidetes (20–30%): Bacteroides , Prevotella , and Xylanibacter ; (c) Actinobacteria (<10%): Bifidobacterium ; (d) Proteobacteria (<1%): Escherichia and Enterobacteriaceae ; and (e) yeast Saccharomyces boulardi [ 59 ]. Obesity/adiposity is undoubtedly a pivotal contributing factor in T2DM. Interestingly, the level of Staphylococcus , Enterobacteriaceae , Faecalibacterium prausnitzii , and E. coli increases during obese conditions, while Bacteroides concentration decreases [ 60 ]. Moreover, in T2DM, Firmicutes , Lactobacillus gasseri , Streptococcus mutans , and E. coli are increased, while proteobacteria, butyrate-producing bacteria, Bacteroidetes , Roseburia , Eubacterium halii , and Faecalibacterium prauznitzii are decreased considerably [ 59 ]. Changes in gut microbiota/gut-brain microbiota result in insulin resistance and disease/metabolic syndrome [ 59 , 61 ]. Also, low-grade inflammation is remarkably influenced by obesity in association with alteration of gut-brain-microbiota interactions that render T2DM as an inflammatory disorder [ 62 ]. An increased intestinal permeability due to inflammation is evident in obesity and diabetes that may reach to leak gut conditions to facilitate the entry of gut microbes into circulation. This increases circulating LPS and thereby activates inflammasome formation [ 63 ]. Moreover, vagal control is significantly compromised in diabetes in association with chronic hyperglycemia, damaged interstitial cells of Cajal and gastroparesis (5–12% diabetic patients) [ 64 ]. Increase in mucosal surface area, intestinal weight, and number of goblet cells per villus leads to disrupted esophagus peristalsis and lower sphincter tone [ 65 ]. The overall disturbances in intestinal motor functions lead to stasis and bacterial outgrowth; thus, possibly disturbing the intestinal barrier and affecting permeability to allow the entry of microbes [ 63 , 64 , 65 ]. Moreover, circulating LPS are involved in the insulin resistance and diabetes progression toward comorbidities [ 63 , 65 , 66 ]. Gut microbes influence the metabolic and immune networks of the host to cause obesity and diabetes through enhanced nutrient absorption from the diet, cellular uptake of circulating triglycerides, prolonged intestinal transit time, altered bile acid enterohepatic cycle, enhanced de novo lipogenesis, reduced FFA oxidation, altered tissue composition of biologically active polyunsaturated fatty acid, chronic low-grade inflammation triggered by the endotoxin TLR-4 axis, and altered intestinal barrier function [ 67 ].
Lifestyle Modifications, Environmental Factors, and Management of T2DM
The pharmacological approach to treat T2DM can be only partly effective in the long-term management of diabetes. Major modifications in the lifestyle of patients along with the interventions through pharmacological approaches are crucial to ensure an effective management of the disease. These include changes in physical activity, dietary modifications, management of stress or associated factors, and improved sleeping patterns. The next few sections of this review will discuss and explore the potential of these factors in the management of diabetes when followed in parallel with the pharmacological management of the disease.
Physical Activity
Physical activity is positively associated with controlled glycemic levels among T2DM patients. Moderate but daily physical activity has been found to be an effective way to control the long-term manifestations of diabetes. These include walking, gardening, and performing common household chores. Walking is the most effective physical activity in T2DM, as it allows significant glycemic control with limited physical burden in patients who are already physically weak [ 68 ]. Moreover, a much warranted lifestyle alteration in T2DM patients are changes in sedentary patterns. Sedentary behavior leads to considerably low expenditure of energy. An extended sedentary period in T2DM patients is also associated with uncontrolled glycemic levels. A reduced sedentary time, therefore, is crucial in diabetes patients, which can be achieved by increasing the physical work [ 69 ]. In addition, regular aerobic exercise is acknowledged to improve HbA1c levels in patients with diabetes [ 70 ]. Aerobic exercise tends to improve health outcomes in patients through multiple mechanisms that include the manifold increase in mitochondrial densities, improved sensitivity to insulin, improved compliance of blood vessels, and lung functions with enhanced cardiac output [ 71 ].
Dietary Changes and Medical Nutrition Therapy
Insulin resistance and subsequent appearance of T2DM are closely linked with high intake of sugars, fried food, and red meat [ 72 ]. On the contrary, reduced risk of T2DM development is observed in case of intake of vegetables having high content of antioxidants, fiber, and other nutrients [ 73 , 74 ]. The average energy intake of diabetes patients differs with their obesity status. Usually, for a nonobese diabetic patient, an average energy intake of 1,500–2,500 calories per day is recommended, while for obese patients, the average calorie intake is reduced to 800–1,500 calories per day. Limited intake of refined sugars is highly recommended in T2DM patients. Non-nutritive sweeteners (aspartame, saccharine, etc.) can be the good substitutes for sugar in such patients. Moreover, the restricted intake of food rich in saturated fats and cholesterol and its replacement with food rich in polysaturated fats is also recommended. In addition, changes in eating patterns, such as dividing meals into small fractions over the day rather than taking 1 or 2 large meals can prevent vigorous postprandial peaks in blood glucose levels [ 75 ]. Strict adherence to controlled diet with sufficient physical activity is largely associated with lower incidence of diabetes [ 76 ]. Incorporation of Paleolithic diet (a diet rich in lean meat, fish, fruits, and vegetables) in the daily routine of diabetic patients results in marked improvement in glucose handling [ 77 ]. The employment of nutritional therapy in the management of diabetes is also widely suggested. Nutritional therapy is an approach to treat a disease through the modifications in food and nutrition intake. The application of evidence-based nutrition care therapy in diseased patients by a qualified and registered dietician is termed as medical nutrition therapy [ 78 ]. Reduced reliance on oral hypoglycemic therapy is evident in diabetes patients receiving nutritional therapy [ 79 ]. Also, considerable improvements in clinical outcomes are observed in diabetes patients receiving intensive nutritional education by registered dietician in comparison to patients receiving basic nutrition information (BE) [ 80 ]. Taken together, simple but profound changes in dietary pattern in diabetic patients is a potential approach to curb the long-term implications of diabetes. Moreover, successful application of nutritional therapy in individuals with diabetic conditions can be a lucrative approach to achieve a better management of diabetes with improved health outcomes.
Increased levels of stress are associated with poor treatment adherence and glycemic control in T2DM patients [ 81 ]. In a longitudinal study, moderate/high levels of stress were found to be accountable for multifold increase in the incidences of diabetes [ 82 ]. Moreover, consistent exposure to stressors, compromised mental health, and psychological stress are highly implicated in increasing risk of T2DM development [ 83 ]. Allostatic load (wear and tear in the body occurring as a result of chronic exposure to psychological stress) is assumed to be the major factor responsible for this increased risk of T2DM in such individuals [ 84 ]. In addition, consistent stress is also implicated in worsening of clinical outcomes in T2DM patients. Chronic stress is associated with dysregulated glucose metabolism and neuroendocrine function accompanied with low-grade inflammation. A majority of factors that are implicated in T2DM are largely influenced by psychological stress including the release of glucose (and lipids) in circulation, expression of inflammatory cytokines, and elevated blood pressure [ 85 ]. In one study, in type 2 diabetes patients when exposed to acute stress during the postprandial period, considerable increases in blood glucose levels were observed [ 86 ]. Apparently, treatment strategies, including stress management interventions, are a promising approach in effectively preventing or controlling the incidence of type 2 diabetes.
Sleep Patterns and Chronopharmacology
Although physical activity and maintained dietary pattern result in considerable improvements in the management of T2DM, they cannot be envisioned as the sole contributors to the worsening of diabetes incidences. Sleep is another modifiable lifestyle behavior that has proven roles in influencing metabolic health and energy status. Optimization of sleeping patterns is crucial in diabetes control [ 87 ]. A population-based study suggests that short sleep (<5 h) or insomnia is associated with increased risk of T2DM [ 88 ]. In similar studies, poor sleep was associated with higher HbA1c levels (>7%) and insulin resistance in T2DM patients [ 88 ]. Disturbed circadian rhythms and sleep-wake patterns also result in significant effect on onset, development, and management of diabetes [ 89 ]. Shift workers tend to remain much prone to metabolic disorders due to consistent sleep loss and disrupted circadian rhythm [ 90 ]. In addition, developed propensity of napping as a consequence of poor or insufficient nocturnal sleep is also associated with high risk of T2DM [ 91 ]. In one study, experimental manipulation of sleep and circadian pattern resulted in significant reduction in insulin response to standardized meal which could be recovered with restored sleeping patterns [ 92 ]. Changes in hormones that regulate appetite (leptin and ghrelin) are observed to be associated with short sleep causing an increased urge for carbohydrate-rich food and increased calorie intake [ 89 , 93 ]. Moreover, lack of sleep also results in oxidative stress and release of orexin or hypocretin, a neuropeptide that regulates sleep and appetite and causes the stimulation of sympathetic nervous system and increased release of cortisol with simultaneous decrease in growth hormone secretion, all leading to considerable hyperglycemia [ 89 , 94 ].
Pharmacokinetics and pharmacodynamics (PK-PD) are markedly influenced by daily rhythms in physiology. This phenomenon is termed chronopharmacology [ 95 ]. Indeed, the pathogenesis of diabetes largely depends on hormonal and body homeostasis. Chronopharmacology should be considered as part of treatment strategies for diabetes. The failing β-cells in T2DM do not lose all their capability to respond to glucose. Insulin secretion in response to stimulation through amino acids or other hormones such as glucagon-like peptide 1 (GLP-1), remains preserved [ 96 ]. The levels of leptin (satiety hormone) in blood generally remain higher between midnight and early morning, conceivably to suppress appetite during the night [ 97 ]. Moreover, the levels of ghrelin increase with increase in the duration of sleep [ 93 ]. In addition, the time dependency in GLUT4-mediated glucose uptake is also a function of circadian variation [ 98 ]. Furthermore, meal timings can modify the diurnal rhythm of blood leptin levels [ 99 ]. Both ghrelin and leptin work with other hormones and HPA axis through feedback loops to indirectly affect the psychophysiological satisfaction in diabetic patients [ 100 ]. Chronopharmacology, therefore, may considerably affect diabetic pathophysiology and PK-PD of administered drugs.
Interplay of Genetics, Gut Microbiota, Lifestyle, and Environmental Factors
Multiple epidemiological investigations have suggested that the effects of multiple T2DM-associated loci can be attenuated by improving lifestyle, dietary patterns, and other associated environmental factors. For instance, the Ala12 variant of PPARγ is associated with improved insulin sensitivity. Apparently, the Ala12 carriers are more responsive to unsaturated fat and less responsive to saturated fat. On contrary, the Pro12 variant carriers of PPARγ are more responsive to the deleterious effects of saturated fat and altered glucose homeostasis. Seemingly, unsaturated fat interacts with PPARγ Ala12 variant and upregulates the activity of latter [ 101 ]. Potential gene-environment (G × E) interactions also occur between TCF7L2 risk-variant (rs7903146) and lifestyle modifications (physical activity, MNT, and dietary changes). Decreased insulin resistance and reduced risk in TCF7L2 risk-variant carriers is significantly affected by lifestyle modifications [ 102 , 103 ]. A common SNP in fat mass and obesity associated gene (FTO rs9939609) is associated with increased risk of T2DM. Increased physical activity reduces the FTO rs9939609-induced obesity and associated risk of T2DM [ 104 ]. SNP in glucokinase regulatory protein gene results in an insulin-raising allele, GCKRrs780094. Its interaction with the whole grain (increased whole grain intake) results in reduced fasting insulin in the carriers [ 105 ]. The potassium voltage-gated channel subfamily Q member 1 (KCNQ1) is a susceptible gene in T2DM. Mutations in KCNQ1 are associated with decreased insulin secretion. Reduced expression of noncoding RNA Kcnq1ot1 in Kcnq1 genetic region leads to increase in cyclin-dependent kinase inhibitor 1C (Cdkn1c) expression, resulting in reduced pancreatic β-cell mass and insulin release. The CCAAT sequence in the promoter region of Cdkn1c gene serves as the binding site for transcription factor C/EBP that increases the further expression of Cdkn1c. Evidently, the expression of C/EBPβ results in endoplasmic reticulum stress to cause dysfunctions in β-cells. The accumulation of C/EBPβ in pancreatic β-cells increases in the presence of high fat diet, thereby potentiating the β-cells dysfunction in the vulnerable population [ 106 ]. Collectively, the emerging investigations to explore the interactions between gene and environmental factors suggest a high influence of dietary patterns, physical exercise, and other lifestyle interventions on the expression of genes that are peculiar to the development of T2DM.
Apart from gene expression, environmental factors also tend to exert a potential impact on gut microbiota. The gut environment is affected by a number of factors including the diet, pH, and nutrient absorption. While the presence of Firmicutes and Proteobacteria increases under the influence of carbohydrates and simple sugar-rich diet, saturated fats, and animal protein-rich diet encourages the proliferation of Bacteroidetes and Actinobacteria [ 107 ]. Moreover, a high −at diet is also accountable for significant alterations in intestinal flora, including the Bifidobacterium and Bacteroides (increased Gram-negative/Gram-positive bacteria ratio). This allowed and increased secretion of LPS, fat content, body weight, and inflammatory reactions associated with T2DM [ 108 ]. Reduction in butyrate is largely responsible for the loss of tight intestinal barrier. An intestinal pH of 5.5 favors the proliferation of butyrate-producing Phytophthora which starts to diminish with a pH value of 6.5 [ 109 ]. In addition, the hypoglycemic agents utilized for the antidiabetic therapy also pose a remarkable influence on the gut microbiota. Metformin and acarbose are known to increase the proliferation of lactobacilli, Akkermansia, and several other bacteria that are acknowledged to exert beneficial effects in diabetes [ 110 ].
Gut microbiota composition also affects the regulation of expression of different genes in T2DM. Although reports are limited in terms of potential interactions between gut microbes and T2DM associated gene variants, existing reports on the influence of gut microbes in the expression genes that are crucial in T2DM are highly suggestive of a complex gene-microbes interplay in the etiology of T2DM. Also, microbiome plays a crucial role in the epigenetic regulation of genes by the modification of DNA methylation [ 111 ]. F. prausnitzii , a short-chain fatty acid-producing bacteria was found crucial in epigenetic regulation of FFA receptor gene in patients of T2DM. A significant reduced presence of F. prausnitzii was evident in such patients. As a result, a considerably low methylation in the promoter region of FFA receptor gene is observed in these individuals [ 112 ]. Increased release of pro-inflammatory cytokines is a key event in T2DM. Microbes are largely known to be associated with increased release of inflammatory cytokines by producing the products such as LPS that promote low-grade inflammation and endotoxemia. On contrary, several microbes are known to induce the expression of anti-inflammatory cytokines, including the IL-10 and IL-22, that have proven roles in improving the insulin sensitivity Roseburia intestinalis , Bacteroides fragilis , Akkermansia muciniphila , Lactobacillus plantarum , and Lactobacillus casei [ 113 ]. Two other beneficial microbes − Bacteroides vulgatus and Bacteroides dorei − are observed to increase the expression of tight junction genes in T2DM to compensate with the compromised gut permeability (leaky gut) [ 114 ]. A major contribution of probiotics is observed in the case of glucose metabolism and homeostasis. For instance, L. gasseri BNR17 is known to increase the expression of GLUT-4 transporter gene [ 115 ]. Another gut microbe, L. casei is witnessed to increase the expression of multiple T2DM-related genes, including ClC1-7, GlyRα1, SLC26A3, SLC26A6, GABAAα1, Bestrophin-3, and CFTR, thus resulting in a significant reduction in hyperglycemia [ 116 ]. It appears to be of vital importance to consider the potential interplay between various T2DM-related genes and these microbes. Undoubtedly, the absence of these microbes among the gut microbiota can be largely responsible for the altered regulation of different genes in T2DM patients. Also, exploring the interactions between different T2DM-associated gene variants and gut microbiota is warranted to further understand the complex interactions between environmental factors, gut microbiota, and genetics in the development of T2DM.
Current Approaches for Diabetes Management: What Are We Missing?
The guidelines for the pharmacological management of diabetes provided by American Diabetes Association suggest that metformin be prescribed as the initial intervention to T2DM patients. However, the same guideline also indicates that vitamin B 12 deficiency is a prominent side effect observed in metformin consumers and a periodic vitamin B 12 measurement is required in such patients [ 117 , 118 ]. Furthermore, metformin is also notorious for causing lactic acidosis, especially in patients with kidney disease, liver injury, or other CVS complications that create a low level of oxygen in circulation [ 119 ]. For T2DM patients with cardiovascular or CKDs, the guidelines recommend adding sodium-glucose cotransporter 2 (SGTL2) inhibitors and/or glucagon-like peptide 1 receptor agonists along with hypoglycemic agents [ 118 ]. The employability of SGTL2 inhibitors with almost all classes of hypoglycemic agents makes them ideal candidates to be combined when dual and triple combination therapies are warranted [ 120 ]. In an ideal scenario, a drug used in combination should be able to reverse the pathology with an improved overall health status of the patient and ensure that no new complications arise due to the existing management strategies. In case of T2DM, drug combination should not only be able to just merely reduce the glycosylated hemoglobin levels (HbA1C) but also an improved overall metabolic condition of the patient is expected through such interventions [ 120 ]. The combination of SGTL2 inhibitors with metformin may have proved beneficial in curbing hyperglycemia that cannot be controlled by metformin alone [ 120 ], but the adverse effects associated with the SGTL2 inhibitors still remain unresolved. Genital infections caused by SGTL2 inhibitors due to high glycosuria still remain an unfocussed aspect while prescribing such combinations. In addition, during the event of excessive osmotic diuresis caused by SGTL2 inhibitors, a low extracellular fluid volume and subsequent hypotension is another complication that may arise [ 121 ]. Multiple reports have also raised concerns regarding the use of SGTL2 inhibitors in diabetes due to their substantial involvement in causing diabetic ketoacidosis [ 122 ]. Two separate reports published in 2015 claimed that canagliflozin, an SGTL2 inhibitor is implicated in pancreatitis in T2DM patients [ 123 , 124 ]. GLP-1 agonists are also a preferred class of adjuvant hypoglycemic agents that are combined with first-line hypoglycemics [ 125 ]. Apart from gastrointestinal disorders (nausea, vomiting, and constipation), infections and acute renal injury, a major raising concern regarding the use of GLP-1 agonists is their association with pancreatitis [ 125 , 126 ]. Cases of acute pancreatitis are reported with the use of liraglutide and exenatide [ 127 , 128 ]. More importantly, recent reports also raise concerns regarding the long-term reliance on incretin-based therapies due to frequently reported cases of their association with pancreatitis and pancreatic cancer [ 129 ]. Studies based on FDA Adverse Events Reporting System demonstrated that incretin-based therapies are associated with the increased incidences of pancreatic and thyroid cancer [ 130 , 131 ]. Exenatide use is also positively associated with the incidences of bone fractures [ 132 ].
Alternatives: Phytoconstituents
Failure of monotherapy in diabetes is simply managed by the dual or triple drug combination therapies that involve the addition of supportive hypoglycemic agents with the first-line drugs. However, adding the supportive or second-line drugs in combination seldom includes the assessment of risk factors associated with these new additions. The sole aim of these therapies remains to be a controlled glycemic condition. Unfortunately, in the pursuit of maintaining normal blood glucose levels, the occurrence of new complications is largely taken for granted. Monotherapies supplemented with herbal extracts or phytoconstituents have showed appreciable improvements in the blood glucose levels in diabetic patients. Chemical constituents from plants have also proved to be promising alternatives. Table Table1 1 represents the known effects of different phytoconstituents in diabetes exerted through multiple targets. As a result, unlike in the case of conventional single target therapy where chances of treatment failures are high, therapy failures with multi-targeting approach are rare.
Multiple targets of different phytoconstituents in the management of T2DM and their possible outcomes [133–140]
| Phytoconstituents | Mode of action/targets | Outcomes |
|---|---|---|
| Curcumin | ↓ TNF-α, ↓ NFkB activation, ↓ lipid peroxidation, ↓ lysozyme enzyme activity, and ↑ PPAR-γ activation | Increased insulin sensitivity, decreased glucose intolerance, and hypoglycemia [ ] |
| Rutin | ↓ G6Pase and glycogen phosphorylase activity, ↑ hepatic hexokinase activity, and ↑ PPARγ activation | ↓ Hepatic glucose production, ↑ glucose tolerance, and improved insulin sensitivity [ ] |
| Resveratrol | SIRT1 activation, ↓ oxidative stress, and ↑ GLUT4 translocation through AMPK/Akt/iNOS signaling pathway | Improved insulin signaling, ↑ glucose-mediated insulin secretion, and ↓ loss of β cells [ ] |
| Quercetin | ↑ GLUT4 translocation through AMPK signaling, ↓ G6Pase, and ERK1/2 activation | ↑ Glucose uptake, ↓ hepatic glucose production, glucose-induced insulin secretion, and improves β-cell function [135, 136] |
| Genistein | ↑ Hepatic hexokinase activity, and ↓ cytosolic PEPCK | Improved lipid and glucose metabolism and reduced fasting glucose [ ] |
| Hesperidin | ↑ GLUT4 expression, ↓ TNF-α, and IL-6 expression, ↑ antioxidants | ↑ Glucose uptake, ↓ HbA1c, and ↓ oxidative stress [ ] |
| Naringin | ↑ G6Pase activity, ↑ insulin receptor and GLUT4 expression, and ↑ antioxidants | ↓ Hepatic glucose production, ↑ glucose uptake, and ↓ oxidative stress [ ] |
| Naringenin | ↑ Expression of GLUT4 and PPARγ | ↑ Glucose uptake, decreased glucose intolerance, and reduced blood glucose levels [ ] |
| Vitamins A, D, and E | ↑ PPARβ/δ expression, ↑ RAR expression, ↑ DNA tail length of liver and pancreas, and ↓ G6Pase, ↓ β-cell apoptosis | Decreased glucose intolerance, ↑ β-cell mass, ↓ hepatic glucose, and ↓ hyperglycemia [ ] |
| Fisetin | ↓ G6Pase and ↓ cytosolic PEPCK | ↓ Hepatic glucose and improved lipid and glucose metabolism [ ] |
T2DM, type 2 diabetes mellitus; G6Pase, glucose-6-phosphatase; PEPCK, phosphoenolpyruvate carboxykinase.
Conclusions
Diabetes is a metabolic disorder that is influenced by a variety of factors. Recent insights into the pathogenesis of diabetes have unraveled newer pathways and factors that contribute substantially in disease development and progression. Insulin resistance and β-cell dysfunction are the 2 major events that are largely responsible for the onset of diabetes. A major objective of this review is to focus on the unfocused aspects of diabetes to develop better strategies for diabetes treatment. In this review, we have discussed the factors that have played crucial roles in the etiology of T2DM but have not received adequate attention. We have also discussed the efficiency of existing approaches in the treatment of T2DM. Lifestyle modifications that favor the improvement of management of diabetes and their complex interplays with genetics and gut environment is a crucial factor that warrants further research in the development of more efficient and individualized therapy approaches for disease treatment. The use of multidrug combination therapy in diabetes may have improved health outcomes in T2DM patients and also result in additional complications that need serious consideration. Moreover, more attention is required toward the developing comorbidities during diabetes. The diabetic milieu accelerates the formation of advanced glycation end products that may encourage the development of diabetic complications and even cancer in diabetic patients. Multiple pathways are involved in diabetes that can contribute to the manifestation of comorbidities that are largely neglected during disease treatment.
Multitargeting is a promising approach for the treatment of T2DM as it includes multiple pathways. The failure of single target approaches is the major challenge faced in T2DM treatment. Phytoconstituents are promising as they interact with multiple pathways simultaneously. However, the reluctance to rely on phytoconstituents as the main therapy still remains as a limiting factor for such drugs to serve as mainstream interventions.
Conflict of Interest Statement
All authors have read the journal's policy on disclosure of potential conflicts of interest and have none to declare.
Acknowledgement
The authors are thankful to B. V. Patel Pharmaceutical Education and Research Development (PERD) Center, Ahmedabad, and AYUSH − Center of Excellence, Center for Complimentary and Integrative Health (CCIH), Interdisciplinary School of Health Sciences, Savitribai Phule Pune University, Pune, for providing facilities for the successful completion of the work. The authors are also thankful to those colleagues whose work could not be cited directly owing to space constraints.
Swapnil P. Borse and Abu Sufiyan Chhipa contributed equally; Vipin Sharma and Devendra Pratap Singh contributed equally.

IMAGES
VIDEO
COMMENTS
Different classes of diabetes mellitus, type 1, type 2, gestational diabetes and other types of diabetes mellitus are compared in terms of diagnostic criteria, etiology and genetics. The molecular genetics of diabetes received extensive attention in recent years by many prominent investigators and research groups in the biomedical field.
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575-1585. Crossref. ... Chronicle of Diabetes Research and Practice, 3, 1, ...
Diabetes mellitus is associated with an increased risk of various cancers, especially gastrointestinal cancers and female-specific cancers. Hospitalization and mortality from various infections ...
Latest Inventions in Diabetes Management. In addition to the aforementioned innovations in the management of diabetes, several drugs are still at different stages of clinical trial for eventual use. Others are ready and have been recently introduced into the market. 4.6.1. Drugs Recently Introduced.
Type 1 diabetes mellitus affects 8.5 million people globally and is characterized by autoimmune destruction of pancreatic β cells. ... Research 02 Sept 2024 European Journal of Clinical Nutrition ...
Diabetes remains a substantial public health issue. Type 2 diabetes, which makes up the bulk of diabetes cases, is largely preventable and, in some cases, potentially reversible if identified and managed early in the disease course. However, all evidence indicates that diabetes prevalence is increasing worldwide, primarily due to a rise in obesity caused by multiple factors. Preventing and ...
Pharmacology. Diabetes mellitus. 1. Introduction. Diabetes is a long-term, persistent disease that occurs due to the body's inability to process and regulate blood glucose due to the over-secretion of insulin from the pancreas or the inability of the insulin to regulate the blood glucose levels [1]. Insulin is a polypeptide hormone secreted by ...
Journal of Diabetes Research is an open access journal that publishes articles related to type 1 and type 2 diabetes. Topics include etiology, pathogenesis, management, and prevention of diabetes, as well as associated complications such as nephropathy. As part of Wiley's Forward Series, this journal offers a streamlined, faster publication ...
Abstract: Diabetes mellitus has become a serious and chronic metabolic disorder that results from a complex interaction of genetic and environmental factors, principally characterized by hyperglycemia, polyuria, and polyphagia. Uncontrolled high blood sugar can result in a host of diabetic complications.
Two papers—one global and one focused on the USA—together tell the unhappy and inequitable story of diabetes. By 2045, as many as three in four adults with diabetes will be living in low-income and middle-income countries. Currently, only 10% of people with diabetes living in these countries receive guideline-based diabetes care.
Diabetes mellitus (DM) underscores a rising epidemic orchestrating critical socio-economic burden on countries globally. ... Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches ...
ew decades.GlOBAl BurDENGlobally, an estimated 422 million adults were living with diabetes in 2014, compar. d to 108 million in 1980. The global prevalence (age-standardized) of diabetes has nearly doubled since 1980, rising from 4.7% to 8.5.
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... Research 19 Aug 2024 International Journal of ...
Abstract. Background: Type 2 diabetes (T2D) has long been identified as an incurable chronic disease based on traditional means of treatment. Research now exists that suggests reversal is possible through other means that have only recently been embraced in the guidelines. This narrative review examines the evidence for T2D reversal using each ...
This paper was supported by the National Institute for Health Research (NIHR) Leicester Biomedical Research Centre, and the NIHR Leicester Clinical Research Facility. ... Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009; 58:773-795. Crossref. Scopus (1954 ...
Diabetes publishes original research about the physiology and pathophysiology of diabetes mellitus. Submitted manuscripts can report any aspect of laboratory, animal, or human research. More About Diabetes. Editor in Chief. ... Each month, the Editors of Diabetes select an original research article to designate Paper of the Month. View these ...
Type 1, Type 2, and the Gestational diabetes are the three major types of diabetes mellitus, although there is a collection of other specific types. ... Discover the world's research. 25+ million ...
Introduction. Type 2 Diabetes Mellitus (T2DM) is characterized by a persistently elevated blood glucose, or an elevation of blood glucose after a meal containing carbohydrate ().Unlike Type 1 Diabetes which is characterized by a deficiency of insulin, most individuals affected by T2DM have elevated insulin levels (fasting and/or post glucose ingestion), unless there has been beta cell failure ...
Abstract. Type 2 diabetes accounts for nearly 90% of the approximately 537 million cases of diabetes worldwide. The number affected is increasing rapidly with alarming trends in children and young adults (up to age 40 years). Early detection and proactive management are crucial for prevention and mitigation of microvascular and macrovascular ...
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [1, 2]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
This article provides an overview of the main types and common symptoms of diabetes, its acute and long-term complications and its management. It also outlines the nurse's role in diabetes care, which frequently includes assessing and empowering patients. Keywords: blood glucose; clinical; diabetes; diabetic foot ulcers; diabetic ketoacidosis ...
Background The 2019 coronavirus disease (COVID-19) ushered in a period of fear and uncertainty, resulting in structural instability across the globe. Vulnerable individuals, such as patients with diabetes mellitus, are predispose to have adverse effects and complications of COVID-19 when infected. We explored the perception of diabetes mellitus patients during the COVID-19 pandemic and their ...
Type 2 diabetes mellitus (T2DM) accounts for >90% of the cases of diabetes in adults. Resistance to insulin action is the major cause that leads to chronic hyperglycemia in diabetic patients. ... The authors are thankful to B. V. Patel Pharmaceutical Education and Research Development (PERD) Center, Ahmedabad, and AYUSH − Center of Excellence ...
Diabetic vascular disease is one of the major complications of diabetes mellitus (DM), which includes microvascular and macrovascular diseases. More than half of patients with DM may suffer from diabetic vasculopathy, especially leading to peripheral vascular disease and delayed wound healing ( 1 , 2 ).