An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Gestational diabetes mellitus and macrosomia: a literature review
Affiliation.
- 1 Department of Obstetrics and Gynecology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, PR China.
- PMID: 26045324
- DOI: 10.1159/000371628
Background: Fetal macrosomia, defined as a birth weight ≥ 4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation. As a result, extra glucose in the fetus is stored as body fat causing macrosomia, which is also called 'large for gestational age'. This paper reviews studies that explored the impact of GDM and fetal macrosomia as well as macrosomia-related complications on birth outcomes and offers an evaluation of maternal and fetal health.
Summary: Fetal macrosomia is a common adverse infant outcome of GDM if unrecognized and untreated in time. For the infant, macrosomia increases the risk of shoulder dystocia, clavicle fractures and brachial plexus injury and increases the rate of admissions to the neonatal intensive care unit. For the mother, the risks associated with macrosomia are cesarean delivery, postpartum hemorrhage and vaginal lacerations. Infants of women with GDM are at an increased risk of becoming overweight or obese at a young age (during adolescence) and are more likely to develop type II diabetes later in life. Besides, the findings of several studies that epigenetic alterations of different genes of the fetus of a GDM mother in utero could result in the transgenerational transmission of GDM and type II diabetes are of concern.
PubMed Disclaimer
Similar articles
- Efficacy of maternal and biological parameters at the time of diagnosis of gestational diabetes mellitus in predicting neonatal morbidity. Ducarme G, Desroys Du Roure F, Le Thuaut A, Grange J, Dimet J, Crepin-Delcourt I. Ducarme G, et al. Eur J Obstet Gynecol Reprod Biol. 2018 Feb;221:113-118. doi: 10.1016/j.ejogrb.2017.12.036. Epub 2017 Dec 19. Eur J Obstet Gynecol Reprod Biol. 2018. PMID: 29278829
- Shoulder dystocia: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Sentilhes L, Sénat MV, Boulogne AI, Deneux-Tharaux C, Fuchs F, Legendre G, Le Ray C, Lopez E, Schmitz T, Lejeune-Saada V. Sentilhes L, et al. Eur J Obstet Gynecol Reprod Biol. 2016 Aug;203:156-61. doi: 10.1016/j.ejogrb.2016.05.047. Epub 2016 May 30. Eur J Obstet Gynecol Reprod Biol. 2016. PMID: 27318182 Review.
- Reducing macrosomia-related birth complications in primigravid women: ultrasound- and magnetic resonance imaging-based models. Badr DA, Cannie MM, Kadji C, Kang X, Carlin A, Jani JC. Badr DA, et al. Am J Obstet Gynecol. 2024 May;230(5):557.e1-557.e8. doi: 10.1016/j.ajog.2023.10.011. Epub 2023 Oct 11. Am J Obstet Gynecol. 2024. PMID: 37827273
- Interactive effects of prepregnancy overweight and gestational diabetes on macrosomia and large for gestational age: A population-based prospective cohort in Tianjin, China. Yang W, Liu J, Li J, Liu J, Liu H, Wang Y, Leng J, Wang S, Chen H, Chan JCN, Yu Z, Hu G, Yang X. Yang W, et al. Diabetes Res Clin Pract. 2019 Aug;154:82-89. doi: 10.1016/j.diabres.2019.06.014. Epub 2019 Jul 1. Diabetes Res Clin Pract. 2019. PMID: 31271809
- [Delivery management for the prevention of shoulder dystocia in case of identified risk factors]. Schmitz T. Schmitz T. J Gynecol Obstet Biol Reprod (Paris). 2015 Dec;44(10):1261-71. doi: 10.1016/j.jgyn.2015.09.051. Epub 2015 Nov 1. J Gynecol Obstet Biol Reprod (Paris). 2015. PMID: 26530180 Review. French.
- Impact of a 12-Week Dietary Intervention on Adipose Tissue Metabolic Markers in Overweight Women of Reproductive Age. Erta G, Gersone G, Jurka A, Tretjakovs P. Erta G, et al. Int J Mol Sci. 2024 Aug 4;25(15):8512. doi: 10.3390/ijms25158512. Int J Mol Sci. 2024. PMID: 39126081 Free PMC article. Clinical Trial.
- Risk factors and diagnostic performance of predictors as a screening technique for gestational diabetes mellitus: a retrospective cross-sectional study. Khobrani FM, Alzahrani AM, Binmahfoodh DS, Hemedy RA, Abbas SI. Khobrani FM, et al. Ann Med Surg (Lond). 2024 Jun 14;86(8):4384-4388. doi: 10.1097/MS9.0000000000002247. eCollection 2024 Aug. Ann Med Surg (Lond). 2024. PMID: 39118718 Free PMC article.
- Association of Umbilical Cord Perilipin 2 Levels with Neonatal Anthropometric Measurements in Infants of Diabetic Mothers. Celik K, Ozkan Zarif N, Ozen Kucukcetin I, Arayici S, Kihtir Z, Unver Tuhan H, Ongun H. Celik K, et al. Children (Basel). 2024 Jun 25;11(7):771. doi: 10.3390/children11070771. Children (Basel). 2024. PMID: 39062220 Free PMC article.
- Association of DNA Methylation with Infant Birth Weight in Women with Gestational Diabetes. Saucedo R, Ferreira-Hermosillo A, Robledo-Clemente M, Díaz-Velázquez MF, Valencia-Ortega J. Saucedo R, et al. Metabolites. 2024 Jun 27;14(7):361. doi: 10.3390/metabo14070361. Metabolites. 2024. PMID: 39057684 Free PMC article. Review.
- Predictors of Postpartum Hemorrhage and Associated Outcomes at a Midwest Academic Medical Center. Mooberry M, Voss N, Wendt L, Kenne KA, Jackson JB, Rysavy MB. Mooberry M, et al. Womens Health Rep (New Rochelle). 2024 Apr 26;5(1):358-366. doi: 10.1089/whr.2023.0192. eCollection 2024. Womens Health Rep (New Rochelle). 2024. PMID: 39035139
Publication types
- Search in MeSH
Related information
- PubChem Compound (MeSH Keyword)
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- S. Karger AG, Basel, Switzerland
- Genetic Alliance
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- DOI: 10.1159/000371628
- Corpus ID: 6536421
Gestational Diabetes Mellitus and Macrosomia: A Literature Review
- Kamana Kc , Sumisti Shakya , Huafan Zhang
- Published in Annals of Nutrition and… 1 June 2015
Figures from this paper

675 Citations
Effect of gestational diabetes mellitus on macrosomia infants, macrosomia index in neonates of diabetic mothers as a simple predictor of maternal glycemic control, ultrasonic predictors of macrosomia in gestational diabetes mellitus, new born macrosomia in gestational diabetes mellitus, the management of the macrosomic fetus and the assessment of wellbeing in gestational diabetes mellitus, isfhac as a novel predictor of macrosomia in gestational diabetes mellitus and normal pregnancy, gestational diabetes mellitus: the optimal time of delivery, gestational weight gain as an independent risk factor for macrosomia in women with intermediate state gestational blood glucose., comparison of perinatal complications in macrosomic i̇nfants of diabetic and nondiabetic mothers, fasting plasma glucose and fetal ultrasound predict the occurrence of neonatal macrosomia in gestational diabetes mellitus, 53 references, impending macrosomia: will induction of labor modify the risk of cesarean delivery, the influence of obesity and diabetes on the prevalence of macrosomia., complications associated with the macrosomic fetus., influence of maternal insulin-dependent diabetes mellitus on neonatal morbidity., pregnancy outcome in obese and morbidly obese gestational diabetic women., suspicion and treatment of the macrosomic fetus: a review., diagnosing gestational diabetes, elective delivery of infants with macrosomia in diabetic women: reduced shoulder dystocia versus increased cesarean deliveries., diabetes and obesity in pregnancy., prevalence and outcome of the macrosomic infants, related papers.
Showing 1 through 3 of 0 Related Papers
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Gestational Diabetes Mellitus and Macrosomia: A Literature Review

2015, Annals of Nutrition and Metabolism
Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation. As a result, extra glucose in the fetus is stored as body fat causing macrosomia, which is also called ‘large for gestational age'. This paper reviews studies that explored the impact of GDM and fetal macrosomia as well as macrosomia-related complications on birth outcomes and offers an evaluation of maternal and fetal health. Summary: Fetal macrosomia is a common adverse infant outcome of GDM if unrecognized and untreated in time. For the infant, macrosomia increases the risk of shoulder dystocia, clavicle fractures and brachial plexus injury and increases the rate of admissions to the neonatal inten...
Related Papers
BMC Pregnancy and Childbirth
Valentina Soini , Gianpaolo Maso , Daniele Domini
Journal of Obstetrics and Gynaecology Research
María Isabel Hodgson
The Journal of Maternal-fetal Medicine
Diabetes Care
Erica P Gunderson
Fortune Journals
Background: Macrosomia is defined as a birth weight above the 90th percentile for gestational age. Macrosomic infants associated with neonatal morbidities and admissions to the neonatal intensive care unit,also is associated with maternal complications such as cesarean delivery, postpartum hemorrhage and trauma.
Chidiebere Imoh , Christian Isichei
Pakistan Journal of Medical Sciences
Nuzhat Parveen
Objectives: To determine the prevalence, risk factors for macrosomia and pregnancy outcome in women with gestational diabetes (GDM). Methods: In this prospective observational study, we included the data of 161 pregnant females diagnosed with GDM. The study was conducted from December 1st, 2020 to June 30, 2021, at the Maternity and Children Hospital (MCH) of Hail, Saudi Arabia. The data regarding risk factors of macrosomia was obtained from each patient. The patients were followed till the delivery of the baby. The data regarding the prevalence of fetal macrosomia and its associated outcomes was noted. Results: The prevalence of fetal macrosomia was 19.8%. Maternal obesity (OR 4.87), poorly controlled diabetes (OR 3.3), previous history of good-sized baby (OR 2.30), previous history of congenital abnormalities (OR 7.2) were the significant risk factors of fetal macrosomia. The prevalence of maternal and fetal complications was high among pregnancies complicated by fetal macrosomia....
To examine the impact of maternal blood glucose (BG) level and body mass index (BMI) measured at gestational diabetes mellitus (GDM) screening on the risk of macrosomia. A perinatal cohort of women were followed up from receiving perinatal healthcare to giving birth. Beichen District, Tianjin, China between June 2011 and October 2012. 1951 women aged 19-42 years with valid values of BMI and BG level at GDM screening (24-28 weeks gestation), singleton birth and birth weight (BW)>2500 g. Primary outcome was macrosomia (BW>4000 g). BG level and BMI were measured at GDM screening. 191 (9.7%) newborns were macrosomia. The ORs (95% CIs) of macrosomia from multiple logistic regression were 1.14 (1.10 to 1.19, p<0.0001) for BMI and 1.11 (1.01 to 1.23, p=0.03) for BG. When BMI and BG levels (continuous) were modelled simultaneously, the OR for BMI was similar, but significantly attenuated for BG. Areas of receiver operating characteristics (ROC) were 0.6530 (0.6258 to 0.6803) for BM...
Journal of Perinatology
GUSTAVO JIMENEZ
Al-Azhar International Medical Journal
Fahd Elomda
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Annals of Medical and Health Sciences Research
Elizabeta Zisovska
European Journal of Endocrinology
Monica Pratesi
Neda Esmailzadehha
Maternal Health, Neonatology and Perinatology
Corrie Miller
Journal of the American Dietetic Association
monique romon
Evidence Based Women's Health Journal
Mohamed Sweed
Amal Korrida
Journal of Maternal and Child Health
tantri ratna
Diabetologia
American Journal of Obstetrics and Gynecology
Kristina Adams Waldorf
Simona Carniciu
Journal of Maternal-Fetal and Neonatal Medicine
Bryan Mitchell
Diabetes Updates
sonila alia
Marijana Arambašić
Diabetes & metabolism
Paul Landais
Frontiers in Endocrinology
Jimena Pereda
BJOG: An International Journal of Obstetrics & Gynaecology
Elena Magro-Malosso
International Journal of Biomedicine
Khalid Haddad
European Journal of Obstetrics & Gynecology and Reproductive Biology
Erdal Budak
Journal of Neonatal-Perinatal Medicine
Gabriella Zito
BioMed research international
Mark Walker
Thomas Hahn
IP Innovative Publication Pvt. Ltd.
International Journal of Reproduction, Contraception, Obstetrics and Gynecology
SHASHWAT JANI
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Search Menu
- Sign in through your institution
- Advance Articles
- Thematic Issues
- ENDO Meeting Abstracts
- Clinical Practice Guidelines
- Endocrine Reviews
- Endocrinology
- Journal of the Endocrine Society
- The Journal of Clinical Endocrinology & Metabolism
- JCEM Case Reports
- Molecular Endocrinology (Archives)
- Endocrine Society Journals
- Author Guidelines
- Submission Site
- Open Access
- Why Publish with the Endocrine Society?
- Advertising & Corporate Services
- Reprints, ePrints, Supplements
- About Endocrine Reviews
- Editorial Board
- Author Resources
- Reviewer Resources
- Rights & Permissions
- Member Access
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Current gdm diagnostic criteria, contemporary clinical evidence following the revised iadpsg gdm diagnostic criteria, current classification of hyperglycemia in pregnancy and gdm, the impact of preanalytical glucose processing standards on the diagnosis of gdm, incidence and prevalence of gdm, risk factors for gdm, pathophysiology of gdm, genetics of gdm, maturity-onset diabetes of the young, consequences of gdm, neonatal complications, short-term risk, long-term risk in the offspring, maternal complications, management of gdm, lifestyle intervention, gestational weight gain, maternal glucose targets, insulin therapy, oral pharmacotherapy, obstetric management, longer term management of women following gdm, treatment of gdm and long-term offspring outcomes, precision medicine in gdm: physiological heterogeneity, subtype classification, risk prediction, and biomarker utility, the covid-19 pandemic and gdm, financial support, disclosure summary, a clinical update on gestational diabetes mellitus.
- Article contents
- Figures & tables
- Supplementary Data
Arianne Sweeting, Jencia Wong, Helen R Murphy, Glynis P Ross, A Clinical Update on Gestational Diabetes Mellitus, Endocrine Reviews , Volume 43, Issue 5, October 2022, Pages 763–793, https://doi.org/10.1210/endrev/bnac003
- Permissions Icon Permissions
Gestational diabetes mellitus (GDM) traditionally refers to abnormal glucose tolerance with onset or first recognition during pregnancy. GDM has long been associated with obstetric and neonatal complications primarily relating to higher infant birthweight and is increasingly recognized as a risk factor for future maternal and offspring cardiometabolic disease. The prevalence of GDM continues to rise internationally due to epidemiological factors including the increase in background rates of obesity in women of reproductive age and rising maternal age and the implementation of the revised International Association of the Diabetes and Pregnancy Study Groups’ criteria and diagnostic procedures for GDM. The current lack of international consensus for the diagnosis of GDM reflects its complex historical evolution and pragmatic antenatal resource considerations given GDM is now 1 of the most common complications of pregnancy. Regardless, the contemporary clinical approach to GDM should be informed not only by its short-term complications but also by its longer term prognosis. Recent data demonstrate the effect of early in utero exposure to maternal hyperglycemia, with evidence for fetal overgrowth present prior to the traditional diagnosis of GDM from 24 weeks’ gestation, as well as the durable adverse impact of maternal hyperglycemia on child and adolescent metabolism. The major contribution of GDM to the global epidemic of intergenerational cardiometabolic disease highlights the importance of identifying GDM as an early risk factor for type 2 diabetes and cardiovascular disease, broadening the prevailing clinical approach to address longer term maternal and offspring complications following a diagnosis of GDM.

Gestational diabetes mellitus (GDM) is 1 of the most common medical complications of pregnancy and is increasing in prevalence globally.
GDM is associated with obstetric and neonatal complications primarily due to increased birthweight and is a major risk factor for future type 2 diabetes, obesity, and cardiovascular disease in mother and child.
Detecting GDM is important because perinatal complications and stillbirth risk are greatly reduced by treatment.
A precision medicine approach to GDM which recognizes severity and onset of maternal hyperglycemia as well as genetic and physiologic subtypes of GDM may address the current diagnostic controversy via accurate risk stratification and individualized treatment strategies, leading to improved clinical care models and outcomes.
The traditional focus on normalization of obstetric and neonatal outcomes achieved via short-term antenatal maternal glucose management should now shift to early postnatal prevention strategies to decrease the progression from GDM to type 2 diabetes and address longer term maternal and offspring metabolic risk given the global epidemic of diabetes, obesity, and cardiovascular disease.
Diabetes in pregnancy was first described in 1824 by Bennewitz in Germany ( 1 ), with subsequent case series in the United Kingdom and United States reporting high perinatal mortality rates in women with diabetes in pregnancy ( 2-4 ). In 1909, Williams reported arguably the first diagnostic criteria for diabetes in pregnancy in the United States, proposing physiological and pathophysiological thresholds for “transient glycosuria in pregnancy” ( 5 ).
In 1964, O’Sullivan and Mahan defined specific diagnostic criteria for gestational diabetes mellitus (GDM) in the United States derived from the 100-g 3-hour oral glucose tolerance test (OGTT) undertaken in the second and third trimester of pregnancy in 752 women ( 6 ). GDM was defined as ≥2 venous whole blood glucose values greater than 2 SD above the mean glucose values for pregnancy in their initial cohort. These glucose thresholds were primarily chosen because the resulting GDM prevalence of 2% corresponded to the background population prevalence of diabetes, while the requirement of ≥2 elevated glucose values sought to minimize the risk of preanalytical error ( 7 ). These thresholds were validated by their identification of subsequent diabetes up to 8 years postpartum in an additional cohort of 1013 women. Increased perinatal mortality was also observed in women with ≥2 glucose values exceeding the proposed diagnostic criteria ( 6 ). In 1965, the World Health Organization (WHO) concurrently recommended that GDM be diagnosed by either a 50- or 100-g OGTT using the 2-hour postload glucose value, but the threshold used was the same as for diagnosing diabetes in the nonpregnant population ( 8 ). The WHO continued to diagnose GDM based on glucose thresholds for diabetes in the nonpregnant population ( 9 , 10 ) until its endorsement of the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) diagnostic criteria in 2013 ( 11 ).
Since 1973, the screening approach to GDM frequently adopted a 2-step procedure with the 50-g 1-hour glucose challenge test (GCT) followed by the 100-g 3-hour OGTT if the GCT was positive. This was based on data from O’Sullivan et al, which showed that a 2-step diagnostic approach to GDM using the GCT as the initial screening test and a glucose threshold of 7.9 mmol/L (143 mg/dL) was 79% sensitive and 87% specific for diagnosing GDM on the 100-g 3-h OGTT in a cohort of 752 women ( 12 ). The rationale for this approach was the efficient identification of women most at risk of GDM.
In 1979, the US National Diabetes Data Group (NDDG) published conversions of the original O’Sullivan and Mahan 100-g 3-hour OGTT diagnostic criteria for GDM, reflecting the transition from venous whole blood glucose to plasma blood glucose analysis ( 13 ). These revised criteria were subsequently adopted by the American Diabetes Association (ADA) and internationally ( 9 , 14 , 15 ). In 1982, Carpenter and Coustan recommended lowering of the NDDG diagnostic criteria, reflecting newer preanalytical enzymatic methods that were more specific for plasma glucose ( 7 , 16 ). They also advised lowering the GCT glucose threshold to 7.5 mmol/L (135 mg/dL) based on their study of 381 women who underwent the 100-g 3-h OGTT after screening positive on the GCT, whereby a GCT glucose threshold ≤ 7.5 mmol/L (135 mg/dL) strongly correlated with a normal OGTT ( 17 ). However, in the absence of clear evidence supporting a specific glucose threshold for the GCT, the ADA and the American College of Obstetricians and Gynecologists (ACOG) continued to recommend a screen positive GCT glucose threshold from 7.2 to 7.8 mmol/L (130-140 mg/dL) for GDM ( 18 , 19 ).
The ADA did however recommend the modified Carpenter and Coustan diagnostic glucose thresholds for GDM from 2000 ( 20 ), supported by the findings of the Toronto Tri-Hospital Gestational Diabetes Project ( 21 , 22 ). These data demonstrated a positive correlation between increasing maternal hyperglycemia even below the NDDG diagnostic criteria for GDM and risk of obstetric and neonatal complications including preeclampsia, cesarean section, and macrosomia (neonatal birthweight > 4000 g) ( 21 , 22 ). In addition, several large cohort studies showed that women diagnosed (but not treated) with GDM based on the Carpenter and Coustan criteria were at increased risk of perinatal complications including hypertensive disorders of pregnancy, increased birthweight, macrosomia, neonatal hypoglycemia, hyperbilirubinemia, and shoulder dystocia, compared to women diagnosed and treated as GDM by NDDG diagnostic criteria ( 16 , 23-25 ). From 2003 the ADA additionally endorsed the 1-step 75-g 2-hour OGTT for the diagnosis of GDM derived from the modified Carpenter and Coustan fasting, 1- and 2-hour glucose thresholds for the 100-g 3-hour OGTT, particularly for women at high-risk ( 26 ). This approach was deemed more cost-effective, albeit less validated, than the 100-g 3-hour OGTT. The use of the modified Carpenter and Coustan thresholds was associated with an almost 50% increase in prevalence of GDM ( 16 , 23 ).
The evolution of diagnostic criteria for GDM illustrates the historic lack of consensus for the diagnosis of GDM, with the presence or absence of disease varying dependent on expert consensus. The underlying rationale for the diagnosis of GDM also shifted over time toward identifying perinatal risk rather than future maternal diabetes risk.
The seminal Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study sought to provide an evidence base to guide risk in GDM, and its results were published in 2008 ( 27 ). This large, international, prospective, observational study evaluated the relationship between glucose levels on the 75-g 2-hour OGTT performed at 24 to 32 weeks’ gestation (mean 27.8 weeks’ gestation) in over 25 000 pregnant women with the following primary perinatal outcomes: birthweight > 90th percentile for gestational age, primary cesarean section delivery, neonatal hypoglycemia, and cord blood serum C-peptide > 90th centile. Secondary outcomes were preeclampsia, preterm delivery (defined as delivery before 37 weeks’ gestation), shoulder dystocia or birth injury, hyperbilirubinemia, and neonatal intensive care admission. The results showed a continuous positive linear relationship between maternal fasting; 1- and 2-hour plasma glucose levels obtained on the OGTT, below those that were diagnostic of diabetes outside pregnancy; and risk of primary outcomes ( 27 ). Notably, there were no specific glucose thresholds at which obstetric and neonatal complications significantly increased.
Based on these findings and supported by trials [the Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) and the Maternal-Fetal Medicine Units Network (MFMU) trial] showing benefit of treatment of more severe and “mild” degrees of maternal hyperglycemia, respectively ( 28 , 29 ), the IADPSG revised its diagnostic criteria for GDM. Despite the lack of a clear diagnostic glucose threshold in HAPO, the consensus of the IADPSG was to define diagnostic thresholds for the fasting, 1- and 2-hour glucose values for the 75-g 2-hour OGTT based on the average glucose values at which the odds of the primary outcomes were 1.75 times the odds of these outcomes occurring at the mean glucose levels for the HAPO cohort ( 30 ). The IADPSG consensus was also that only 1 elevated glucose level for the OGTT was required for GDM diagnosis, as each glucose threshold represented broadly comparable level of risk. Thus, the main purpose of the diagnostic criteria for GDM post-HAPO was to define the level of risk associated with increased perinatal complications.
Post-HAPO, there exist several different screening and testing approaches for the diagnosis of GDM internationally. The IADPSG and WHO recommend universal testing of all pregnant women between 24 to 28 weeks’ gestation with the 75-g 2-hour OGTT ( 11 , 30 ). These revised recommendations were largely endorsed by several organizations including the ADA ( 18 ), Endocrine Society ( 31 ), International Federation of Gynecology and Obstetrics ( 32 ), Australasian Diabetes in Pregnancy Association ( 33 ), Japan Diabetes Society ( 34 ), Ministry of Health of China ( 35 ), and the European Board of Gynecology and Obstetrics ( 36 ).
The National Institutes of Health did not endorse the IADPSG recommendations, citing the expected increase in prevalence of GDM, cost, and intervention in the context of a lack of evidence for an associated improvement in perinatal outcomes ( 37 ). The National Institutes of Health and ACOG continue to recommend a 2-step testing approach, with the initial screening GCT for all women and those who screen positive proceeding to the diagnostic 100-g 3-hour OGTT ( 19 , 37 ). This approach is also endorsed by ADA ( 18 ). However, the ACOG’s 2018 guidelines now acknowledge that individual practices and institutions may instead choose to use the IADPSG’s 1-step testing approach and diagnostic criteria if appropriate for their population ( 19 ). The UK National Institute for Health and Care Excellence (NICE) guidelines advise a selective screening approach, whereby women with risk factors for GDM are recommended to undergo a diagnostic 75-g 2-hour OGTT at 26 to 28 weeks’ gestation, with diagnostic (fasting or 2-hour) glucose thresholds higher than the IADPSG diagnostic criteria for GDM ( 38 ). Several other European bodies also currently recommend selective risk factor-based screening, with only women fulfilling specific high-risk criteria proceeding to a diagnostic OGTT, even if the IADPSG diagnostic criteria for GDM are applied ( 39 , 40 ). The revised IADPSG diagnostic criteria and testing approach to GDM in comparison to other international organizations are summarized in Table 1 .
Current international testing approach to gestational diabetes mellitus
| Organization/country . | Selective vs universal testing . | Method of screening . | Screen positive threshold (mmol/L) . | Diagnostic test . | Diagnostic (plasma glucose) threshold for GDM (mmol/L) . |
|---|---|---|---|---|---|
| IADPSG ( ) WHO ( ) ADIPS ( ) FIGO ( ) JDS ( ) EBCOG ( ) Endocrine Society ( ) China ( ) | Universal | One-step: 75-g 2-h OGTT | 75-g 2-hour OGTT | Fasting ≥ 5.1 1-h ≥ 10.0 2-h ≥ 8.5 One abnormal value needed for diagnosis | |
| ADA ( ) | Universal | One-step: 75-g 2-h OGTT Two-step: 50-g GCT | ≥7.2 to 7.8 | 75-g 2-hour OGTT 100-g 3-hour OGTT | Fasting ≥ 5.1 1-h ≥ 10.0 2-h ≥ 8.5 One abnormal value needed for diagnosis Carpenter and Coustan ( ) or NDDG ( ) Fasting ≥ 5.3 Fasting ≥ 5.8 1-hour ≥ 10.0 1-hour ≥ 10.6 2-hour ≥ 8.6 2-hour ≥ 9.2 3-hour ≥ 7.8 3-hour ≥ 8.0 Two abnormal values needed for diagnosis |
| ACOG ( ) | Universal | Two-step: 50-g GCT | ≥7.2 to 7.8* | 100-g OGTT | Carpenter and Coustan ( ) or NDDG ( ) Fasting ≥ 5.3 Fasting ≥ 5.8 1-hour ≥ 10.0 1-hour ≥ 10.6 2-hour ≥ 8.6 2-hour ≥ 9.2 3-hour ≥ 7.8 3-hour ≥ 8.0 Two abnormal values needed for diagnosis |
| CDA ( ) | Universal | Two-step: 50-g GCT (preferred) One-step: 75-g 2-h OGTT (alternative) | ≥7.8 | 50-g GCT 75-g 2-hour OGTT | ≥11.1 mmol/L Fasting ≥ 5.3 1-hour ≥ 10.6 2-hour ≥ 9.0 One abnormal value needed for diagnosis |
| NICE ( ) | Selective | Risk factors | 75-g 2-hour OGTT | Fasting ≥ 7.0 2-hour ≥ 7.8 One abnormal value needed for diagnosis | |
| CNGOF ( ) | Selective | First trimester fasting glucose 75-g OGTT | ≥5.1 Fasting ≥ 5.1 1-hour ≥ 10.0 2-hour ≥ 8.5 One abnormal value needed for diagnosis | ||
| DDG/DGGG ( ) | Universal | Two-step: 50-g GCT One-step: 75-g OGTT (preferred) | ≥7.5 | 50-g GCT 75-g OGTT | ≥11.1 mmol/L Fasting ≥ 5.1 1-hour ≥ 10.0 2-hour ≥ 8.5 One abnormal value needed for diagnosis |
| DIPSI ( ) | Universal | One-step: 75-g OGTT | 75-g OGTT | 2-hour ≥ 7.8 |
| Organization/country . | Selective vs universal testing . | Method of screening . | Screen positive threshold (mmol/L) . | Diagnostic test . | Diagnostic (plasma glucose) threshold for GDM (mmol/L) . |
|---|---|---|---|---|---|
| IADPSG ( ) WHO ( ) ADIPS ( ) FIGO ( ) JDS ( ) EBCOG ( ) Endocrine Society ( ) China ( ) | Universal | One-step: 75-g 2-h OGTT | 75-g 2-hour OGTT | Fasting ≥ 5.1 1-h ≥ 10.0 2-h ≥ 8.5 One abnormal value needed for diagnosis | |
| ADA ( ) | Universal | One-step: 75-g 2-h OGTT Two-step: 50-g GCT | ≥7.2 to 7.8 | 75-g 2-hour OGTT 100-g 3-hour OGTT | Fasting ≥ 5.1 1-h ≥ 10.0 2-h ≥ 8.5 One abnormal value needed for diagnosis Carpenter and Coustan ( ) or NDDG ( ) Fasting ≥ 5.3 Fasting ≥ 5.8 1-hour ≥ 10.0 1-hour ≥ 10.6 2-hour ≥ 8.6 2-hour ≥ 9.2 3-hour ≥ 7.8 3-hour ≥ 8.0 Two abnormal values needed for diagnosis |
| ACOG ( ) | Universal | Two-step: 50-g GCT | ≥7.2 to 7.8* | 100-g OGTT | Carpenter and Coustan ( ) or NDDG ( ) Fasting ≥ 5.3 Fasting ≥ 5.8 1-hour ≥ 10.0 1-hour ≥ 10.6 2-hour ≥ 8.6 2-hour ≥ 9.2 3-hour ≥ 7.8 3-hour ≥ 8.0 Two abnormal values needed for diagnosis |
| CDA ( ) | Universal | Two-step: 50-g GCT (preferred) One-step: 75-g 2-h OGTT (alternative) | ≥7.8 | 50-g GCT 75-g 2-hour OGTT | ≥11.1 mmol/L Fasting ≥ 5.3 1-hour ≥ 10.6 2-hour ≥ 9.0 One abnormal value needed for diagnosis |
| NICE ( ) | Selective | Risk factors | 75-g 2-hour OGTT | Fasting ≥ 7.0 2-hour ≥ 7.8 One abnormal value needed for diagnosis | |
| CNGOF ( ) | Selective | First trimester fasting glucose 75-g OGTT | ≥5.1 Fasting ≥ 5.1 1-hour ≥ 10.0 2-hour ≥ 8.5 One abnormal value needed for diagnosis | ||
| DDG/DGGG ( ) | Universal | Two-step: 50-g GCT One-step: 75-g OGTT (preferred) | ≥7.5 | 50-g GCT 75-g OGTT | ≥11.1 mmol/L Fasting ≥ 5.1 1-hour ≥ 10.0 2-hour ≥ 8.5 One abnormal value needed for diagnosis |
| DIPSI ( ) | Universal | One-step: 75-g OGTT | 75-g OGTT | 2-hour ≥ 7.8 |
Abbreviations: ACOG, American College of Obstetricians and Gynecologists; ADA, American Diabetes Association; ADIPS, Australasian Diabetes in Pregnancy Association; CDA, Canadian Diabetes Association; CNGOF, Organisme professionnel des médecins exerçant la gynécologie et l'obstétrique en France; DDG, German Diabetes Association; DGGG, European Board of Gynecology and Obstetrics; DIPSI, Diabetes in Pregnancy Study Group of India; FIGO, International Federation of Gynecology and Obstetrics; GCT, glucose challenge test; IADPSG, International Association of the Diabetes and Pregnancy Study Groups; JDS, Japan Diabetes Society; NDDG, US National Diabetes Data Group; NICE, National Institute for Health and Care Excellence; OGTT, oral glucose tolerance test; WHO, World Health Organization.
a The ADA states that the choice of a specific positive GCT screening threshold is based upon the trade-off between sensitivity and specificity ( 41 ). ACOG advises that in the absence of clear evidence that supports a specific GCT threshold value between 7.2 and 7.8 mmol/L, obstetricians and obstetric care providers may select a single consistent GCT threshold for their practice based on factors such as community prevalence rates of GDM ( 19 ).
b Plasma or serum glucose.
c ACOG 2018 Clinical Practice Bulletin on GDM continues to recommend 2-step testing for GDM but states that individual practices and institutions may choose to use the IADPSG’s 1-step testing approach and diagnostic criteria if appropriate for their population ( 19 ).
d ACOG 2018 Clinical Practice Bulletin on GDM acknowledges that women who have even 1 abnormal value on the 100-g 3-hour OGTT have a significantly increased risk of adverse perinatal outcomes compared to women without GDM but state that further research is needed to clarify the risk of adverse outcomes and benefits of treatment in these women ( 19 ).
e A glucose level ≥ 11.1 mmol/L following the initial screening GCT is classified as GDM, and there is no need for a subsequent 2-hour 75-g OGTT.
f BMI > 30 kg/m 2 , previous macrosomia (≥4500 g), previous GDM, family history of diabetes, and family origin with a high prevalence of diabetes (South Asian, Black Caribbean, Middle Eastern) ( 38 ).
g Maternal age ≥ 35 years, body mass index ≥ 25 kg/m 2 , family history of diabetes, previous GDM, previous macrosomia ( 39 ).
h If first trimester fasting glucose normal (ie, < 5.1 mmol/L).
i Adapted from the WHO 1999 diagnostic criteria for GDM ( 45 ), using a nonfasting 75-g 2-hour OGTT ( 44 ).
It is important to consider the increase in GDM prevalence associated with the IADPSG diagnostic criteria in the context of the rising background rates of impaired glucose tolerance, type 2 diabetes, and obesity among young adults and women of reproductive age ( 46 , 47 ). For example, almost 18% of HAPO study participants would have met the IADPSG diagnostic thresholds for GDM. By comparison, the rate of prediabetes in US adults aged between 20 and 44 years is >29% ( 48 , 49 ).
Studies in Indian, Israeli, and US cohorts have suggested that the IADPSG testing approach and intervention for GDM is cost-effective based on a combination of delaying future type 2 diabetes and preventing perinatal complications ( 50-53 ). For example, a US study found that the IADPSG diagnostic criteria would be cost-effective if associated intervention decreased the absolute incidence of preeclampsia by >0.55% and cesarean delivery by >2.7% ( 53 ). In contrast, UK health economic data show that routinely identifying GDM is not cost-effective based on perinatal outcomes ( 54 ) and that the universal WHO (IADPSG) testing approach is less cost-effective than the NICE selective screening approach ( 55 ).
The lack of randomized controlled trials (RCTs) evaluating outcomes in women diagnosed with GDM based on the IADPSG criteria and the clinical relevance of treating the resulting milder degrees of hyperglycemia remain controversial ( 56 ). Several retrospective studies have shown that women diagnosed with GDM by the IADPSG criteria but who were previously classified as having normal glucose tolerance were still at increased risk for obstetric and neonatal complications, including gestational hypertension, preeclampsia, cesarean delivery, macrosomia, large-for-gestational-age (LGA), shoulder dystocia, and neonatal intensive care admission, compared to women with normal glucose tolerance ( 57-59 ). For example, a 2015 retrospective study in Taiwan comparing pregnancy outcomes in women diagnosed and treated for GDM using the 2-step (GCT followed by the 100-g 3-hour OGTT) approach compared to the IADPSG 1-step approach found that the latter was associated with a reduction in gestational weight gain (GWG), birthweight, macrosomia, and LGA ( 60 ). Another retrospective study in the United Kingdom reported that women who were diagnosed with GDM based on modified IADPSG diagnostic glucose thresholds but who screened negative for GDM on 2015 NICE diagnostic criteria had a higher risk of LGA, cesarean delivery, and polyhydramnios ( 61 ). Other retrospective studies have also demonstrated higher birthweight, birthweight z-score, ponderal index, and increased rates of LGA and cesarean delivery in untreated women diagnosed with GDM based on the IADPSG criteria, compared to women with normal glucose tolerance ( 62 , 63 ).
The recent randomized ScreenR2GDM trial compared 1-step screening (75-g 2-hour OGTT) with 2-step screening (2 GCT thresholds ≥7.2 mmol/L and ≥7.8 mmol/L used, followed by the 100-g 3-hour OGTT) in 23 792 pregnant women in the United States ( 64 ). Despite doubling the diagnosis of GDM with the 1-step approach (16.5% vs 8.5%), there were no differences in pregnancy complications including LGA [relative risk (RR) 0.95; 97.5% CI 0.87-1.05], perinatal composite outcome (RR 1.04; 97.5% CI 0.88-1.23), gestational hypertension or preeclampsia (RR 1.00; 97.5% CI 0.93-1.08), and primary cesarean section (RR 0.98; 97.5% CI 0.93-1.02) between the different screening approaches. These findings have not resolved the diagnostic debate for GDM, with some arguing that the 1-step approach therefore demonstrates insufficient perinatal benefit for the associated increased healthcare costs ( 65 ), while others have identified potential limitations in study methodology ( 7 , 47 , 65 , 66 ). Despite randomization to either testing strategy, the pragmatic trial design allowed clinicians to select a preferred strategy. Consequently, one third of women randomized to the 1-step approach did not adhere to the assigned screening and were tested via the 2-step approach, compared to only 8% of women randomized to the 2-step approach. Although the study attempted to adjust for this difference using inverse probability weighting, residual provider bias cannot be excluded ( 47 ). Given this was a population level analysis of GDM screening, GDM (treatment) status differed only for the 8% of women not diagnosed with GDM based on the 2-step approach who may have otherwise been diagnosed with GDM based on the 1-step approach. Whether these women had potentially worse outcomes that may have been mitigated by treatment cannot be determined by this study. However, given the rates of pharmacotherapy were similar between the 1- and 2-step cohorts at 43% and 46%, respectively ( 64 ), this strategy detected women with essentially an equivalent risk of hyperglycemia warranting pharmacotherapy ( 47 ). This observation is consistent with other studies in UK cohorts comparing the IADPSG testing approach to the less sensitive NICE and Canadian criteria, whereby women demonstrated insulin resistance and required pharmacotherapy for control of hyperglycemia even at the most sensitive thresholds of the IADPSG diagnostic criteria ( 67 ).
More generally, the GCT fails to detect approximately 20% to 25% of women with GDM, particularly those diagnosed with GDM based on an elevated fasting glucose ( 68 ). The frequency of GDM diagnosed by the OGTT fasting glucose threshold in the HAPO study ranged from 24% to 26% in Thailand and Hong Kong to >70% in the United States ( 69 ). This highlights the variability and thus limitations of post-glucose load screening based on ethnicity. Moreover, a recent systematic review and meta-analysis of 25 studies (n = 4466 women) showed that even 1 abnormal value on the diagnostic 3-hour 100-g OGTT is associated with an increased risk of perinatal complications compared to women with a normal GCT, and this risk was similar to that of women actually diagnosed with GDM ( 70 ).
The degree of benefit of treating women with GDM defined by the IADPSG diagnostic criteria is yet to be determined. The potential benefit is inferred from the treatment of maternal hyperglycemia described in the ACHOIS and MFMU intervention trials ( 28 , 29 ), whereby maternal glucose levels overlapped with the thresholds recommended by the IADPSG. It is worth noting that there are differences in these 2 trials with regards to the diagnostic criteria used to define GDM and cohort characteristics (eg, women were excluded from the MFMU trial if they had an abnormal glucose screening test prior to 24 weeks’ gestation or previous GDM), and thus the generalizability of these findings in women diagnosed with GDM based on the IADPSG criteria remains contentious.
The WHO first defined GDM in 1965 as “hyperglycemia of diabetic levels occurring during pregnancy” ( 8 ). Thus, historically, the term “GDM” encompassed the entire spectrum of maternal hyperglycemia in pregnancy, from pregestational diabetes to hyperglycemia first detected in pregnancy. In 1979, the NDDG defined GDM as “glucose intolerance that has its onset or recognition during pregnancy” ( 13 ). This was subsequently modified in 1985 at the Second International Workshop-Conference on Gestational Diabetes as “carbohydrate intolerance resulting in hyperglycemia of variable severity with onset or first recognition during pregnancy” and remained the most widely used definition of GDM until recently ( 71 ).
Contemporary nomenclature and diagnostic criteria now more clearly differentiate between women with pregestational diabetes and those with hyperglycemia first detected in pregnancy ( 30 ) ( Fig. 1 ). Pregestational diabetes includes type 1 diabetes, type 2 diabetes, and other types of diabetes such as cystic fibrosis-related diabetes, steroid/medication-induced diabetes, and monogenic diabetes.

Flowchart summarizing the contemporary nomenclature for hyperglycemia in pregnancy.
Hyperglycemia in pregnancy is now subclassified by the IADPSG into 2 separate categories, namely “overt diabetes mellitus during pregnancy” (overt diabetes) and GDM ( 30 ). Similarly, the WHO has a binary definition of hyperglycemia in pregnancy but has replaced the term “overt diabetes” with “diabetes mellitus in pregnancy” (DIP) ( 11 ). The rationale for the IADPSG recommendation for early testing in high-risk women is to diagnose DIP early in pregnancy. This is because DIP, diagnosed based on nonpregnant diabetes glucose thresholds, recognizes the increasing prevalence of undiagnosed preexisting diabetes in women of childbearing age as well as the greater risk associated with this degree of hyperglycemia ( 72-74 ). For example, a recent study in almost 5000 women in France found that DIP was associated with a 3.5-fold greater risk of hypertensive disorders in pregnancy compared to women with normal glucose tolerance, while early‐diagnosed DIP was associated with an increased risk of congenital malformation (7.7% vs 1.0% for women with normal glucose tolerance), suggesting that early hyperglycemia in pregnancy may sometimes be present at conception ( 75 ). However, DIP is not synonymous with preexisting diabetes. In Australian, women with DIP who performed an OGTT at 6 to 8 weeks postpartum, 21% had diabetes, 38% had impaired fasting glucose or impaired glucose tolerance, and 41% returned to normal glucose tolerance ( 76 ).
Regardless of the specific nomenclature used, DIP is distinct from GDM, which is defined by lower glucose thresholds on the OGTT and was historically considered to be a condition of mid to late pregnancy. The ADA has not accepted this nomenclature and defines GDM based on timing of diagnosis: women diagnosed with diabetes in the first trimester are classified as having (preexisting) type 2 diabetes, while GDM is defined as diabetes diagnosed in later pregnancy and not meeting the diagnostic criteria for type 2 diabetes ( 18 ). A summary of the current international nomenclature and diagnostic criteria for hyperglycemia in pregnancy is presented in Table 2 .
Classification and diagnostic criteria for hyperglycemia in pregnancy
| Organization . | Results . | ||
|---|---|---|---|
| IADPSG/EBCOG ( , ) | |||
| GDM | 75-g 2-hour OGTT Fasting glucose 5.1-6.9 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose 8.5-11.0 mmol/L | ||
| Overt diabetes during pregnancy | Fasting glucose ≥ 7.0 mmol/L Random glucose ≥ 11.1 mmol/L HbA1c ≥ 6.5% | ||
| WHO/FIGO/ADIPS ( , , ) | |||
| GDM | 75-g 2-hour OGTT Fasting glucose 5.1-6.9 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose 8.5-11.0 mmol/L | ||
| Diabetes mellitus in pregnancy | Fasting glucose ≥ 7.0 mmol/L 2-hour glucose ≥ 11.1 mmol/L post 75-g OGTT Random glucose ≥ 11.1 mmol/L in the presence of diabetes symptoms | ||
| ADA ( ) | |||
| GDM | 1-step strategy: 75-g 2-h OGTT Fasting glucose ≥ 5.1 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose ≥ 8.5 mmol/L | 2-step strategy: 50-g 1-hour GCT ≥ 7.8 mmol/L 100 g 3-hour OGTT Carpenter and Coustan ( ) or Fasting glucose ≥ 5.3 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose ≥ 8.6 mmol/L 3-hour glucose ≥ 7.8 mmol/L | NDDG ( ) Fasting glucose ≥ 5.8 mmol/L 1-h glucose ≥ 10.6 mmol/L 2-h glucose ≥ 9.2 mmol/L 3-h glucose ≥ 8.0 mmol/L |
| Type 2 diabetes mellitus | Fasting glucose ≥ 7.0 mmol/L 2-hour glucose ≥ 11.1 mmol/L post 75 g 2-hour OGTT Random glucose ≥ 11.1 mmol/L in the presence of diabetes symptoms HbA1c ≥ 6.5% | ||
| Organization . | Results . | ||
|---|---|---|---|
| IADPSG/EBCOG ( , ) | |||
| GDM | 75-g 2-hour OGTT Fasting glucose 5.1-6.9 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose 8.5-11.0 mmol/L | ||
| Overt diabetes during pregnancy | Fasting glucose ≥ 7.0 mmol/L Random glucose ≥ 11.1 mmol/L HbA1c ≥ 6.5% | ||
| WHO/FIGO/ADIPS ( , , ) | |||
| GDM | 75-g 2-hour OGTT Fasting glucose 5.1-6.9 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose 8.5-11.0 mmol/L | ||
| Diabetes mellitus in pregnancy | Fasting glucose ≥ 7.0 mmol/L 2-hour glucose ≥ 11.1 mmol/L post 75-g OGTT Random glucose ≥ 11.1 mmol/L in the presence of diabetes symptoms | ||
| ADA ( ) | |||
| GDM | 1-step strategy: 75-g 2-h OGTT Fasting glucose ≥ 5.1 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose ≥ 8.5 mmol/L | 2-step strategy: 50-g 1-hour GCT ≥ 7.8 mmol/L 100 g 3-hour OGTT Carpenter and Coustan ( ) or Fasting glucose ≥ 5.3 mmol/L 1-hour glucose ≥ 10.0 mmol/L 2-hour glucose ≥ 8.6 mmol/L 3-hour glucose ≥ 7.8 mmol/L | NDDG ( ) Fasting glucose ≥ 5.8 mmol/L 1-h glucose ≥ 10.6 mmol/L 2-h glucose ≥ 9.2 mmol/L 3-h glucose ≥ 8.0 mmol/L |
| Type 2 diabetes mellitus | Fasting glucose ≥ 7.0 mmol/L 2-hour glucose ≥ 11.1 mmol/L post 75 g 2-hour OGTT Random glucose ≥ 11.1 mmol/L in the presence of diabetes symptoms HbA1c ≥ 6.5% | ||
75-g 2-hour OGTT: only 1 plasma glucose level needs to be elevated for the diagnosis of GDM. 100 g 3-hour OGTT: at least 2 plasma glucose levels need to be elevated for the diagnosis of GDM.
Abbreviations: ADA, American Diabetes Association; ADIPS, Australasian Diabetes in Pregnancy Association; EBCOG, European Board & College of Obstetrics and Gynaecology; FIGO, International Federation of Gynecology and Obstetrics; GCT, glucose challenge test; HbA1c, hemoglobulin A1c; IADPSG/; International Association of the Diabetes and Pregnancy Study Groups; GDM, gestational diabetes mellitus; OGTT, oral glucose tolerance test; WHO, World Health Organization.
a The IADPSG recommends confirmation by fasting plasma glucose or HbA1c for the diagnosis of overt diabetes during pregnancy ( 30 ).
Most international guidelines now recommend early antenatal testing for women at high risk to identify women with DIP ( 11 , 18 , 30 , 38 , 39 , 42-44 ). This has resulted in increased detection of milder degrees of hyperglycemia below the threshold of DIP, referred to as GDM diagnosed prior to 24 weeks’ gestation or early GDM. Studies in women with GDM have reported that between 27% and 66% of GDM can be detected in early pregnancy depending on the population as well as the screening and diagnostic criteria used ( 77-81 ).
Recent studies evaluating the relationship between maternal glycemia and fetal growth trajectories confirm the early impact of maternal glycemia on excess fetal growth and adiposity prior to the diagnosis of standard GDM from 24 weeks’ gestation. A US multiethnic prospective cohort study of 2458 women enrolled between 8 and 13 weeks’ gestation included 107 (4.4%) women with GDM ( 82 ). GDM was associated with an increase in estimated fetal weight from 20 weeks’ gestation, which became significant at 28 weeks’ gestation. Similarly, Sovio et al showed that excessive fetal growth occurred between 20 to 28 weeks’ gestation, prior to the diagnosis of GDM, especially among women with higher body mass index [BMI (kg/m 2 )] ( 83 ). An Indian study also showed that excess subcutaneous abdominal adiposity was first detected at 20 weeks’ gestation, at least 4 weeks prior to the diagnosis of GDM ( 84 ). Early excess adiposity persisted despite adjustments for maternal age, BMI, GWG, fetal sex, and gestational age and remained higher at 32 weeks’ gestation ( 84 ).
Currently, there is no consensus for the preferred testing approach or diagnostic glycemic thresholds for early GDM. The IADPSG recommends diagnosing early GDM based on a fasting glucose of 5.1 mmol/L to 6.9 mmol/L (92-124 mg/dL) ( 30 ), consistent with the diagnostic fasting glucose threshold for standard GDM. The utility of a single fasting glucose measurement for early GDM diagnosis warrants consideration. First, preanalytical glucose handling variation, particularly in the setting of a single glucose measurement, is a major issue for GDM diagnostic accuracy (discussed in the following text). Second, an Israeli cohort study of 6129 women who underwent a fasting glucose test at a median of 9.5 weeks’ gestation demonstrated a positive association between first trimester fasting glucose up to 5.8 mmol/L (104.5 mg/dL) and increased risk for subsequent diagnosis of GDM, LGA, macrosomia, and cesarean section ( 85 ). Similar to the HAPO study, a clear glucose threshold was lacking, with pregnancy complications evident at fasting glucose levels <5.1 mmol/L (92 mg/dL). Third, maternal fasting glucose decreases in the first trimester, most pronounced between 6 to 10 weeks’ gestation [median decrease in glucose 0.11 mmol/L (1.98 mg/dL)] ( 86 ), while studies have consistently shown that early fasting glucose is poorly predictive of GDM at 24 to 28 weeks’ gestation ( 86-88 ), leading to potential overdiagnosis of GDM. In China, an early fasting glucose between 6.1 mmol/L to 6.9 mmol/L (110-124 mg/dL) best corresponded to later GDM diagnosis ( 88 ), but this requires further validation.
The WHO recommends the same diagnostic OGTT glucose thresholds for GDM in early pregnancy as those derived from HAPO by the IADPSG ( 11 ). However, the prognostic value of these glucose levels in early pregnancy is yet to be established. Others have proposed an hemoglobin A1c (HbA1c) risk threshold ( 89 ), based primarily on evidence that an early HbA1c ≥ 5.9% (41 mmol/mol) detected all cases of DIP and predicted adverse pregnancy outcomes in a New Zealand cohort ( 90 ). However, studies in other cohorts have found that while an elevated HbA1c in early pregnancy is highly specific, it lacks sensitivity for identifying hyperglycemia and certain perinatal complications ( 91 , 92 ), with no clear benefit of treating women with HbA1c 5.7% to 6.4% (39-46 mmol/mol) in early pregnancy ( 93 , 94 ). A summary of the various international criteria for testing of GDM in early pregnancy is presented in Table 3 .
International criteria for testing of gestational diabetes mellitus in early pregnancy
| Organization . | Early pregnancy testing . | Method of testing . | Diagnostic test . | Criteria for diagnosing early GDM (mmol/L) . |
|---|---|---|---|---|
| IADPSG ( ) | Yes | Selective—women at risk of overt diabetes during pregnancy | Fasting glucose | ≥5.1 |
| WHO ( ) | Not specified | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 | |
| ADIPS ( ) | Yes | Selective—women at risk of hyperglycemia in pregnancy | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| ADA ( ) | Yes | Selective—women with risk factors for undiagnosed type 2 diabetes | One-step: 75-g 2-hour OGTT Two-step: 50-g GCT 100-g 3-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 ≥7.2 to 7.8 Carpenter and Coustan ( ) NDDG ( ) Fasting ≥ 5.3 ≥ 5.8 1-hour ≥ 10.0 ≥ 10.6 2-hour ≥ 8.6 ≥ 9.2 3-hour ≥ 7.8 ≥ 8.0 |
| ACOG ( ) | Yes | Selective—women with risk factors for undiagnosed type 2 diabetes or GDM | 75-g 2-h OGTT 50-g GCT Confirmatory 100-g 3-hour OGTT | Fasting ≥ 7.0 2-hour ≥ 11.1 ≥7.2 to 7.8 Carpenter and Coustan ( ) NDDG ( ) Fasting ≥ 5.3 ≥ 5.8 1-hour ≥ 10.0 ≥ 10.6 2-hour ≥ 8.6 ≥ 9.2 3-hour ≥ 7.8 ≥ 8.0 |
| EBCOG ( ) | Yes | Selective—women at risk of overt diabetes during pregnancy | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| DDG/DGGG ( ) | Yes | Selective—women with risk factors for “manifest diabetes” | Random glucose Fasting glucose 75-g 2-hour OGTT | 7.8-11.05 mmol/L followed by a second blood glucose measurement or an OGTT 5.1-6.9 Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| CNGOF ( ) | Yes | Selective | Fasting glucose | ≥5.1 |
| NICE ( ) | Yes | Selective | 75-g 2-hour OGTT | Fasting ≥ 5.6 2-hour ≥ 7.8 |
| DIPSI ( ) | Yes | Universal | 75-g 2-hour OGTT | 2-hour ≥ 7.8 |
| Organization . | Early pregnancy testing . | Method of testing . | Diagnostic test . | Criteria for diagnosing early GDM (mmol/L) . |
|---|---|---|---|---|
| IADPSG ( ) | Yes | Selective—women at risk of overt diabetes during pregnancy | Fasting glucose | ≥5.1 |
| WHO ( ) | Not specified | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 | |
| ADIPS ( ) | Yes | Selective—women at risk of hyperglycemia in pregnancy | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| ADA ( ) | Yes | Selective—women with risk factors for undiagnosed type 2 diabetes | One-step: 75-g 2-hour OGTT Two-step: 50-g GCT 100-g 3-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 ≥7.2 to 7.8 Carpenter and Coustan ( ) NDDG ( ) Fasting ≥ 5.3 ≥ 5.8 1-hour ≥ 10.0 ≥ 10.6 2-hour ≥ 8.6 ≥ 9.2 3-hour ≥ 7.8 ≥ 8.0 |
| ACOG ( ) | Yes | Selective—women with risk factors for undiagnosed type 2 diabetes or GDM | 75-g 2-h OGTT 50-g GCT Confirmatory 100-g 3-hour OGTT | Fasting ≥ 7.0 2-hour ≥ 11.1 ≥7.2 to 7.8 Carpenter and Coustan ( ) NDDG ( ) Fasting ≥ 5.3 ≥ 5.8 1-hour ≥ 10.0 ≥ 10.6 2-hour ≥ 8.6 ≥ 9.2 3-hour ≥ 7.8 ≥ 8.0 |
| EBCOG ( ) | Yes | Selective—women at risk of overt diabetes during pregnancy | 75-g 2-hour OGTT | Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| DDG/DGGG ( ) | Yes | Selective—women with risk factors for “manifest diabetes” | Random glucose Fasting glucose 75-g 2-hour OGTT | 7.8-11.05 mmol/L followed by a second blood glucose measurement or an OGTT 5.1-6.9 Fasting 5.1-6.9 1-hour ≥ 10.0 2-hour 8.5-11.0 |
| CNGOF ( ) | Yes | Selective | Fasting glucose | ≥5.1 |
| NICE ( ) | Yes | Selective | 75-g 2-hour OGTT | Fasting ≥ 5.6 2-hour ≥ 7.8 |
| DIPSI ( ) | Yes | Universal | 75-g 2-hour OGTT | 2-hour ≥ 7.8 |
75-g 2-h OGTT: Only 1 abnormal glucose level needs to be elevated for the diagnosis of GDM. 100-g 3-h OGTT: 2 abnormal glucose levels need to be elevated for the diagnosis of GDM.
Abbreviations: ADA, American Diabetes Association; ACOG, American College of Obstetricians and Gynecologists; ADIPS, Australasian Diabetes in Pregnancy Association; CNGOF, Organisme professionnel des médecins exerçant la gynécologie et l'obstétrique en France; DDG, German Diabetes Association; DGGG, European Board of Gynecology and Obstetrics; DIPSI, Diabetes in Pregnancy Study Group of India; EBCOG, European Board & College of Obstetrics and Gynaecology; GCT, glucose challenge test; GDM, gestational diabetes mellitus; IADPSG, International Association of the Diabetes and Pregnancy Study Groups; NICE, National Institute for Health and Care Excellence; OGTT, oral glucose tolerance test; WHO, World Health Organization.
a High-risk criteria not explicitly defined.
b IADPSG does not recommend routinely performing the 75-g 2-h OGTT prior to 24 weeks’ gestation but advises that a fasting glucose ≥ 5.1 mmol/L in early pregnancy be classified as GDM ( 30 ).
c GDM diagnosed at any time in pregnancy based on an abnormal 75-g 2-h OGTT ( 11 ).
d High-risk criteria defined as previous hyperglycemia in pregnancy; previously elevated blood glucose level; maternal age ≥ 40 years; ethnicity: Asian, Indian subcontinent, Aboriginal, Torres Strait Islander, Pacific Islander, Maori, Middle Eastern, non-White African; family history of diabetes (first-degree relative with diabetes or sister with hyperglycemia in pregnancy); prepregnancy body mass index > 30 kg/m 2 ; previous macrosomia (birth weight > 4500 g or > 90th percentile); polycystic ovary syndrome; and medications: corticosteroids, antipsychotics ( 33 ).
e High-risk criteria defined as body mass index ≥ 25 kg/m 2 (≥ 23 kg/m 2 in Asian Americans) plus 1 of the following: physical inactivity; previous GDM; previous macrosomia (≥ 4000 g); previous stillbirth; hypertension; high density lipoprotein cholesterol ≤ 0.90 mmol/L; fasting triglycerides ≥ 2.82 mmol/L; polycystic ovary syndrome; acanthosis nigricans; nonalcoholic steatohepatitis; morbid obesity and other conditions associated with insulin resistance; hemoglobulin A1c ≥ 5.7%; impaired glucose tolerance or impaired fasting glucose; cardiovascular disease; family history of diabetes (first-degree relative); and ethnicity: African American, American Indian, Asian American, Hispanic, Latina, or Pacific Islander ethnicity. Note that the ADA recommends testing for GDM at 24 to 28 weeks’ gestation and have no specific definition for early GDM ( 41 ).
f ACOG states that the best test for early GDM screening is not clear but suggest the testing approach and diagnostic criteria used to diagnose type 2 diabetes in the nonpregnant population and thus have no specific definition for early GDM ( 19 ).
g High-risk criteria defined as previous GDM; overweight/obesity; family history of diabetes (first-degree relative with diabetes); previous macrosomia (>4000g or >90th percentile); polycystic ovary syndrome; ethnicity: Mediterranean, South Asian, black African, North African, Caribbean, Middle Eastern, or Hispanic ( 36 ).
h High-risk criteria defined as age ≥ 45 years; prepregnancy body mass index ≥ 30 kg/m 2 ; physical inactivity; family history of diabetes; high-risk ethnicity (eg. Asians, Latin Americans); previous macrosomia ≥ 4500 g; previous GDM; hypertension; prepregnancy dyslipidemia (high-density lipoprotein cholesterol ≤ 0.90 mmol/L, fasting triglycerides ≥ 2.82 mmol/L); polycystic ovary syndrome; prediabetes in an earlier test; other clinical conditions associated with insulin resistance (eg, acanthosis nigricans); history of coronary artery disease/peripheral artery disease/cerebral vascular disease; medications associated with hyperglycemia (eg. glucocorticoids). Note that the DDG/DGGG recommends that a 75-g 2-h OGTT be the initial early test in high-risk women (defined as women with ≥2 risk factors for GDM) ( 43 ).
i High-risk criteria are defined as previous GDM, previous impaired glucose tolerance, and/or obesity ( 39 ).
j High-risk criteria defined as body mass index> 30 kg/m 2 ; previous macrosomia (≥4500 g); previous GDM; family history of diabetes (first-degree relative with diabetes); minority ethnic family origin with a high prevalence of diabetes. The updated 2015 NICE guidelines state that women with previous GDM should undergo early self-monitoring of blood glucose or a 75-g 2-hour OGTT as soon as possible after booking (first or second trimester), and a repeat 75-g 2-hour OGTT at 24 to 28 weeks’ gestation if the initial OGTT was negative ( 38 ).
k 2-hour postload glucose measured on nonfasting 75-g OGTT ( 44 ).
Despite the lack of diagnostic clarity for early GDM, increasing evidence suggests that women with early GDM represent a high-risk cohort ( 81 ). Early studies also reported worse pregnancy outcomes and increased insulin resistance in early GDM ( 78 , 95-97 ) but were confounded by the inclusion of women with pregestational diabetes. The first large retrospective cohort study excluding women with DIP showed that women diagnosed and treated for early GDM, especially those diagnosed in the first trimester, were more insulin resistant and at significantly greater risk for obstetric and neonatal complications compared to women diagnosed and treated for GDM from 24 weeks’ gestation ( 81 ). Other studies have since confirmed these findings ( 98 , 99 ). Concerningly, an increased risk of perinatal mortality and congenital abnormalities has also been reported in the offspring of women with early GDM ( 75 , 78 , 95 , 96 ), with some data demonstrating that 5% of women with early GDM have abnormal fetal echocardiograms ( 97 ). A recent meta-analysis of 13 cohort studies showed greater perinatal mortality among women with early GDM (RR 3.58; 95% CI 1.91-6.71) compared to women with a later diagnosis of GDM despite treatment ( 100 ).
A recent study assessing the pathophysiological characteristics of women diagnosed with GDM at a median of 16 weeks’ gestation compared to those diagnosed from 24 weeks’ gestation using IADPSG diagnostic criteria reported that women with early GDM had lower insulin sensitivity (defined by insulin-mediated glucose clearance during an OGTT), even after accounting for maternal BMI ( 101 ). Consistent with the pathophysiology of GDM, women with both early and standard GDM demonstrated impairment in pancreatic β-cell function ( 102 ). These data underscore GDM phenotypic differences, specifically based on timing of diagnosis and degree of hyperglycemia ( 103 ).
A key issue is the current lack of high-quality evidence that diagnosing and treating early GDM improves pregnancy outcomes. A recent major RCT in the United States evaluating early testing for GDM in 962 women with obesity included a subgroup analysis of women diagnosed and treated for GDM [early n = 69 (15.0%) vs standard n = 56 (12.1%)] based on the 2-step testing approach ( 104 ). The average gestational age at GDM diagnosis was similar at 24.3 ± 5.2 weeks for the early screen group compared to 27.1 ± 1.7 weeks in the routine screen group. There was no difference in pregnancy outcomes, although the primary composite perinatal outcome (macrosomia, primary cesarean delivery, gestational hypertension, preeclampsia, hyperbilirubinemia, shoulder dystocia, and neonatal hypoglycemia) was nonsignificantly higher in the early-screen group (56.9% vs 50.8%; P = 0.06). Requirement for insulin therapy was almost 4-fold higher, while gestational age at delivery was lower (36.7 vs 38.7 weeks’ gestation; P = 0.001) in women with early GDM. In a post hoc analysis of the Lifestyle in Pregnancy study ( 105 ), no difference in pregnancy outcomes was shown between women randomized to either lifestyle intervention (n = 36) or standard treatment (n = 54) in early pregnancy. Whether different glycemic targets are required reflecting physiological differences in early maternal glucose or whether additional risk factors contributing to a more insulin resistant phenotype such as maternal adiposity might also have a role remain unanswered ( 81 ). The ongoing Treatment of Booking Gestational Diabetes Mellitus study, evaluating the impact of immediate vs delayed care for gestational diabetes diagnosed at booking, will seek to determine whether or not there is benefit from treating early GDM ( 106 ).
Although the contemporary testing approach to GDM remains contentious, it is important to recognize that the diagnosis of GDM is based on the laboratory measurement of maternal glucose rather than a clinical diagnosis. Arguably then, a major issue in the contemporary diagnosis of GDM is optimizing preanalytical processing and measurement of maternal plasma glucose to ensure diagnostic accuracy ( 107 , 108 ). This includes optimization of sample handling and minimization of any analytic error. Unfortunately, stringent preanalytical processing standards are not currently routinely applied. The American Association for Clinical Chemistry (AACC) and ADA recommendations on laboratory testing in diabetes advise collection of plasma glucose in sodium fluoride tubes, with immediate placement in an ice slurry and centrifugation within 30 minutes ( 109 ). Citrate tubes are recommended as an alternative where early centrifugation is not possible. These standards are important because a major source of preanalytical glucose measurement error in sodium fluoride tubes is glycolysis by erythrocytes and leukocytes, which at room temperature lowers glucose levels prior to centrifugation at a rate of 5% to 7% per hour [~0.6 mmol/L (10 mg/dL)] ( 109 , 110 ). By 1 hour, this degree of glucose lowering is higher than the total analytical error threshold for glucose based on biological variation ( 107 ).
Recent studies have shown that OGTT preanalytical glucose processing variability greatly impacts the prevalence of GDM ( 67 , 111 ). Implementation of the AACC/ADA recommendations in a UK cohort resulted in higher mean glucose concentrations and 2.7-fold increased detection of GDM based on IADPSG criteria compared with the standard practice of storing sodium fluoride tubes at room temperature and delaying centrifugation until collection of all 3 OGTT samples ( 112 ). This increase in GDM diagnosis was entirely attributable to control of glycolysis ( 107 ). Similarly, in a large Australian multiethnic cohort (n = 12317), the rate of GDM diagnosis based on IADPSG criteria increased from 11.6% to 20.6% with early (within 10 minutes) vs delayed centrifugation ( 111 ). Mean glucose concentrations for the fasting, 1-hour, and 2-hour OGTT samples were 0.24 mmol/L (5.4%), 0.34 mmol/L (4.9%), and 0.16 mmol/L (2.3%) higher with early centrifugation, with the increase in GDM diagnosis primarily due to the resulting increase in fasting glucose levels ( 111 ). Importantly, the HAPO study, upon which the IADPSG diagnostic criteria for GDM was based, followed these AACC/ADA preanalytical glucose processing standards ( 111 ).
GDM is 1 of the most common medical complications of pregnancy ( 73 ). In 2019, the International Diabetes Federation (IDF) estimated that 1 in 6 live births worldwide were complicated by GDM ( 113 ). More than 90% of cases of hyperglycemia in pregnancy occur in low- and middle-income countries ( 114 ), where the prevalence and severity of maternal and neonatal complications associated with GDM ( 47 , 113 ) contrast with the near-normal pregnancy outcomes of modern management of GDM in developed countries ( 115 ).
The prevalence of GDM varies widely, depending on the population, the specific screening and the diagnostic criteria utilized. A 2012 systematic review of the diagnostic criteria used to define GDM reported a worldwide prevalence of GDM of 2% to 24.5% for the WHO criteria, 3.6% to 38% for the Carpenter and Coustan criteria, 1.4 to 50% for the NDDG criteria, and 2% to 19% for the IADPSG criteria ( 116 ).
Regardless of the specific diagnostic criteria or population, the prevalence of GDM continues to rise internationally, corresponding to epidemiological factors including the background rates of type 2 diabetes and increased incidence of obesity in women of childbearing age and rising maternal age ( 117-124 ). Implementation of the revised IADPSG diagnostic criteria have further increased the proportion of women being diagnosed with GDM ( 69 , 125 , 126 ). The incidence of GDM in the original HAPO study cohort applying the IADPSG diagnostic criteria ranged from 9.3% to 25.5% depending on study site ( 69 ). Recent international prevalence data also demonstrate marked variability in the rate of GDM, ranging from 6.6% in Japan and Nepal to 45.3% of pregnancies in the United Arab Emirates ( 127 ).
Several modifiable and nonmodifiable risk factors for GDM have been identified ( Table 4 ). A history of GDM in a previous pregnancy is the strongest risk factor for GDM, with reported recurrence rates of up to 84% ( 128 ). The risk of recurrence varies greatly depending on ethnicity ( 128 ). Ethnicities at increased risk for development of type 2 diabetes, such as South and East Asians, Hispanic, Black and Native Americans, Aboriginal and Torres Strait Islanders, and Middle Easterners are also associated with an increased risk of GDM ( 129 , 130 ). A US study of over 123 000 women reported the prevalence of GDM using the 2000 ADA diagnostic criteria to be the highest among Filipinas (10.9%) and Asians (10.2%), followed by Hispanics (6.8%), non-Hispanic Whites (4.5%) and Black Americans (4.4%) ( 131 ). Women who have had GDM are at increased risk for subsequent type 2 diabetes, while family history of type 2 diabetes in a first-degree relative or sibling with GDM is a major risk factor for GDM ( 129 , 132-134 ).
Key risk factors for gestational diabetes mellitus
| Previous GDM |
| An ethnicity with a high prevalence of diabetes |
| Maternal age > 35 years |
| Family history of diabetes (first-degree relative with diabetes) |
| Obesity (BMI > 30 kg/m ) |
| Previous macrosomia (birthweight > 4500 g) |
| Polycystic ovary syndrome |
| Iatrogenic: glucocorticoids and antipsychotic medication |
| Previous GDM |
| An ethnicity with a high prevalence of diabetes |
| Maternal age > 35 years |
| Family history of diabetes (first-degree relative with diabetes) |
| Obesity (BMI > 30 kg/m ) |
| Previous macrosomia (birthweight > 4500 g) |
| Polycystic ovary syndrome |
| Iatrogenic: glucocorticoids and antipsychotic medication |
Abbreviations: BMI, body mass index; GDM, gestational diabetes mellitus.
Increasing maternal age is also a risk factor for GDM ( 129 , 133-135 ). The prospective First and Second Trimester Evaluation of Risk trial (n = 36 056) demonstrated a continuous positive relationship between increasing maternal age and risk for adverse pregnancy outcomes, including GDM ( 135 ). Maternal age 35 to 39 years and ≥40 years was associated with an adjusted odds ratio (OR) for GDM of 1.8 (95% CI 1.5-2.1) and 2.4 (95% CI 1.9-3.1), respectively ( 135 ). Other studies in high-risk cohorts have reported a lesser risk between increasing maternal age and GDM after adjustment for other risk factors ( 136 ).
Maternal prepregnancy overweight (BMI 25-29.99 kg/m 2 ) or obesity (BMI ≥ 30 kg/m 2 ) are common risk factors for GDM ( 129 , 130 , 133 , 134 , 136 , 137 ). The risk of GDM is increased almost 3-fold (95% CI 2.1-3.4) in women with class I obesity (BMI 30-34.99 kg/m 2 ) and 4-fold (95% CI 3.1-5.2) in women with class II obesity (BMI 35-39.99 kg/m 2 ), compared to women with a BMI < 30 kg/m 2 ( 138 ). High GWG, particularly in the first trimester, is also associated with an increased risk for GDM ( 131 , 139 , 140 ). Further, women with obesity and high GWG are 3- to 4-fold more likely to develop abnormal glucose tolerance compared to women who remained within the 1990 Institute of Medicine (IOM) recommendations for GWG ( 131 , 141 ). Interpregnancy weight gain is also a risk factor for GDM and perinatal complications in a subsequent pregnancy ( 142 ) and may be a potential confounder when considering the risk of GDM recurrence.
Studies have demonstrated an association between polycystic ovary syndrome and GDM, although this is significantly attenuated after adjustment for maternal BMI ( 143 , 144 ). Other risk factors for GDM include multiparity ( 133 , 134 ), twin pregnancy ( 145 , 146 ), previous macrosomia ( 123 ), a history of perinatal complications ( 134 ), maternal small-for-gestational-age (SGA) or LGA ( 134 ), physical inactivity ( 129 , 147 , 148 ), low-fiber high-glycemic load diets ( 149 ), greater dietary fat and lower carbohydrate intake ( 137 ), and medications such as glucocorticoids and anti-psychotic agents ( 150 , 151 ). Maternal pre- and early pregnancy hypertension is also associated with an increased risk of developing GDM ( 152 , 153 ).
Overall, noting the variation in performance and utility of clinical risk factors based on local population factors, previous GDM and family history of diabetes appear to be the strongest clinical risk factors for GDM ( 154-157 ). Ethnicity, higher maternal age, and BMI are also strong predictors for GDM ( 154-158 ).
Normal pregnancy is associated with marked changes in glycemic physiology ( 159 , 160 ). There is a progressive increase in insulin resistance, predominantly due to increased circulating placental hormones including growth hormone, corticotrophin-releasing hormone, human placental lactogen, prolactin, estrogen, and progesterone ( 161-166 ). Increased maternal adiposity particularly in early pregnancy also promotes insulin resistance, contributing to facilitated lipolysis by late pregnancy ( 167 , 168 ). The resultant increase in maternal free fatty acid (FFA) levels exacerbates maternal insulin resistance by inhibiting maternal glucose uptake and stimulating hepatic gluconeogenesis ( 168 , 169 ). By late pregnancy, studies have reported decreases in maternal glucose sensitivity between 40% and 80% in women with normal or increased BMI ( 170-172 ). Increased maternal insulin resistance results in higher maternal postprandial glucose levels and FFAs for maternal growth ( 164 , 167 , 173 ) and increased facilitated diffusion across the placenta, leading to greater availability of glucose for fetal growth ( 161 , 174 ). This progressive rise in maternal insulin resistance underpins the delayed testing approach to GDM, aiming to maximize detection of GDM when insulin resistance is at its greatest in mid- to late gestation.
In addition to increased insulin resistance and elevated postprandial glucose, adaptations in normal pregnancy include enhanced insulin secretion ( 160 , 165 ). Maternal glucose levels are maintained at lower levels than in healthy nonpregnant women ( 175 , 176 ), and euglycemia is maintained by a corresponding 200% to 250% increase in insulin secretion, most notable in early pregnancy ( 161 , 167 , 177 ). Human placental lactogen, in addition to prolactin and growth hormone, primarily regulate increased maternal β-cell insulin secretion and proliferation during pregnancy ( 178-180 ). Rodent studies have demonstrated a 3- to 4-fold increase in β-cell mass during pregnancy, mediated via hypertrophy, hyperplasia, neogenesis, and/or reduced apoptosis ( 181 , 182 ).
GDM is characterized by a relative insulin secretory deficit ( 177 ), in which maternal β-cell insulin secretion is unable to compensate for the progressive rise in insulin resistance during pregnancy ( 183 ). This leads to decreased glucose uptake, increased hepatic gluconeogenesis, and maternal hyperglycemia ( 167 ). It is hypothesized that this results from the failure of β-cell mass expansion ( 182 , 184 ). Hyperlipidemia, characterized predominantly by higher serum triglycerides, may also cause lipotoxic β-cell injury, further impairing insulin secretion ( 185 , 186 ). The pathogenesis of GDM therefore parallels that of type 2 diabetes, characterized by both increased insulin resistance and relative insulin deficiency arising from a reduction in β-cell function and mass ( 187 , 188 ).
Serial studies of the insulin secretory response in women who develop GDM suggest that the abnormal insulin secretory response is present from prepregnancy and increases in early pregnancy, prior to and independent of changes in insulin sensitivity ( 170 , 189-191 ). These data suggest that many women with GDM may have chronic or preexisting β-cell dysfunction, potentially mediated by circulating hormones including leptin ( 191 ).
The genetics of GDM and glucose metabolism in pregnancy remain poorly defined. Data on epigenetic mechanisms in GDM are especially lacking and primarily limited to the potential role of DNA methylation in mediating the intrauterine effects of GDM on offspring outcomes ( 192 , 193 ).
Most genetic studies have focused on variants associated with type 2 diabetes and have demonstrated a similar association with GDM ( 194 , 195 ). A meta-analysis of 28 case-control studies (n = 23425) ( 196 ) identified 6 genetic polymorphisms at loci involved in insulin secretion [insulin-like growth factor 2 messenger RNA-binding protein 2 ( IGF2BP2 ), melatonin receptor 1B ( MTNR1B ) and transcription factor 7-like 2 ( TCF7L2 )] ( 197-199 ), insulin resistance [insulin receptor substrate 1 ( IRS1 ) and peroxisome proliferator-activated receptor gamma ( PPARG )] ( 200 , 201 ), and inflammation [tumor necrosis factor alpha ( TNF-α )] ( 202 ) in type 2 diabetes. Overall, only MTNR1B , TCF7L2 , and IRS1 were also significantly associated with GDM, supporting the role of both impaired insulin secretion and insulin resistance in the pathogenesis of GDM as well as type 2 diabetes ( 196 ). Subgroup analysis showed the risk alleles of TCF7L2 and PPARG were significant only in Asian populations, while the association between IRS1 and TCF7L2 and GDM risk varied depending on diagnostic criteria and genotype methodology ( 196 ), highlighting the need for further large confirmatory studies.
Two genome-wide association studies (GWAS) have evaluated the genetic associations for GDM and glucose metabolism ( 194 , 203 ). The first, a 2-stage GWAS in Korean women, compared 468 women with GDM and 1242 normoglycemic women using 2.19 million genotyped markers before further genotyping 11 loci in 1714 women, identifying 2 loci significantly associated with GDM ( 203 ). A variant in cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like 1 ( CDKAL1 ) had the strongest association with GDM, followed by a variant near MTNR1B expressed in pancreatic β-cells ( 204 ). The IGF2BP2 variant did not reach genome-wide significance with GDM in this study. CDKAL1 was significantly associated with decreased fasting insulin concentration and homeostasis model assessment of β-cell function in women with GDM, consistent with impaired β-cell compensation. MTNR1B was associated with decreased fasting insulin concentrations in women with GDM and increased fasting glucose concentrations in both women with and without GDM ( 203 ). Variants in CDKAL1 and MTNR1B have previously been associated with type 2 diabetes risk ( 205 , 206 ).
A subsequent GWAS performed in a subset of the HAPO cohort (n = 4528) comprising European, Thai, Afro-Caribbean, and Hispanic women evaluated maternal metabolic traits in pregnancy ( 194 ). This study reported 5 variants associated with quantitative glycemic traits in the general population ( 207 , 208 ) that were also associated with glucose or C-peptide levels in pregnancy, although strength of association varied across cohorts ( 194 ). Specifically, loci in glucokinase regulator ( GCKR ), glucose-6-phosphatase 2 ( G6PC2 ), proprotein convertase subtilisin/kexin type 1 ( PCSK1 ), protein phosphatase 1, regulatory subunit 3B ( PPP1R3B ), and MTNR1B were associated with fasting glucose. In addition, GCKR and PPP1R3B were associated with fasting C-peptide levels, while MTNR1B was associated with 1-hour postload glucose. These loci have also previously been associated with lipid metabolism ( GCKR and PPP1R3B ), glycogen metabolism ( PPP1R3B ), and obesity-related traits ( PCSK1 ) ( 209-214 ).
Two additional novel loci identified near hexokinase domain containing 1 ( HKDC1 ) associated with 2-hour postload glucose, and β-site amyloid polypeptide cleaving enzyme 2 ( BACE2 ) associated with fasting C-peptide, demonstrated limited association with glycemic traits outside of compared to in pregnancy ( 215 ). In general, however, studies evaluating associations between genetic risk scores, glycemic traits in pregnancy, and GDM have also confirmed that genetic determinants of fasting glucose and insulin, insulin secretion, and insulin sensitivity reported outside of pregnancy influence GDM risk ( 216 ). A summary of the genes associated with GDM is provided in Table 5 .
Genes linked to gestational diabetes mellitus
| Gene symbol . | Gene name . | Function . |
|---|---|---|
| Melatonin receptor 1B | Receptor mediating the action of melatonin, including its inhibitory effect on insulin secretion | |
| Transcription factor 7-like 2 | Blood glucose homeostasis | |
| Insulin receptor substrate 1 | Receptor mediating the control of various cellular processes by insulin | |
| Cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like 1 | Proinsulin to insulin conversion | |
| Glucokinase regulator | Inhibits glucokinase in liver and pancreatic islet cells | |
| Glucose-6-phosphatase 2 | Glucose metabolism | |
| Proprotein convertase subtilisin/kexin type 1 | Endoprotease involved in proteolytic activation of polypeptide hormones and neuropeptides precursors including proinsulin, proglucagon-like peptide 1, and pro-opiomelanocortin | |
| Protein phosphatase 1, regulatory subunit 3B | Regulates glycogen metabolism | |
| Hexokinase domain containing 1 | Involved in glucose homeostasis and hepatic lipid accumulation | |
| Beta-site amyloid polypeptide cleaving enzyme 2 | Proteolytic processing of in pancreatic β-cells |
| Gene symbol . | Gene name . | Function . |
|---|---|---|
| Melatonin receptor 1B | Receptor mediating the action of melatonin, including its inhibitory effect on insulin secretion | |
| Transcription factor 7-like 2 | Blood glucose homeostasis | |
| Insulin receptor substrate 1 | Receptor mediating the control of various cellular processes by insulin | |
| Cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like 1 | Proinsulin to insulin conversion | |
| Glucokinase regulator | Inhibits glucokinase in liver and pancreatic islet cells | |
| Glucose-6-phosphatase 2 | Glucose metabolism | |
| Proprotein convertase subtilisin/kexin type 1 | Endoprotease involved in proteolytic activation of polypeptide hormones and neuropeptides precursors including proinsulin, proglucagon-like peptide 1, and pro-opiomelanocortin | |
| Protein phosphatase 1, regulatory subunit 3B | Regulates glycogen metabolism | |
| Hexokinase domain containing 1 | Involved in glucose homeostasis and hepatic lipid accumulation | |
| Beta-site amyloid polypeptide cleaving enzyme 2 | Proteolytic processing of in pancreatic β-cells |
Genes were identified and selected from the genome-wide association studies ( 194 , 203 ). The name and function of each gene was determined from GeneCards ( https://www.genecards.org ).
a Collectrin, amino acid transport regulator is a stimulator of β-cell replication.
Maturity-onset diabetes of the young (MODY) is the most common form of monogenic diabetes; inherited forms of diabetes characterized by defects in single genes regulating β-cell development and function ( 217 , 218 ). MODY consists of several autosomal dominant forms of diabetes accounting for up to 2% of all diabetes diagnoses ( 219 ). A diagnosis of MODY requires confirmatory molecular genetic testing, and thus MODY is frequently misdiagnosed as preexisting diabetes or GDM, accounting for up to 5% of GDM “cases” ( 220-223 ). A UK study reported that HNF-1α (MODY3) (52%) and glucokinase (GCK)-MODY subtype (MODY2) (32%) were most frequent in probands confirmed with MODY, followed by HNF-4α (MODY1) and HNF-1β (MODY5) ( 224 ).
Women with GCK-MODY often first present following antenatal screening for GDM, with an estimated prevalence of 1% of all GDM “cases” actually GCK-MODY ( 220 , 222 ). GCK-MODY is caused by mutations in the glucokinase gene, leading to a greater set point for glucose stimulated insulin release ( 219 ). Clinically, GCK-MODY is defined by mild, stable fasting hyperglycemia [fasting glucose 98-150 mg/dL (5.4-8.3 mmol/L)] and low rates of microvascular and macrovascular complications ( 220 ). It should be suspected following a positive OGTT in pregnancy if the fasting glucose is ≥5.5 mmol/L, the glucose increment from the fasting to 2-hour (75-g) OGTT is small (<4.6 mmol/L), and there is a positive family history of mild hyperglycemia or diabetes. In addition, a combination of fasting glucose ≥ 100 mg/dL (5.6 mmol/L) and BMI < 25 kg/m 2 has been shown to have a sensitivity of 68% and a specificity of 99% for differentiating GCK-MODY from GDM ( 220 ). Importantly, management differs from that of GDM because the need for intensive maternal glycemic control largely depends on whether the GCK-MODY mutation is also present in the fetus ( 220 , 225 , 226 ). Maternal insulin therapy is therefore only recommended in the presence of increased fetal abdominal growth (>75th centile) measured on serial ultrasounds from 26 weeks’ gestation, as this indicates that the fetus does not have the GCK mutation ( 220 ).
GDM is associated with excess neonatal and maternal short- and long-term morbidity, summarized in Table 6 .
Maternal and neonatal complications of gestational diabetes mellitus
| Complications . | Maternal . | Neonatal . |
|---|---|---|
| Short term | Preeclampsia Gestational hypertension Hydramnios Urinary tract/vaginal infections Instrumental delivery Cesarean delivery Traumatic labor/perineal tears Postpartum hemorrhage Difficulty initiating and/or maintaining breastfeeding | Stillbirth Neonatal death Preterm birth Congenital malformations Macrosomia Cardiomyopathy Birth trauma: Shoulder dystocia Bone fracture Brachial plexus injury Hypoglycemia Hyperbilirubinemia Respiratory distress syndrome |
| Long term | Recurrence of GDM Type 2 diabetes mellitus Hypertension Ischemic heart disease Nonalcoholic fatty liver disease Dyslipidemia Chronic kidney disease | Metabolic syndrome Hyperinsulinemia Childhood obesity Excess abdominal adiposity Higher blood pressure Possible earlier onset cardiovascular disease Possible attention-deficit hyperactivity disorder Autism spectrum disorder |
| Complications . | Maternal . | Neonatal . |
|---|---|---|
| Short term | Preeclampsia Gestational hypertension Hydramnios Urinary tract/vaginal infections Instrumental delivery Cesarean delivery Traumatic labor/perineal tears Postpartum hemorrhage Difficulty initiating and/or maintaining breastfeeding | Stillbirth Neonatal death Preterm birth Congenital malformations Macrosomia Cardiomyopathy Birth trauma: Shoulder dystocia Bone fracture Brachial plexus injury Hypoglycemia Hyperbilirubinemia Respiratory distress syndrome |
| Long term | Recurrence of GDM Type 2 diabetes mellitus Hypertension Ischemic heart disease Nonalcoholic fatty liver disease Dyslipidemia Chronic kidney disease | Metabolic syndrome Hyperinsulinemia Childhood obesity Excess abdominal adiposity Higher blood pressure Possible earlier onset cardiovascular disease Possible attention-deficit hyperactivity disorder Autism spectrum disorder |
Sources: Scholtens et al ( 227 ) and Saravanan ( 228 ).
Abbreviation: GDM, gestational diabetes mellitus.
The Pedersen hypothesis describes the pathophysiology contributing to perinatal complications in GDM ( 229 ). Maternal hyperglycemia results in fetal hyperglycemia via facilitated diffusion of glucose by the glucose transporter 1 (GLUT1) ( 230 ). Fetal hyperglycemia results in fetal hyperinsulinemia, promoting fetal anabolism, excessive fetal adiposity, and accelerated growth, leading to LGA and macrosomia ( 231-239 ). Maternal hyperlipidemia also contributes to excess fetal growth ( 233 , 240 ). Macrosomia and LGA increase the risk of cesarean section, birth trauma, and perinatal complications including shoulder dystocia, brachial plexus injury and fracture, and perinatal asphyxia ( 27 , 132 , 237 , 238 , 241-243 ). Increased risk of perinatal asphyxia is associated with fetal death in utero, polycythemia, and hyperbilirubinemia ( 27 , 244-246 ). Fetal hyperinsulinemia can also increase the risk of metabolic abnormalities including neonatal hypoglycemia, hyperbilirubinemia, and respiratory distress syndrome postpartum ( 27 , 244 ). The risk appears to be greater among offspring of women with more severe hyperglycemia ( 247 ). Figure 2 summarizes the perinatal consequences of GDM.

Perinatal consequences of gestational diabetes mellitus.
In the HAPO study, higher maternal glucose levels were associated with an increased risk of LGA, shoulder dystocia or birth injury, and neonatal hypoglycemia ( 27 ). A recent systematic review (n = 207 172) confirmed similar positive linear associations for maternal glycemia based on maternal glucose thresholds for the GCT, 75-g 2-hour OGTT, or 100-g 3-hour OGTT and risk of cesarean section, induction of labor (IOL), LGA, macrosomia, and shoulder dystocia ( 248 ). GDM has also been associated with an increased risk of preterm birth, birth trauma, neonatal respiratory distress syndrome, and hypertrophic cardiomyopathy ( 27 , 244 , 249 ). An increased risk of congenital malformations in the offspring has been reported, although whether this persists after adjustment for maternal age, BMI, ethnicity, and other contributing factors is unknown ( 250 ). A French cohort study (n = 796 346) reported a 30% higher risk of cardiac malformations in the offspring of women with GDM compared to women with normal glucose tolerance, after excluding women with likely undiagnosed pregestational diabetes ( 249 ). However, this increased risk only reached statistical significance in women treated with insulin therapy. Maternal BMI, which was not evaluated in these studies, may account for these findings ( 251 , 252 ). Similarly, a reported increase in perinatal mortality after 35 weeks’ gestation in the offspring of women with GDM may also be confounded by obesity ( 253-256 ). An increased risk of perinatal mortality after 37 weeks’ gestation was demonstrated in French women with GDM on dietary intervention, possibly because these women delivered later than women treated with insulin therapy ( 249 ). In contrast, the HAPO study did not demonstrate excess perinatal mortality in their untreated cohort ( 27 ).
Modern management of GDM and associated maternal risk factors is associated with near-normal birthweight in developed countries ( 115 , 257 ). This is important because birthweight is the major risk factor for shoulder dystocia, brachial plexus injury, neonatal hypoglycemia, and neonatal respiratory distress syndrome in the offspring of women with and without GDM ( 242 ). A retrospective cohort study of 36 241 pregnancies in the United States reported that the risk of shoulder dystocia among infants of women without GDM compared to women with GDM was 0.9% vs 1.6% if birthweight was <4000 g and 6.0% vs 10.5% if birthweight was ≥4000 g (macrosomia) ( 242 ). The risk of neonatal hypoglycemia in infants with birthweight < 4000 g was 1.2% vs 2.6% and 2.4% vs 5.3% for birthweight ≥ 4000 g, in women without GDM compared to women with GDM, respectively. Similar findings were seen for brachial plexus injury and neonatal respiratory distress syndrome. Thus, GDM confers increased risk of perinatal complications independent of birthweight.
The risk of stillbirth is also greater in women with GDM. A large US retrospective analysis examined stillbirth rates at various stages of gestation in over 4 million women, including 193 028 women with GDM. The overall risk of stillbirth from 36 to 42 weeks’ gestation was higher in women with GDM compared to women without GDM (17.1 vs 12.7 per 10 000 deliveries; RR 1.34; 95% CI 1.2-1.5) ( 253 ). This increased risk of stillbirth was also observed at each gestational week: 3.3 to 8.6 per 10 000 ongoing pregnancies in women with GDM compared to 2.1 to 6.4 per 10 000 ongoing pregnancies in women without GDM from 36 to 41 weeks’ gestation ( 253 ). For women with GDM, the relative risk of stillbirth was highest in week 37 (RR 1.84, 95% CI 1.5-2.3). Notably, the risk of stillbirth is highest in women with undiagnosed GDM. In a UK prospective case-control study (n = 1024), women with undiagnosed GDM based on a fasting glucose level ≥ 5.6mmol/L (≥100 mg/dL) had a 4-fold greater risk of late stillbirth (defined as occurring ≥28 weeks’ gestation) compared to women with fasting glucose < 5.6mmol/L (<100 mg/dL) ( 74 ). In contrast, women at risk of GDM based on NICE risk factors who were diagnosed with GDM on the OGTT had a similar risk of stillbirth to women who were not at risk of GDM. This suggests that diagnosing and managing GDM reduces the risk of stillbirth to near-normal levels ( 74 ).
Recent epidemiological studies suggest an increased risk of later adverse cardiometabolic sequelae in the offspring of women with GDM ( 227 , 258 ). A large Danish population-based cohort study (n = 2 432 000) demonstrated an association between maternal diabetes and an increased rate of early onset cardiovascular disease (CVD; ≤40 years of age) among offspring ( 259 ). GDM specifically was associated with a 19% increased risk of early onset CVD (95% CI 1.07-1.32). A longitudinal UK study provides potential mechanistic insight, finding that GDM was associated with alterations in fetal cardiac function and structure, with reduced systolic and diastolic ventricular function persisting in infancy ( 260 ). This is consistent with the association between in utero exposure to maternal hyperglycemia and fetal programming first reported in the Native American Pima population, characterized by a high prevalence of obesity, type 2 diabetes, and GDM ( 261 ).
The recent HAPO Follow Up Study (HAPO-FUS), which was not confounded by treatment of maternal glycemia, included 4832 children 10 to 14 years of age whose mothers were participants of HAPO ( 227 ). The HAPO-FUS demonstrated a durable impact of maternal glycemia with long-term offspring glucose metabolism, including at glucose levels lower than those diagnostic for GDM ( 227 ). A generally linear relationship between maternal antenatal glucose and offspring glucose levels and related outcomes was observed. Increasing maternal glucose categories were associated with a higher risk of impaired fasting glucose and impaired glucose tolerance and higher timed glucose measures and HbA1c levels and were inversely associated with insulin sensitivity and disposition index by 14 years of age, independent of maternal and childhood BMI and family history of diabetes ( 227 ). A positive association was observed between GDM defined by any criteria and glucose levels and impaired glucose tolerance in the offspring at ages 10 to 14 years and an inverse association with offspring insulin sensitivity ( 262 ). Higher frequencies of childhood obesity and measures of adiposity across increasing categories of maternal OGTT glucose levels were also noted ( 262 ). Recent evidence for increased glucose-linked hypothalamic activation in offspring aged 7 to 11 years previously exposed to maternal obesity and GDM in utero, which predicted higher subsequent BMI, represents 1 possible mechanism for this increased childhood obesity risk ( 263 ).
Women with GDM are at an increased risk of obstetric intervention including IOL, cesarean section ( 27-29 , 264 , 265 ), and complications associated with delivery including perineal lacerations and uterine rupture, predominantly relating to fetal macrosomia and polyhydramnios ( 266 ).
As demonstrated in HAPO and other studies, women with GDM also have an increased risk of gestational hypertension and preeclampsia ( 267-269 ). Consistent with the association between diabetes and microvascular disease, abnormalities in glucose metabolism affect trophoblast invasion, leading to impaired placentation and greater risk for preeclampsia ( 270 ). The mechanism likely relates to insulin resistance and inflammatory pathway activation ( 271 , 272 ), with in vitro studies showing that elevated glucose concentrations inhibit trophoblast invasiveness by preventing uterine plasminogen activator activity ( 272 ).
Long-term Maternal Risk Following GDM
Women diagnosed with GDM based on pre-IADPSG diagnostic criteria are at increased risk of GDM in future pregnancies, with reported recurrence rates of 30% to 84% ( 128 ). A diagnosis of GDM is also associated with up to a 20-fold greater lifetime risk of type 2 diabetes ( 273 , 274 ). A recent large meta-analysis and systematic review (20 studies, n = 1 332 373 including 67 956 women with GDM) showed that women with a history of GDM have a 10-fold increased risk of developing type 2 diabetes, mostly within the first 5 years post-GDM ( 273 ). HAPO-FUS demonstrated that over 50% of women whose OGTT thresholds met (untreated) IADPSG diagnostic criteria for GDM had developed impaired glucose tolerance after 14 years of follow-up ( 275 ). These data highlight the importance of a management approach to GDM that focuses on early prevention of type 2 diabetes. For example, the updated NICE guidelines now recommend diabetes prevention for all women with previous GDM ( 276 , 277 ).
Previous GDM is also associated with cardiovascular risk factors such as obesity, hypertension, and dyslipidemia ( 274 , 278-280 ). The lifetime risk of cardiovascular disease following GDM is almost 3-fold higher in women who develop type 2 diabetes and 1.5 fold higher even in women without type 2 diabetes ( 280 ). Studies also report a 26% greater risk of hypertension and a 43% greater risk of myocardial infarction or stroke in women with previous GDM compared to women without GDM ( 281 , 282 ). The significance of GDM as a risk factor for type 2 diabetes and cardiovascular disease has been recently recognized by international organizations including the American Heart Association ( 283 ).
Benefits of Intervention on Perinatal Outcomes
Contemporary changes to the detection and management of GDM have been associated with almost comparable neonatal birthweight and adiposity outcomes to the background maternity population in developed countries ( 115 ).
The ACHOIS trial (n = 1000) was the first large RCT to evaluate whether treatment of women with GDM reduced the risk of perinatal complications ( 28 ). GDM was diagnosed based on a combination of fasting glucose < 7.8 mmol/L (140 mg/dL) and 2-hour postload glucose 7.8 to 11.0 mmol/L (140-199 mg/dL), respectively, using the 75-g 2-hour OGTT between 24 and 34 weeks’ gestation, following screening with either positive clinical risk factors or the GCT ( 28 ). ACHOIS demonstrated that a combination of dietary advice, self-monitoring of maternal glucose levels (SMBG), and insulin therapy, if required, to achieve SMBG targets [fasting glucose 3.5-5.5 mmol/L (63-99 mg/dL), preprandial glucose ≤ 5.5 mmol/L (99 mg/dL), and 2-hour postprandial glucose ≤ 7.0 mmol/L (126 mg/dL)], reduced the rate of serious perinatal complications (a composite of death, shoulder dystocia, nerve palsy, and fracture) compared to routine care (1% vs 4%; P = 0.01). In addition, such interventions were associated with a reduced incidence of macrosomia (10% vs 21%; P < 0.001), preeclampsia (12% vs 18%; P = 0.02), and improved maternal health-related quality of life ( 28 ).
In 2009, the MFMU trial (n = 958) reported that treatment of “mild” GDM was also associated with improved outcomes ( 29 ). Following a positive GCT between 24 and 30 + 6 weeks’ gestation, “mild” GDM was defined on a positive 100-g 3-hour OGTT by a fasting glucose < 5.3 mmol/L (95 mg/dL), and at least 2 postload glucose thresholds that exceeded the 2000 ADA diagnostic thresholds [1-, 2-, or 3-hour thresholds 10.0 mmol/L (180 mg/dL), 8.6 mmol/L (155 mg/dL), and 7.8 mmol/L (140 mg/dL), respectively]. Women with previous GDM were excluded from the study. Dietary intervention, SMBG, and insulin therapy, if required, to achieve a fasting glucose target < 5.3 mmol/L (95 mg/dL) and 2-hour postprandial glucose target < 6.7 mmol/L (121 mg/dL) was associated with reduced rates of macrosomia (5.9% vs 14.3%; P < 0.001), LGA (7.1% vs 14.5%; P < 0.001), shoulder dystocia (1.5% vs 4.0%; P = 0.02), cesarean section (26.9% vs 33.8%; P = 0.02), and preeclampsia and gestational hypertension (8.6% vs 13.6%; P = 0.01) compared to routine care. However, the intervention did not lead to a significant difference in the primary composite outcome of stillbirth, perinatal death, and neonatal complications (hyperbilirubinemia, hypoglycemia, hyperinsulinemia, and birth trauma) ( 29 ). Treatment targets in the MFMU trial were lower than that of the ACHOIS trial, and whether this may account for the reduction in cesarean section not shown in the ACHOIS trial is unclear. These key findings, supported by other studies ( 22 , 284 ), were highlighted by the IADPSG to support the lowering of the GDM diagnostic criteria and treating mild hyperglycemia ( 30 ).
A recent Cochrane review (8 RCTs; n = 1418) reported that GDM treatment, including dietary intervention and insulin therapy, reduced a composite outcome of perinatal morbidity (death, shoulder dystocia, bone fracture, and nerve palsy) by 68% compared to routine antenatal care ( 285 ). Treatment was also associated with reductions in macrosomia, LGA, and preeclampsia but an increase in IOL and neonatal intensive care admission.
The main objective of GDM management is to attain maternal normoglycemia because evidence suggests that excessive fetal growth can be attenuated by maintaining near normal glucose levels ( 286 , 287 ). The foundation of this approach is medical nutrition therapy. Given carbohydrates are the primary determinant of maternal postprandial glucose levels, current dietary practice aims to modify carbohydrate quality (glycemic index) and distribution ( 32 , 288 , 289 ). The original nutritional approach for GDM decreased total carbohydrate intake to 33% to 40% of total energy intake (EI) and was associated with reduced postprandial glycemia and fetal overgrowth ( 290 ). More recent evidence suggests that higher carbohydrate intake and quality (lower glycemic index) between 60% and 70% EI can also limit maternal hyperglycemia ( 291-293 ). Nevertheless, there remain limited data to support a specific dietary intervention for GDM ( 294 ). A recent meta-analysis (18 RCTs; n = 1151) showed that enhancing nutritional quality (modified dietary intervention, defined as a dietary intervention different from the usual one used in the control group) after GDM diagnosis, irrespective of the specific dietary approach, improved maternal fasting and postprandial glycemia, and reduced pharmacotherapy requirements, birthweight, and macrosomia ( 295 ).
Guidelines therefore currently recommend a range of carbohydrate intake between 33% and 55% EI ( 32 , 288 , 289 ). Studies have reported improved pregnancy outcomes in GDM with both lower carbohydrate (42%E) and high‐carbohydrate (55%E) diets ( 296 ), reflected in the most recent Academy of Nutrition and Dietetics guidelines, which state that beneficial effects on pregnancy outcomes in GDM are seen with a range of carbohydrate intakes ( 288 ). The IOM guidelines recommend a carbohydrate intake of at least 175 g/day and a total daily caloric intake of 2000 to 2500 kilocalories during pregnancy ( 289 ). The ACOG recommends a lower carbohydrate diet (33-40%E) ( 297 ). However, the ADA has raised concerns over the corresponding higher maternal fat intake, fetal lipid exposure, and overgrowth resulting from lowering carbohydrate intake ( 298 ) and withdrew specific dietary guidelines for GDM in 2005 ( 299 ).
Given maternal glucose primarily supports fetal growth and brain development ( 300 ), theoretically if the maternal diet is too low in carbohydrate, the maternal-fetal glucose gradient may be compromised. Restriction of total maternal EI is associated with reduced fetal growth ( 301 ). A recent systematic review similarly showed that lower carbohydrate intake correlated with lower birthweight and greater incidence of SGA ( 302 ), with a lower carbohydrate threshold of 47% EI associated with appropriate fetal growth ( 302 , 303 ). Importantly, the lower carbohydrate threshold independent of energy restriction in GDM is yet to be established. Related safety concerns with lower carbohydrate diets include the potential risk of higher fetal exposure to maternal ketones ( 304 ) and micronutrient deficiency ( 305 , 306 ). In vitro studies have shown that ketones suppress trophoblast uptake of glucose, jeopardizing glucose transfer across the placenta ( 307 ). Clinically, a prospective US cohort study of women with preexisting diabetes, GDM, or normal glucose tolerance demonstrated an inverse correlation between higher maternal third trimester beta-hydroxybutyrate and FFAs and lower offspring intellectual development scores at 2 to 5 years of age, although total carbohydrate, EI, and maternal BMI were not reported ( 304 ).
The IOM has published recommendations for weight gain during pregnancy based on prepregnancy BMI ( 289 ), but no specific recommendations for weight gain in GDM exist ( 286 ). In women with overweight or obesity, studies have suggested that weight reduction or gain ≤ 5 kg increased the risk of SGA ( 308 ). A recent systematic review based on data from almost 740 000 women demonstrated that GWG of 5 kg to 9 kg in women with class I obesity (BMI 30-34.99 kg/m 2 ), 1 to <5 kg for class II obesity (35-39.99 kg/m 2 ), and no GWG for women with class III obesity (BMI ≥ 40kg/m 2 ), minimized the combined risk of LGA, SGA, and cesarean section ( 309 ).
A meta-analysis (n = 88 599) evaluating the relationship between GWG and pregnancy outcomes in GDM specifically showed that GWG greater than the IOM recommendations was associated with an increased risk of pharmacotherapy, as well as of hypertensive disorders of pregnancy, cesarean section, LGA, and macrosomia ( 310 ). GWG below the IOM recommendations was protective for LGA (RR 0.71; 95% CI 0.56-0.90) and macrosomia (RR 0.57; 95% CI 0.40-0.83) and did not increase the risk of SGA (RR 1.40; 95% CI 0.86-2.27) ( 289 ). This suggests that GWG targets in GDM may need to be lower than the current recommendations for normal pregnancy. However, from a practical perspective, only 30% of women gained less than the recommended IOM GWG targets ( 310 ).
Fasting and postprandial glucose testing with either the 1- or 2-hour postprandial glucose value is recommended in women with GDM. The 1-hour postprandial glucose approximates to the peak glucose excursion in pregnancy in women without diabetes and those with type 1 diabetes ( 175 ). Studies have shown that the 1-hour postprandial peak glucose level correlates with amniotic fluid insulin levels, reflecting fetal hyperinsulism ( 311 ) and with fetal abdominal circumference in women with type 1 diabetes ( 286 ). An RCT that compared pre- to postprandial maternal SMBG values showed that titrating insulin therapy based on the 1-hour postprandial values was associated with improved maternal glycemic control and may better attenuate the risk of neonatal complications attributed to fetal hyperinsulinemia ( 312 ).
Treatment targets based on maternal SMBG levels vary internationally ( Table 7 ). There is some suggestion that lower glucose targets may improve pregnancy outcomes in GDM ( 176 , 313 , 314 ), but this is yet to be evaluated in adequately powered RCTs. Conversely, lower glycemic targets may be associated with an increased risk of SGA ( 315-317 ) and maternal and fetal hypoglycemia ( 318 , 319 ). A small study evaluating stringent glycemic targets in 180 women with GDM failed to demonstrate additional benefits, with no differences in the rates of cesarean section, birthweight, macrosomia, or SGA in the offspring of women randomized to intensive [preprandial glucose ≤ 5.0 mmol/L (90 mg/dL) and 1-hour postprandial glucose ≤ 6.7 mmol/L (121 mg/dL)] compared to standard treatment targets [preprandial glucose ≤ 5.8 mmol/L (104.5 mg/dL) and 1-hour postprandial glucose ≤ 7.8 mmol/L (140 mg/dL)] ( 320 ).
Recommended glycemic treatment targets in GDM
| . | Fasting plasma glucose (mmol/L) . | Preprandial plasma glucose (mmol/L) . | 1-hour post-prandial plasma glucose (mmol/L) . | 2-h post-prandial plasma glucose (mmol/L) . |
|---|---|---|---|---|
| ADIPS ( ) | ≤5.0 | ≤7.4 | ≤6.7 | |
| ADA ( ) CDA ( ) | ≤5.3 | ≤7.8 | ≤6.7 | |
| NICE ( ) | <5.3 | <7.8 | <6.4 | |
| ACHOIS ( ) | 3.5-5.5 | ≤5.5 | ≤7.0 | |
| MFMU ( ) | <5.3 | <6.7 |
| . | Fasting plasma glucose (mmol/L) . | Preprandial plasma glucose (mmol/L) . | 1-hour post-prandial plasma glucose (mmol/L) . | 2-h post-prandial plasma glucose (mmol/L) . |
|---|---|---|---|---|
| ADIPS ( ) | ≤5.0 | ≤7.4 | ≤6.7 | |
| ADA ( ) CDA ( ) | ≤5.3 | ≤7.8 | ≤6.7 | |
| NICE ( ) | <5.3 | <7.8 | <6.4 | |
| ACHOIS ( ) | 3.5-5.5 | ≤5.5 | ≤7.0 | |
| MFMU ( ) | <5.3 | <6.7 |
Abbreviations: ACHOIS, Australian Carbohydrate Intolerance Study in Pregnant Women Study; ADA, American Diabetes Association; ADIPS, Australasian Diabetes in Pregnancy Society; CDA, Canadian Diabetes Association; NICE, UK National Institute for Health and Care Excellence; MFMU, National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network.
Insulin has traditionally been the preferred treatment for GDM if maternal glucose levels remain elevated on medical nutrition therapy ( 267 ). Depending on targets, approximately 50% of women with GDM are prescribed insulin therapy to maintain normoglycemia ( 321 , 322 ), with a combination of evening intermediate-acting insulin if fasting glucose levels are elevated and mealtime rapid-acting insulin when indicated. Additional daytime intermediate-acting insulin may also be needed to control prelunch or predinner hyperglycemia.
Decreasing insulin doses in the third trimester may simply reflect the physiological increase in maternal insulin sensitivity observed at this stage of pregnancy ( 176 , 323 ). However, substantial insulin dose reduction, recurrent maternal hypoglycemia, and/or slowing of fetal growth or preeclampsia may indicate underlying pathophysiological placental insufficiency ( 324 ), impacting the timing of delivery and intensity of obstetric monitoring.
Risk factors for insulin therapy include earlier diagnosis of GDM ( 81 ), the pattern and degree of elevation of the 75-g 2-hour OGTT diagnostic glucose thresholds ( 325 ), and ethnicity ( 325 ). Other risk factors including gestational age and HbA1c level at the time of GDM diagnosis, BMI, and family history of diabetes account for only 9% of the attributable risk for insulin therapy ( 321 ). A recent Australian study found that maternal age > 30 years, family history of diabetes, prepregnancy obesity, previous GDM, early diagnosis of GDM, fasting glucose ≥ 5.3 mmol/L (96 mg/dL) and HbA1c ≥ 5.5% (37 mmol/mol) at diagnosis were all independent predictors for insulin therapy ( 326 ). Insulin usage could also be estimated according to the number of predictors present, with up to 93% of women with 6 to 7 predictors using insulin therapy compared with less than 15% of women with 0 to 1 predictors ( 326 ).
Oral pharmacotherapy options include glyburide and metformin. Oral pharmacotherapy is associated with improved cost effectiveness, compliance, and acceptability compared to insulin therapy ( 327 ). However, there are issues regarding efficacy and safety, particularly longer term, and thus insulin is generally preferred as first-line pharmacotherapy following lifestyle intervention.
Glyburide is commonly prescribed as first-line therapy for GDM in the United States ( 328 ). An early study evaluating the efficacy of glyburide vs insulin therapy in 404 women with GDM reported no differences in maternal glucose levels or neonatal outcomes between the treatment groups ( 329 ). However, subsequent studies show that approximately 20% of women treated with glyburide required additional insulin therapy to achieve adequate maternal glycemia ( 330 ). Moreover, a large retrospective US study of almost 111 000 women with GDM, in which 4982 women were treated with glyburide and 4191 women were treated with insulin, reported that glyburide was associated with an increased risk of neonatal complications including neonatal intensive care admission, respiratory distress syndrome, hypoglycemia, birth injury, and LGA compared to insulin therapy ( 331 ). Although transplacental transfer of glyburide to the fetus is highly variable, it can reach 50% to 70% of maternal plasma concentration ( 332 ), potentially causing direct stimulation of fetal insulin production ( 333 ).
The use of metformin in pregnancy continues to rise ( 334 ). However, its use remains controversial, due to the potential concerns regarding long-term metabolic programming effects of placental transfer of metformin to the fetus, with some studies suggesting similar plasma concentrations of metformin in the maternal and fetal circulation ( 335 ). A recent systematic review and meta-analysis of 28 studies (n = 3976) evaluating growth in offspring of women with GDM exposed to metformin compared to insulin therapy found that neonates exposed to metformin had lower birthweights (mean difference −107.7 g; 95% CI −182.3 to −32.7), decreased risk of LGA (OR 0.78; 95% CI 0.62-0.99), and macrosomia (OR 0.59; 95% CI 0.46-0.77) and lower ponderal indices than neonates whose mothers were treated with insulin ( 336 ). No difference in the risk of SGA was found, in contrast to outcomes in women with type 2 diabetes, with the Metformin in Women with Type 2 Diabetes RCT observing more than double the rate of SGA (95% CI 1.16-3.71) in the metformin treated cohort, in association with lower insulin doses, HbA1c, and GWG ( 337 ). Offspring of women with GDM exposed to metformin also demonstrate accelerated postnatal growth at 18 to 24 months of age (2 studies; n = 411; mean difference in weight 440 g; 95% CI 50-830), resulting in higher BMI at 5 to 9 years of age (3 studies; n = 520; BMI mean difference 0.78 kg/m 2 , 95% CI 0.23-1.33) ( 336 ).
The Metformin in Gestational Diabetes trial randomized 751 women to receive either metformin or insulin therapy, finding no significant difference in the composite neonatal outcome of neonatal hypoglycemia, respiratory distress syndrome, hyperbilirubinemia, low Apgar scores, birth trauma, and preterm birth ( 322 ). There was a trend toward increased preterm birth and decreased maternal GWG in women treated with metformin, while severe neonatal hypoglycemia was highest in those treated with insulin. Almost 50% of women treated with metformin required the addition of insulin therapy ( 322 ). Other studies have reported that between 14.0% and 55.8% of women treated with metformin also require insulin therapy to achieve optimal glycemic control ( 338 , 339 ). The Metformin in Gestational Diabetes: The Offspring Follow-Up 2-year follow-up study found that children exposed to metformin had increased subcutaneous fat localized to the arm compared with children whose mothers were treated with insulin alone ( 340 ). By 7 and 9 years of age the children exposed to metformin had similar offspring total and abdominal body fat percentage and metabolic biochemistry including fasting glucose, insulin, and lipids but were larger overall based on measures including weight, arm and waist circumference, waist-to-height ratio, and dual-energy X-ray absorptiometry fat mass and lean mass ( 341 ). These findings are consistent with a recent follow-up study of metformin therapy in pregnant women with polycystic ovary syndrome, which showed that children exposed to metformin in utero had higher BMI and rates of overweight and obesity at 4 years of age ( 342 ).
A recent Cochrane review (8 RCTs; n = 1487) evaluating the use of metformin, glyburide, and acarbose in women with GDM found that the benefits and potential harms of these therapies in comparison to each other are unclear ( 343 ). Other meta-analyses comparing glyburide, metformin, and insulin have shown that metformin was associated with lower GWG, gestational hypertension, and postprandial maternal glucose levels compared to either glyburide or insulin ( 344 , 345 ), but metformin was associated with an increased risk of preterm birth compared to insulin ( 345 ). Compared to metformin, glyburide was associated with a higher risk of increased birthweight, LGA, macrosomia, neonatal hypoglycemia, and increased GWG ( 344 ). More recently, a small RCT (n = 104) suggested that glyburide and metformin were comparable in terms of maternal glycemia and perinatal outcomes ( 346 ). Treatment success after second-line (oral) therapy was higher in the (first-line) metformin vs glyburide cohort (87% vs 50%; P = 0.03), suggesting that metformin may be the preferred first-line therapy. Overall, most women required either a combination of metformin and glyburide to achieve glycemic control and/or replacement of first-line oral therapy due to hypoglycemia and gastrointestinal side effects, suggesting neither agent alone is likely to be successful in most women with GDM. Combined oral pharmacotherapy had an efficacy rate of 89%, with only 11% of women required third-line therapy with insulin ( 346 ). However, the effects of dual oral therapy crossing the placenta on long-term potential fetal programming via their effects on cellular metabolism, hepatic gluconeogenesis, and insulin sensitivity (metformin) ( 347 ) and fetal hyperinsulinemia (glyburide) is unknown ( 348 ).
A recent Cochrane review consisting of only 3 small RCTs (n = 524) reported insufficient (very low certainty) evidence to evaluate the use of fetal biometry in guiding the medical management of GDM ( 349 ). Nevertheless, serial fetal growth ultrasounds, particularly assessing fetal abdominal circumference, are potentially useful in guiding the intensity of maternal glucose targets and insulin therapy ( 350-352 ). Studies have demonstrated that neonates with an estimated fetal weight ≥ 75th percentile on early third trimester ultrasound were 10-fold more likely to be LGA compared to neonates with an estimated fetal weight < 75th percentile ( 353 ). Measured fetal abdominal circumference < 90th percentile on 2 ultrasounds at 3- to 4-week intervals has also been shown to provide high reliability in excluding the risk of LGA ( 351 ). Moreover, a recent retrospective study (n = 275) found that estimated fetal weight or abdominal circumference up to the 30th percentile on third trimester ultrasound was associated with a greater risk of adverse neonatal outcomes, comparable to that observed with abdominal circumference or estimated fetal weight > 95th percentile in women with hyperglycemia in pregnancy (including GDM) ( 354 ). These findings suggest the potential utility of fetal biometry at thresholds other than defining SGA or LGA in identifying higher risk pregnancies in GDM.
The optimal timing of delivery in GDM is complex, guided by maternal glycemic control in addition to maternal and fetal factors, and has not been definitively established. Current guidelines recommend delivery by 40 + 6 weeks’ gestation in low-risk women with GDM managed with diet alone and from 39 + 0 to 39 + 6 weeks’ gestation for women with GDM well controlled with therapy ( 38 , 277 , 355 ). A recent Canadian population-based cohort study examining the week-specific risks of severe pregnancy complications in women with diabetes included 138 917 women with GDM and 2 553 243 women without diabetes over a 10-year period ( 356 ). There was no significant difference in gestational age-specific maternal mortality or morbidity (defined as ≥1 of the following in the immediate perinatal period: obstetric embolism, obstetric shock, postpartum hemorrhage with hysterectomy or other procedures to control bleeding, sepsis, thromboembolism, or uterine rupture) between iatrogenic delivery and expectant management in women with GDM. However, iatrogenic delivery was associated with an increased risk of neonatal mortality and morbidity (birth or fetal asphyxia, grade 3 or 4 intraventricular hemorrhage, neonatal convulsions, other disturbances of cerebral status of newborn, respiratory distress syndrome, birth injury, shoulder dystocia, stillbirth or neonatal death) at 36 to 37 weeks’ gestation (76.7 and 27.8 excess cases per 1000 deliveries, respectively) but a lower risk of neonatal morbidity and mortality at 38 to 40 weeks’ gestation (7.9, 27.3, and 15.9 fewer cases per 1000 deliveries, respectively) compared with expectant management, suggesting that delivery at 38, 39, or 40 weeks’ gestation may provide the best neonatal outcomes in women with GDM ( 356 ).
Up to one third of women with GDM diagnosed by pre-IADPSG criteria will have glucose levels consistent with diabetes or prediabetes on postpartum testing at 6 to 12 weeks ( 357 ). Thus, a repeat OGTT or fasting glucose as early as 6 to 12 weeks’ postpartum is recommended to confirm maternal glucose status ( 41 , 277 ). Only around 25% of women are tested at this time point with compliance with postpartum testing ranging between 23% and 58% ( 357 , 358 ). In women with GDM with overweight or obesity, a reduction in interpregnancy BMI of ≥2.0 kg/m 2 reduces the risk of subsequent GDM by 74% ( 359 ). Longer term, women should perform regular cardiometabolic health assessment and optimization of lifestyle measures to reduce their greater risk of type 2 diabetes and cardiovascular disease ( 282 , 360 , 361 ). Up to 74% of women with obesity and previous GDM develop type 2 diabetes compared with <25% of women who achieve a normal BMI postpartum following GDM ( 362 ). It is unclear how relevant these studies in older women are for current clinical care given recent data that 50% of women develop type 2 diabetes within 5 to 10 years post-GDM diagnosis ( 273 ). The Diabetes Prevention Program demonstrated that lifestyle intervention and metformin therapy improved insulin sensitivity and preserved β-cell function in women with a history of previous GDM ( 363 ). Early type 2 diabetes prevention following GDM is therefore an essential component of the contemporary GDM detection and management paradigm ( 276 ).
Importantly, despite a reduction in the risk of macrosomia at birth, the ACHOIS and MFMU follow-up studies did not demonstrate a beneficial impact on childhood obesity and glucose tolerance at 5 to 10 years of age in the offspring of women who received treatment for maternal hyperglycemia ( 364 , 365 ). Other prospective cohort studies similarly suggest that the offspring of women with treated GDM still have a greater risk of obesity, type 2 diabetes, the metabolic syndrome, and cardiovascular disease from early childhood and adolescence ( 258 , 366-380 ). For example, a 2017 Danish National Birth Cohort study (n = 561) reported increased adiposity, an adverse cardiometabolic profile, and earlier onset puberty among adolescent females of women with GDM ( 381 ). A prospective offspring cohort study of women with GDM who achieved good antenatal glycemic control demonstrated that offspring adiposity (adipose tissue quantity measured using magnetic resonance imaging) was similar in the GDM and normal glucose tolerance groups within 2 weeks postpartum but was 16.0% greater (95% CI 6.0-27.1; P = 0.002) by 2 months of age ( 382 ). The mechanism for this greater adiposity and rapid weight gain in early infancy is uncertain given both groups were predominantly breastfed. Consistent with the ACHOIS and MFMU follow-up studies ( 364 , 365 ), these data suggest that the current approach to glycemic control in GDM may not mitigate its impact on longer term infant health. Further, this pathway may be potentially mediated by excess infant adiposity, which correlates with childhood adiposity ( 383 ). Table 8 presents practical tips for managing women with GDM.
Practical tips for managing women with GDM
| Period . | Tips . |
|---|---|
| Preconception | All women should be encouraged to plan for pregnancy. Optimize modifiable risk factors prior to pregnancy (eg. BMI, diet, physical activity). Glucose assessment in high-risk women to detect undiagnosed preexisting glucose intolerance or diabetes. |
| During pregnancy | All pregnant women should be encouraged to have a nutritionally dense diet and undertake regular exercise during pregnancy unless there are obstetric contraindications. All pregnant women should be given personalized gestational weight gain targets and have their weight monitored at clinical reviews. High-risk women who have not undergone prepregnancy glucose assessment should be tested early for diabetes in pregnancy. Test all pregnant women without known diabetes/early GDM for GDM at 24 to 28 weeks’ gestation according to recommended screening and diagnostic criteria. GDM management ideally involves a multidisciplinary team with regular diabetes and obstetric assessment and includes patient education, lifestyle modification and support. Women should monitor their blood glucose levels. Pharmacotherapy, usually insulin, should be commenced if glucose levels are elevated despite lifestyle optimization. Metformin can be considered unless there are concerns with inadequate fetal growth. Timing of delivery is an individualized decision based on maternal and fetal well-being in addition to maternal glycemic control. |
| Postpartum | Early postpartum OGTT to assess glucose status. Regular long-term follow-up focused on diabetes and vascular risk factor modification and assessment to reduce subsequent risk of GDM, diabetes, and cardiovascular disease. Family lifestyle support, which includes optimizing diet, physical activity, and weight in the offspring. |
| Period . | Tips . |
|---|---|
| Preconception | All women should be encouraged to plan for pregnancy. Optimize modifiable risk factors prior to pregnancy (eg. BMI, diet, physical activity). Glucose assessment in high-risk women to detect undiagnosed preexisting glucose intolerance or diabetes. |
| During pregnancy | All pregnant women should be encouraged to have a nutritionally dense diet and undertake regular exercise during pregnancy unless there are obstetric contraindications. All pregnant women should be given personalized gestational weight gain targets and have their weight monitored at clinical reviews. High-risk women who have not undergone prepregnancy glucose assessment should be tested early for diabetes in pregnancy. Test all pregnant women without known diabetes/early GDM for GDM at 24 to 28 weeks’ gestation according to recommended screening and diagnostic criteria. GDM management ideally involves a multidisciplinary team with regular diabetes and obstetric assessment and includes patient education, lifestyle modification and support. Women should monitor their blood glucose levels. Pharmacotherapy, usually insulin, should be commenced if glucose levels are elevated despite lifestyle optimization. Metformin can be considered unless there are concerns with inadequate fetal growth. Timing of delivery is an individualized decision based on maternal and fetal well-being in addition to maternal glycemic control. |
| Postpartum | Early postpartum OGTT to assess glucose status. Regular long-term follow-up focused on diabetes and vascular risk factor modification and assessment to reduce subsequent risk of GDM, diabetes, and cardiovascular disease. Family lifestyle support, which includes optimizing diet, physical activity, and weight in the offspring. |
Abbreviations: GDM, gestational diabetes mellitus; OGTT, oral glucose tolerate test.
Precision medicine seeks to improve diagnostics, prognostics, prediction, and therapeutics in diabetes, including GDM, by evaluating and translating various biological axes including metabolomics, genomics, lipidomics, proteomics, technology, clinical risk factors and biomarkers, and mathematical and computer modeling into clinical practice ( 384 ). The Precision Medicine in Diabetes Initiative was launched in 2018 by the ADA, in partnership with the European Association for the Study of Diabetes, with their first consensus report published in 2020 ( 384 ).
In GDM, precision medicine represents the increasing understanding of heterogeneity within its genotype and phenotype ( 170 , 385-388 ) to identify and translate subclassification of GDM into more personalized clinical care ( 388 ). For example, physiologic subtypes of GDM based on the underlying mechanisms leading to maternal hyperglycemia have been recently characterized ( 386 ). Among 809 women from the Genetics of Glucose Regulation in Gestation and Growth pregnancy cohort, heterogeneity in the contribution of insulin resistance and deficiency to GDM were characterized based on validated indices of insulin sensitivity and secretory response measured during the 75-g OGTT performed between 24 and 30 weeks’ gestation ( 388 ). Compared to women with normal glucose tolerance, women with insulin resistant GDM (51% of GDM) had higher BMI and fasting glucose, hypertriglyceridemia, and hyperinsulinemia, larger infants, and almost double the risk of GDM-associated pregnancy complications. In contrast, women with predominantly insulin secretion defects had comparable BMI, fasting glucose, infant birthweight, and risk of adverse outcomes to those with normal glucose tolerance ( 388 ).
Other studies have also suggested that greater insulin resistance in GDM carries a higher risk of perinatal complications ( 389 ). A recent multicenter prospective study of 1813 women evaluating subtypes of GDM based on insulin resistance ( 389 ) found that women with GDM and high insulin resistance [n = 189 (82.9%)] had a higher BMI, systolic blood pressure, fasting glucose, and lipid levels in early pregnancy compared to women with normal glucose tolerance or those diagnoses with insulin-sensitive GDM. Insulin-sensitive women with GDM [n = 39 (17.1%)] had a significantly lower BMI than women with normal glucose tolerance but similar blood pressure, early pregnancy fasting glucose and lipid levels, and pregnancy outcomes. Despite no differences in insulin treatment and early postpartum glucose intolerance among the GDM subtypes, women with GDM and high insulin resistance had a greater than 2-fold risk of preterm birth and an almost 5-fold increased risk of neonatal hypoglycemia compared with women with normal glucose tolerance. This suggests the high insulin resistance GDM subtype has a greater risk of pregnancy complications potentially arising from the resultant fetal hyperinsulinemia ( 389 ).
The contemporary precision medicine approach to GDM also includes the increasing exploration of early pregnancy risk prediction and risk management models ( 390 ). The traditional binary clinical risk factor approach to identifying women at high risk in early pregnancy is limited by poor sensitivity and specificity, with studies showing that clinical risk factor-based screening fails to identify 10% to over 30% of women with GDM ( 391-396 ). The Pregnancy Outcome for Women with Pre-gestational Diabetes Along the Irish Atlantic Seaboard study found that the prevalence of women with GDM who had no risk factors was low, ranging from 2.7% to 5.4% ( 397 ). However, despite the absence of risk factors, these women with GDM had more pregnancy complications than those with normal glucose tolerance ( 397 ). Other studies have also reported that women without risk factors diagnosed with GDM have comparable pregnancy outcomes to women with GDM identified as high risk ( 393 ). Thus, clinical risk factors alone are not predictive of GDM risk for all women. Although some improvement in the predictive accuracy for GDM is seen in clinical risk scoring approaches ( 158 , 398 ), greater improvement via multivariate risk prediction and mathematical or computer models combining clinical risk factors and biomarkers have been reported in the GDM research setting ( 154-156 , 399-403 ).
Biomarkers are defined as a biological observation that substitutes and ideally predicts the clinically relevant endpoint (ie, GDM) ( 404 ). Biomarker discovery and application in the early detection of GDM has become a major research area. However, few biomarkers are specific enough for clinical application ( 405 ). Most novel biomarkers with potential utility for the prediction of GDM are involved in pathophysiological pathways related to insulin resistance, dyslipidemia, and type 2 diabetes ( 402 , 406 ) but are frequently mediated by maternal obesity ( 240 , 407 ). Early pregnancy risk prediction models for GDM combining clinical risk factors and biomarkers have included various measures of maternal glucose, lipids, adipokines, inflammatory markers, and pragmatic aneuploidy and preeclampsia screening markers, with model performance (area under the curve) up to 0.91 ( 153 , 154 , 399 , 402 , 403 , 408-416 ). Limitations to the clinical application of novel biomarkers and model performance include heterogeneity in the testing approach to GDM and cohort characteristics, potential overestimation of model performance due to overfitting of the data to the index study population, the lack of external clinical validation studies, and limited regulatory guidance for validating biomarker assays ( 405 ).
The COVID-19 pandemic has led to dynamic changes in the testing approach and model of care for women with GDM to minimize the risk of virus transmission and because of decreased clinical capacity. Several temporary pragmatic diagnostic strategies have been suggested as an alternative to the OGTT, including measurement of fasting plasma glucose, random plasma glucose, and HbA1c ( 417-419 ). A secondary analysis of 5974 women from the HAPO study ( 420 ), reported that the UK, Canadian, and Australian COVID-19–modified diagnostic approaches reduced the frequency of GDM by 81%, 82%, and 25%, respectively. Short-term pregnancy complications in the subgroup of women now with undiagnosed GDM (“missed GDM”) were comparable to women diagnosed with GDM based on the Canadian-modified diagnostic criteria, slightly lower for the UK-modified criteria, but significantly lower for the Australasian Diabetes in Pregnancy Association–modified criteria. While all approaches recommend universal testing, the Australian approach adopts a lower fasting glucose threshold of 4.7 mmol/L to identify women who require an OGTT and does not include HbA1c measurement ( 420 ). A retrospective UK study of over 18 000 women sought to define evidence-based recommendations for pragmatic GDM testing during the COVID-19 pandemic ( 421 ), reporting that ~5% of women would be identified as GDM based on a random glucose threshold ≥ 8.5 mmol/L (153 mg/dL) at 12 weeks’ gestation and fasting glucose ≥ 5.2 to 5.4 mmol/L (94-97 mg/dL) or HbA1c ≥ 5.7% (39 mmol/mol) measured at 28 weeks’ gestation. Each test predicted some, but not all, obstetric and perinatal complications, lacking the sensitivity of the OGTT for the diagnosis of GDM but overall may provide adequate risk stratification where the OGTT is not feasible ( 421 ).
GDM is one of the most common complications of pregnancy and is increasing in global prevalence. Diagnosing GDM is important because perinatal complications and stillbirth risk are reduced by treatment. Despite the benefit of identifying and treating GDM, much of the current (short-term) diagnostic and management approach to GDM remains contentious. These differences confound interpretation and application of trial data, preventing a single standard international approach to GDM.
Recent data indicates near normal birthweight and maternity population outcomes in women with GDM based on modern IADPSG criteria in developed countries, demonstrating that even treatment of “milder” maternal hyperglycemia improves pregnancy outcomes. However, most cases of GDM occur in low- and middle-income countries where perinatal risks are far greater and universal 1-step testing may be more practical. There are limited RCT data to guide diagnosis and management in this setting, and further evidence is urgently needed. In developed countries including the United Kingdom, the main issue arguably does not pertain to women diagnosed with GDM but rather high-risk women who remain unscreened (associated with factors such as lower socioeconomic status and higher BMI) who are at highest risk of stillbirth ( 74 ).
The background to the various GDM diagnostic criteria is informative in demonstrating that no approach clearly separates risk groups. It is also now evident that a continuum of risk for GDM exists based on both the timing and degree of maternal hyperglycemia. This underscores the difficulty of defining absolute glucose thresholds at a single timepoint in pregnancy for the diagnosis of GDM and is confounded further by variation in glucose measurement due to preanalytical glucose processing and reproducibility issues. Thus, current diagnostic glucose thresholds for GDM must inevitably reflect compromise and consensus.
A precision medicine approach that recognizes GDM subtype and heterogeneity, enhanced by further research into the genetics of GDM and validation of novel biomarkers and new technologies such as continuous glucose monitoring may improve risk stratification, optimize clinical models of care, and facilitate more individualized and consumer-friendly detection and treatment strategies.
The recent HAPO-FUS data confirming the long-term impact of maternal hyperglycemia on maternal and offspring metabolic health ( 227 , 262 ) highlight an important paradigm shift. The approach to GDM should reflect an evidence base that evaluates diagnostic glucose thresholds and measurement within a framework that includes timing of detection and treatment trials with long-term clinical and health economic outcomes. For example, if the ongoing Treatment of Booking Gestational Diabetes Mellitus trial demonstrates a benefit for early GDM detection and treatment, there are implications for the prevailing diagnostic GDM glucose thresholds in later pregnancy. This is because these thresholds were derived from the risk of perinatal complications in a heterogeneous GDM cohort, which included women who would fulfill early GDM criteria.
Other important areas for research include the evaluation of dietary interventions establishing the optimal carbohydrate threshold in GDM, further clarity on the potential long-term impact of intrauterine metformin on the offspring, as well as the efficacy of preconception and early pregnancy preventive strategies targeting risk factors other than glycemia, such as maternal obesity and GWG. Improved obstetric assessment of placental function, especially in late pregnancy, to inform timing of delivery and identify women at highest risk of stillbirth in GDM is also needed.
The complications of GDM may indeed be greater based on the severity of maternal glycemia and associated vascular risk factors. Nevertheless, the traditional focus on diagnostic criteria and short-term antenatal maternal glucose management fails to address the importance of identifying “milder” (IADPSG-defined) GDM as a risk factor for future maternal and offspring diabetes and CVD risk. It should also be apparent that the increasing prevalence of GDM largely reflects the worsening metabolic health burden including prediabetes and obesity in women of childbearing age. The clinical focus for GDM must therefore urgently shift to early postnatal prevention strategies to decrease the progression from GDM to type 2 diabetes and address longer term maternal and offspring cardiometabolic risk post-GDM via a life course management approach.
A.S. was supported by an NHMRC Fellowship Grant (GNT1148952).
A.S., J.W., H.M., and G.P.R. have nothing to declare.
Bennewitz H. De Diabete Mellito, Gravidatatis Symptomate . MD thesis, University of Berlin ; 1824 .
Google Scholar
Google Preview
Barker DJP. Mothers Babies and Diseases in Later Life. BMJ ; 1994 .
Duncan J . On puerperal diabetes . Trans Obstet Soc Lond. 1882 ; 24 : 256-285 .
Miller HC . The effect of diabetic and prediabetic pregnancies on the fetus and newborn infant . J Pediatr. 1946 ; 29 ( 4 ): 455 - 461 .
Williams J . The clinical significance of glycosuria in pregnant women . Am J Med Sci. 1909 ; 137 : 1 - 26 .
O’Sullivan JB , Mahan CM . Criteria for the oral glucose tolerance test in pregnancy . Diabetes. 1964 ; 13 : 278 - 285 .
Coustan DR . Gestational diabetes. In: Harris MI , Cowie CC , Stern MP , Boyko EJ , Reiber GE , Bennett PH , eds. Diabetes in America . National Institute of Health ; 1995 : 703 - 717 .
World Health Organization . Technical Report Series. No 310. Diabetes Mellitus . Report of a WHO Expert Committee. 1965 .
World Health Organization . Technical Report Series. No 646. Second Report on Diabetes Mellitus . Report of a WHO Expert Committee. 1980 .
World Health Organization . Technical Report Series. No 727. Second Report on Diabetes Mellitus . Report of a WHO Expert Committee. 1985 .
World Health Organisation . Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization guideline . Diabetes Res Clin Pract. 2014 ; 103 ( 3 ): 341 - 363 .
O’Sullivan JB , Mahan CM , Charles D , Dandrow RV . Screening criteria for high-risk gestational diabetic patients . Am J Obstet Gynecol. 1973 ; 116 ( 7 ): 895 - 900 .
National Diabetes Data Group . Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance . Diabetes. 1979 ; 28 ( 12 ): 1039 - 1057 .
American College of Obstetricians and Gynecologists . Management of Diabetes Mellitus During Pregnancy . Technical Bulletin No. 92. 1986 .
American Diabetes Association . Gestational diabetes mellitus . Diabetes Care. 1986 ; 9 ( 4 ): 430 - 431 .
Ferrara A , Hedderson MM , Quesenberry CP , Selby JV . Prevalence of gestational diabetes mellitus detected by the National Diabetes Data Group or the Carpenter and Coustan plasma glucose thresholds . Diabetes Care. 2002 ; 25 ( 9 ): 1625 - 1630 .
Carpenter MW , Coustan DR . Criteria for screening tests for gestational diabetes . Am J Obstet Gynecol. 1982 ; 144 ( 7 ): 768 - 773 .
American Diabetes Association . 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018 . Diabetes Care. 2018 ; 41 ( suppl 1 ): S13 - S27 .
American College of Obstetricians and Gynecologists . Practice Bulletin No. 190: gestational diabetes mellitus . Obstet Gynecol. 2018 ; 131 ( 2 ): e49 - e64 .
American Diabetes Association . Gestational diabetes mellitus . Diabetes Care. 2000 ; 23 ( suppl 1 ): S77 - S79 .
Sermer M , Naylor CD , Farine D , et al. The Toronto tri-hospital gestational diabetes project: a preliminary review . Diabetes Care. 1998 ; 21 ( Suppl 2 ): B33 - B42 .
Sermer M , Naylor CD , Gare DJ , et al. Impact of increasing carbohydrate intolerance on maternal-fetal outcomes in 3637 women without gestational diabetes: the Toronto Tri-Hospital Gestational Diabetes Project . Am J Obstet Gynecol. 1995 ; 173 ( 1 ): 146 - 156 .
Berggren EK , Boggess KA , Stuebe AM , Jonsson Funk M . National Diabetes Data Group vs Carpenter-Coustan criteria to diagnose gestational diabetes . Am J Obstet Gynecol. 2011 ; 205 ( 3 ): 253 e1 - 253.e7 .
Cheng YW , Block-Kurbisch I , Caughey AB . Carpenter-Coustan criteria compared with the National Diabetes Data Group thresholds for gestational diabetes mellitus . Obstet Gynecol. 2009 ; 114 ( 2 Pt 1 ): 326 - 332 .
Chou CY , Lin CL , Yang CK , et al. Pregnancy outcomes of Taiwanese women with gestational diabetes mellitus: a comparison of Carpenter-Coustan and National Diabetes Data Group criteria . J Womens Health (Larchmt). 2010 ; 19 ( 5 ): 935 - 939 .
American Diabetes Association . Gestational diabetes mellitus . Diabetes Care. 2003 ; 26 ( suppl 1 ): S103 - S105 .
Metzger BE , Lowe LP , Dyer AR , et al. ; HAPO Study Cooperative Group. Hyperglycemia and adverse pregnancy outcomes . N Engl J Med. 2008 ; 358 ( 19 ): 1991 - 2002 .
Crowther CA , Hiller JE , Moss JR , et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes . N Engl J Med. 2005 ; 352 ( 24 ): 2477 - 2486 .
Landon MB , Spong CY , Thom E , et al. A multicenter, randomized trial of treatment for mild gestational diabetes . N Engl J Med. 2009 ; 361 ( 14 ): 1339 - 1348 .
Metzger BE , Gabbe SG , Persson B , et al. ; International Association of Diabetes and Pregnancy Study Groups Consensus Panel . International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy . Diabetes Care. 2010 ; 33 ( 3 ): 676 - 682 .
Blumer I , Hadar E , Hadden DR , et al. Diabetes and pregnancy: an Endocrine Society clinical practice guideline . J Clin Endocrinol Metab. 2013 ; 98 ( 11 ): 4227 - 4249 .
Hod M , Kapur A , Sacks DA , et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care . Int J Gynaecol Obstet. 2015 ; 131 ( suppl 3 ): S173 - S211 .
Nankervis A , McIntyre HD , Moses R , et al. ADIPS Consensus Guidelines for the Testing and Diagnosis of Hyperglycaemia in Pregnancy in Australia and New Zealand. Modified November 2014 . http://adips.org/downloads/2014ADIPSGDMGuidelinesV18.11.2014_000.pdf . Accessed June 1, 2021.
Japan Diabetes Society . Evidence-based practice guideline for the treatment for diabetes in Japan 2013 . Last updated November 26, 2020. http://www.jds.or.jp/modules/en/index.php?content_id=44 . Accessed June 1, 2021.
Yang HX . Diagnostic criteria for gestational diabetes mellitus . Chin Med J. 2012 ; 125 ( 7 ): 1212 - 1213 .
Benhalima K , Mathieu C , Damm P , et al. A proposal for the use of uniform diagnostic criteria for gestational diabetes in Europe: an opinion paper by the European Board & College of Obstetrics and Gynaecology (EBCOG) . Diabetologia. 2015 ; 58 ( 7 ): 1422 - 1429 .
Vandorsten JP , Dodson WC , Espeland MA , et al. NIH consensus development conference: diagnosing gestational diabetes mellitus . NIH Consens State Sci Statements. 2013 ; 29 ( 1 ): 1 - 31 .
National Institute for Health and Care Excellence . Diabetes in Pregnancy: Management of Diabetes and its Complications from Pre-conception to the Postnatal Period . NICE Clinical Guideline NG3. 2015 .
Vambergue A . Expert consensus on gestational diabetes mellitus . Diabetes Metab. 2010 ; 36 ( 6 Pt 2 ): 511 .
Associazione Medici Diabetologi and Società Italiana di Diabetologia. Italian National Health System Guidelines for the screening of gestational diabetes mellitus . May 28, 2014. http://www.standarditaliani.it/skin/www.standarditaliani.it/pdf/STANDARD_2014_May28.pdf . Accessed June 1, 2021.
American Diabetes Association . 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2020 . Diabetes Care. 2020 ; 43 ( suppl 1 ): S183 - SS92 .
Canadian Diabetes Association Clinical Practice Guidelines Expert Committee . Clinical practice guidelines for the prevention and management of diabetes in Canada . Canadian J Diabetes. 2013 ; 37(suppl 1):S1-S3 .
Kleinwechter H , Schafer-Graf U , Buhrer C , et al. Gestational diabetes mellitus (GDM) diagnosis, therapy and follow-up care: practice Guideline of the German Diabetes Association (DDG) and the German Association for Gynaecology and Obstetrics (DGGG) . Exp Clin Endocrinol Diabetes. 2014 ; 122 ( 7 ): 395 - 405 .
Seshiah V , Das AK , Balaji V , et al. Gestational diabetes mellitus—guidelines . J Assoc Physicians India. 2006 ; 54 : 622 - 628 .
World Health Organization . Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications . Report of WHO Consultation. 1999 .
Coustan DR , Lowe LP , Metzger BE , et al. ; on behalf of the International Association of Diabetes in Pregnancy Study Groups. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus . Am J Obstet Gynecol. 2010 ; 202 ( 6 ): 654 e1 - 654 e6 .
McIntyre HD , Oats JJ , Kihara AB , et al. Update on diagnosis of hyperglycemia in pregnancy and gestational diabetes mellitus from FIGO’s Pregnancy & Non-Communicable Diseases Committee . Int J Gynaecol Obstet. 2021; 154 (2):189-194.
Menke A , Casagrande S , Geiss L , Cowie CC . Prevalence of and trends in diabetes among adults in the United States, 1988-2012 . JAMA. 2015 ; 314 ( 10 ): 1021 - 1029 .
Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2020 . US Department of Health and Human Services ; 2020 .
Lieberman N , Kalter-Leibovici O , Hod M . Global adaptation of IADPSG recommendations: a national approach . Int J Gynaecol Obstet. 2011 ; 115 ( suppl 1 ): S45 - S47 .
Marseille E , Lohse N , Jiwani A , et al. The cost-effectiveness of gestational diabetes screening including prevention of type 2 diabetes: application of a new model in India and Israel . J Matern Fetal Neonatal Med. 2013 ; 26 ( 8 ): 802 - 810 .
Werner EF , Pettker CM , Zuckerwise L , et al. Screening for gestational diabetes mellitus: are the criteria proposed by the International Association of the Diabetes and Pregnancy Study Groups cost-effective? Diabetes Care . 2012 ; 35 ( 3 ): 529 - 535 .
Mission JF , Ohno MS , Cheng YW , Caughey AB . Gestational diabetes screening with the new IADPSG guidelines: a cost-effectiveness analysis . Am J Obstet Gynecol. 2012 ; 207 ( 4 ): 326 e1 - 326 e9 .
Farrar D , Simmonds M , Griffin S , et al. The identification and treatment of women with hyperglycaemia in pregnancy: an analysis of individual participant data, systematic reviews, meta-analyses and an economic evaluation . Health Technol Assess. 2016 ; 20 ( 86 ): 1 - 348 .
Jacklin PB , Maresh MJ , Patterson CC , et al. A cost-effectiveness comparison of the NICE 2015 and WHO 2013 diagnostic criteria for women with gestational diabetes with and without risk factors . BMJ Open. 2017 ; 7 ( 8 ): e016621 .
Cundy T , Ackermann E , Ryan EA . Gestational diabetes: new criteria may triple the prevalence but effect on outcomes is unclear . BMJ. 2014 ; 348 : g1567 .
O’Sullivan EP , Avalos G , O’Reilly M , et al. Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria . Diabetologia . 2011 ; 54 ( 7 ): 1670 -167 5 .
Lapolla A , Dalfra MG , Ragazzi E , et al. New International Association of the Diabetes and Pregnancy Study Groups (IADPSG) recommendations for diagnosing gestational diabetes compared with former criteria: a retrospective study on pregnancy outcome . Diabet Med. 2011 ; 28 ( 9 ): 1074 - 1077 .
Benhalima K , Hanssens M , Devlieger R , et al. Analysis of pregnancy outcomes using the new IADPSG recommendation compared with the Carpenter and Coustan criteria in an area with a low prevalence of gestational diabetes . Int J Endocrinol. 2013 ; 2013 : 248121 .
Hung TH , Hsieh TT . The effects of implementing the International Association of Diabetes and Pregnancy Study Groups criteria for diagnosing gestational diabetes on maternal and neonatal outcomes . PLoS One. 2015 ; 10 ( 3 ): e0122261 .
Meek CL , Lewis HB , Patient C , et al. Diagnosis of gestational diabetes mellitus: falling through the net . Diabetologia. 2015 ; 58 ( 9 ): 2003 - 2012 .
Djelmis J , Pavic M , Mulliqi Kotori V , et al. Prevalence of gestational diabetes mellitus according to IADPSG and NICE criteria . Int J Gynaecol Obstet. 2016 ; 135 ( 3 ): 250 - 254 .
Ethridge JK Jr , Catalano PM , Waters TP . Perinatal outcomes associated with the diagnosis of gestational diabetes made by the international association of the diabetes and pregnancy study groups criteria . Obstet Gynecol. 2014 ; 124 ( 3 ): 571 - 578 .
Hillier TA , Pedula KL , Ogasawara KK , et al. A pragmatic, randomized clinical trial of gestational diabetes screening . N Engl J Med. 2021 ; 384 ( 10 ): 895 - 904 .
Casey B . Gestational diabetes—on broadening the diagnosis . N Engl J Med. 2021 ; 384 ( 10 ): 965 - 966 .
Dunne F , Lindsay R , Loeken M . This is the decade to find the solution for gestational diabetes mellitus screening and treatments . Diabet Med. 2021 ; 38 ( 8 ): e14602 .
O’Malley EG , Reynolds CME , O’Kelly R , et al. The diagnosis of gestational diabetes mellitus (GDM) using a 75 g oral glucose tolerance test: a prospective observational study . Diabetes Res Clin Pract . 2020 ; 163 : 108144 .
van Leeuwen M , Louwerse MD , Opmeer BC , et al. Glucose challenge test for detecting gestational diabetes mellitus: a systematic review . BJOG. 2012 ; 119 ( 4 ): 393 - 401 .
Sacks DA , Hadden DR , Maresh M , et al. Frequency of gestational diabetes mellitus at collaborating centers based on IADPSG consensus panel-recommended criteria: the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study . Diabetes Care. 2012 ; 35 ( 3 ): 526 - 528 .
Roeckner JT , Sanchez-Ramos L , Jijon-Knupp R , et al. Single abnormal value on 3-hour oral glucose tolerance test during pregnancy is associated with adverse maternal and neonatal outcomes: a systematic review and metaanalysis . Am J Obstet Gynecol. 2016 ; 215 ( 3 ): 287 - 297 .
Freinkel N , Metzger BE , Phelps RL , et al. Gestational diabetes mellitus: heterogeneity of maternal age, weight, insulin secretion, HLA antigens, and islet cell antibodies and the impact of maternal metabolism on pancreatic B-cell and somatic development in the offspring . Diabetes. 1985 ; 34 ( suppl 2 ): 1 - 7 .
Schaefer UM , Songster G , Xiang A , et al. Congenital malformations in offspring of women with hyperglycemia first detected during pregnancy . Am J Obstet Gynecol. 1997 ; 177 ( 5 ): 1165 - 1171 .
Omori Y , Jovanovic L . Proposal for the reconsideration of the definition of gestational diabetes . Diabetes Care. 2005 ; 28 ( 10 ): 2592 - 2593 .
Stacey T , Tennant P , McCowan L , et al. Gestational diabetes and the risk of late stillbirth: a case-control study from England, UK . BJOG. 2019 ; 126 ( 8 ): 973 - 982 .
Cosson E , Bentounes SA , Nachtergaele C , et al. Prognosis associated with sub-types of hyperglycaemia in pregnancy . J Clin Med. 2021 ; 10 ( 17 ): 3904 .
Wong T , Ross GP , Jalaludin BB , Flack JR . The clinical significance of overt diabetes in pregnancy . Diabet Med. 2013 ; 30 ( 4 ): 468 - 474 .
Bartha JL , Martinez-Del-Fresno P , Comino-Delgado R . Early diagnosis of gestational diabetes mellitus and prevention of diabetes-related complications . Eur J Obstet Gynecol Reprod Biol. 2003 ; 109 ( 1 ): 41 - 44 .
Bartha JL , Martinez-Del-Fresno P , Comino-Delgado R . Gestational diabetes mellitus diagnosed during early pregnancy . Am J Obstet Gynecol. 2000 ; 182 ( 2 ): 346 - 350 .
Berkowitz GS , Roman SH , Lapinski RH , et al. Maternal characteristics, neonatal outcome, and the time of diagnosis of gestational diabetes . Am J Obstet Gynecol. 1992 ; 167 ( 4 Pt 1 ): 976 - 8282 .
Meyer WJ , Carbone J , Gauthier DW , et al. Early gestational glucose screening and gestational diabetes . J Reprod Med. 1996 ; 41 ( 9 ): 675 - 679 .
Sweeting AN , Ross GP , Hyett J , et al. Gestational diabetes mellitus in early pregnancy: evidence for poor pregnancy outcomes despite treatment . Diabetes Care. 2016 ; 39 ( 1 ): 75 - 81 .
Li M , Hinkle SN , Grantz KL , et al. Glycaemic status during pregnancy and longitudinal measures of fetal growth in a multi-racial US population: a prospective cohort study . Lancet Diabetes Endocrinol. 2020 ; 8 ( 4 ): 292 - 300 .
Sovio U , Murphy HR , Smith GC . Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women . Diabetes Care. 2016 ; 39 ( 6 ): 982 - 987 .
Venkataraman H , Ram U , Craik S , et al. Increased fetal adiposity prior to diagnosis of gestational diabetes in South Asians: more evidence for the “thin-fat” baby . Diabetologia. 2017 ; 60 ( 3 ): 399 - 405 .
Riskin-Mashiah S , Damti A , Younes G , et al. Normal fasting plasma glucose levels during pregnancy: a hospital-based study . J Perinat Med. 2011 ; 39 ( 2 ): 209 - 211 .
Mills JL , Jovanovic L , Knopp R , et al. Physiological reduction in fasting plasma glucose concentration in the first trimester of normal pregnancy: the diabetes in early pregnancy study . Metabolism. 1998 ; 47 ( 9 ): 1140 - 1144 .
Corrado F , D’Anna R , Cannata ML , et al. Correspondence between first-trimester fasting glycaemia, and oral glucose tolerance test in gestational diabetes diagnosis . Diabetes Metab . 2012 ; 38 ( 5 ): 458 - 61 .
Zhu WW , Yang HX , Wei YM , et al. Evaluation of the value of fasting plasma glucose in the first prenatal visit to diagnose gestational diabetes mellitus in china . Diabetes Care. 2013 ; 36 ( 3 ): 586 - 590 .
McIntyre HD , Sacks DA , Barbour LA , et al. Issues with the diagnosis and classification of hyperglycemia in early pregnancy . Diabetes Care. 2016 ; 39 ( 1 ): 53 - 54 .
Hughes RC , Moore MP , Gullam JE , et al. An early pregnancy HbA1c ≤5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes . Diabetes Care. 2014 ; 37 ( 11 ): 2953 - 2959 .
Sweeting AN , Ross GP , Hyett J , et al. Baseline HbA1c to identify high-risk gestational diabetes: utility in early vs standard gestational diabetes . J Clin Endocrinol Metab. 2017 ; 102 ( 1 ): 150 - 156 .
Immanuel J , Simmons D , Desoye G , et al. Performance of early pregnancy HbA1c for predicting gestational diabetes mellitus and adverse pregnancy outcomes in obese European women . Diabetes Res Clin Pract. 2020 ; 168 : 108378 .
Osmundson SS , Norton ME , El-Sayed YY , et al. Early screening and treatment of women with prediabetes: a randomized controlled trial . Am J Perinatol. 2016 ; 33 ( 2 ): 172 - 179 .
Roeder HA , Moore TR , Wolfson T , Ramos GA . Treating hyperglycemia in the first trimester: a randomized controlled trial . Am J Obstet Gynecol MFM. 2017 ; 1 ( 1 ): 33 - 41 .
Hawkins JS , Lo JY , Casey BM , et al. Diet-treated gestational diabetes mellitus: comparison of early vs routine diagnosis . Am J Obstet Gynecol. 2008 ; 198 ( 3 ): 287 e1 - 287 e6 .
Most OL , Kim JH , Arslan AA , et al. Maternal and neonatal outcomes in early glucose tolerance testing in an obstetric population in New York city . J Perinat Med. 2009 ; 37 ( 2 ): 114 - 117 .
Gupta S , Dolin C , Jadhav A , et al. Obstetrical outcomes in patients with early onset gestational diabetes . J Matern Fetal Neonatal Med. 2016 ; 29 ( 1 ): 27 - 31 .
Harreiter J , Simmons D , Desoye G , et al. IADPSG and WHO 2013 gestational diabetes mellitus criteria identify obese women with marked insulin resistance in early pregnancy . Diabetes Care. 2016 ; 39 ( 7 ): e90 - e92 .
Egan AM , Vellinga A , Harreiter J , et al. Epidemiology of gestational diabetes mellitus according to IADPSG/WHO 2013 criteria among obese pregnant women in Europe . Diabetologia. 2017 ; 60 ( 10 ): 1913 - 1921 .
Immanuel J , Simmons D . Screening and treatment for early-onset gestational diabetes mellitus: a systematic review and meta-analysis . Curr Diab Rep. 2017 ; 17 ( 11 ): 115 .
Bozkurt L , Gobl CS , Pfligl L , et al. Pathophysiological characteristics and effects of obesity in women with early and late manifestation of gestational diabetes diagnosed by the International Association of Diabetes and Pregnancy Study Groups criteria . J Clin Endocrinol Metab. 2015 ; 100 ( 3 ): 1113 - 1120 .
Bozkurt L , Gobl CS , Hormayer AT , et al. The impact of preconceptional obesity on trajectories of maternal lipids during gestation . Sci Rep. 2016 ; 6 : 29971 .
Sweeting AN , Ross GP , Hyett J , et al. Gestational diabetes in the first trimester: is early testing justified? Lancet Diabetes Endocrinol. 2017 ; 5 ( 8 ): 571 - 573 .
Harper LM , Jauk V , Longo S , et al. Early gestational diabetes screening in obese women: a randomized controlled trial . Am J Obstet Gynecol. 2020 ; 222 ( 5 ): 495 e1 - 495 e8 .
Vinter CA , Tanvig MH , Christensen MH , et al. Lifestyle intervention in Danish obese pregnant women with early gestational diabetes mellitus according to WHO 2013 criteria does not change pregnancy outcomes: results from the LiP (Lifestyle in Pregnancy) study . Diabetes Care. 2018 ; 41 ( 10 ): 2079 - 2085 .
Simmons D , Hague WM , Teede HJ , et al. Hyperglycaemia in early pregnancy: the Treatment of Booking Gestational Diabetes Mellitus (TOBOGM) study: a randomised controlled trial . Med J Aust. 2018 ; 209 ( 9 ): 405 - 406 .
Bruns DE , Metzger BE , Sacks DB . Diagnosis of gestational diabetes mellitus will be flawed until we can measure glucose . Clin Chem. 2020 ; 66 ( 2 ): 265 - 267 .
Bogdanet D , O’Shea P , Lyons C , et al. The oral glucose tolerance test-is it time for a change?-a literature review with an emphasis on pregnancy . J Clin Med. 2020 ; 9 ( 11):3451 .
Sacks DB , Arnold M , Bakris GL , et al. Position statement executive summary: guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus . Diabetes Care. 2011 ; 34 ( 6 ): 1419 - 1423 .
Chan AY , Swaminathan R , Cockram CS . Effectiveness of sodium fluoride as a preservative of glucose in blood . Clin Chem. 1989 ; 35 ( 2 ): 315 - 317 .
Potter JM , Hickman PE , Oakman C , et al. Strict preanalytical oral glucose tolerance test blood sample handling is essential for diagnosing gestational diabetes mellitus . Diabetes Care. 2020 ; 43 ( 7 ): 1438 - 1441 .
Daly N , Flynn I , Carroll C , et al. Impact of implementing preanalytical laboratory standards on the diagnosis of gestational diabetes mellitus: a prospective observational study . Clin Chem. 2016 ; 62 ( 2 ): 387 - 391 .
International Diabetes Federation . IDF Diabetes Atlas . 9th ed. 2019 .
Guariguata L , Linnenkamp U , Beagley J , et al. Global estimates of the prevalence of hyperglycaemia in pregnancy . Diabetes Res Clin Pract. 2014 ; 103 ( 2 ): 176 - 185 .
Prentice PM , Olga L , Petry CJ , et al. Reduced size at birth and persisting reductions in adiposity in recent, compared with earlier, cohorts of infants born to mothers with gestational diabetes mellitus . Diabetologia. 2019 ; 62 ( 11 ): 1977 - 1987 .
Hartling L , Dryden DM . Screening and diagnosing gestational diabetes mellitus . Evid Rep Technol Assess (Full Rep). 2012 ; 210 : 1 - 327 .
Bottalico JN . Recurrent gestational diabetes: risk factors, diagnosis, management, and implications . Semin Perinatol. 2007 ; 31 ( 3 ): 176 - 184 .
Anna V , van der Ploeg H , P , Cheung NW , et al. Sociodemographic correlates of the increasing trend in prevalence of gestational diabetes mellitus in a large population of women between 1995 and 2005 . Diabetes Care. 2008 ; 31 ( 12 ): 2288 - 2293 .
Chu SY , Callaghan WM , Kim SY , et al. Maternal obesity and risk of gestational diabetes mellitus . Diabetes Care. 2007 ; 30 ( 8 ): 2070 - 2076 .
Torloni MR , Betran AP , Horta BL , et al. Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta-analysis . Obes Rev. 2009 ; 10 ( 2 ): 194 - 203 .
Mokdad AH , Ford ES , Bowman BA , et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003 ; 289 ( 1 ): 76 - 79 .
Mulla WR , Henry TQ , Homko CJ . Gestational diabetes screening after HAPO: has anything changed? Curr Diab Rep. 2010 ; 10 ( 3 ): 224 - 228 .
Petry CJ . Gestational diabetes: risk factors and recent advances in its genetics and treatment . Br J Nutr. 2010 ; 104 ( 6 ): 775 - 787 .
Hunt KJ , Schuller KL . The increasing prevalence of diabetes in pregnancy . Obstet Gynecol Clin North Am. 2007 ; 34 ( 2 ): 173 - 199 , vii.
Agarwal MM , Dhatt GS , Shah SM . Gestational diabetes mellitus: simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucose . Diabetes Care. 2010 ; 33 ( 9 ): 2018 - 2020 .
Moses RG , Morris GJ , Petocz P , et al. The impact of potential new diagnostic criteria on the prevalence of gestational diabetes mellitus in Australia . Med J Aust. 2011 ; 194 ( 7 ): 338 - 340 .
Brown FM , Wyckoff J . Application of one-step IADPSG versus two-step diagnostic criteria for gestational diabetes in the real world: impact on health services, clinical care, and outcomes . Curr Diab Rep. 2017 ; 17 ( 10 ): 85 .
Kim C , Berger DK , Chamany S . Recurrence of gestational diabetes mellitus: a systematic review . Diabetes Care. 2007 ; 30 ( 5 ): 1314 - 1319 .
Solomon CG , Willett WC , Carey VJ , et al. A prospective study of pregravid determinants of gestational diabetes mellitus . JAMA. 1997 ; 278 ( 13 ): 1078 - 1083 .
Chamberlain C , McNamara B , Williams ED , et al. Diabetes in pregnancy among indigenous women in Australia, Canada, New Zealand and the United States . Diabetes Metab Res Rev. 2013 ; 29 ( 4 ): 241 - 256 .
Hedderson MM , Gunderson EP , Ferrara A . Gestational weight gain and risk of gestational diabetes mellitus . Obstet Gynecol. 2010 ; 115 ( 3 ): 597 - 604 .
Kjos SL , Buchanan TA . Gestational diabetes mellitus . N Engl J Med. 1999 ; 341 ( 23 ): 1749 - 1756 .
Di Cianni G , Volpe L , Lencioni C , et al. Prevalence and risk factors for gestational diabetes assessed by universal screening . Diabetes Res Clin Pract. 2003 ; 62 ( 2 ): 131 - 137 .
Cypryk K , Szymczak W , Czupryniak L , et al. Gestational diabetes mellitus—an analysis of risk factors . Endokrynol Pol. 2008 ; 59 ( 5 ): 393 - 397 .
Cleary-Goldman J , Malone FD , Vidaver J , et al. Impact of maternal age on obstetric outcome . Obstet Gynecol. 2005 ; 105 ( 5 Pt 1 ): 983 - 990 .
Yang H , Wei Y , Gao X , et al. Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16,286 pregnant women in China . Diabet Med. 2009 ; 26 ( 11 ): 1099 - 1104 .
Morisset AS , St-Yves A , Veillette J , et al. Prevention of gestational diabetes mellitus: a review of studies on weight management . Diabetes Metab Res Rev. 2010 ; 26 ( 1 ): 17 - 25 .
Weiss JL , Malone FD , Emig D , et al. Obesity, obstetric complications and cesarean delivery rate—a population-based screening study . Am J Obstet Gynecol. 2004 ; 190 ( 4 ): 1091 - 1097 .
Gibson KS , Waters TP , Catalano PM . Maternal weight gain in women who develop gestational diabetes mellitus . Obstet Gynecol. 2012 ; 119 ( 3 ): 560 - 565 .
Morisset AS , Tchernof A , Dube MC , et al. Weight gain measures in women with gestational diabetes mellitus . J Womens Health (Larchmt). 2011 ; 20 ( 3 ): 375 - 380 .
Tovar A , Must A , Bermudez OI , et al. The impact of gestational weight gain and diet on abnormal glucose tolerance during pregnancy in Hispanic women . Matern Child Health J. 2009 ; 13 ( 4 ): 520 - 530 .
Teulings N , Masconi KL , Ozanne SE , et al. Effect of interpregnancy weight change on perinatal outcomes: systematic review and meta-analysis . BMC Pregnancy Childbirth. 2019 ; 19 ( 1 ): 386 .
Lo JC , Feigenbaum SL , Escobar GJ , et al. Increased prevalence of gestational diabetes mellitus among women with diagnosed polycystic ovary syndrome: a population-based study . Diabetes Care. 2006 ; 29 ( 8 ): 1915 - 1917 .
Mikola M , Hiilesmaa V , Halttunen M , et al. Obstetric outcome in women with polycystic ovarian syndrome . Hum Reprod. 2001 ; 16 ( 2 ): 226 - 229 .
Dinham GK , Henry A , Lowe SA , et al. Twin pregnancies complicated by gestational diabetes mellitus: a single centre cohort study . Diabet Med. 2016 ; 33 ( 12 ): 1659 - 1667 .
Rauh-Hain JA , Rana S , Tamez H , et al. Risk for developing gestational diabetes in women with twin pregnancies . J Matern Fetal Neonatal Med. 2009 ; 22 ( 4 ): 293 - 299 .
Chasan-Taber L , Schmidt MD , Pekow P , et al. Physical activity and gestational diabetes mellitus among Hispanic women . J Womens Health (Larchmt). 2008 ; 17 ( 6 ): 999 - 1008 .
Mottola MF . The role of exercise in the prevention and treatment of gestational diabetes mellitus . Curr Diab Rep. 2008 ; 8 ( 4 ): 299 - 304 .
Zhang C , Liu S , Solomon CG , et al. Dietary fiber intake, dietary glycemic load, and the risk for gestational diabetes mellitus . Diabetes Care. 2006 ; 29 ( 10 ): 2223 - 2230 .
Kucukgoncu S , Guloksuz S , Celik K , et al. Antipsychotic exposure in pregnancy and the risk of gestational diabetes: a systematic review and meta-analysis . Schizophr Bull. 2020 ; 46 ( 2 ): 311 - 318 .
Galbally M , Frayne J , Watson SJ , et al. The association between gestational diabetes mellitus, antipsychotics and severe mental illness in pregnancy: a multicentre study . Aust N Z J Obstet Gynaecol. 2020 ; 60 ( 1 ): 63 - 69 .
Hedderson MM , Ferrara A . High blood pressure before and during early pregnancy is associated with an increased risk of gestational diabetes mellitus . Diabetes Care. 2008 ; 31 ( 12 ): 2362 - 2367 .
Lao TT , Ho LF . First-trimester blood pressure and gestational diabetes in high-risk Chinese women . J Soc Gynecol Investig. 2003 ; 10 ( 2 ): 94 - 98 .
Sweeting AN , Appelblom H , Ross GP , et al. First trimester prediction of gestational diabetes mellitus: a clinical model based on maternal demographic parameters . Diabetes Res Clin Pract. 2017 ; 127 : 44 - 50 .
Syngelaki A , Visser GH , Krithinakis K , et al. First trimester screening for gestational diabetes mellitus by maternal factors and markers of inflammation . Metabolism. 2016 ; 65 ( 3 ): 131 - 137 .
Nanda S , Savvidou M , Syngelaki A , et al. Prediction of gestational diabetes mellitus by maternal factors and biomarkers at 11 to 13 weeks . Prenat Diagn. 2011 ; 31 ( 2 ): 135 - 141 .
van Leeuwen M , Opmeer BC , Zweers EJ , et al. Estimating the risk of gestational diabetes mellitus: a clinical prediction model based on patient characteristics and medical history . BJOG. 2010 ; 117 ( 1 ): 69 - 75 .
Naylor CD , Sermer M , Chen E , et al. ; Toronto Trihospital Gestational Diabetes Project Investigators. Selective screening for gestational diabetes mellitus . N Engl J Med. 1997 ; 337 ( 22 ): 1591 - 1596 .
Catalano PM . Trying to understand gestational diabetes . Diabet Med. 2014 ; 31 ( 3 ): 273 - 281 .
Catalano PM . Carbohydrate metabolism and gestational diabetes . Clin Obstet Gynecol. 1994 ; 37 ( 1 ): 25 - 38 .
Lain KY , Catalano PM . Metabolic changes in pregnancy . Clin Obstet Gynecol. 2007 ; 50 ( 4 ): 938 - 948 .
Costrini NV , Kalkhoff RK . Relative effects of pregnancy, estradiol, and progesterone on plasma insulin and pancreatic islet insulin secretion . J Clin Invest. 1971 ; 50 ( 5 ): 992 - 999 .
Kalkhoff RK , Kissebah AH , Kim HJ . Carbohydrate and lipid metabolism during normal pregnancy: relationship to gestational hormone action . Semin Perinatol. 1978 ; 2 ( 4 ): 291 - 307 .
Leturque A , Hauguel S , Sutter Dub MT , et al. Effects of placental lactogen and progesterone on insulin stimulated glucose metabolism in rat muscles in vitro . Diabete Metab. 1989 ; 15 ( 4 ): 176 - 181 .
Ryan EA , Enns L . Role of gestational hormones in the induction of insulin resistance . J Clin Endocrinol Metab. 1988 ; 67 ( 2 ): 341 - 347 .
Alvarez JJ , Montelongo A , Iglesias A , Lasuncion MA , Herrera E . Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women . J Lipid Res. 1996 ; 37 ( 2 ): 299 - 308 .
Barbour LA , McCurdy CE , Hernandez TL , Kirwan JP , Catalano PM , Friedman JE . Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes . Diabetes Care. 2007 ; 30 ( suppl 2 ): S112 - S119 .
Bomba-Opon D , Wielgos M , Szymanska M , et al. Effects of free fatty acids on the course of gestational diabetes mellitus . Neuro Endocrinol Lett. 2006 ; 27 ( 1-2 ): 277 - 280 .
Boden G , Chen X , Ruiz J , et al. Mechanisms of fatty acid-induced inhibition of glucose uptake . J Clin Invest. 1994 ; 93 ( 6 ): 2438 - 2446 .
Catalano PM , Huston L , Amini SB , et al. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus . Am J Obstet Gynecol. 1999 ; 180 ( 4 ): 903 - 916 .
Buchanan TA , Metzger BE , Freinkel N , et al. Insulin sensitivity and B-cell responsiveness to glucose during late pregnancy in lean and moderately obese women with normal glucose tolerance or mild gestational diabetes . Am J Obstet Gynecol. 1990 ; 162 ( 4 ): 1008 - 1014 .
Sivan E , Chen X , Homko CJ , et al. Longitudinal study of carbohydrate metabolism in healthy obese pregnant women . Diabetes Care. 1997 ; 20 ( 9 ): 1470 - 1475 .
Caro JF , Dohm LG , Pories WJ , et al. Cellular alterations in liver, skeletal muscle, and adipose tissue responsible for insulin resistance in obesity and type II diabetes . Diabetes Metab Rev. 1989 ; 5 ( 8 ): 665 - 689 .
Freinkel N , Metzger BE , Nitzan M , et al. Faciltated anabolism in late pregnancy: some novel maternal compensations for accelerated starvation. In: Malaise WJ , Pirart J , Vallence-Own J , eds. International Congress Series 312 . Excerpta Medica ; 1974 : 474 - 488 .
Yogev Y , Ben-Haroush A , Chen R , et al. Diurnal glycemic profile in obese and normal weight nondiabetic pregnant women . Am J Obstet Gynecol. 2004 ; 191 ( 3 ): 949 - 953 .
Hernandez TL , Friedman JE , Van Pelt RE , et al. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged? Diabetes Care. 2011 ; 34 ( 7 ): 1660 - 1668 .
Kuhl C . Etiology and pathogenesis of gestational diabetes . Diabetes Care. 1998 ; 21 ( suppl 2 ): B19 - B26 .
Parsons JA , Brelje TC , Sorenson RL . Adaptation of islets of Langerhans to pregnancy: increased islet cell proliferation and insulin secretion correlates with the onset of placental lactogen secretion . Endocrinology. 1992 ; 130 ( 3 ): 1459 - 1466 .
Sorenson RL , Brelje TC . Adaptation of islets of Langerhans to pregnancy: beta-cell growth, enhanced insulin secretion and the role of lactogenic hormones . Horm Metab Res. 1997 ; 29 ( 6 ): 301 - 307 .
Nielsen JH , Galsgaard ED , Moldrup A , et al. Regulation of beta-cell mass by hormones and growth factors . Diabetes. 2001 ; 50 ( suppl 1 ): S25 - S29 .
Parsons JA , Bartke A , Sorenson RL . Number and size of islets of Langerhans in pregnant, human growth hormone-expressing transgenic, and pituitary dwarf mice: effect of lactogenic hormones . Endocrinology. 1995 ; 136 ( 5 ): 2013 - 2021 .
Rieck S , White P , Schug J , et al. The transcriptional response of the islet to pregnancy in mice . Mol Endocrinol. 2009 ; 23 ( 10 ): 1702 - 1712 .
Buchanan TA , Kitzmiller JL . Metabolic interactions of diabetes and pregnancy . Annu Rev Med. 1994 ; 45 : 245 - 260 .
Rieck S , Kaestner KH . Expansion of beta-cell mass in response to pregnancy . Trends Endocrinol Metab. 2010 ; 21 ( 3 ): 151 - 158 .
Koukkou E , Watts GF , Lowy C . Serum lipid, lipoprotein and apolipoprotein changes in gestational diabetes mellitus: a cross-sectional and prospective study . J Clin Pathol. 1996 ; 49 ( 8 ): 634 - 637 .
Nolan CJ . Controversies in gestational diabetes . Best Pract Res Clin Obstet Gynaecol. 2011 ; 25 ( 1 ): 37 - 49 .
Talchai C , Xuan S , Lin HV , Sussel L , Accili D . Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure . Cell. 2012 ; 150 ( 6 ): 1223 - 1234 .
Halban PA , Polonsky KS , Bowden DW , et al. beta-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment . Diabetes Care. 2014 ; 37 ( 6 ): 1751 - 1758 .
Catalano PM , Tyzbir ED , Wolfe RR , et al. Carbohydrate metabolism during pregnancy in control subjects and women with gestational diabetes . Am J Physiol. 1993 ; 264 ( 1 Pt 1 ): E60 - E67 .
Homko C , Sivan E , Chen X , et al. Insulin secretion during and after pregnancy in patients with gestational diabetes mellitus . J Clin Endocrinol Metab. 2001 ; 86 ( 2 ): 568 - 573 .
Powe CE , Huston Presley LP , Locascio JJ , et al. Augmented insulin secretory response in early pregnancy . Diabetologia. 2019 ; 62 ( 8 ): 1445 - 1452 .
Dluski DF , Wolińska E , Skrzypczak M . Epigenetic changes in gestational diabetes mellitus . Int J Mol Sci. 2021 ; 22 ( 14 ):7649.
Elliott HR , Sharp GC , Relton CL , et al. Epigenetics and gestational diabetes: a review of epigenetic epidemiology studies and their use to explore epigenetic mediation and improve prediction . Diabetologia. 2019 ; 62 ( 12 ): 2171 - 2178 .
Hayes MG , Urbanek M , Hivert MF , et al. Identification of HKDC1 and BACE2 as genes influencing glycemic traits during pregnancy through genome-wide association studies . Diabetes. 2013 ; 62 ( 9 ): 3282 - 3291 .
Liu S , Liu Y , Liao S . Heterogeneous impact of type 2 diabetes mellitus-related genetic variants on gestational glycemic traits: review and future research needs . Mol Genet Genomics. 2019 ; 294 ( 4 ): 811 - 847 .
Wu L , Cui L , Tam WH , et al. Genetic variants associated with gestational diabetes mellitus: a meta-analysis and subgroup analysis . Sci Rep. 2016 ; 6 : 30539 .
Chon SJ , Kim SY , Cho NR , et al. Association of variants in PPARgamma(2), IGF2BP2, and KCNQ1 with a susceptibility to gestational diabetes mellitus in a Korean population . Yonsei Med J. 2013 ; 54 ( 2 ): 352 - 357 .
Kim JY , Cheong HS , Park BL , et al. Melatonin receptor 1 B polymorphisms associated with the risk of gestational diabetes mellitus . BMC Med Genet. 2011 ; 12 : 82 .
Klein K , Haslinger P , Bancher-Todesca D , et al. Transcription factor 7-like 2 gene polymorphisms and gestational diabetes mellitus . J Matern Fetal Neonatal Med. 2012 ; 25 ( 9 ): 1783 - 1786 .
Alharbi KK , Khan IA , Abotalib Z , et al. Insulin receptor substrate-1 (IRS-1) Gly927Arg: correlation with gestational diabetes mellitus in Saudi women . Biomed Res Int. 2014 ; 2014 : 146495 .
Tok EC , Ertunc D , Bilgin O , et al. PPAR-gamma2 Pro12Ala polymorphism is associated with weight gain in women with gestational diabetes mellitus . Eur J Obstet Gynecol Reprod Biol. 2006 ; 129 ( 1 ): 25 - 30 .
Montazeri S , Nalliah S , Radhakrishnan AK . Is there a genetic variation association in the IL-10 and TNF alpha promoter gene with gestational diabetes mellitus? Hereditas. 2010 ; 147 ( 2 ): 94 - 102 .
Kwak SH , Kim SH , Cho YM , et al. A genome-wide association study of gestational diabetes mellitus in Korean women . Diabetes. 2012 ; 61 ( 2 ): 531 - 541 .
Lyssenko V , Nagorny CL , Erdos MR , et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion . Nat Genet. 2009 ; 41 ( 1 ): 82 - 88 .
Wellcome Trust Case Control Consortium . Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls . Nature. 2007 ; 447 ( 7145 ): 661 - 678 .
Bouatia-Naji N , Bonnefond A , Cavalcanti-Proenca C , et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk . Nat Genet. 2009 ; 41 ( 1 ): 89 - 94 .
Saxena R , Elbers CC , Guo Y , et al. Large-scale gene-centric meta-analysis across 39 studies identifies type 2 diabetes loci . Am J Hum Genet. 2012 ; 90 ( 3 ): 410 - 425 .
Manning AK , Hivert MF , Scott RA , et al. A genome-wide approach accounting for body mass index identifies genetic variants influencing fasting glycemic traits and insulin resistance . Nat Genet. 2012 ; 44 ( 6 ): 659 - 669 .
Sparso T , Andersen G , Nielsen T , et al. The GCKR rs780094 polymorphism is associated with elevated fasting serum triacylglycerol, reduced fasting and OGTT-related insulinaemia, and reduced risk of type 2 diabetes . Diabetologia. 2008 ; 51 ( 1 ): 70 - 75 .
Vaxillaire M , Cavalcanti-Proenca C , Dechaume A , et al. The common P446L polymorphism in GCKR inversely modulates fasting glucose and triglyceride levels and reduces type 2 diabetes risk in the DESIR prospective general French population . Diabetes. 2008 ; 57 ( 8 ): 2253 - 2257 .
Agius L . Glucokinase and molecular aspects of liver glycogen metabolism . Biochem J. 2008 ; 414 ( 1 ): 1 - 18 .
Chasman DI , Pare G , Mora S , et al. Forty-three loci associated with plasma lipoprotein size, concentration, and cholesterol content in genome-wide analysis . PLoS Genet. 2009 ; 5 ( 11 ): e1000730 .
Seidah NG . The proprotein convertases, 20 years later . Methods Mol Biol. 2011 ; 768 : 23 - 57 .
Benzinou M , Creemers JW , Choquet H , et al. Common nonsynonymous variants in PCSK1 confer risk of obesity . Nat Genet. 2008 ; 40 ( 8 ): 943 - 945 .
Hayes A , Chevalier A , D’Souza M , et al. Early childhood obesity: association with healthcare expenditure in Australia . Obesity (Silver Spring) . 2016 ; 24 ( 8 ): 1752 - 8 .
Powe CE , Nodzenski M , Talbot O , et al. Genetic determinants of glycemic traits and the risk of gestational diabetes mellitus . Diabetes. 2018 ; 67 ( 12 ): 2703 - 2709 .
Fajans SS , Bell GI , Polonsky KS . Molecular mechanisms and clinical pathophysiology of maturity-onset diabetes of the young . N Engl J Med. 2001 ; 345 ( 13 ): 971 - 980 .
Hattersley AT , Patel KA . Precision diabetes: learning from monogenic diabetes . Diabetologia. 2017 ; 60 ( 5 ): 769 - 777 .
Dickens LT , Naylor RN . Clinical management of women with monogenic diabetes during pregnancy . Curr Diab Rep. 2018 ; 18 ( 3 ): 12 .
Chakera AJ , Steele AM , Gloyn AL , et al. Recognition and management of individuals with hyperglycemia because of a heterozygous glucokinase mutation . Diabetes Care. 2015 ; 38 ( 7 ): 1383 - 1392 .
Urbanova J , Brunerova L , Nunes M , et al. Identification of MODY among patients screened for gestational diabetes: a clinician’s guide . Arch Gynecol Obstet. 2020 ; 302 ( 2 ): 305 - 314 .
Wang Z , Ping F , Zhang Q , et al. Preliminary screening of mutations in the glucokinase gene of Chinese patients with gestational diabetes . J Diabetes Investig. 2018 ; 9 ( 1 ): 199 - 203 .
Gjesing AP , Rui G , Lauenborg J , et al. High prevalence of diabetes-predisposing variants in MODY genes among Danish women with gestational diabetes mellitus . J Endocr Soc. 2017 ; 1 ( 6 ): 681 - 690 .
Shields BM , Hicks S , Shepherd MH , et al. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia. 2010 ; 53 ( 12 ): 2504 - 2508 .
Spyer G , Hattersley AT , Sykes JE , et al. Influence of maternal and fetal glucokinase mutations in gestational diabetes . Am J Obstet Gynecol. 2001 ; 185 ( 1 ): 240 - 241 .
Hattersley AT , Beards F , Ballantyne E , et al. Mutations in the glucokinase gene of the fetus result in reduced birth weight . Nat Genet. 1998 ; 19 ( 3 ): 268 - 270 .
Scholtens DM , Kuang A , Lowe LP , et al. Hyperglycemia and adverse pregnancy outcome follow-up study (HAPO FUS): maternal glycemia and childhood glucose metabolism . Diabetes Care. 2019 ; 42 ( 3 ): 381 - 392 .
Saravanan P ; Diabetes in Pregnancy Working Group . Gestational diabetes: opportunities for improving maternal and child health . Lancet Diabetes Endocrinol. 2020 ; 8 ( 9 ): 793 - 800 .
Pedersen J . Hyperglycaemia-hyperinsulinism theory and birthweight. In: The Pregnant Diabetic and Her Newborn: Problems and Management . Williams and Wilkins ; 1977 : 211 - 220 .
Illsley NP . Glucose transporters in the human placenta . Placenta. 2000 ; 21 ( 1 ): 14 - 22 .
Pedersen J . Weight and length at birth of infants of diabetic mothers . Acta Endocrinol (Copenh). 1954 ; 16 ( 4 ): 330 - 342 .
Whitelaw A . Subcutaneous fat in newborn infants of diabetic mothers: an indication of quality of diabetic control . Lancet. 1977 ; 1 ( 8001 ): 15 - 18 .
Vrijkotte TG , Krukziener N , Hutten BA , et al. Maternal lipid profile during early pregnancy and pregnancy complications and outcomes: the ABCD study . J Clin Endocrinol Metab. 2012 ; 97 ( 11 ): 3917 - 3925 .
Yang X , Hsu-Hage B , Zhang H , et al. Women with impaired glucose tolerance during pregnancy have significantly poor pregnancy outcomes . Diabetes Care. 2002 ; 25 ( 9 ): 1619 - 1624 .
Spellacy WN , Miller S , Winegar A , et al. Macrosomia—maternal characteristics and infant complications . Obstet Gynecol. 1985 ; 66 ( 2 ): 158 - 161 .
Jang HC , Cho NH , Min YK , et al. Increased macrosomia and perinatal morbidity independent of maternal obesity and advanced age in Korean women with GDM . Diabetes Care. 1997 ; 20 ( 10 ): 1582 - 1588 .
Langer O , Yogev Y , Most O , et al. Gestational diabetes: the consequences of not treating . Am J Obstet Gynecol. 2005 ; 192 ( 4 ): 989 - 997 .
Weiss PA , Haeusler M , Tamussino K , et al. Can glucose tolerance test predict fetal hyperinsulinism? BJOG. 2000 ; 107 ( 12 ): 1480 - 1485 .
Boulet SL , Alexander GR , Salihu HM , et al. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk . Am J Obstet Gynecol. 2003 ; 188 ( 5 ): 1372 - 1378 .
Ryckman KK , Spracklen CN , Smith CJ , et al. Maternal lipid levels during pregnancy and gestational diabetes: a systematic review and meta-analysis . BJOG. 2015 ; 122 ( 5 ): 643 - 651 .
Jovanovic L , Pettitt DJ . Gestational diabetes mellitus . JAMA. 2001 ; 286 ( 20 ): 2516 - 2518 .
Esakoff TF , Cheng YW , Sparks TN , et al. The association between birthweight 4000 g or greater and perinatal outcomes in patients with and without gestational diabetes mellitus . Am J Obstet Gynecol. 2009 ; 200 ( 6 ): 672 e1 - 672 e4 .
Henriksen T . The macrosomic fetus: a challenge in current obstetrics . Acta Obstet Gynecol Scand. 2008 ; 87 ( 2 ): 134 - 145 .
Reece EA , Leguizamon G , Wiznitzer A . Gestational diabetes: the need for a common ground . Lancet. 2009 ; 373 ( 9677 ): 1789 - 1797 .
Cetin H , Yalaz M , Akisu M , et al. Polycythaemia in infants of diabetic mothers: beta-hydroxybutyrate stimulates erythropoietic activity . J Int Med Res. 2011 ; 39 ( 3 ): 815 - 821 .
Farrar D , Fairley L , Santorelli G , et al. Association between hyperglycaemia and adverse perinatal outcomes in south Asian and white British women: analysis of data from the Born in Bradford cohort . Lancet Diabetes Endocrinol. 2015 ; 3 ( 10 ): 795 - 804 .
Balsells M , Corcoy R , Adelantado JM , et al. Gestational diabetes mellitus: metabolic control during labour . Diabetes Nutr Metab. 2000 ; 13 ( 5 ): 257 - 262 .
Farrar D , Simmonds M , Bryant M , et al. Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis . BMJ. 2016 ; 354 : i4694 .
Billionnet C , Mitanchez D , Weill A , et al. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012 . Diabetologia. 2017 ; 60 ( 4 ): 636 - 644 .
Allen VM , Armson BA . SOGC Clinical Practice Guideline: teratogenicity associated with pre-existing and gestational diabetes . J Obstet Gynaecol Can. 2007 ; 29 ( 11 ): 927 - 934 .
Owens LA , O’Sullivan EP , Kirwan B , et al. ATLANTIC DIP: the impact of obesity on pregnancy outcome in glucose-tolerant women . Diabetes Care. 2010 ; 33 ( 3 ): 577 - 579 .
Dennedy MC , Avalos G , O’Reilly MW , et al. ATLANTIC-DIP: raised maternal body mass index (BMI) adversely affects maternal and fetal outcomes in glucose-tolerant women according to International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria . J Clin Endocrinol Metab. 2012 ; 97 ( 4 ): E608 - E612 .
Rosenstein MG , Cheng YW , Snowden JM , et al. The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes . Am J Obstet Gynecol. 2012 ; 206 ( 4 ): 309 e1 - 309 e7 .
Mitanchez D . Foetal and neonatal complications in gestational diabetes: perinatal mortality, congenital malformations, macrosomia, shoulder dystocia, birth injuries, neonatal complications . Diabetes Metab. 2010 ; 36 ( 6 Pt 2 ): 617 - 627 .
Cundy T , Gamble G , Townend K , et al. Perinatal mortality in type 2 diabetes mellitus . Diabet Med. 2000 ; 17 ( 1 ): 33 - 39 .
Hutcheon JA , Kuret V , Joseph KS , et al. Immortal time bias in the study of stillbirth risk factors: the example of gestational diabetes . Epidemiology. 2013 ; 24 ( 6 ): 787 - 790 .
Poston L , Bell R , Croker H , et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial . Lancet Diabetes Endocrinol. 2015 ; 3 ( 10 ): 767 - 777 .
Tam WH , Ma RCW , Ozaki R , et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in Offspring . Diabetes Care. 2017 ; 40 ( 5 ): 679 - 686 .
Yu Y , Arah OA , Liew Z , et al. Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up . BMJ. 2019 ; 367 : l6398 .
Hod M . The fetal heart in gestational diabetes: long-term effects . BJOG. 2021 ; 128 ( 2 ): 280 .
Dabelea D , Hanson RL , Lindsay RS , et al. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships . Diabetes. 2000 ; 49 ( 12 ): 2208 - 2211 .
Lowe WL Jr. , Lowe LP , Kuang A , et al. Maternal glucose levels during pregnancy and childhood adiposity in the Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study . Diabetologia. 2019 ; 62 ( 4 ): 598 - 610 .
Page KA , Luo S , Wang X , et al. Children exposed to maternal obesity or gestational diabetes mellitus during early fetal development have hypothalamic alterations that predict future weight gain . Diabetes Care. 2019 ; 42 ( 8 ): 1473 - 1480 .
Anderberg E , Kallen K , Berntorp K . The impact of gestational diabetes mellitus on pregnancy outcome comparing different cut-off criteria for abnormal glucose tolerance . Acta Obstet Gynecol Scand. 2010 ; 89 ( 12 ): 1532 - 1537 .
Ju H , Rumbold AR , Willson KJ , et al. Borderline gestational diabetes mellitus and pregnancy outcomes . BMC Pregnancy Childbirth. 2008 ; 8 : 31 .
Jastrow N , Roberge S , Gauthier RJ , et al. Effect of birth weight on adverse obstetric outcomes in vaginal birth after cesarean delivery . Obstet Gynecol. 2010 ; 115 ( 2 Pt 1 ): 338 - 343 .
Metzger BE , Coustan DR . Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee . Diabetes Care. 1998 ; 21 ( suppl 2 ): B161 - B167 .
Hiden U , Lassance L , Tabrizi NG , et al. Fetal insulin and IGF-II contribute to gestational diabetes mellitus (GDM)-associated up-regulation of membrane-type matrix metalloproteinase 1 (MT1-MMP) in the human feto-placental endothelium . J Clin Endocrinol Metab. 2012 ; 97 ( 10 ): 3613 - 3621 .
Dunne FP , Avalos G , Durkan M , et al. ATLANTIC DIP: pregnancy outcomes for women with type 1 and type 2 diabetes . Ir Med J. 2012 ; 105 ( 5 suppl ): 6 - 9 .
Roberts JM , Redman CW . Pre-eclampsia: more than pregnancy-induced hypertension . Lancet. 1993 ; 341 ( 8858 ): 1447 - 1451 .
Desoye G , Hauguel-de Mouzon S . The human placenta in gestational diabetes mellitus. The Insulin and Cytokine Network . Diabetes Care. 2007 ; 30 ( suppl 2 ): S120 - S126 .
Belkacemi L , Lash GE , Macdonald-Goodfellow SK , et al. Inhibition of human trophoblast invasiveness by high glucose concentrations . J Clin Endocrinol Metab. 2005 ; 90 ( 8 ): 4846 - 4851 .
Vounzoulaki E , Khunti K , Abner SC , et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis . BMJ. 2020 ; 369 : m1361 .
Daly B , Toulis KA , Thomas N , et al. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. . PLoS Med. 2018 ; 15 ( 1 ): e1002488 .
Lowe WL Jr , Scholtens DM , Kuang A , et al. Hyperglycemia and adverse pregnancy outcome follow-up study (HAPO FUS): maternal gestational diabetes mellitus and childhood glucose metabolism . Diabetes Care. 2019 ; 42 ( 3 ): 372 - 380 .
Murphy HR . 2020 NICE guideline update: good news for pregnant women with type 1 diabetes and past or current gestational diabetes . Diabet Med. 2021 ; 38 ( 6 ): e14576 .
National Institute for Health and Care Excellence . Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period . NICE Guidelines NG3. 2015 . Last updated December 16, 2020. https://www.nice.org.uk/guidance/ng3
Carr DB , Utzschneider KM , Hull RL , et al. Gestational diabetes mellitus increases the risk of cardiovascular disease in women with a family history of type 2 diabetes . Diabetes Care. 2006 ; 29 ( 9 ): 2078 - 2083 .
Gunderson EP , Chiang V , Pletcher MJ , et al. History of gestational diabetes mellitus and future risk of atherosclerosis in mid-life: the Coronary Artery Risk Development in Young Adults study . J Am Heart Assoc. 2014 ; 3 ( 2 ): e000490 .
Retnakaran R . Glucose tolerance status in pregnancy: a window to the future risk of diabetes and cardiovascular disease in young women . Curr Diabetes Rev. 2009 ; 5 ( 4 ): 239 - 244 .
Tobias DK , Hu FB , Forman JP , et al. Increased risk of hypertension after gestational diabetes mellitus: findings from a large prospective cohort study . Diabetes Care. 2011 ; 34 ( 7 ): 1582 - 1584 .
Tobias DK , Stuart JJ , Li S , et al. Association of history of gestational diabetes with long-term cardiovascular disease risk in a large prospective cohort of US Women . JAMA Intern Med. 2017 ; 177 ( 12 ): 1735 - 1742 .
Brown HL , Warner JJ , Gianos E , et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists . Circulation. 2018 ; 137 ( 24 ): e843 - ee52 .
Knudsen LS , Christensen IJ , Lottenburger T , et al. Pre-analytical and biological variability in circulating interleukin 6 in healthy subjects and patients with rheumatoid arthritis . Biomarkers. 2008 ; 13 ( 1 ): 59 - 78 .
Alwan N , Tuffnell DJ , West J . Treatments for gestational diabetes . Cochrane Database Syst Rev. 2009 ; 3 : CD003395 .
Jovanovic-Peterson L , Peterson CM , Reed GF , et al. Maternal postprandial glucose levels and infant birth weight: the Diabetes in Early Pregnancy Study. The National Institute of Child Health and Human Development—Diabetes in Early Pregnancy Study . Am J Obstet Gynecol. 1991 ; 164 ( 1 Pt 1 ): 103 - 111 .
Bain E , Crane M , Tieu J , et al. Diet and exercise interventions for preventing gestational diabetes mellitus . Cochrane Database Syst Rev. 0443 ; 2015 ; 4 : CD01 .
Duarte-Gardea MO , Gonzales-Pacheco DM , Reader DM , et al. Academy of nutrition and dietetics gestational diabetes evidence-based nutrition practice guideline . J Acad Nutr Diet. 2018 ; 118 ( 9 ): 1719 - 1742 .
Rasmussen KM , Yaktine AL , eds.; Institute of Medicine and National Research Council Committee to Reexamine IOM Pregnancy Weight Guidelines . Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press ; 2009 .
Jovanovic-Peterson L , Peterson CM . Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes . J Am Coll Nutr. 1990 ; 9 ( 4 ): 320 - 325 .
Hernandez TL , Van Pelt RE , Anderson MA , et al. A higher-complex carbohydrate diet in gestational diabetes mellitus achieves glucose targets and lowers postprandial lipids: a randomized crossover study . Diabetes Care. 2014 ; 37 ( 5 ): 1254 - 1262 .
Hernandez TL , Van Pelt RE , Anderson MA , et al. Women with gestational diabetes mellitus randomized to a higher-complex carbohydrate/low-fat diet manifest lower adipose tissue insulin resistance, inflammation, glucose, and free fatty acids: a pilot study . Diabetes Care. 2016 ; 39 ( 1 ): 39 - 42 .
Asemi Z , Tabassi Z , Samimi M , et al. Favourable effects of the Dietary Approaches to Stop Hypertension diet on glucose tolerance and lipid profiles in gestational diabetes: a randomised clinical trial . Br J Nutr. 2013 ; 109 ( 11 ): 2024 - 2030 .
Han S , Middleton P , Shepherd E , et al. Different types of dietary advice for women with gestational diabetes mellitus . Cochrane Database Syst Rev. 2017 ; 2 : CD009275 .
Yamamoto JM , Kellett JE , Balsells M , et al. Gestational diabetes mellitus and diet: a systematic review and meta-analysis of randomized controlled trials examining the impact of modified dietary interventions on maternal glucose control and neonatal birth weight . Diabetes Care. 2018 ; 41 ( 7 ): 1346 - 1361 .
Major CA , Henry MJ , De Veciana M , et al. The effects of carbohydrate restriction in patients with diet-controlled gestational diabetes . Obstet Gynecol. 1998 ; 91 ( 4 ): 600 - 604 .
American College of Obstetrics and Gynecology . Practice Bulletin No. 137: gestational diabetes mellitus . Obstet Gynecol. 2013 ; 122 ( 2 Pt 1 ): 406 - 416 .
Metzger BE , Buchanan TA , Coustan DR , et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus . Diabetes Care. 2007 ; 30 ( suppl 2 ): S251 - S260 .
American Diabetes Association . Standards of medical care in diabetes-2011 . Diabetes Care. 2011 ; 34 ( suppl 1 ): S11 - S61 .
Battaglia FC , Meschia G. An Introduction to Fetal Physiology . Academic Press ; 1986 .
Harding JE , Johnston BM . Nutrition and fetal growth . Reprod Fertil Dev. 1995 ; 7 ( 3 ): 539 - 547 .
Sweeting A , Markovic TP , Mijatovic J , et al. The carbohydrate threshold in pregnancy and gestational diabetes: how low can we go? Nutrients. 2021 ; 13 ( 8 ): 2599 .
Morisaki N , Nagata C , Yasuo S , et al. Optimal protein intake during pregnancy for reducing the risk of fetal growth restriction: the Japan Environment and Children’s Study . Br J Nutr. 2018 ; 120 ( 12 ): 1432 - 1440 .
Rizzo T , Metzger BE , Burns WJ , et al. Correlations between antepartum maternal metabolism and intelligence of offspring . N Engl J Med. 1991 ; 325 ( 13 ): 911 - 916 .
Shaw GM , Yang W . Women’s periconceptional lowered carbohydrate intake and NTD-affected pregnancy risk in the era of prefortification with folic acid . Birth Defects Res. 2019 ; 111 ( 5 ): 248 - 253 .
Mijatovic J , Louie JCY , Buso MEC , et al. Effects of a modestly lower carbohydrate diet in gestational diabetes: a randomized controlled trial . Am J Clin Nutr. 2020 ; 112 ( 2 ): 284 - 292 .
Shubert PJ , Gordon MC , Landon MB , et al. Ketoacids attenuate glucose uptake in human trophoblasts isolated from first-trimester chorionic villi . Am J Obstet Gynecol. 1996 ; 175 ( 1 ): 56 - 62 .
Catalano PM , Mele L , Landon MB , et al. Inadequate weight gain in overweight and obese pregnant women: what is the effect on fetal growth? Am J Obstet Gynecol. 2014 ; 211 ( 2 ): 137 e1 - 137 e7 .
Faucher MA , Barger MK . Gestational weight gain in obese women by class of obesity and select maternal/newborn outcomes: a systematic review . Women Birth. 2015 ; 28 ( 3 ): e70 - e79 .
Viecceli C , Remonti LR , Hirakata VN , et al. Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta-analysis . Obes Rev. 2017 ; 18 ( 5 ): 567 - 580 .
Kainer F , Weiss PA , Huttner U , et al. Levels of amniotic fluid insulin and profiles of maternal blood glucose in pregnant women with diabetes type-I . Early Hum Dev. 1997 ; 49 ( 2 ): 97 - 105 .
de Veciana M , Major CA , Morgan MA , et al. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy . N Engl J Med. 1995 ; 333 ( 19 ): 1237 - 1241 .
Hernandez TL . Glycemic targets in pregnancies affected by diabetes: historical perspective and future directions . Curr Diab Rep. 2015 ; 15 ( 1 ): 565 .
Abell SK , Boyle JA , Earnest A , et al. Impact of different glycaemic treatment targets on pregnancy outcomes in gestational diabetes . Diabet Med. 2019 ; 36 ( 2 ): 177 - 183 .
Garner P , Okun N , Keely E , et al. A randomized controlled trial of strict glycemic control and tertiary level obstetric care versus routine obstetric care in the management of gestational diabetes: a pilot study . Am J Obstet Gynecol. 1997 ; 177 ( 1 ): 190 - 195 .
Langer O , Levy J , Brustman L , et al. Glycemic control in gestational diabetes mellitus--how tight is tight enough: small for gestational age versus large for gestational age? Am J Obstet Gynecol . 1989 ; 161 ( 3 ): 646 - 653 .
Langer O , Rodriguez DA , Xenakis EM , et al. Intensified versus conventional management of gestational diabetes . Am J Obstet Gynecol. 1994 ; 170 ( 4 ): 1036 - 1046 .
Pregnancy outcomes in the diabetes control and complications trial . Am J Obstet Gynecol. 1996 ; 174 ( 4 ): 1343 - 1353 .
Martis R , Brown J , Alsweiler J , et al. Different intensities of glycaemic control for women with gestational diabetes mellitus . Cochrane Database Syst Rev. 2016 ; 4 : CD011624 .
Snyder JMI , Melzter S , Nadeau J . Gestational diabetes and glycemic control: a randomized clinical trial . Am J Obstet Gynecol. 1998 ; 178 ( 1 Pt 2 ): S55 .
Pertot T , Molyneaux L , Tan K , et al. Can common clinical parameters be used to identify patients who will need insulin treatment in gestational diabetes mellitus? Diabetes Care. 2011 ; 34 ( 10 ): 2214 - 2216 .
Rowan JA , Hague WM , Gao W , et al. Metformin versus insulin for the treatment of gestational diabetes . N Engl J Med. 2008 ; 358 ( 19 ): 2003 - 2015 .
Murphy HR , Rayman G , Duffield K , et al. Changes in the glycemic profiles of women with type 1 and type 2 diabetes during pregnancy . Diabetes Care. 2007 ; 30 ( 11 ): 2785 - 2791 .
Padmanabhan S , McLean M , Cheung NW . Falling insulin requirements are associated with adverse obstetric outcomes in women with preexisting diabetes . Diabetes Care. 2014 ; 37 ( 10 ): 2685 - 2692 .
Wong VW . Gestational diabetes mellitus in five ethnic groups: a comparison of their clinical characteristics . Diabet Med. 2012 ; 29 ( 3 ): 366 - 371 .
Barnes RA , Wong T , Ross GP , et al. A novel validated model for the prediction of insulin therapy initiation and adverse perinatal outcomes in women with gestational diabetes mellitus . Diabetologia. 2016 ; 59 ( 11 ): 2331 - 2338 .
Ryu RJ , Hays KE , Hebert MF . Gestational diabetes mellitus management with oral hypoglycemic agents . Semin Perinatol. 2014 ; 38 ( 8 ): 508 - 515 .
Camelo Castillo W , Boggess K , Sturmer T , et al. Trends in glyburide compared with insulin use for gestational diabetes treatment in the United States, 2000-2011 . Obstet Gynecol. 2014 ; 123 ( 6 ): 1177 - 1184 .
Langer O , Conway DL , Berkus MD , et al. A comparison of glyburide and insulin in women with gestational diabetes mellitus . N Engl J Med. 2000 ; 343 ( 16 ): 1134 - 1138 .
Kremer CJ , Duff P . Glyburide for the treatment of gestational diabetes . Am J Obstet Gynecol. 2004 ; 190 ( 5 ): 1438 - 1439 .
Camelo Castillo W , Boggess K , Sturmer T , et al. Association of adverse pregnancy outcomes with glyburide vs insulin in women with gestational diabetes . JAMA Pediatr. 2015 ; 169 ( 5 ): 452 - 458 .
Schwartz RA , Rosenn B , Aleksa K , et al. Glyburide transport across the human placenta . Obstet Gynecol. 2015 ; 125 ( 3 ): 583 - 588 .
Cheng YW , Chung JH , Block-Kurbisch I , et al. Treatment of gestational diabetes mellitus: glyburide compared to subcutaneous insulin therapy and associated perinatal outcomes . J Matern Fetal Neonatal Med. 2012 ; 25 ( 4 ): 379 - 384 .
Lindsay RS , Loeken MR . Metformin use in pregnancy: promises and uncertainties . Diabetologia. 2017 ; 60 ( 9 ): 1612 - 1619 .
Charles B , Norris R , Xiao X , et al. Population pharmacokinetics of metformin in late pregnancy . Ther Drug Monit. 2006 ; 28 ( 1 ): 67 - 72 .
Tarry-Adkins JL , Aiken CE , Ozanne SE . Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: a systematic review and meta-analysis . PLoS Med. 2019 ; 16 ( 8 ): e1002848 .
Feig DS , Donovan LE , Zinman B , et al. Metformin in women with type 2 diabetes in pregnancy (MiTy): a multicentre, international, randomised, placebo-controlled trial . Lancet Diabetes Endocrinol. 2020 ; 8 ( 10 ): 834 - 844 .
Niromanesh S , Alavi A , Sharbaf FR , et al. Metformin compared with insulin in the management of gestational diabetes mellitus: a randomized clinical trial . Diabetes Res Clin Pract. 2012 ; 98 ( 3 ): 422 - 429 .
Khin MO , Gates S , Saravanan P . Predictors of metformin failure in gestational diabetes mellitus (GDM) . Diabetes Metab Syndr. 2018 ; 12 ( 3 ): 405 - 410 .
Rowan JA , Rush EC , Obolonkin V , et al. Metformin in gestational diabetes: the offspring follow-up (MiG TOFU): body composition at 2 years of age . Diabetes Care. 2011 ; 34 ( 10 ): 2279 - 2284 .
Rowan JA , Rush EC , Plank LD , et al. Metformin in gestational diabetes: the offspring follow-up (MiG TOFU): body composition and metabolic outcomes at 7-9 years of age . BMJ Open Diabetes Res Care. 2018 ; 6 ( 1 ): e000456 .
Hanem LGE , Stridsklev S , Juliusson PB , et al. Metformin use in PCOS pregnancies increases the risk of offspring overweight at 4 years of age: follow-up of two RCTs . J Clin Endocrinol Metab. 2018 ; 103 ( 4 ): 1612 - 1621 .
Brown J , Martis R , Hughes B , et al. Oral anti-diabetic pharmacological therapies for the treatment of women with gestational diabetes . Cochrane Database Syst Rev. 2017 ; 1 : CD011967 .
Balsells M , Garcia-Patterson A , Sola I , et al. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis . BMJ. 2015 ; 350 : h102 .
Poolsup N , Suksomboon N , Amin M . Efficacy and safety of oral antidiabetic drugs in comparison to insulin in treating gestational diabetes mellitus: a meta-analysis . PLoS One. 2014 ; 9 ( 10 ): e109985 .
Nachum Z , Zafran N , Salim R , et al. Glyburide versus metformin and their combination for the treatment of gestational diabetes mellitus: a randomized controlled study . Diabetes Care. 2017 ; 40 ( 3 ): 332 - 337 .
Sacco F , Calderone A , Castagnoli L , et al. The cell-autonomous mechanisms underlying the activity of metformin as an anticancer drug . Br J Cancer. 2016 ; 115 ( 12 ): 1451 - 1456 .
Barbour LA , Davies JK . Comment on Nachum et al . Glyburide versus metformin and their combination for the treatment of gestational diabetes mellitus: a randomized controlled study. Diabetes Care. 2017;40:332-337. Diabetes Care. 2017; 40 (8):e115.
Rao U , de Vries B , Ross GP , et al. Fetal biometry for guiding the medical management of women with gestational diabetes mellitus for improving maternal and perinatal health . Cochrane Database Syst Rev. 2019 ; 9 : CD012544 .
Schaefer-Graf UM , Kjos SL , Fauzan OH , et al. A randomized trial evaluating a predominantly fetal growth-based strategy to guide management of gestational diabetes in Caucasian women . Diabetes Care. 2004 ; 27 ( 2 ): 297 - 302 .
Schaefer-Graf UM , Wendt L , Sacks DA , et al. How many sonograms are needed to reliably predict the absence of fetal overgrowth in gestational diabetes mellitus pregnancies? Diabetes Care. 2011 ; 34 ( 1 ): 39 - 43 .
Kjos SL , Schaefer-Graf UM . Modified therapy for gestational diabetes using high-risk and low-risk fetal abdominal circumference growth to select strict versus relaxed maternal glycemic targets . Diabetes Care. 2007 ; 30 ( suppl 2 ): S200 - S205 .
Nelson L , Wharton B , Grobman WA . Prediction of large for gestational age birth weights in diabetic mothers based on early third-trimester sonography . J Ultrasound Med. 2011 ; 30 ( 12 ): 1625 - 1628 .
McLean A , Katz M , Oats J , et al. Rethinking third trimester ultrasound measurements and risk of adverse neonatal outcomes in pregnancies complicated by hyperglycaemia: a retrospective study . Aust N Z J Obstet Gynaecol. 2021 ; 61 ( 3 ): 366 - 372 .
American College of Obstetricians and Gynecologists . ACOG Committee Opinion No. 560: medically indicated late-preterm and early-term deliveries . Obstet Gynecol. 2013 ; 121 ( 4 ): 908 - 910 .
Metcalfe A , Hutcheon JA , Sabr Y , et al. Timing of delivery in women with diabetes: a population-based study . Acta Obstet Gynecol Scand. 2020 ; 99 ( 3 ): 341 - 349 .
Hunt KJ , Logan SL , Conway DL , et al. Postpartum screening following GDM: how well are we doing? Curr Diab Rep. 2010 ; 10 ( 3 ): 235 - 241 .
Gabbe SG , Landon MB , Warren-Boulton E , et al. Promoting health after gestational diabetes: a National Diabetes Education Program call to action . Obstet Gynecol. 2012 ; 119 ( 1 ): 171 - 176 .
Ehrlich SF , Hedderson MM , Feng J , et al. Change in body mass index between pregnancies and the risk of gestational diabetes in a second pregnancy . Obstet Gynecol. 2011 ; 117 ( 6 ): 1323 - 1330 .
Kim C , Newton KM , Knopp RH . Gestational diabetes and the incidence of type 2 diabetes: a systematic review . Diabetes Care. 2002 ; 25 ( 10 ): 1862 - 1868 .
Bellamy L , Casas JP , Hingorani AD , et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis . Lancet. 2009 ; 373 ( 9677 ): 1773 - 1779 .
Dornhorst A , Bailey PC , Anyaoku V , et al. Abnormalities of glucose tolerance following gestational diabetes . Q J Med. 1990 ; 77 ( 284 ): 1219 - 1228 .
Aroda VR , Christophi CA , Edelstein SL , et al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up . J Clin Endocrinol Metab. 2015 ; 100 ( 4 ): 1646 - 1653 .
Pirc LK , Owens JA , Crowther CA , et al. Mild gestational diabetes in pregnancy and the adipoinsular axis in babies born to mothers in the ACHOIS randomised controlled trial . BMC Pediatr. 2007 ; 7 : 18 .
Landon MB , Rice MM , Varner MW , et al. Mild gestational diabetes mellitus and long-term child health . Diabetes Care. 2015 ; 38 ( 3 ): 445 - 452 .
Dabelea D , Pettitt DJ . Intrauterine diabetic environment confers risks for type 2 diabetes mellitus and obesity in the offspring, in addition to genetic susceptibility . J Pediatr Endocrinol Metab. 2001 ; 14 ( 8 ): 1085 - 1091 .
Pettitt DJ , Baird HR , Aleck KA , et al. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy . N Engl J Med. 1983 ; 308 ( 5 ): 242 - 245 .
Gillman MW , Rifas-Shiman S , Berkey CS , Field AE , Colditz GA . Maternal gestational diabetes, birth weight, and adolescent obesity . Pediatrics. 2003 ; 111 ( 3 ): e221 - e226 .
Plagemann A , Harder T , Kohlhoff R , et al. Overweight and obesity in infants of mothers with long-term insulin-dependent diabetes or gestational diabetes . Int J Obes Relat Metab Disord. 1997 ; 21 ( 6 ): 451 - 456 .
Pribylova H , Dvorakova L . Long-term prognosis of infants of diabetic mothers. Relationship between metabolic disorders in newborns and adult offspring . Acta Diabetol. 1996 ; 33 ( 1 ): 30 - 34 .
Silverman BL , Metzger BE , Cho NH , et al. Impaired glucose tolerance in adolescent offspring of diabetic mothers: relationship to fetal hyperinsulinism . Diabetes Care. 1995 ; 18 ( 5 ): 611 - 617 .
Crume TL , Ogden L , West NA , et al. Association of exposure to diabetes in utero with adiposity and fat distribution in a multiethnic population of youth: the Exploring Perinatal Outcomes among Children (EPOCH) Study . Diabetologia. 2011 ; 54 ( 1 ): 87 - 92 .
West NA , Crume TL , Maligie MA , et al. Cardiovascular risk factors in children exposed to maternal diabetes in utero . Diabetologia. 2011 ; 54 ( 3 ): 504 - 507 .
Hillier TA , Pedula KL , Schmidt MM , et al. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia . Diabetes Care. 2007 ; 30 ( 9 ): 2287 - 2292 .
Whincup PH , Kaye SJ , Owen CG , et al. Birth weight and risk of type 2 diabetes: a systematic review . JAMA. 2008 ; 300 ( 24 ): 2886 - 2897 .
Guerrero-Romero F , Aradillas-Garcia C , Simental-Mendia LE , et al. Birth weight, family history of diabetes, and metabolic syndrome in children and adolescents . J Pediatr. 2010 ; 156 ( 5 ): 719 - 723 , 23 e1.
Harder T , Roepke K , Diller N , et al. Birth weight, early weight gain, and subsequent risk of type 1 diabetes: systematic review and meta-analysis . Am J Epidemiol. 2009 ; 169 ( 12 ): 1428 - 1436 .
Reece EA . The fetal and maternal consequences of gestational diabetes mellitus . J Matern Fetal Neonatal Med. 2010 ; 23 ( 3 ): 199 - 203 .
Ornoy A . Prenatal origin of obesity and their complications: gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia . Reprod Toxicol. 2011 ; 32 ( 2 ): 205 - 212 .
Page KA , Romero A , Buchanan TA , et al. Gestational diabetes mellitus, maternal obesity, and adiposity in offspring . J Pediatr. 2014 ; 164 ( 4 ): 807 - 810 .
Grunnet LG , Hansen S , Hjort L , et al. Adiposity, dysmetabolic traits, and earlier onset of female puberty in adolescent offspring of women with gestational diabetes mellitus: a clinical study within the Danish National Birth Cohort . Diabetes Care. 2017 ; 40 ( 12 ): 1746 - 1755 .
Logan KM , Emsley RJ , Jeffries S , et al. Development of early adiposity in infants of mothers with gestational diabetes mellitus . Diabetes Care. 2016 ; 39 ( 6 ): 1045 - 1051 .
Catalano PM , Farrell K , Thomas A , et al. Perinatal risk factors for childhood obesity and metabolic dysregulation . Am J Clin Nutr. 2009 ; 90 ( 5 ): 1303 - 1313 .
Chung WK , Erion K , Florez JC , et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) . Diabetes Care. 2020 ; 43 ( 7 ): 1617 - 1635 .
Cheney C , Shragg P , Hollingsworth D . Demonstration of heterogeneity in gestational diabetes by a 400-kcal breakfast meal tolerance test . Obstet Gynecol. 1985 ; 65 ( 1 ): 17 - 23 .
Powe CE , Allard C , Battista MC , et al. Heterogeneous contribution of insulin sensitivity and secretion defects to gestational diabetes mellitus . Diabetes Care. 2016 ; 39 ( 6 ): 1052 - 1055 .
Catalano PM , Tyzbir ED , Roman NM , et al. Longitudinal changes in insulin release and insulin resistance in nonobese pregnant women . Am J Obstet Gynecol. 1991 ; 165 ( 6 Pt 1 ): 1667 - 1672 .
Powe CE , Hivert MF , Udler MS . Defining heterogeneity among women with gestational diabetes mellitus . Diabetes. 2020 ; 69 ( 10 ): 2064 - 2074 .
Benhalima K , Van Crombrugge P , Moyson C , et al. Characteristics and pregnancy outcomes across gestational diabetes mellitus subtypes based on insulin resistance . Diabetologia. 2019 ; 62 ( 11 ): 2118 - 2128 .
Sweeting A , Park F , Hyett J . The first trimester: prediction and prevention of the great obstetrical syndromes . Best Pract Res Clin Obstet Gynaecol. 2015 ; 29 ( 2 ): 183 - 193 .
Coustan DR , Nelson C , Carpenter MW , et al. Maternal age and screening for gestational diabetes: a population-based study . Obstet Gynecol. 1989 ; 73 ( 4 ): 557 - 561 .
Lavin JP Jr . Screening of high-risk and general populations for gestational diabetes. Clinical application and cost analysis . Diabetes. 1985 ; 34 ( suppl 2 ): 24 - 27 .
Weeks JW , Major CA , de Veciana M , et al. Gestational diabetes: does the presence of risk factors influence perinatal outcome? Am J Obstet Gynecol. 1994 ; 171 ( 4 ): 1003 - 1007 .
Cosson E , Benbara A , Pharisien I , et al. Diagnostic and prognostic performances over 9 years of a selective screening strategy for gestational diabetes mellitus in a cohort of 18,775 subjects . Diabetes Care. 2013 ; 36 ( 3 ): 598 - 603 .
Chevalier N , Fenichel P , Giaume V , et al. Universal two-step screening strategy for gestational diabetes has weak relevance in French Mediterranean women: should we simplify the screening strategy for gestational diabetes in France? Diabetes Metab. 2011 ; 37 ( 5 ): 419 - 425 .
Moses RG , Moses J , Davis WS . Gestational diabetes: do lean young Caucasian women need to be tested? Diabetes Care. 1998 ; 21 ( 11 ): 1803 - 1806 .
Avalos GE , Owens LA , Dunne F , et al. Applying current screening tools for gestational diabetes mellitus to a European population: is it time for change? Diabetes Care. 2013 ; 36 ( 10 ): 3040 - 3044 .
Teede HJ , Harrison CL , Teh WT , et al. Gestational diabetes: development of an early risk prediction tool to facilitate opportunities for prevention . Aust N Z J Obstet Gynaecol. 2011 ; 51 ( 6 ): 499 - 504 .
Syngelaki A , Pastides A , Kotecha R , et al. First-trimester screening for gestational diabetes mellitus based on maternal characteristics and history . Fetal Diagn Ther. 2015 ; 38 ( 1 ): 14 - 21 .
Savvidou M , Nelson SM , Makgoba M , et al. First-trimester prediction of gestational diabetes mellitus: examining the potential of combining maternal characteristics and laboratory measures . Diabetes. 2010 ; 59 ( 12 ): 3017 - 3022 .
Lamain-de Ruiter M , Kwee A , Naaktgeboren CA , et al. Prediction models for the risk of gestational diabetes: a systematic review . Diagn Progn Res. 2017 ; 1 : 3 .
Sweeting AN , Wong J , Appelblom H , et al. A novel early pregnancy risk prediction model for gestational diabetes mellitus . Fetal Diagn Ther. 2019 ; 45 ( 2 ): 76 - 84 .
Sweeting AN , Wong J , Appelblom H , et al. A first trimester prediction model for gestational diabetes utilizing aneuploidy and pre-eclampsia screening markers . J Matern Fetal Neonatal Med. 2018 ; 31 ( 16 ): 2122 - 2130 .
Aronson JK , Ferner RE . Biomarkers-a general review . Curr Protoc Pharmacol. 2017 ; 76 : 9 23 19 17 .
Allinson JL . Clinical biomarker validation . Bioanalysis. 2018 ; 10 ( 12 ): 957 - 968 .
Sattar N , Wannamethee SG , Forouhi NG . Novel biochemical risk factors for type 2 diabetes: pathogenic insights or prediction possibilities? Diabetologia. 2008 ; 51 ( 6 ): 926 - 940 .
O’Malley EG , Reynolds CME , Killalea A , et al. The use of biomarkers at the end of the second trimester to predict Gestational Diabetes Mellitus . Eur J Obstet Gynecol Reprod Biol. 2020 ; 250 : 101 - 106 .
Richardson AC , Carpenter MW . Inflammatory mediators in gestational diabetes mellitus . Obstet Gynecol Clin North Am. 2007 ; 34 ( 2 ): 213 - 224 , viii.
Eleftheriades M , Papastefanou I , Lambrinoudaki I , et al. Elevated placental growth factor concentrations at 11-14 weeks of gestation to predict gestational diabetes mellitus . Metabolism. 2014 ; 63 ( 11 ): 1419 - 1425 .
Lovati E , Beneventi F , Simonetta M , et al. Gestational diabetes mellitus: including serum pregnancy-associated plasma protein-A testing in the clinical management of primiparous women? A case-control study . Diabetes Res Clin Pract. 2013 ; 100 ( 3 ): 340 - 347 .
White SL , Lawlor DA , Briley AL , et al. Early antenatal prediction of gestational diabetes in obese women: development of prediction tools for targeted intervention . PLoS One. 2016 ; 11 ( 12 ): e0167846 .
Rasanen JP , Snyder CK , Rao PV , et al. Glycosylated fibronectin as a first-trimester biomarker for prediction of gestational diabetes . Obstet Gynecol. 2013 ; 122 ( 3 ): 586 - 594 .
Watanabe N , Morimoto S , Fujiwara T , et al. Prediction of gestational diabetes mellitus by soluble (pro)renin receptor during the first trimester . J Clin Endocrinol Metab. 2013 ; 98 ( 6 ): 2528 - 2535 .
Theriault S , Giguere Y , Masse J , et al. Early prediction of gestational diabetes: a practical model combining clinical and biochemical markers . Clin Chem Lab Med. 2016 ; 54 ( 3 ): 509 - 518 .
Syngelaki A , Kotecha R , Pastides A , et al. First-trimester biochemical markers of placentation in screening for gestational diabetes mellitus . Metabolism. 2015 ; 64 ( 11 ): 1485 - 1489 .
Gobl CS , Bozkurt L , Rivic P , et al. A two-step screening algorithm including fasting plasma glucose measurement and a risk estimation model is an accurate strategy for detecting gestational diabetes mellitus . Diabetologia. 2012 ; 55 ( 12 ): 3173 - 3181 .
Australasian Diabetes in Pregnancy Society. Diagnostic testing for gestational diabetes mellitus (GDM) during the COVID 19 pandemic: antenatal and postnatal testing advice: a statement from the Australasian Diabetes in Pregnancy Society (ADIPS) . Last updated April 7, 2020. Accessed June 12, 2021 . https://www.adips.org/documents/COVID19-WITHQLDGUIDELINES0704201150ADIPSADSADEADAupdated.pdf
Royal College of Obstetricians . Guidance for maternal medicine in the evolving coronavirus Covid-19 pandemic . Published July 10, 2020 . Accessed June 30, 2021. https://www.rcog.org.uk/globalassets/documents/guidelines/2020-07-10-guidance-for-maternal-medicine.pdf
Simmons D , Rudland VL , Wong V , et al. Options for screening for gestational diabetes mellitus during the SARS-CoV-2 pandemic . Aust N Z J Obstet Gynaecol. 2020 ; 60 ( 5 ): 660 - 666 .
McIntyre HD , Gibbons KS , Ma RCW , et al. Testing for gestational diabetes during the COVID-19 pandemic. An evaluation of proposed protocols for the United Kingdom, Canada and Australia . Diabetes Res Clin Pract. 2020 ; 167 : 108353 .
Meek CL , Lindsay RS , Scott EM , et al. Approaches to screening for hyperglycaemia in pregnant women during and after the COVID-19 pandemic . Diabet Med. 2021 ; 38 ( 1 ): e14380 .
| Month: | Total Views: |
|---|---|
| January 2022 | 135 |
| February 2022 | 217 |
| March 2022 | 521 |
| April 2022 | 639 |
| May 2022 | 802 |
| June 2022 | 809 |
| July 2022 | 1,607 |
| August 2022 | 752 |
| September 2022 | 1,986 |
| October 2022 | 3,671 |
| November 2022 | 2,602 |
| December 2022 | 1,565 |
| January 2023 | 1,823 |
| February 2023 | 2,389 |
| March 2023 | 3,133 |
| April 2023 | 3,125 |
| May 2023 | 3,154 |
| June 2023 | 2,608 |
| July 2023 | 3,019 |
| August 2023 | 2,642 |
| September 2023 | 2,821 |
| October 2023 | 3,583 |
| November 2023 | 3,852 |
| December 2023 | 2,512 |
| January 2024 | 2,948 |
| February 2024 | 3,215 |
| March 2024 | 3,424 |
| April 2024 | 3,092 |
| May 2024 | 3,027 |
| June 2024 | 2,470 |
| July 2024 | 2,439 |
| August 2024 | 823 |
Email alerts
Citing articles via.
- About the Endocrine Society
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1945-7189
- Print ISSN 0163-769X
- Copyright © 2024 Endocrine Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 05 August 2024
Functional genetic variants and susceptibility and prediction of gestational diabetes mellitus
- Gongchen Huang 1 na1 ,
- Yan Sun 1 na1 ,
- Ruiqi Li 1 ,
- Qiulian Liang 1 &
- Xiangyuan Yu 1
Scientific Reports volume 14 , Article number: 18123 ( 2024 ) Cite this article
183 Accesses
2 Altmetric
Metrics details
- Computational biology and bioinformatics
- Endocrinology
- Risk factors
The aetiological mechanism of gestational diabetes mellitus (GDM) has still not been fully understood. The aim of this study was to explore the associations between functional genetic variants screened from a genome-wide association study (GWAS) and GDM risk among 554 GDM patients and 641 healthy controls in China. Functional analysis of single nucleotide polymorphisms (SNPs) positively associated with GDM was further performed. Univariate regression and multivariate logistic regression analyses were used to screen clinical risk factors, and a predictive nomogram model was established. After adjusting for age and prepregnancy BMI, rs9283638 was significantly associated with GDM susceptibility ( P < 0.05). Moreover, an obvious interaction between rs9283638 and clinical variables was detected ( P interaction < 0.05). Functional analysis confirmed that rs9283638 can regulate not only target gene transcription factor binding, but it also regulates the mRNA levels of SAMD7 ( P < 0.05). The nomogram model constructed with the factors of age, FPG, 1hPG, 2hPG, HbA1c, TG and rs9283638 revealed an area under the ROC curve of 0.920 (95% CI 0.902–0.939). Decision curve analysis (DCA) suggested that the model had greater net clinical benefit. Conclusively, genetic variants can alter women's susceptibility to GDM by affecting the transcription of target genes. The predictive nomogram model constructed based on genetic and clinical variables can effectively distinguish individuals with different GDM risk factors.
Similar content being viewed by others

Fine-tuning of Genome-Wide Polygenic Risk Scores and Prediction of Gestational Diabetes in South Asian Women
Genetic polymorphisms associated with adverse pregnancy outcomes in nulliparas

Distinct and shared genetic architectures of gestational diabetes mellitus and type 2 diabetes
Introduction.
Gestational diabetes mellitus (GDM) is one of the most common complications of pregnancy and is defined as the onset or the first discovery of glucose intolerance during pregnancy 1 . Worldwide, it affects approximately 2–20% of all pregnant women, but, in China, approximately 14.8% of pregnant women are affected 2 . Studies have confirmed that GDM can ultimately lead to adverse outcomes and long-term adverse effects on mothers and their offspring, such as foetal macrosomia, preeclampsia (PE), preterm birth, spontaneous abortion, respiratory distress syndrome, small for gestational age (SGA), large for gestational age (LGA), polycythemia, future obesity and type 2 diabetes mellitus (T2DM) 3 , 4 , 5 . GDM poses a serious threat to the health and quality of life of patients and their offspring 6 , 7 .
Similar to the pathogenesis of T2DM, GDM can be caused by insulin resistance and insufficient insulin secretion compensation 8 , 9 . Currently, the known causes of GDM include older age at pregnancy, prepregnancy overweight or obesity, excessive weight gain during pregnancy, family history of T2DM, and past history of GDM 8 , 10 . Epidemiological evidence shows that a family history of diabetes is an independent risk factor for GDM, and the closer individuals are to diabetes patients, the greater the risk of GDM is during pregnancy 11 , 12 . In addition, the incidence rate of GDM in Asian women during pregnancy is approximately 3–7 times greater than that in Caucasians 13 , 14 . This indicates that genetic factors are also involved in the pathogenesis of GDM. Therefore, identifying individual genetic risk factors for GDM is highly important for disease prevention and control.
Single nucleotide polymorphisms (SNPs) are the main variant form of the human genome and determine the core information of genetic susceptibility to disease. It has been widely applied in disease risk prediction and patient prognosis assessment 15 . SNPs located in different functional regions of genes may affect promoter and enhancer activity, alternative splicing, messenger RNA (mRNA) conformation and posttranscription level, protein function and structure and even cause changes in the biological traits of an individual 16 , 17 , 18 . Genome-wide association studies (GWASs) are considered an effective approach for detecting SNPs associated with complex disease phenotypes or traits across the entire genome, providing more genetic clues for the pathogenesis of human diseases. At present, a certain number of GDM susceptibility SNPs have been successfully identified 14 , 19 , 20 , 21 .
Disease prediction models can predict individuals’ probability of developing disease or experiencing certain conditions in the future 22 . Previous studies have extensively constructed GDM nomogram prediction models based on conventional clinical parameters (age, BMI, blood pressure, FPG, HbA1c, glucose and lipid levels, etc.) for early disease detection, prevention and treatment 23 , 24 , 25 . During the construction process of the nomogram model, the factors included in the model were scored based on the size of the logistic regression coefficients and then presented in the form of scaled line segments. The probability of corresponding outcome events occurring was determined by calculating the total score. This type of model can effectively predict the risk of individual GDM occurrence and help doctors make decisions through the use of visualized clinical predictions that provide personalized and highly accurate risk estimates 26 . However, there is a lack of risk factors characterized by genetic susceptibility as a predictive indicator. It is of great clinical significance to establish a practical risk prediction model for complex human diseases, including GDM prevention and control, by combining genetic variants and environmental risk factors.
Here, a large sample size case‒control study was conducted to validate the effects of SNPs screened by GWAS on the incidence of GDM. Subsequently, a nomogram model with GDM-positively associated SNPs and clinical indicators was constructed for early GDM prediction.
Study population
All subjects who met the following inclusion criteria were enrolled in the Affiliated Hospital of Guilin Medical University from September 2014 to April 2016: singleton pregnancy, no family relationship and no metabolic disease, such as type 1/2 diabetes mellitus. A routine 75-g oral glucose tolerance test (OGTT) was performed between 24 and 28 weeks of gestation. According to the standards of the International Association of Diabetes and Pregnancy Research Groups (IADPSG), women can be diagnosed with GDM if their fasting plasma glucose (FPG) is ≥ 5.1 mmol/L, 1-h plasma glucose (1hPG) is ≥ 10.0 mm/L or 2-h plasma glucose (2hPG) is ≥ 8.5 mmol/L.
At the initial discovery stage, 96 GDM patients and age and pre-BMI matched 96 healthy pregnant women from the same period were recruited to conduct a genome-wide association study (GWAS) for screening GDM associated SNPs (GDM-SNPs) by using infinium Asian Screening Array (ASA, illumina) BeadChip. During the validation phase, singleton pregnant women of the same conditions were recruited, and candidate SNPs were genotyped in 554 GDM patients and 641 healthy pregnancies. In addition, biological samples from the other 42 normal pregnant women, including peripheral whole blood and placental tissues, were collected to detect the biological functions of the positively associated variants.
The Ethics Committee of Guilin Medical University approved this research (Number: GLMC20131205), and the study was conducted in accordance with the Declaration of Helsinki. All included subjects signed informed consent forms prior to study procedures. The details of this study design are depicted in the flowchart in Fig. 1 .
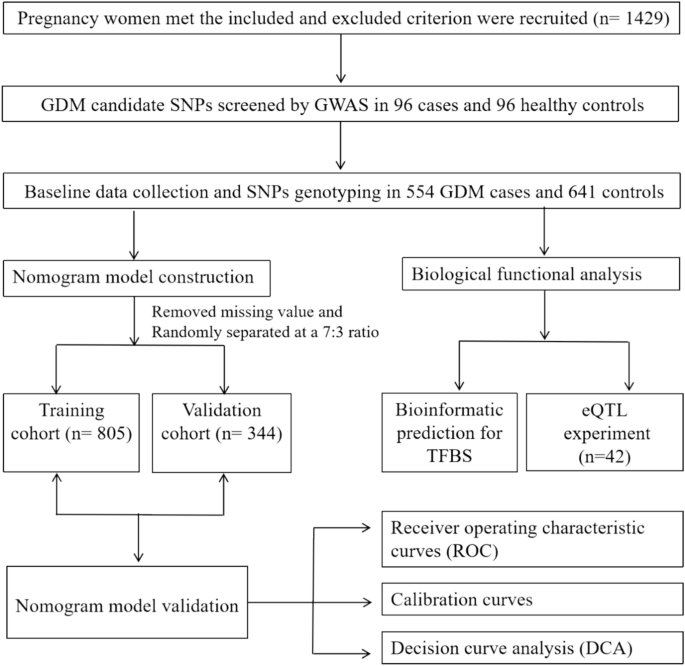
The flowchart of the study design. TFBS indicated transcription factor-binding sites, e QTL indicated expression quantitative trait locus.
Infinium Asian screening array (ASA)
All DNA samples were extracted using DNA-extraction kits (Tiangen Biotech). Genotyping module of Genomestudio v2.1 (illumina) was used to call the genotype, and to obtain high-quality data for GWAS. We pruned the data set of discovery stage with the following criteria: (1) SNP call rate > 95%, and a threshold for Hardy–Weinberg equilibrium (HWE) of 0.0001, minimum allele frequencies (MAF) < 1% and sex chromosome SNP sites; (2) Sample call rates > 95%; In addition, to exclude closely related individuals, we calculated genome-wide identity by descent (IBD) for each pair of samples and removed samples with PI-HAT > 0.25. We took group analysis quality control from 1000Geomics Northern and Western European Ancestry (CEU), Japanese in Tokyo (JPT) and Han Chinese in Bejing (CHB) database to Confirm whether the sample grouping meets expectations and detect outlier samples.
Clinical and biochemical characteristics
Clinical and biological characteristics, including age, prepregnancy weight (kg), height (m), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting plasma glucose (FPG), 1-h plasma glucose (1hPG), 2-h plasma glucose (2hPG), triglyceride (TG), total cholesterol (TC), haemoglobin A1c (HbA1c), low-density lipoprotein cholesterol (LDL-c) and high-density lipoprotein cholesterol (HDL-c), etc., were obtained from a unified questionnaire and patient medical records.
Candidate SNP selection and genotyping
Preliminary selection of candidate SNPs was based on the strength of the association effect on GDM ( P < 1.0 × 10 −3 ) according to the Infinium Asian Screening Array (ASA) BeadChip. The SNP function prediction (FuncPred) tool ( https://manticore.niehs.nih.gov/snpinfo/snpfunc.html ) was subsequently used for screening potential functional variants in the Chinese Han population in Beijing (CHB) with minimum allele frequencies (MAF) greater than 0.05.
The candidate variants were genotyped via the Sequenom MassARRAY platform. The multiplex PCR master mix was composed of 1.0 μl of template DNA (20 ~ 100 ng/μl), 1.850 μl of ddH 2 O, 0.625 μl of 1.25 × PCR buffer (15 mmol/L MgCl 2 ), 0.325 μl of 25 mmol/L MgCl 2 , 0.1 μl of 25 mmol/L dNTPs, 1 μl of 0.5 μmol/L primer mix, and 0.1 μl of 5 U/μl HotStar Taq polymerase. The reaction was conducted at 94 °C for 15 min, followed by 45 cycles at 94 °C for 20 s, 56 °C for 30 s and 72 °C for 1 min, with a final incubation at 72 °C for 3 min. The primers used are listed in Supplemental Table S1 .
Functional analysis of positively associated SNPs
For positively associated SNPs located in TFBSs, the Alibaba 2.1 tool ( http://gene-regulation.com/pub/programs/alibaba2/index.html ) was used to explore potential biological functions. In addition, to determine whether the SNP was an expression quantitative trait locus (eQTL), we also carried out validated experiments in our study.
According to the Aidlab DNA Extraction Kit (Aidlab Biotechnology Co., Ltd., China), genomic DNA was extracted from peripheral blood of 42 healthy pregnant women, and then the optical density values of each sample at 260 nm and 280 nm were measured using a NanoDrop spectrophotometer (Thermo Scientific, Waltham, MA, USA) to determine the DNA concentration and purity. Next, the genotypes of the candidate SNPs were determined using Kompetitive Allele Specific Polymerase Chain Reaction (KASP) 27 in a StepOnePlus™ real-time PCR system (Thermo Fisher Scientific, Life Technologies Holding Pte Ltd., China). The 10-µl reaction system contained 5 µl of Flu Arms 2 × PCR mix, 0.5 µl of three specific primers (F1: 0.1 µl, F2: 0.1 µl, and R: 0.3 µl), 0.5 µl (25–150 ng) of DNA and 4 µl of ddH 2 O. The cycling conditions were as follows: hot-start Tap activation at 95 °C for 3 min, followed by 10 touchdown cycles at 95 °C for 15 s and at 61–55 °C for 60 s (61 °C decreasing to 0.6 °C per cycle to achieve a final annealing and elongation temperature of 55 °C), followed by 30 amplification cycles at 95 °C for 15 s, 55 °C for 60 s and postread at 30 °C for 60 s. The primer sequences are shown in Supplemental Table S1 .
Total RNA was extracted from the placental tissues of 42 normal pregnant women using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. The concentration and purity of the extracted RNA were tested using a Thermo Scientific Nanodrop-2000c microspectrophotometer. Total RNA (2 µg) was reverse transcribed into cDNA according to the instructions for the reverse transcription kit (HaiGene, Harbin, China). Finally, quantitative real time polymerase chain reaction (QRT-PCR) was performed using the GLPBIO SYBR Green qPCR Mix (2 ×) kit on the StepOne Plus TM real-time PCR system. The 10 µl RT‒qPCR system contained 1 µl of cDNA template, 5 µl of 2 × SYBR Green PCR Mastermix, 2 µl of forwards and reverse primer concentrations and 3.4 µl of DEPC ddH2O. The PCR mixtures were denatured at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 65 °C for 60 s. The 2^(− ΔΔCt) method was used to quantify gene expression, with GAPDH serving as an internal control 28 . The primer sequences are shown in Supplemental Table S1 .
Data processing
In this study, the data were processed with IBM SPSS Statistics 28 for Windows (IBM Corp., Armonk, NY, USA) and R 4.3.1 software. Clinical and biochemical variables are shown as the mean ± SD or percentage and were analysed using independent sample t tests or chi square (χ 2 ) tests. Logistic regression analysis was adopted to evaluate the association between variants and GDM risk with the odds ratio (OR) and its corresponding 95% confidence interval (CI). One-way ANOVA was used to compare expression levels among the different genotypic samples. Additionally, univariate logistic regression and multivariate regression analysis by forwards stepwise selection with the Akaike information criterion (AIC) were employed to determine the clinical risk factors for GDM.
A predictive nomogram model composed of clinical risk factors and positive SNPs was eventually constructed using the R package “rms”. The area under the receiver operating characteristic curve (AUC) was used to evaluate the model’s performance. The calibration curve by internal validation with a bootstrap method with 1000 resamples was generated to assess the level of consistency between the predicted and observed values. The clinical utility and net benefit were estimated by decision curve analysis (DCA). Finally, a web-based interactive dynamic nomogram was established via the R package “DynNom”. A two-sided test was adopted, and P values < 0.05 were considered to indicate statistical significance.
Patient characteristics
The selected characteristics of the patients are shown in Table 1 . There were no significant differences in TC, HDL-c or LDL-c between the two groups ( P > 0.05). However, the mean age, pre-BMI, SBP, DBP, FPG, 1hPG, 2hPG, HbA1c and TG levels in GDM patients were much greater than those in controls ( P < 0.05).
Candidate SNPs Screening
According to the GWAS, a large amount of GDM associated SNPs were screened (Fig. 2 ). Based on the established variant screening strategy, 5 SNPs were ultimately selected, of which 4 SNPs (rs17099985, rs9283638, rs6798181, rs796749) were predicted to be located at transcription factor-binding sites (TFBS), and one SNP (rs1742473) was predicted to be located at a splicing site (SS) (Supplemental Table S2 ).

Manhattan plot demonstrating the -log 10 P value for the SNPs in the gestational diabetes mellitus genome-wide association study at the discovery stage. The red line represents the genome-wide significance threshold ( P = 5 × 10 –4 ).
SAMD7 rs9283638 C > T and GDM risk
The frequency distribution of the three genotypes of the 5 variants followed the Hardy Weinberg equilibrium (HWE) law ( P HWE > 0.05) in the control group. Significant differences in the genotype distribution of rs9283638 were observed between GDM patients and controls (χ 2 = 9.06, P = 0.011) (Table 2 ).
Unconditional logistic regression analysis revealed that rs9283638 was significantly associated with GDM risk. Compared with the CC genotype, the TT genotype increased GDM risk by 54% (TT vs. CC: crude OR = 1.54, 95% CI 1.05–2.26, P = 0.029). However, after adjusting for age and BMI, the positive associations previously described no longer existed. However, we did find a significant correlation with GDM risk in the recessive model (TT vs. CC/CT: adjusted OR = 1.57, 95% CI 1.06–2.32, P = 0.025) as shown in Table 2 .
According to the stratified analysis, compared with individuals with the CT/TT genotype, individuals with the rs9283638 TT genotype had a greater risk of GDM in the age > 30.09 years (adjusted OR = 2.80, 95% CI 1.45–5.41, P = 0.002), DBP ≤ 69.53 mmHg (adjusted OR = 1.75, 95% CI 1.06–2.91, P = 0.035) and TG subgroup ≤ 2.54 mmol/L (adjusted OR = 2.20, 95% CI 1.29–3.75, P = 0.004) subgroups. A significant interaction effect of rs9283638 with age ( P interaction = 0.017) was observed under the recessive model (Table 3 ).
However, there was no significant association between GDM risk and other variants (rs17099985, rs1742473, rs6798181 and rs796749) in the present study ( P > 0.05) (Table 2 ).
According to bioinformatic analysis, the rs9283638 polymorphism located at a TFBS can change the types of transcription factors binding to the promoter region under different alleles, which may affect gene transcription (Fig. 3 a and b). Furthermore, expression quantitative trait locus (eQTL) analysis of placental tissues revealed that rs9283638 C > T could significantly regulate the mRNA levels of SAMD7 ( P = 0.017). As shown in Fig. 4 a and b.

The prediction for the transcription factor binding site (TFBS) using AliBaba 2.1. ( a ) The transcription factors of rs9283638 C allele in 97–106 bp. ( b ) The transcription factors of rs9283638 T allele in 101–110 bp.

Schematic diagram of the genotyping of rs9283638 and the expression quantitative trait locus (eQTL) analysis of SAMD7 . ( a ) rs9283638 genotyping plot by Kompetitive Allele Specific Polymerase Chain Reaction (KASP-PCR). ( b ) Analysis of SAMD7 differential expression level under different genotypes. * P < 0.05.
Variable screening and nomogram establishment
Through the univariate and multivariate logistic regression analysis, 6 clinical factors were considered risk factors for GDM: age, FPG, 1hPG, 2hPG, HbA1c and TG. Considered the rs9283638 was associated with an increased GDM risk, the predictive nomogram model was eventually constructed with the positive SNP (rs9283638 recessive model) and significant clinical factors (Supplemental Table S3 ). The patients were randomly assigned to the training and validation cohorts at a 7:3 ratio; thus, there were 805 patients in the training set and 344 patients in the validation set. The GDM risk can be predicted based on the sum of assigned points for each risk factor’s level. Higher total scores indicate that GDM events are more likely to occur (Fig. 5 a). In addition, to facilitate the use of nomograms for clinicians, we constructed a dynamic nomogram online to visualize the predictive results for GDM. The probability of GDM occurrence can be easily determined by inputting personal values of risk indicators into the web-based application (Fig. 5 b–d).

The static and dynamic nomogram for predicting individual GDM risk. ( a ) A static nomogram for GDM risk prediction. Each risk indicators corresponding to level can be given different scores, and the total scores obtained by adding these scores from all variables can use to predict the GDM risk. ( b ) The risk variables input panel of the online dynamic nomogram ( https://qiulianl.shinyapps.io/GDM Predict/). ( c ) Person GDM predictive results’ graph visualization. ( d ) Showing individual GDM predictive probability and its corresponding 95% confidence intervals.
Validation of the nomogram
The predictive nomogram had an area under the curve (AUC) of 0.920 (95% CI 0.902–0.939, P < 0.001) in the training cohort and 0.834 (95% CI 0.778–0.890, P < 0.001) in the validation cohort, indicating the good discriminating ability of the model (Fig. 6 a and b). The nomogram calibration plot was roughly close to the ideal line, revealing good agreement between the predicted and observed values (Fig. 6 c and d). As shown in the DCA analysis, the model curves for most of the risk threshold probabilities were above the two lines (“treat all” or “treat none”), suggesting that the nomogram model had greater net clinical benefit (Fig. 6 e and f).

Validation of the nomogram. ( a ) Receiver operating characteristic (ROC) curves in training set with an area under the curve (AUC) of 0.920, cutoff value of 0.428, specificity of 80.6%, sensitivity of 89.9%. ( b ) ROC curve in validation set with a AUC of 0.834. ( c ) Calibration plot in training set conducted by a bootstrap method with 1000 resamples. ( d ) Calibration plot in validation set conducted by a bootstrap method with 1000 resamples. ( e ) A decision curve analysis (DCA) in training set. ( f ) DCA curve in validation set.
GDM is considered to pose a serious threat to the short-term and long-term health of mothers and their offspring 29 . Identifying high-risk populations for GDM is particularly useful for early intervention and prevention of disease progression 30 , 31 . Although significant progress has been made in identifying the mechanism of GDM susceptibility, they have not been fully understood. It is now recognized that GDM is a multifactorial disease and exhibits a clear genetic tendency. That is, genetic variants may alter individuals’ genetic susceptibility to GDM, even under the same environmental conditions 32 , 33 . Here, while clarifying the association between genomic SNPs and GDM, we further attempted to construct a nomogram predictive model to predict the risk of GDM in pregnant women. It is believed to be of great social significance for the prevention and control of GDM.
In the present study, we observed a significant association between rs9283638 and the risk of GDM in the population of Guilin, China. This finding is consistent with the findings of numerous previous studies 8 , 10 , 13 , 14 , 19 , 20 , 21 . Meaning, there are obvious genetic characteristics involved in the pathogenesis of GDM, and a series of associated genes and SNPs are involved in disease occurrence at the genetic level. Furthermore, these findings suggest that the studied SNPs exert different effects on different levels of some clinical indicators, and significant interactions have been observed between rs9283638 and age. Similarly, Kwak SH et al. reported that the CDKAL1 SNP rs7754840 was significantly associated with insulin expression, inhibition of insulin secretion in pancreatic β-cells and birth weight of a baby 20 , while Polina V et al. suggested that genetic variants of MTNR1B (rs10830963 and rs1387153) can reduce early insulin secretion through parallel signalling pathways in pancreatic β-cells, thereby regulating glucose metabolism 34 . These findings indicated that genetic variants may modify the genetic background of an individual or, combine with environmental features or clinical traits, may affect individuals’ susceptibility to complex human diseases. Personal differences associated with GDM may be affected by SNPs or SNP-environmental factor interactions.
It is speculated that the construction of a predictive model can serve as an important bridge between clinical epidemiology or molecular epidemiology and clinical practice, and it could become an effective means of identifying high-risk populations, guiding clinical diagnosis and treatment, promoting the prevention and control of complex diseases, and improving patient clinical prognosis 35 , 36 . The nomogram prediction model integrates multiple disease-related indicators and draws scaled line segments on the same plane in a certain proportion to express the relationships between selected variables. The model quantifies the occurrence rate and high-risk factors for GDM risk, intuitively representing the probability of patients developing GDM, and provides personalized risk assessment for subjects 26 , 37 , 38 .
Given the independent hazard effect of environmental and genetic factors on the pathogenesis of GDM, this study incorporated validated SNPs significantly associated with GDM and clinical indicators (age, FPG, 1hPG, 2hPG, HbA1c and TG) to construct a GDM risk prediction nomogram model. This model demonstrated a good ability to distinguish individual GDM risks, with an area under the ROC curve of 0.920. The genetic-clinical model can help clarify the probability of women developing GDM during pregnancy, thereby identifying high-risk individuals and leading to personalized prevention. It is extremely important to accurately prevent GDM in individuals during early pregnancy.
The potential gene expression regulatory region variants not only serve as genetic markers but also may affect individual physiological and pathological manifestations by regulating the expression of genes or interacting with environmental exposure factors, making them suitable for revealing the susceptibility mechanisms of complex traits and diseases. For example, the functional variant rs10830963 was associated with GDM risk by regulating the expression levels of the MTNR1B gene, fasting blood glucose, fasting insulin, and homeostasis model assessment for insulin resistance 39 . In the present study, we found that rs9283638 is significantly associated with the risk of GDM and has significant interactions with age. Furthermore, we found that the above association findings seem to be biologically plausible. Functional analysis suggested that rs9283638 C > T can affect transcription factor binding to specific binding motifs and alter the transcription of the SAMD7 gene. In addition, mRNA level detection in placental tissues revealed that rs9283638 can be an eQTL that regulates the expression levels of SAMD7 mRNA. This finding provides new insight into the biological genetic mechanism of susceptibility to GDM.
However, this study has several limitations. First, as a hospital-based case‒control study, there will inevitably be bias in subject selection and data collection. Second, potential confounding factors of GDM, such as smoking status, poor obstetrics, malnutrition, and socioeconomic factors, were not assessed. These factors are likely to interfere with the true effects of the association between the studied variants and GDM risk. Third, the very low frequency of genotypes tested in the studied variants may still limit the statistical performance, especially in subgroup analysis. Finally, limited in-depth biological functional analysis of significantly associated variants was conducted in this study.
In the present study, we confirmed that rs9283638 is significantly related to the risk of GDM. The potential mechanism may involve independent genetic risk effects and genetic-environmental interactions affecting female individuals′ susceptibility to GDM. Based on key genetic SNPs and clinical parameters, a predictive nomogram model with good potential for the early identification and prevention of GDM has been successfully established.
Data availability
The datasets generated and/or analysed during the current study are available in the dryad repository, doi: https://doi.org/ https://doi.org/10.5061/dryad.fj6q5743m .
Goedegebure, E. A. R. et al. Pregnancy outcomes in women with gestational diabetes mellitus diagnosed according to the WHO-2013 and WHO-1999 diagnostic criteria: A multicentre retrospective cohort study. BMC Pregnancy Childbirth 18 , 152 (2018).
Article PubMed PubMed Central Google Scholar
Gao, C., Sun, X., Lu, L., Liu, F. & Yuan, J. Prevalence of gestational diabetes mellitus in mainland China: A systematic review and meta-analysis. J. Diabetes Investig. 10 , 154–162 (2019).
Article CAS PubMed Google Scholar
Coustan, D. R. Pregnancy outcomes in women with and without gestational diabetes mellitus according to the international association of the diabetes and pregnancy study groups criteria. Obstet. Gynecol. 121 , 377 (2013).
Article PubMed Google Scholar
Farrar, D. et al. Hyperglycaemia and risk of adverse perinatal outcomes: Systematic review and meta-analysis. BMJ 354 , i4694 (2016).
Li, M. et al. Genetic factors and risk of type 2 diabetes among women with a history of gestational diabetes: Findings from two independent populations. BMJ Open Diabetes Res. Care 8 , e000850 (2020).
Xiang, A. H. Diabetes in pregnancy for mothers and offspring: reflection on 30 years of clinical and translational research: The 2022 Norbert Freinkel award lecture. Diabetes Care 46 , 482–489 (2023).
Zeng, J. et al. Association of maternal obesity and gestational diabetes mellitus with overweight/obesity and fatty liver risk in offspring. World J. Gastroenterol. 28 , 1681–1691 (2022).
Article CAS PubMed PubMed Central Google Scholar
Plows, J. F., Stanley, J. L., Baker, P. N., Reynolds, C. M. & Vickers, M. H. The pathophysiology of gestational diabetes mellitus. Int. J. Mol. Sci. 19 , 3342 (2018).
You, H., Hu, J., Liu, Y., Luo, B. & Lei, A. Risk of type 2 diabetes mellitus after gestational diabetes mellitus: A systematic review & meta-analysis. Indian J. Med. Res. 154 , 62–77 (2021).
Chen, P. et al. Risk factors and management of gestational diabetes. Cell Biochem. Biophys. 71 , 689–694 (2015).
Zhou, Y., Xie, N., Zhang, L. & Chen, D. Impact of family history of diabetes on blood glucose, lipid levels and perinatal outcomes in pregnant women with gestational diabetes mellitus. Zhejiang Da Xue Xue Bao Yi Xue Ban 50 , 329–334 (2021).
PubMed PubMed Central Google Scholar
Monod, C. et al. Prevalence of gestational diabetes mellitus in women with a family history of type 2 diabetes in first- and second-degree relatives. Acta Diabetol. 60 , 345–351 (2023).
Benny, P. et al. Genetic risk factors associated with gestational diabetes in a multi-ethnic population. PLoS One 16 , e0261137 (2021).
Wei, W. et al. Gestational diabetes mellitus: The genetic susceptibility behind the disease. Horm. Metab. Res. 53 , 489–498 (2021).
Acosta-España, J. D. & Voigt, K. Mini review: Risk assessment, clinical manifestation, prediction, and prognosis of mucormycosis: Implications for pathogen- and human-derived biomarkers. Front. Microbiol. 13 , 895989 (2022).
Li, G. Expression quantitative trait loci analysis in multiple tissues. Methods Mol. Biol. 2082 , 231–237 (2020).
McRae, A. F. et al. Identification of 55,000 replicated DNA methylation QTL. Sci. Rep. 8 , 17605 (2018).
Article ADS PubMed PubMed Central Google Scholar
Prasad, R. B., Kristensen, K., Katsarou, A. & Shaat, N. Association of single nucleotide polymorphisms with insulin secretion, insulin sensitivity, and diabetes in women with a history of gestational diabetes mellitus. BMC Med. Genom. 14 , 274 (2021).
Article CAS Google Scholar
Dalfrà, M. G., Burlina, S., Del Vescovo, G. G. & Lapolla, A. Genetics and epigenetics: New insight on gestational diabetes mellitus. Front. Endocrinol. (Lausanne) 11 , 602477 (2020).
Kwak, S. H. et al. A genome-wide association study of gestational diabetes mellitus in Korean women. Diabetes 61 , 531–541 (2012).
Wu, N. N. et al. A genome-wide association study of gestational diabetes mellitus in Chinese women. J. Matern. Fetal Neonatal Med. 34 , 1557–1564 (2021).
Article ADS CAS PubMed Google Scholar
Sammani, A., Baas, A. F., Asselbergs, F. W. & Te Riele, A. Diagnosis and risk prediction of dilated cardiomyopathy in the era of big data and genomics. J. Clin. Med. 10 , 921 (2021).
Tong, J. N. et al. Fasting plasma glucose in the first trimester is related to gestational diabetes mellitus and adverse pregnancy outcomes. Endocrine 75 , 70–81 (2022).
Zhang, D. et al. A clinical model and nomogram for early prediction of gestational diabetes based on common maternal demographics and routine clinical parameters. J. Obstet. Gynaecol. Res. 48 , 2738–2747 (2022).
Zhang, X. et al. Risk prediction model of gestational diabetes mellitus based on nomogram in a Chinese population cohort study. Sci. Rep. 10 , 21223 (2020).
Article ADS CAS PubMed PubMed Central Google Scholar
Li, S., Li, H., Li, C., He, X. & Wang, Y. Development and validation of a nomogram for predicting the risk of pregnancy-induced hypertension: A retrospective cohort study. J. Womens Health (Larchmt) 30 , 1182–1191 (2021).
He, C., Holme, J. & Anthony, J. SNP genotyping: The KASP assay. Methods Mol. Biol. 1145 , 75–86 (2014).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25 , 402–408 (2001).
Moon, J. H. & Jang, H. C. Gestational diabetes mellitus: Diagnostic approaches and maternal-offspring complications. Diabetes Metab. J. 46 , 3–14 (2022).
Clarke, E., Cade, T. J. & Brennecke, S. Early pregnancy screening for women at high-risk of GDM results in reduced neonatal morbidity and similar maternal outcomes to routine screening. J. Pregnancy 2020 , 9083264 (2020).
Zhang, C., Rawal, S. & Chong, Y. S. Risk factors for gestational diabetes: Is prevention possible?. Diabetologia 59 , 1385–1390 (2016).
Wu, Q. et al. An early prediction model for gestational diabetes mellitus based on genetic variants and clinical characteristics in China. Diabetol. Metab. Syndr. 14 , 15 (2022).
Xie, K. et al. Genetic predisposition to gestational glucose metabolism and gestational diabetes mellitus risk in a Chinese population. J. Diabetes 11 , 869–877 (2019).
Popova, P. V. et al. Association of common genetic risk variants with gestational diabetes mellitus and their role in GDM prediction. Front. Endocrinol. (Lausanne) 12 , 628582 (2021).
Niu, Z. R., Bai, L. W. & Lu, Q. Establishment of gestational diabetes risk prediction model and clinical verification. J. Endocrinol. Investig. 47 , 1281–1287 (2023).
Article Google Scholar
Lin, Q. & Fang, Z. J. Establishment and evaluation of a risk prediction model for gestational diabetes mellitus. World J. Diabetes 14 , 1541–1550 (2023).
Li, W. et al. Predictive nomogram of RAGE Genetic polymorphisms and metabolic risk factors for myocardial infarction risk in a Han Chinese population. Angiology 68 , 877–883 (2017).
Tang, G. et al. Evaluation and analysis of incidence and risk factors of lower extremity venous thrombosis after urologic surgeries: A prospective two-center cohort study using LASSO-logistic regression. Int. J. Surg. 89 , 105948 (2021).
Konig, M. & Shuldiner, A. R. The genetic interface between gestational diabetes and type 2 diabetes. J. Matern. Fetal Neonatal Med. 25 , 36–40 (2012).
Download references
This study was supported by: Guangxi Science and Technology Base and Talent Special Project (AD24010027); self-funded research project of The Health Committee of Guangxi (Z-C20241580); the Guangxi Natural Science Foundation of China (2020GXNSFAA238025); Guangxi Young and middle-aged teachers' basic ability improvement project (2020KY12028); Maternal and Child Health Research Project of Guangxi Bagui Scholars (Jun Zhang).
Author information
These authors contributed equally: Gongchen Huang and Yan Sun.
Authors and Affiliations
The Guangxi Key Laboratory of Environmental Exposomics and Entire Lifecycle Health, The School of Public Health, Guilin Medical University, Guilin, 541000, China
Gongchen Huang, Yan Sun, Ruiqi Li, Qiulian Liang & Xiangyuan Yu
Department of Obstetrics and Gynecology, The Second Affiliated Hospital of Guilin Medical University, Guilin, 541000, China
You can also search for this author in PubMed Google Scholar

Contributions
Conceptualization: X.Y.Y., Q.L.L.; Data curation: L.M.; Formal analysis: Q.L.L., Y.S.; Investigation:Y.S., R.Q.L.; Methodology: X.Y.Y., Q.L.L.; Software: G.C.H., Q.L.L.; Visualization: G.C.H.; Writing-original draft: G.C.H., Y.S., Q.L.L.; Writing-review & editing: X.Y.Y., R.Q.L. All authors reviewed the article and approved the submitted version.
Corresponding authors
Correspondence to Qiulian Liang or Xiangyuan Yu .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Huang, G., Sun, Y., Li, R. et al. Functional genetic variants and susceptibility and prediction of gestational diabetes mellitus. Sci Rep 14 , 18123 (2024). https://doi.org/10.1038/s41598-024-69079-y
Download citation
Received : 30 April 2024
Accepted : 31 July 2024
Published : 05 August 2024
DOI : https://doi.org/10.1038/s41598-024-69079-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gestational diabetes mellitus
- Genetic susceptibility
- Nomogram model
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
Improved Diabetes Screening for Women After Gestational Diabetes Mellitus
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Cite Icon Cite
- Get Permissions
Brittany Strelow , Justine Herndon , AnneMarie McMahon , Mark Takagi , Rozalina McCoy , Rachel Olson , Danielle O’Laughlin; Improved Diabetes Screening for Women After Gestational Diabetes Mellitus. Diabetes Spectr 2024; ds240005. https://doi.org/10.2337/ds24-0005
Download citation file:
- Ris (Zotero)
- Reference Manager
This study aimed to assess the need for practice-wide quality improvement to support evidence-based type 2 diabetes screening for women with a history of gestational diabetes mellitus (GDM) receiving primary care. We sought to add the diagnosis of GDM to the problem list of women who did not have it at baseline.
We identified all women in our practice with a history of GDM diagnosed between 2002 and 2023, quantified the proportion with GDM documented in their problem list, and examined patient- and clinician-level factors associated with having GDM appropriately documented at baseline.
We identified 203 women with GDM receiving primary care within internal medicine. Of the 203 women, 73 (35.0%) did not have GDM documented in their problem list. Of those without GDM included on the problem list, 52% were overdue for type 2 diabetes screening compared with 41% of those with GDM documented before our intervention. We found race, parity, and previous abnormal glycemic laboratory test results to be highly predictive of whether the history of GDM was on patients’ problem list. Upon completion of our intervention, we successfully achieved a 100% documentation rate for GDM diagnosis for women who previously lacked documentation in their problem list.
This work paves the way for targeted interventions aimed at improving care for women with a history of GDM, including delivery of interventions and education to prevent the onset of an appropriate clinical screening for type 2 diabetes.
Sign in via ADA
Sign in via your institution, email alerts.
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Advanced search
- Peer review
Call for Papers: Preclinical Investigations of Nutrigenetic/Nutrigenomic Targets
Submit here before january 31, 2025.
About Lifestyle Genomics : 2.0 Impact Factor I 4.0 CiteScore I 0.539 Scimago Journal & Country Rank (SJR)
- Record : found
- Abstract : found
- Article : found
Gestational Diabetes Mellitus and Macrosomia: A Literature Review
Read this article at.
- open (via free pdf)

- Review article
- Invite someone to review
Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation. As a result, extra glucose in the fetus is stored as body fat causing macrosomia, which is also called ‘large for gestational age'. This paper reviews studies that explored the impact of GDM and fetal macrosomia as well as macrosomia-related complications on birth outcomes and offers an evaluation of maternal and fetal health. Summary: Fetal macrosomia is a common adverse infant outcome of GDM if unrecognized and untreated in time. For the infant, macrosomia increases the risk of shoulder dystocia, clavicle fractures and brachial plexus injury and increases the rate of admissions to the neonatal intensive care unit. For the mother, the risks associated with macrosomia are cesarean delivery, postpartum hemorrhage and vaginal lacerations. Infants of women with GDM are at an increased risk of becoming overweight or obese at a young age (during adolescence) and are more likely to develop type II diabetes later in life. Besides, the findings of several studies that epigenetic alterations of different genes of the fetus of a GDM mother in utero could result in the transgenerational transmission of GDM and type II diabetes are of concern.
Related collections
Karger: Nutrition and Dietetics
Most cited references 33
- Abstract : not found
- Article : not found
Developmental origins of health and disease.
The influence of obesity and diabetes on the prevalence of macrosomia.
Obesity, insulin resistance, and pregnancy outcome., author and article information , affiliations, author notes.
Copyright: All rights reserved. No part of this publication may be translated into other languages, reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, microcopying, or by any information storage and retrieval system, without permission in writing from the publisher. Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new and/or infrequently employed drug. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor(s). The appearance of advertisements or/and product references in the publication is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety. The publisher and the editor(s) disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements.
Comment on this article
Similar content 836 .
- Fetal macrosomia and pregnancy outcomes. Authors: Tim Donovan , Hong Ju , Y Chadha …
- Prenatal detection and consequences of fetal macrosomia. Authors: Christian Bamberg , Larry Hinkson , Wolfgang Henrich
- Growth factor concentrations and their placental mRNA expression are modulated in gestational diabetes mellitus: possible interactions with macrosomia Authors: Oussama Grissa , Akadiri Yessoufou , Inès Mrisak …
Cited by 276
- Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: A systematic review and meta-analysis Authors: Jane Tarry-Adkins , Catherine Aiken , Susan E. Ozanne
- Gut Microbiota and Gestational Diabetes Mellitus: A Review of Host-Gut Microbiota Interactions and Their Therapeutic Potential Authors: Zubaidah Bt Hasain , Norfilza Mokhtar , Nor Kamaruddin …
- Gestational Diabetes Mellitus: A Harbinger of the Vicious Cycle of Diabetes Authors: Emilyn Alejandro , Therriz Mamerto , Grace Chung …
Most referenced authors 391
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- AME Case Rep
- PMC11292075

Progression of gestational diabetes mellitus to pregnancy-associated fulminant type 1 diabetes: a case report
1 Department of Endocrinology, Hainan Hospital Affiliated Hospital of Hainan Medical University/Hainan General Hospital, Haikou, China;
Kaining Chen
Huibiao quan.
2 Department of Obstetrics, Hainan Hospital Affiliated Hospital of Hainan Medical University/Hainan General Hospital, Haikou, China
Associated Data
The article’s supplementary files as
Pregnancy-associated fulminant type 1 diabetes (PF) occurs during pregnancy or within 2 weeks of delivery. Although it occurs infrequently, it is associated with high fetal mortality rate. Few studies have examined whether PF is associated with gestational diabetes mellitus (GDM).
Case Description
A 29-year-old woman diagnosed with GDM at 24 weeks of gestation developed a fever, sore throat, nausea and vomiting at 29 weeks of gestation. Ketoacidosis was considered based on her blood ketone and glucose levels and the results of a blood gas analysis. Since the patient’s islet function declined rapidly, fluid replacement, insulin therapy, and other treatments were administered. The patient was ultimately diagnosed with PF, and has required ongoing insulin therapy. She delivered a healthy baby girl by elective cesarean section at 37-week gestation. Her blood glucose has been satisfactorily controlled over the 12 months since her acute presentation.
Conclusions
PF is characterized by poor maternal and infant outcomes and a high stillbirth rate. Blood glucose should be regularly monitored in pregnant women with GDM. A sudden increase in blood glucose may indicate the possibility of PF, which needs to be managed in a timely manner to avoid adverse pregnancy outcomes.
Highlight box
Key findings.
• Gestational diabetes mellitus (GDM) and gestational pregnancy-associated fulminant type 1 diabetes (PF) have different pathogenesis, and only a few patients have GDM before PF.
What is known and what is new?
• Fulminant type 1 diabetes mellitus (FT1DM) that occurs during pregnancy or the perinatal period is known as PF.
• PF is always without history of abnormal glucose metabolism. Here, we present a patient who developed PF during treatment but were first diagnosed with GDM.
What is the implication, and what should change now?
• Body mass index was not a predictor of PF; patients with GDM need to monitor their blood sugar regularly during pregnancy, and a sudden rise in blood sugar may alert them to turn into PF, which requires high attention and timely medical treatment to avoid adverse pregnancy outcomes.
Introduction
Pregnancy-associated fulminant type 1 diabetes (PF) occurs during pregnancy or within 2 weeks of delivery, has a low incidence, and is characterized by a rapid decline in islet cell function and the onset of ketoacidosis ( 1 ). It is a highly dangerous condition associated with a high incidence of stillbirth. The cause of PF is not yet clear. Gestational diabetes mellitus (GDM) occurs during pregnancy and is harmful to both the mother and fetus ( 2 ). Unfortunately, few studies have examined the possible correlation between GDM and PF.
The current patient was diagnosed with GDM in her second trimester, but subsequently represented with PF. The fetus survived after active treatment. This report summarizes the clinical features of this patient along with review of the relevant literature with the aim to extend understanding about PF and to prevent its misdiagnosis and mistreatment. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-52/rc ).
Case presentation
All the procedures performed in this study were conducted in accordance with the ethical standards of Hainan General Hospital and the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Chief complaints
A 29-year-old female in her 29 th gestational week was admitted to hospital on January 23, 2021. Over the 3 days prior, she had experienced fever, fatigue, mild sore throat, and cough without any obvious trigger. She also reported one day of nausea and vomiting and stated that fetal movements appeared to have decreased over the preceding 12 hours ( Table 1 ).
| Parameters | Value |
|---|---|
| Age (years) | 29 |
| Gravida | 1 |
| Family history of diabetes | Denied |
| History of drug allergies | Denied |
| Maternal pre-pregnancy BMI (kg/m ) | 22.3 |
BMI, body mass index.
Five weeks earlier, she had been diagnosed with GDM after an oral glucose tolerance test (OGTT), which revealed a 1-hour postprandial glucose of 10.6 mmol/L ( Table 2 ) [diagnostic criteria for GDM developed by the International Association of Diabetes and Pregnancy Study Group (IADPSG) in 2010: GDM is diagnosed by meeting or exceeding at least one of the following indicators: fasting plasma glucose (FPG) ≥5.1 mmol/L, glucose level at 1-hour postprandial glucose (1 h PG) ≥10.0 mmol/L and (or) at 2 hours postprandial glucose after OGTT (2 h PG) ≥8.5 mmol/L]. Subsequent to this, her blood glucose had been satisfactorily controlled with diet and exercise alone.
| Time to diagnosis of GDM | OGTT results in the second trimester (mmol/L) | Fasting insulin levels in the second trimester (4–23 pmol/L) | HbA1c in the second trimester (4–6%) | Insulin use | |||
|---|---|---|---|---|---|---|---|
| 0 h (<5.1 mmol/L) | 1 h (<10 mmol/L) | 2 h (<8.5 mmol/L) | |||||
| At the 24 gestational week | 4.8 | 10.6 | 8.0 | 66.5 | 5.1% | Not used | |
Data in parentheses are ranges of normal values. PF, pregnancy-associated fulminant type 1 diabetes; GDM, gestational diabetes mellitus; OGTT, oral glucose tolerance test; HbA1c, glycated hemoglobin.
The initial laboratory test results (normal range) showed capillary blood glucose: 19 mmol/L (FPG 3.9–6.1 mmol/L); urine ketone bodies: 4+ (negative); pH: 7.1 (7.35–7.45); base excess (BE): −22 (−3 to 3); and urine amylase: 735.5 U/L (4–32 U/dL). A diagnosis of diabetic ketoacidosis (DKA) was considered. She received fluid replacement and glucose-lowering treatment [0.9% sodium chloride infusion (500 mL) + 10% potassium chloride (15 mL) + one-off human insulin (6–8 IU)], intravenous (IV) drip in the obstetrics department and was then transferred to the Endocrinology ward for ongoing care.
History of illness
The patient had a previous history of α-thalassemia [Southeast Asian (SEA) deletion] and denied a family history of diabetes. She previously had regular menstrual cycles, and the first day of her last menstrual period was June 30, 2020. Her childbearing history was G 1 P 0 ( Table 1 ).
Physical examination
General observations demonstrated body temperature: 36.7 ℃; heart rate: 103 beats per minute; respiratory rate: 20 breathes per minute; and blood pressure: 122/72 mmHg. Maternal pre-pregnancy body mass index (BMI) was 22.3 kg/m 2 . She was alert and cooperative during the physical examination. She had normal vesicular breath sounds bilaterally with no added sounds on auscultation. Her heart rhythm was regular, with normal findings on examination of the praecordium. Longitudinal oval bulges were observed on abdominal inspection. Visible peristaltic waves were not present. There was no peripheral edema. Her upper and lower limb muscle strength and muscle tone were normal.
Gynecological examination showed uterine height: 25 cm; abdominal circumference: 85 cm; cephalic presentation; left occiput anterior position; head not engaged; palpable irregular uterine contractions; and fetal heart sounds: regular (136 beats/minute). A colposcopy showed that the cervix was not dilated.
Laboratory examinations
The ancillary test results (normal range) of the patient were as follows—white blood cell count: 14×10 9 /L (3.5–9.5 ×10 9 /L); neutrophils (percentage): 80.9% (40–75%); serum glucose: 22.5 mmol/L (≤7.8 mmol/L); D3-hydroxybutyric acid: 8.1 mmol/L (0.03–0.3 mmol/L); lactic acid: 0.97 mmol/L (0.6–2.2 mmol/L); pH: 7.1 (7.35–7.45); and BE: 22 (−3 to 3). The routine urine tests showed urine glucose: 4+ (negative); and urine ketone bodies: 4+ (negative). There were no obvious abnormalities on routine stool tests. The test results for influenza A and B antibodies were negative, as was a nucleic acid test for severe acute respiratory syndrome coronavirus.
The biochemical results (normal range) of the patient were as follows—blood sodium: 131 mmol/L (137–147 mmol/L); and normal liver/kidney function. The pancreatic enzyme results (normal range) of the patient were as follows—blood amylase: 346 U/L (35–135 U/L); pancreatic amylase: 331 U/L (30–220 U/L); lipase: 320 U/L (150–200 U/L); islet function: C-peptide (0') [CP (0')], 0.017 nmol/L (0.37–1.47 nmol/L); and C-peptide (120') [CP (120')], 0.09 nmol/L (0.37–1.47 nmol/L). The glycated hemoglobin (HbA1c%) was 6.1% (4–6%), and the islet cell antibodies, antibodies to glutamate decarboxylase, and insulin autoantibodies were negative ( Table 3 ).
| Parameters (range and unit of normal value) | Value at the 29 gestational week |
|---|---|
| Interval between GDM and PF (weeks) | 5 |
| Clinical symptom | Fever, fatigue, sore throat, cough, and vomiting |
| Routine blood test (WBC, 3.5–9.5 ×10 /L; NE%, 40–75%) | WBC, 14×10 /L; NE%, 80.9% |
| Blood glucose (≤7.8 mmol/L) | 22.5 |
| Serum D3-hydroxybutyric acid (0.03–0.3 mmol/L) | 8.1 |
| pH value (7.35–7.45) | 7.1 |
| FCP (0.37–1.47 nmol/L) | 0.017 |
| PCP (0.37–1.47 nmol/L) | 0.09 |
| HbA1c (4–6%) | 6.1% |
| Islet antibodies | Negative |
| PG/HbA1c (<3.3) | 3.68 |
| SCr (57–97 μmol/L) | 41 |
| CK (50–310 U/L) | 65 |
| Lactic acid (0.6–2.2 mmol/L) | 0.97 |
| Serum amylase level (35–135 U/L) | 346 |
| Pancreatic amylase level (30–220 U/L) | 331 |
| Serum lipase level (150–200 U/L) | 320 |
| Abdomen ultrasound or CT | No signs of pancreatitis |
| Fetal outcomes | Survived |
| Delivery mode | Cesarean section |
| Long-term treatment options | Insulin pump |
PF, pregnancy-associated fulminant type 1 diabetes; GDM, gestational diabetes mellitus; WBC, white blood cell count; NE%, neutrophils (percentage); FCP, fasting C-peptide; PCP, 2-hour postprandial C-peptide; PG, plasma glucose; HbA1c, glycated hemoglobin; SCr, serum creatinine; CK, creatine kinase; CT, computed tomography.
Imaging examinations
Computed tomography (CT) of the upper abdomen revealed possible cholestasis of the gallbladder, but no obvious abnormalities were observed in the liver, pancreas, or spleen. Abdominal color ultrasound revealed thickened and unevenly distributed echoes in the liver parenchyma, but no sign of pancreatitis was observed. An electrocardiogram showed sinus tachycardia.
Final diagnoses
The patient’s diagnoses were as follows: (I) PF; (II) DKA; (III) GDM.
DKA treatment was started immediately after the identification of DKA, and included active fluid replacement [0.9% sodium chloride infusion (500 mL) + 10% potassium chloride (15 mL) + one-off human insulin (6–8 IU)], alternating with 5% glucose + 0.9% sodium chloride infusion (500 mL) + 10% potassium chloride (15 mL) + one-off human insulin (8–12 IU), IV insulin pump [human insulin (50 IU) + 0.9% sodium chloride (50 mL), infused at a rate of 2–5 mL/h], once every hour blood glucose monitoring, electrocardiogram monitoring, and fetal heart rate monitoring.
After DKA was corrected, a subcutaneous insulin pump was used (Medtronic, MMT-712EWS, Minneapolis, USA) with a total baseline dose of insulin aspart injection 26 IU/d (0:00–3:00 0.8 IU/h, 03:00–7:00 1.4 IU/h, 07:00–12:00 1.1 IU/h, 12:00–17:00 1.0 IU/h, 17:00–22:00 1.1 IU/d, 22:00–24:00 0.9 IU/h) and bolus dose before meals of 10–14 IU to maintain a stable blood glucose fluctuation range as follows: fasting: 4.5–5.7 mmol/L; 2-hour postprandial: 6–9 mmol/L.
In addition, a multidisciplinary team of experts from the nutrition, obstetrics, and psychology departments was established. Nutritious meals were provided after the correction of ketoacidosis, The nutritious meals were: 1,800 kcal of total calories, 250 g of carbohydrates, 80 g of proteins, 53 g of fats, and the proportion of breakfast, lunch and dinner is 1/5, 2/5, and 2/5, respectively. And the fetal condition was assessed by the obstetricians. The mother was diagnosed with mild depression by the psychology department, and psychological counseling was offered.
Outcome and follow-up
After active treatment, the patient’s mental status improved remarkably. Her nausea and vomiting resolved, and her appetite improved. Her blood glucose after DKA correction was well controlled (fasting: 4.5–5.7 mmol/L; 2-hour postprandial: 6–9 mmol/L). Fetal heart rate monitoring revealed no obvious abnormality.
Two months subsequent to her presentation with DKA (at 37 weeks of gestation), the mother delivered a healthy baby girl by elective cesarean section. Over the subsequent 12 months, she maintained stable glucose control using an insulin pump (fasting blood glucose 4.5–7 mmol/L; 2-hour postprandial glucose 6–11 mmol/L). Her most recent HbA1c was recorded to be 7.6%. She has not had recurrence of episodes of DKA.
Fulminant type 1 diabetes mellitus (FT1DM) is a new subtype of type 1 diabetes mellitus (T1DM) that was first proposed by Imagawa and colleagues in 2000 ( 3 ). FT1DM diagnosis was proposed by the Japan Diabetes Association in 2016 Standard ( 4 ). It is more common in Asian populations, and is especially common in Japan, South Korea, and China. FP is defined as FT1DM that occurs during pregnancy or within 2 weeks of delivery. FP is the most common type of FT1DM ( 5 ) and typically occurs in the third trimester. However, few studies have examined the possible correlation between GDM and PF.
The current report summarizes the clinical features of a woman diagnosed with PF. She had been diagnosed with GDM in the second trimester, and then experienced an acute onset of hyperglycemia and ketoacidosis in the third trimester. Her blood glucose was ≥16.0 mmol/L, but her HbA1c was not high (<8.7%). Her fasting and postprandial serum C-peptide levels were almost undetectable. There were no abnormal findings on the pancreatic ultrasound or CT (to determine the presence of pancreatitis, CT was performed with the patient’s informed consent). These findings represented the typical clinical and laboratory features for PF and she met the diagnostic criteria for PF.
Both the 2021 American Diabetes Association standards ( 6 ) and the 2019 World Health Organization guidelines ( 7 ) mention hyperglycemia during pregnancy. These descriptions include GDM, overt diabetes diagnosed in pregnancy, and pre-conceptional diabetes, but do not include PF. This suggests that the pathogenesis and clinical features of PF are completely different from any other type of hyperglycemia during pregnancy.
Both GDM and overt diabetes diagnosed in pregnancy occur due to the increased insulin resistance caused by insulin-antagonizing hormones secreted by adipocytes and placental tissues after pregnancy, the low-level inflammatory responses, and the reduced sensitivity to insulin of pregnant women ( 8 ). They can be regarded as compensatory and decompensated manifestations that help maintain the normal physiological glucose metabolism ( 8 ). After the delivery of the fetus and placenta, insulin resistance is alleviated and blood sugar improves or even returns to normal; thus, insulin can be used in much lower dosages or stopped. However, for person with PF, postpartum blood glucose is difficult to control due to the complete loss of islet function, and lifelong insulin use is consequently required.
The common etiologies of PF include viral infections, human leukocyte antigen ( HLA ) gene susceptibility and autoimmunity. Various viral infections have been described: these include coxsackievirus ( 9 ), herpes virus, and influenza virus. These viruses can directly and rapidly destroy β cells and also initiate autoimmunity by exposing the antigens. In one Chinese report, however, few patients were shown to have a viral trigger ( 10 ). Consistent with that observation, although the current case initially had a fever and symptoms of an upper respiratory tract infection, viral testing was negative.
The presence of specific HLA class II genes, notably HLA DR and DQ genes is closely related to the occurrence of PF ( 11 ). Next, with the patient’s informed consent, we intend to improve the testing of the woman’s related genes.
Autoimmunity also plays a key role in the pathogenesis of PF ( 12 ). While most individuals with PF have negative antibodies, a small proportion may have islet autoantibodies. Given the low rate of seropositivity, this is not regarded as a diagnostic criterion for PF. However, the autoantibodies in the current case were negative, which is consistent with most individuals with PF.
The pancreatic histopathology of patients with FT1DM is characterized by the rapid destruction of both α and β cells, which differs from classic T1DM, in which only β cells are destroyed at a relatively low rate of destruction. In addition, the elevated pancreatic enzymes in the current patient were consistent with the reported elevated exocrine pancreatic indicators in patients with PF ( 10 ). There were, however, no signs of pancreatitis on imaging. This combination of results might be explained by lymphocyte infiltration of the exocrine pancreas without pancreatic edema ( 6 ).
The clinical manifestations and metabolic disorders of patients with PF are more severe than those of patients with FT1DM who are not pregnant. Clinically, it is manifested as a rapid onset (typically within 1 week). PF also has the following clinical features: (I) influenza-like symptoms or gastrointestinal symptoms before onset; (II) a high blood glucose level and a nearly normal HbA1c level; (III) elevated exocrine enzymes of the pancreas; (IV) no signs of pancreatitis on imaging; and (V) an onset during pregnancy or within 2 weeks of delivery. In addition, unlike pre-GDM complicated by gestational DKA, PF has a much higher fetal mortality rate. In one report, stillbirth occurred in eight (89%) of nine cases of PF ( 13 ). In contrast, the fetal mortality rate of pre-pregnancy T1DM complicated by DKA is only about 9–36% ( 14 ).
Emaciation is a common characteristic of patients with classic T1DM and non-pregnancy-associated FT1DM. Conversely, the body weight of patients with PF is typically quite different from that of patients with non-pregnancy-associated FT1DM. Based on the body weight of several other patients with PF admitted to our department and the cases described by Peking Union Medical College Hospital, we noted that PF is more likely to occur in those who are overweight or obese (personal unpublished observation). In one of our previous studies ( 15 ), the preconception BMI of patients with PF did not differ from that of those with GDM. However, due to the small sample sizes, the reliability of these conclusions needs further verification.
According to the literature, most pregnant women deny a history of GDM before the occurrence of PF ( 11 ). In contrast, our patient had GDM during pregnancy. Thus, the question arises as to whether GDM is directly associated with the development of PF. It has been reported that patients with GDM are at risk of developing T1DM diabetes and a variety of autoimmune diseases ( 16 ). Islet autoimmunity may be involved in the development of PF, but the specific mechanism needs to be further studied.
In the current case, blood glucose fluctuations were revealed by close monitoring, which was important in identifying the cut-off time point at which GDM turned into PF. If blood glucose suddenly becomes difficult to control and deteriorates rapidly in a woman with GDM whose lifestyle interventions and insulin doses remain unchanged, the risk of PF should be considered. In the current case, the patient received regular blood glucose monitoring after the diagnosis of GDM. Before PF occurred, her blood glucose was basically well controlled. However, she later suffered from a sudden blood sugar increase and sought medical treatment promptly. Her fetus ultimately survived.
Early detection is especially important for PF. GDM turned into PF in the current case, which indicates that blood glucose should be monitored regularly in women with GDM until after delivery. According to Liu et al. ( 17 ), a PG/HbA1c ratio with a threshold of ≥3.3 can be used as a cut-off point in predicting PF from DKA in China. An elevated PG/HbA1c ratio at the time of diagnosis is predictive of more severe insulin secretion dysfunction and a poor prognosis. In our case, a sudden increase of blood glucose for unknown reasons and a PG/HbA1c ratio of ≥3.3 are highly suggestive of the possibility of PF, and further tests for blood glucose, HbA1c, D3-hydroxybutyric acid, C peptide, and islet antibodies should be performed.
Treatment for DKA should be commenced as early as possible, even before the diagnosis of PF is confirmed. DKA therapies include aggressive fluid replacement, the early insulin administration (via an insulin pump), the maintenance of the water-electrolyte balance, infection control, and fetal heart rate monitoring. In addition, due to the high basal cardiopulmonary stress in pregnant women, special attention should be paid to rehydration rate. After the DKA is corrected, an insulin pump or an intensive insulin regimen may be applied to maintain target blood glucose levels. Hosokawa et al. ( 18 ) recently reported that induced pluripotent stem cells may be a new therapeutic strategy for PF.
In summary, PF is characterized by poor maternal and infant outcomes and a high stillbirth rate. However, early recognition and treatment of FT1DM is crucial in preventing unfavourable pregnancy outcomes ( 19 ). The current patient had been diagnosed with GDM in the second trimester 5 weeks prior to presenting with influenza-like symptoms. She then experienced an acute onset of hyperglycemia, with ketoacidosis and reduced pancreatic islet cell function, but her HbA1c was not elevated. Together, these findings represent the typical clinical and laboratory features of PF. Moreover, patients with GDM are at risk of developing T1DM diabetes and a variety of autoimmune diseases. Islet autoimmunity may be involved in the development of PF, but the specific mechanism needs to be elucidated.
Supplementary
Acknowledgments.
We thank Dr. Andrew S. Day (University of Otago Christchurch, New Zealand) and Dr. Maria Ruth B. Pineda-Cortel (Research Center for the Natural and Applied Sciences, University of Santo Tomas, Philippines) for their critical comments and valuable advice on this study.
Funding: This study was granted by the Hainan Provincial Natural Science Foundation-Youth Cultivation Fund ( No. 822QN454 to Q.J.), National Natural Science Fund Cultivating 530 Project of Hainan General Hospital - Youth Cultivation Fund Project ( No. 2021QNXM09 to Q.J.), Hainan Health Science and Education Project ( No. 21A200219 to Q.J.) and project supported by Hainan Province Clinical Medical Center (to Q.J.).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All the procedures performed in this study were conducted in accordance with the ethical standards of Hainan General Hospital and the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-52/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-52/coif ). Q.J. reports that this study was granted by the Hainan Provincial Natural Science Foundation-Youth Cultivation Fund (No. 822QN454 to Q.J.), National Natural Science Fund Cultivating 530 Project of Hainan General Hospital - Youth Cultivation Fund Project (No. 2021QNXM09 to Q.J.), Hainan Health Science and Education Project (No. 21A200219 to Q.J.) and project supported by Hainan Province Clinical Medical Center (to Q.J.). The other authors have no conflicts of interest to declare.
- AME Case Rep. 2024; 8: 83.
Peer Review File
Available at https://acr.amegroups.com/article/view/10.21037/acr-24-52/prf

IMAGES
COMMENTS
Background: Fetal macrosomia, defined as a birth weight ≥ 4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation.
Background: Fetal macrosomia, defined as a birth weight ≥ 4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The ...
Introduction and background. Gestational diabetes mellitus (GDM) is a metabolic condition of pregnancy that presents as newly developing hyperglycemia in pregnant women who did not have diabetes before getting pregnant, and it normally resolves after giving birth [].]. Around 9% of pregnancies around the globe are affected by this prevalent antepartum condition [].
Gestational diabetes mellitus (GDM) is a state of hyperglycemia (fasting plasma glucose ≥ 5.1 mmol/L, 1 h ≥ 10 mmol/L, 2 h ≥ 8.5 mmol/L during a 75 g oral glucose tolerance test according to IADPSG/WHO criteria) that is first diagnosed during pregnancy [ 1 ]. GDM is one of the most common medical complications of pregnancy, and its ...
Fetal macrosomia is a common adverse infant outcome of GDM if unrecognized and untreated in time and is at an increased risk of becoming overweight or obese at a young age and are more likely to develop type II diabetes later in life. Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational ...
FOCUS Macrosomic fetuses in diabetic pregnancies develop a unique pattern of overgrowth, involving the central deposition of subcutaneous fat in the abdominal and interscapular areas Gestational Diabetes Mellitus and Macrosomia: A Literature Review by Kamana KC et al. Key insights Fetal macrosomia is a term used to define newborns who are significantly larger than average (birth weight ≥ ...
Gestational diabetes mellitus (GDM) is defined as glucose intolerance of variable degrees with an onset, or first recognized, during pregnancy. About 15-45% of babies born to diabetic mothers can have macrosomia, which is a 3-fold higher rate when compared to normoglycemic controls. Macrosomia is typically defined as a birth weight above the ...
(macrosomia, LGA, small-for-gestational-age [SGA]), preterm delivery, birth trauma, metabolic sequelae (e.g., hypoglycemia) or mortality, and 3) presented data in text or tables that allowed for
Summary When adjusted for confounders, gestational diabetes mellitus was signi cantly associated with a range of adverse pregnancy outcomes. Study design Systematic review and meta-analysis. Data sources 156 Overall risk of bias: 7 506 061 studies 19% low, % medium, % high pregnancies were evaluated.
We searched the mobile application market and literature database using the keywords of "gestational diabetes mellitus," "diabetes in pregnancy," "GDM," and "app" to identify GDM-related apps. By analyzing the functions and features of these apps, we gained insight into the current development status and functionality of these apps.
Abstract. Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation ...
Abstract. Gestational diabetes mellitus (GDM) is a metabolic complication of pregnancy. The pathogenesis of GDM is considered to involve β-cell dysfunction and insulin resistance (IR). GDM is associated with a significant risk of macrosomia in addition to a high probability of metabolic complications for the offspring.
1. Introduction. Gestational diabetes mellitus (GDM) is defined as any degree of glucose intolerance with onset or first recognition, and overt diabetes before pregnancy was excluded [1].The prevalence of GDM is increasing globally in recent years, affecting 1%-14% of all pregnancies and offspring [2].It is widely accepted that GDM is associated with serious pregnancy complications and short ...
Previous GDM is also associated with cardiovascular risk factors such as obesity, hypertension, and dyslipidemia ( 274, 278-280 ). The lifetime risk of cardiovascular disease following GDM is almost 3-fold higher in women who develop type 2 diabetes and 1.5 fold higher even in women without type 2 diabetes ( 280 ).
Gestational diabetes mellitus (GDM), which is defined as a state of hyperglycemia that is first recognized during pregnancy, affects approximately 15% of pregnancies worldwide [1]. Prevalence of ...
1. In 2016 in the United States, pre-existing (including type 1 or 2) and gestational diabetes mellitus (GDM) had a prevalence of 0.9% and 6.0%, respectively, among women who delivered a live infant. 2. Recently, efforts have redoubled to diagnose and treat diabetes earlier in pregnancy. 3.
Europe PMC is an archive of life sciences journal literature. This website requires cookies, and the limited processing of your personal data in order to function.
Fetal macrosomia, defined as a birth weight ≥ 4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the ...
Gestational diabetes mellitus (GDM) is a known risk factor for macrosomia [ 11 ], with recent estimates suggesting that between 15 and 45% of newborns of mothers with GDM are macrosomic compared with 12% in children of non-GDM mothers [ 12 ]. Epigenetic reprogramming in the in utero environment is one suspected driver of this relationship.
Gestational diabetes mellitus (GDM) is one of the most common complications of pregnancy and is defined as the onset or the first discovery of glucose intolerance during pregnancy 1.Worldwide, it ...
Introduction. Gestational diabetes mellitus is defined as any degree of glucose intolerance with an onset during pregnancy [Citation 1-4].Pregnancy is associated with significant changes in hormonal and metabolic elements in order to ensure adequate fetal nutrition [Citation 5, Citation 6].Dysregulation of insulin levels may increase the risk of gestational diabetes [Citation 4, Citation 7-9].
This study aimed to assess the need for practice-wide quality improvement to support evidence-based type 2 diabetes screening for women with a history of gestational diabetes mellitus (GDM) receiving primary care. We sought to add the diagnosis of GDM to the problem list of women who did not have it at baseline.
Gestational diabetes mellitus (GDM) affects both immediate and future disease risk in the offspring. We hypothesized that GDM alters miRNA expression in human umbilical vein endothelial cells (HUVECs) that may influence metabolic processes. ... (IGDM) and infants born to normoglycaemic controls. miRNAs were identified using microarray profiling ...
BACKGROUND: Fetal macrosomia, defined as a birth weight ≥ 4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through ...
Fitria N, van Asselt ADI, Postma MJ. Cost-effectiveness of controlling gestational diabetes mellitus: A systematic review. Eur J Health Econ. 2019; 20:407-417. [PMC free article] [Google Scholar] Kamana K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: A literature review. Ann Nutr Metab 2015; 66 (Suppl.): 14-20.
Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation. As a ...
Background: Women with gestational diabetes mellitus (GDM) have lower rates of exclusive breastfeeding compared with women without diabetes. Objectives: To assess associations between GDM and breastfeeding intentions and attitudes, formula supplementation, reasons for formula supplementation, and knowledge of type 2 diabetes mellitus (T2DM) risk reduction associated with breastfeeding among U ...
Background: Gestational diabetes mellitus (GDM) is a form of diabetes that develops during pregnancy. The incidence of GDM has been on the rise in tandem with the increasing prevalence of obesity worldwide. ... Kc K., Shakya S., Zhang H. Gestational Diabetes Mellitus and Macrosomia: A Literature Review. Ann. Nutr. Metab. 2015; 66:14-20. doi ...
Gestational diabetes mellitus (GDM) occurs during pregnancy and is harmful to both the mother and fetus . Unfortunately, few studies have examined the possible correlation between GDM and PF. ... This report summarizes the clinical features of this patient along with review of the relevant literature with the aim to extend understanding about ...